Abstract
Despite high consultation rates, little is known about predictors of primary care use by older people. A survey of patients aged ≥65 years from two London practices included details on physical health and functioning, psychological measures, social support, and socioeconomic measures. The response rate was 75% (1704/2276). We obtained consent to link the survey data to subjects' computerised primary care records for 92% (1565/1704) of responders. Individual factors (physical ill health, anxiety, female sex), social factors (frequent telephone contact with friends or family), and practice factors independently predicted consultation in the year post survey. Although physical ill health was the most important, the other factors had independent effects and may be useful in understanding the increase in consulting by older people.
Keywords: health services for the aged, medical record linkage, primary care, surveys
Introduction
PHYSICAL ill health and psychological and social factors predict primary care consultations in adults, but little work has focused on older people (≥65 years),1 despite their high and steadily increasing use of primary care services.2 United Kingdom (UK) surveys of older people have good data on the predictors of primary care use,3,4 but are limited by reliance on self-reported consultation measures, which are prone to recall bias. General practice databases and the fourth national morbidity study have reliable consultation data, but the former lack any background individual measures2 and the latter lacks information on psychological factors and disability.5 To predict primary care use by older people, accurate information on consultations from records needs to be linked with detailed information on individuals, and this now requires individual informed consent.6 Of the UK studies seeking consent for patient records to be accessed for medical research, only one has actually linked survey data to electronic records, and this was based on adults rather than older people.7 We aimed to demonstrate the feasibility of obtaining older peoples' consent to link survey data with their computerised primary care records and to use these linked data to predict consultations.
Method
The detailed survey methodology has been published elsewhere.8 Participants consisted of patients aged 65 years and over (n = 2843) registered with two fully computerised London group general practices. Practices excluded those with terminal illness or dementia, and identified those who were more appropriate for interview, including, for example, those who were frail or had poor vision. A postal survey was conducted, and assistance in completion offered. It was sent again to non-responders after 4 weeks. Information on consultations was downloaded for those giving consent, for the period 2001 to 2002, 1 year after survey completion at that practice. The outcome variable was the total number of consultations per individual for the year following the questionnaire return date (Figure 1). The questionnaire included standardised measures, which are highlighted as potential predictors of consulting by older people:1,3-5 physical health and functional status; psychological factors, including depression, anxiety and health beliefs; social networks and support; and socioeconomic factors. This has been described in detail previously,8 except for the anxiety score (Table 1). This was measured using a four-item version of the Anxiety Disorder Scale; the FEAR (frequency of anxiety; enduring nature of anxiety; alcohol or sedative use; restlessness or fidgeting), developed and validated for use as a rapid screening instrument in primary care.10
Figure 1.
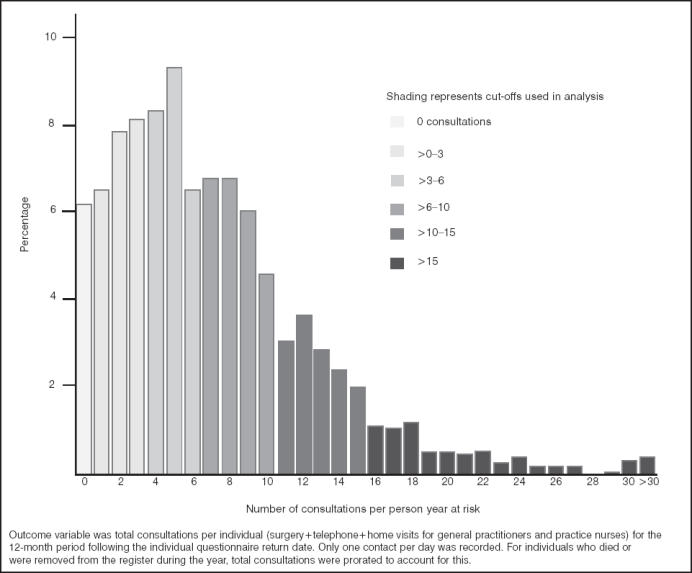
Distribution of consultation rates for 12-month period following questionnaire (n = 1481), mean = 7.1 (standard deviation = 5.8), range = 0–49.
Table 1.
Factors selected into the best-fit model for predicting consultations by older people.
| n (%) | Odds ratios (95% CI) adjusted for age, sex and practicea | Odds ratios (95% CI) adjusted for factors in the final modelb | P-value | |
|---|---|---|---|---|
| Age in years (n = 1481) | ||||
| 65–69 | 350 (24) | 1 | 1 | |
| 70–74 | 365 (25) | 1.0 (0.8 to 1.3) | 0.9 (0.7 to 1.2) | 0.594 |
| 75–79 | 330 (22) | 1.5 (1.1 to 1.9) | 1.2 (0.9 to 1.6) | 0.222 |
| 80–84 | 227 (15) | 1.7 (1.2 to 2.2) | 1.4 (1.0 to 1.9) | 0.033 |
| ≥85 | 209 (14) | 1.3 (0.9 to 1.7) | 1.1 (0.9 to 1.6) | 0.480 |
| Sex (n = 1481) | ||||
| Male | 568 (38) | 1 | 1 | |
| Female | 913 (62) | 1.5 (1.2 to 1.8) | 1.3 (1.1 to 1.6) | 0.013 |
| Practice (n = 1481) | ||||
| 1 (suburban) | 878 (59) | 1 | 1 | |
| 2 (inner city) | 603 (41) | 1.6 (1.3 to 1.9) | 1.4 (1.2 to 2.0) | <0.001 |
| General health (n = 1465) | ||||
| Very good/good | 852 (58) | 1 | 1 | |
| Fair | 519 (35) | 1.8 (1.5 to 2.2) | 1.4 (1.1 to 1.7) | 0.003 |
| Bad/very bad | 94 (7) | 3.3 (2.2 to 4.8) | 2.0 (1.3 to 3.1) | 0.002 |
| Disease scorec (n = 1481) | ||||
| 0 | 408 (28) | 1 | 1 | |
| 1 | 574 (39) | 2.0 (1.6 to 2.6) | 1.9 (1.5 to 2.5) | <0.001 |
| 2 | 339 (23) | 2.8 (2.2 to 3.7) | 2.5 (1.8 to 3.3) | <0.001 |
| 3 or more diseases | 160 (11) | 5.7 (4.0 to 8.0) | 4.6 (3.2 to 6.6) | <0.001 |
| Telephone contact with friends or relatives (n = 1446) | ||||
| Monthly or less | 208 (14) | 1 | 1 | |
| Weekly | 673 (47) | 1.6 (1.2 to 2.1) | 1.7 (1.3 to 2.3) | <0.001 |
| Daily | 565 (39) | 1.7 (1.2 to 2.2) | 1.8 (1.4 to 2.5) | <0.001 |
| Anxiety scored (n = 1410) | ||||
| 0 (low) | 714 (51) | 1 | 1 | |
| 1–2 (medium) | 570 (40) | 1.4 (1.2 to 1.8) | 1.3 (1.0 to 1.6) | 0.020 |
| 3–4 (high) | 126 (9) | 2.5 (1.8 to 3.6) | 1.9 (1.3 to 2.7) | 0.001 |
aOdds ratios from ordered logistic regression of total number of consultations/individual/year following questionnaire. Age was fitted in 5-year bands, as its effect was not linear.
bOdds ratios from forward stepwise ordered logistic regression of total number of consultations/individual/year following questionnaire.
cA disease score for each subject was calculated from an adapted checklist of doctor-diagnosed chronic conditions.8 All diseases considered likely to be currently active were included in the score: angina, stroke, high blood pressure, chronic bronchitis, asthma, diabetes, and arthritis.
dAnxiety symptoms were measured using a four-item version of the Anxiety Disorder Scale.10
HOW THIS FITS IN
What do we know?
Older people are major primary care consulters, and consultation rates among older people are increasing year by year. Studies on adult frequent attenders have shown that physical ill health and psychological and social factors are all important predictors of consulting, but studies on older people have been limited by self-reported consultation measures.
What does this paper add?
The majority of older people are happy to give their consent for a health and social survey to be linked with their computerised primary care records. Physical ill health was the main predictor of consulting in older people, but after controlling for this, psychological and social factors as well as sex and practice factors also independently predicted consulting.
Ethical approval was given by the Wandsworth Local Research Ethics Committee.
Analysis
Consultation rates did not follow Poisson or negative binomial distributions, therefore associations between consultations and other factors were modelled using ordered logistic regression with multiple cuts to increase power (Figure 1). Results were expressed as odds ratios with 95% confidence intervals. Initial adjustments were for age, sex and practice. A best-fit model for predicting consultations was selected using forward stepwise ordered logistic regression (P<0.05) with age, sex and practice locked into the model. The odds ratios presented are from the maximal dataset, n = 1369.
Results
Out of 2843 participants, 149 (5.2%) had dementia and 118 (4.2%) were excluded by general practitioners (GPs) and district nurses for other health reasons; 300 (10.6%) had moved or died. This gave a response rate of 75% (1704/2276), of whom 92% (1565/1704) gave consent for questionnaire and medical record linkage. Variations between practices in contact and recording of contacts for participants in residential and nursing homes (n = 84), meant these were excluded from the analysis, which is restricted to 1481 older people living in the community.
Table 1 shows the factors selected into a model for predicting consultations. Increasing age was positively associated with consulting, but not after controlling for other factors in the final model. Women consulted more than men and subjects from Practice 2 (inner city) consulted more than subjects from Practice 1 (suburban). However, factors related to consulting were the same in the two practices. The strongest consultation predictors were physical ill health measures; the two selected into the final model were self-reported general health and the number of chronic diseases. Disability and pain were initially associated with consulting (data not shown), but not after controlling for other measures of physical ill health. In terms of psychological and behavioural factors, subjects with higher anxiety levels were more likely to consult. Higher depression scores, being a non-smoker and health belief measures were associated with consulting (data not shown), but were not selected into the final model. Most measures of social support were not associated with consulting; only frequency of telephone contact with friends or relatives was positively associated with consulting and selected into the final model. Although there were some weakly positive associations between socioeconomic measures of deprivation and consulting (data not shown), none of these remained after controlling for physical ill health, and none were selected into the final model.
Discussion
The study methodology was successful and could be more broadly applied. Ninety-two per cent of responders gave consent to record linkage, compared with 70% in adults ≥18 years7 and 99% in women aged 60–79 years.9 At a time when it is becoming more difficult to undertake this type of research, it is reassuring that older people of both sexes show their willingness to participate. Our study showed similar consulting patterns by age, sex, smoking status and between–practice variation to the fourth national morbidity survey.5 Other UK studies of older people have shown that disability predicts consulting.3,4 We showed that its effect is not independent of physical ill-health measures. Anxiety has previously been shown to independently predict consulting by older people,3 but using cross-sectional data and self-reported consultation measures, which may have been prone to recall bias. We confirm this finding, linking data on symptoms prospectively to a robust consultation measure. To our knowledge, a relationship between consulting and increased social contact has not been shown before for older people in the UK. This study emphasises that, as well as physical ill health, other individual factors (anxiety, sex), social contact, and practice factors may influence consulting by older people in primary care. This may help the process of understanding the year-on-year increase in consulting by older people, with its workload implications for primary care.2
Acknowledgments
We thank the two practices involved (Benhill and Belmont Practice, Sutton; and Bridge Lane Health Centre, Battersea, London) and all of the participants who gave their time to respond to the survey and their consent for us to link it to their primary care records. Thanks also to Pit Rink and Sunil Shah for their involvement early on in the study, particularly with questionnaire development. The BUPA Foundation funded the study.
References
- 1.Gill D, Sharpe M. Frequent consulters in general practice: a systematic review of studies of prevalence, associations and outcome. J Psychosom Res. 1999;47:115–130. doi: 10.1016/s0022-3999(98)00118-4. [DOI] [PubMed] [Google Scholar]
- 2.Rowlands S, Moser K. Consultation rates from the general practice research database. Br J Gen Pract. 2002;52:658–660. [PMC free article] [PubMed] [Google Scholar]
- 3.Vetter NJ, Jones DA, Victor CR. The importance of mental disabilities for the use of services by the elderly. J Psychosom Res. 1982;26:607–612. doi: 10.1016/0022-3999(82)90076-9. [DOI] [PubMed] [Google Scholar]
- 4.Iliffe S, Tai SS, Haines A, et al. Assessment of elderly people in general practice. 4. Depression, functional ability and contact with services. Br J Gen Pract. 1993;43:371–374. [PMC free article] [PubMed] [Google Scholar]
- 5.McCormick A, Fleming DM, Charlton J. Morbidity statistics from general practice. Fourth national study, 1991–1992. London: HMSO; 1995. [Google Scholar]
- 6.Coleman MP, Evans BG, Barrett G. Confidentiality and the public interest in medical research — will we ever get it right? Clin Med. 2003;3:219–228. doi: 10.7861/clinmedicine.3-3-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jordan K, Ong BN, Croft P. Previous consultation and self reported health status as predictors of future demand for primary care. J Epidemiol Community Health. 2003;57:109–113. doi: 10.1136/jech.57.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris T, Cook DG, Victor C, et al. Predictors of depressive symptoms in older people. A survey of two general practice populations. Age Ageing. 2003;32:510–518. doi: 10.1093/ageing/afg087. [DOI] [PubMed] [Google Scholar]
- 9.Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ. 2003;327:712–717. doi: 10.1136/bmj.327.7417.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krasucki C, Ryan P, Ertan T, et al. The FEAR: a rapid screening instrument for generalised anxiety in elderly primary care attenders. Int J Geriatr Psychiatry. 1999;14:60–68. doi: 10.1002/(sici)1099-1166(199901)14:1<60::aid-gps893>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]


