
WILLIAM Pickles demonstrated that by collecting simple information from a practice over many years, it is poss-ible to make important discoveries concerning the nature of health and illness in local communities. This work was helped by his long-term knowledge of patients and families, and by the natural bonds of goodwill and helpfulness that exist between local communities and their general practitioners (GPs). Three types of more recent family study are described: using simple population data to sample families for investig-ations of susceptibility to diet, the pathophysiology of disease, and perceptions and understandings of familial risk. Research of this nature is increasingly relevant as new genetic technologies are developed and applied, and require not only increased collaboration between GPs; epidemiologists; and clinical, laboratory, and social scientists, but also sustainable relationships with families and communities. General practice is the ideal setting for such research, with its hallmark features of continuity, mutuality, and trust.
Introduction
With the rapid development and application of new methods of genetic investigation, there is unprecedented interest in studies of health and illness in families. Beginning with the work of William Pickles, this lecture describes a series of family studies, based in general practice and in local communities, and considers their relevance for future research and clinical practice.
In the first RCGP Mackenzie Lecture,1 William Pickles recalled:
‘… a particularly lovely evening in early summer, when I climbed alone to the summit of one of our noble hills. One by one, I made out our grey villages with their thin pall of smoke. And as I watched the evening train creeping up the valley with its pauses at our three stations, a strange thought came into my head that there was hardly a man, woman or child in all those villages of whom I did not know even the Christian name and with whom I was not on terms of intimate friendship.’
In A Fortunate Man,2 John Berger describes the landscape as a curtain, behind which human stories unfold. In their daily work, GPs have unique, privileged access ‘behind the curtain’ to the lives and circumstances of their patients. The information is useful clinically, informing core aspects of general medical practice such as holism, coordination, continuity, and tolerance of uncertainty. Such features of practice do not require long-term knowledge of patients, but they are often enhanced by it.
Pickles also applied his local knowledge to research. Over a 20-year period, he charted nearly 9000 cases of infectious disease in his practice.3 In a self-contained community, where travel was limited and incomers were few, Pickles used local knowledge to track and explain the incidence and spread of infection, providing original information on the incubation periods of several infectious diseases, such as Bornholm's disease and hepatitis. He was 45 years old when his first paper from practice was published.
What he did was extraordinary, but he did it in an ordinary place and his methods were simple. Several other GPs, including John Fry4 and Keith Hodgkin5 followed his example by collecting practice data over a long period of time to obtain otherwise unknowable perspectives about the nature of health and illness in practice populations. Franz Huygen, a Dutch GP, used a similar approach in charting the occurrence of illnesses in successive generations of families.6
Family studies at Wensleydale
Pickles is not known for family studies, but in the 1930s he carried out a Medical Research Council (MRC) study on consanguinity in his practice, enquiring into the blood relationship, if any, between husbands and wives in 500 married couples.7 He found it a little embarrassing to ask his married patients if they were related in this way. One farmer's wife replied with Yorkshire bluntness: ‘Do you think we're a bit funny, then?’. Pickles commented:
‘These are just the people to help a doctor in his investigations. Matters so delicate as heredity and consanguinity have to be approached with care and tact, but I have found my own patients co-operative, and slow to take offence’.
In 1943, he published a paper in The Lancet,8 which mapped the occurrence of rheumatic heart disease in 23 out of 53 descendants of an incident case. He wrote:
‘After 30 years' close experience, I have no hesitation in singling these people out as among the most outstanding in the district. With insignificant exceptions they are prosperous, well-housed and well-fed. They are as a rule, successful farmers, but a switch-over to other occupations has simply meant adaptation of talents and successes in a new sphere. Yet none of these sufferers has up to the present died from heart disease at an early age. It may be that the environment has hitherto been so favourable for this family that it has helped family members in part to elude the shackles of inheritance’.
Families share environments and habits, as well as their genes, and it is the interaction that counts. Pickles' observation and insight remind us that there is more to life, health, and illness than the genetic prescription with which we are born.
Family studies at Glyncorrwg in South Wales
The South Wales coalfield contains many small communities, which are very different in social composition from Wensleydale, but they are well defined and ideal for epidemiological study. This is where Archie Cochrane pioneered the modern practice of population-based research.9
Most people have heard of the Cochrane Collaboration, — the intellectual driving force of evidence-based medicine — but Cochrane himself pioneered a different type of collaboration in which whole communities took part in research projects to describe and explain the occurrence of major diseases.
In the Rhondda Fach, for example, his colleague Bill Miall showed that, on average, there is a straight line relationship between the blood pressure levels of family members. At any level of pressure, the blood pressures of first-degree relatives tend to resemble each other.10
Julian Tudor Hart worked on Cochrane's team, but the doctor in him recoiled at simply observing people when clearly they had illnesses needing medical attention. So he left, and in 1961 set up in single-handed practice in Glyncorrwg, at the top of the Upper Afan valley in West Glamorgan, where he and his wife Mary spent the next 30 years.11
When I arrived for work in Glyncorrwg in 1980, as an MRC research registrar, Julian had already applied Cochrane's techniques of population coverage to the management of clinical problems in general practice, and was the first GP to have measured the blood pressures of all his patients. He was in his early 40s when this work was published in The Lancet.12
Despite clinical, epidemiological, and public health interest, no-one had managed to show a convincing relationship between salt intake and blood pressure in individuals.13 We thought it might be possible to do this by looking at families with contrasting susceptibility to high blood pressure.
Bill Miall had provided the map, but while most family history studies had compared families with or without one hypertensive parent (Figure 1a), the population approach to screening at Glyncorrwg made it possible to compare families in which parents either both had high or both had low blood pressure (Figure 1b), thus increasing the contrast in susceptibility between offspring.14
Figure 1.
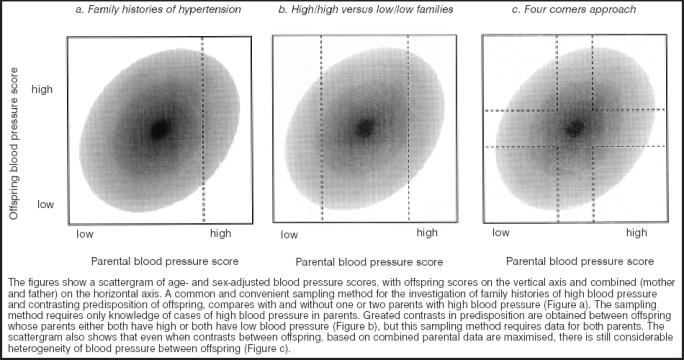
Sampling methods for offspring with contrasting familial predisposition to high blood pressure.
The technology was simple. Ingested salt is excreted in urine, so measurement of salt intake requires a 24-hour urine collection. However, because intakes vary from day to day, individual characterisation required seven consecutive 24-hour collections. We became milkmen in reverse, delivering empties and picking up full bottles in return.
Response rates were about 90%. Completeness was judged, not on the basis of chemical markers, or adjustments for creatinine, but on an honest exchange with participants. We explained that we had done what we were asking them to do, we knew it was difficult, but that much worse than incomplete collections were incomplete collections we did not know about — so would they please let us know if a 24-hour collection was not complete, so that we could inform the statistician. This wasn't research on the community — it was research with the community.
We found no difference in salt intake between sons and daughters with and without a familial disposition to high blood pressure,15 but all intakes were high — 7–10 g per day — and we couldn't exclude the possibility that some people were more susceptible than others to the effect of such high intakes.
Testing this hypothesis required an experiment, comprising what is still the only randomised controlled trial of lowering salt intake in a free living population in the United Kingdom (UK). For 10 weeks, everyone reduced their salt intake to that of a South Seas islander (less than 3 g per day) Low sodium bread was baked and delivered, along with many other specially prepared low-salt foods. Throughout the period everyone took part in a randomised, double-blind, controlled trial, in which they took either salt tablets, bringing their salt intake back up to normal, or placebo. It was a brilliantly simple study design.
When comparing two periods with salt intakes below 3 g and above 8 g per day, there was no difference in blood pressure in either group of offspring.16 We could not exclude the susceptibility hypothesis entirely, but we discounted the idea that there are some people for whom the huge effort and upheaval of sodium restriction is quickly worthwhile.
During the tea interval that followed the presentation of these results at an international meeting in Finland, I was approached by a small, elderly gentleman, speaking with an impeccably polite English accent — Professor Fred Epstein of Zurich, who was formerly one of the pioneers of cardiovascular epidemiology in the United States.
At the Tecumseh Community Health Study in Michigan, his team had also found that blood pressure aggregates in families,17 and that the likelihood of offspring having high blood pressure was highest when both parents had high blood pressure and lowest when both parents had low blood pressure. The map that he sketched (Figure 2), however, showed that even with such contrasting parental blood pressures, there were some offspring whose blood pressures were markedly different from those of their parents — low offspring of high parents and high offspring of low parents — offspring, who in Pickles' phrase, had ‘eluded the shackles of inheritance’. I wondered, what is the difference between such offspring? Might this provide a clue to the pathophysiology and genetics of high blood pressure?
Figure 2.
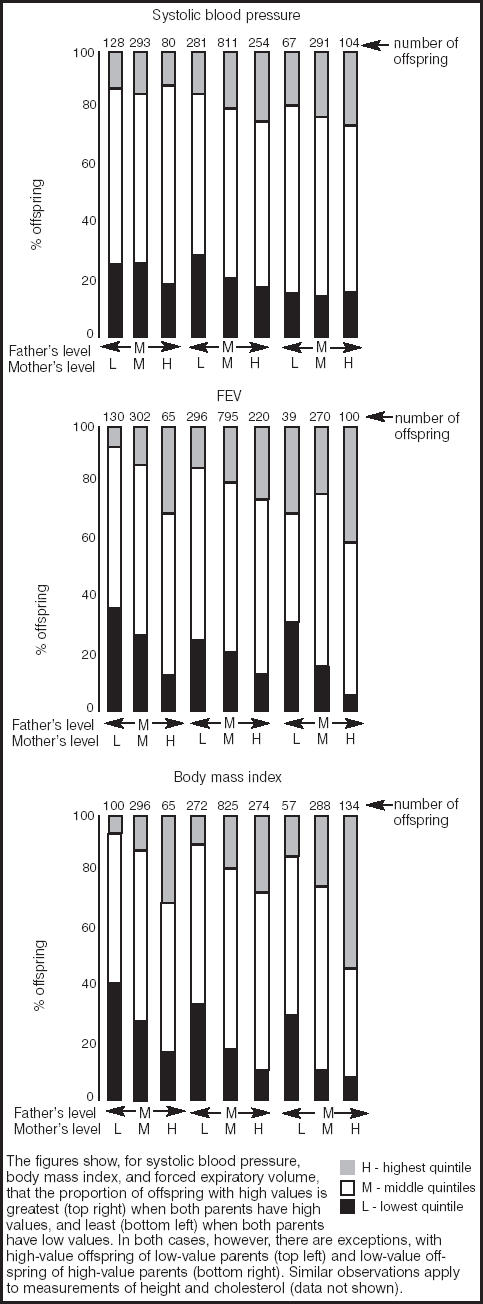
Familial aggregation of quantitative traits.
Family studies at Ladywell
I gave it no more thought, but remembered this conversation and map when continuing my GP training at Ladywell Medical Centre in Edinburgh. Some years earlier, the senior partner of the practice had pioneered ‘family portraits’ as a method of recording basic family information in case notes,18 but more significantly, both of the practices at the medical centre were participating in the MRC mild hypertension trial.19 Eighteen hundred and six married couples had taken part in the screening phase of the study 8 years previously. With a grant of only £11 000 from the Scottish Office, we were able to track down and measure blood pressure in 864 young adults, aged 16–24 years, from 603 families.
The data allowed us to reconstruct Professor Epstein's map, in the form of a scattergram (Figure 1c). The key point is that even at the extremes of parental blood pressure, low on the left and high on the right, and even though the offspring of parents with high blood pressure already have higher pressures, there is still considerable variation between offspring. We set out, therefore, to study offspring from the four corners of the figure.
The protocol involved 100 sons travelling from Edinburgh to Glasgow for admission to the MRC blood pressure unit, fasting overnight for an oral glucose tolerance test in the morning, and having their renal function and adrenergic responses monitored during a test of mental arithmetic.
It was an improbable thing to ask young adults to do, but we had several advantages, including the loyalty and good will of patients served by two particular general practices, the interest and help of the practice teams, and the natural interest and enthusiasm that exists for family studies.
In summary, we found in these and other studies that the group of offspring with high personal and parental blood pressures differed from the three other groups of offspring in several respects, including pulse and adrenergic responses to a glucose load,20 renal function,21 the number and reactivity of small blood vessels in the nailbed,22 and their sensitivity to glucocorticoids.23,24
The results are remarkable, because the group was not a highly selected distillate of patients, of the type found in most hospital research studies, but came instead from a carefully defined group of families within a typical UK general practice, representing, in this example, 14% of the general population (the top right corner in Figure 1c). The practice and population are not significantly different from the 190 other practices that participated in the MRC trial.
The findings lend support to the prediction made by Professor John Bell of Oxford that there is a new taxonomy of disease waiting to be described, based on pathophysiology rather than signs and symptoms, with origins that we understand at a molecular level, and with the potential to transform clinical medicine.25 The source of such information lies not in academia, nor in teaching hospitals, but in long-term studies in the community. Focusing on families does not necessarily lead to the identification of genetic pathways, but it does help to identify groups of individuals in whom such evidence is most and least likely to be found.26
Family studies in Renfrew and Paisley
In the early 1970s, Professor Victor Hawthorne set up the MIDSPAN study in Renfrew and Paisley, based on over 15 000 people aged 45–64 years, and comprising nearly 80% of the general populations of men and women in these two adjacent towns on the southwest border of Glasgow.27,28 Although it was not designed to be a family study, the effect of the high response rate in a single locality was to include over 4000 married couples. In 1996 we were able to trace and study 1040 adult sons and 1298 adult daughters from 1477 families, using the same methods used to study their parents over 20 years previously.29 The response rate of 72% compared favourably with the figure of 24% achieved more recently as part of the evaluation of a community heart disease prevention project, but we had two advantages —widespread community interest and loyalty to a long-term study. Although MIDSPAN is not based on general practices, the inclusion of 80% of the middle-aged population of two towns has meant that all general practices in the towns have been involved. Their cooperation has been central to the longevity of the study.
With its large number of variables collected in two generations, MIDSPAN shows that many quantitative traits, such as serum cholesterol, forced expiratory volume (FEV), height, and body mass index, aggregate in families in the same way as for blood pressure, with fascinating clusters and exceptions at both ends of the population distributions (Figure 2).
One of the most important findings from the original cohort study is the importance of respiratory function. Reduced forced expiratory volume is second only to smoking as an independent predictor of all-cause mortality — stronger than blood pressure, cholesterol, and social class.29 We were very interested, therefore, in familial aspects of respiratory function.
Within families, the effect of a mother smoking 10 cig-arettes per day over 20 years has the same effect on airflow limitation in offspring as 10 years of personal smoking.30 The same level of maternal smoking also increases the prevalence of chronic obstructive pulmonary disease in offspring who smoke by 70%. A parallel stream of work is looking at the familial aggregation of obesity. Work like this, requiring simple measurements from large numbers of fathers and mothers, is ideally suited to primary care.
Family medical histories
The follow-up data on parents have made it possible to investigate family medical histories. In this study it is known exactly and completely which parents have died of what. After 20 years, just over a quarter of sons and daughters had experienced a parent dying of heart disease. The experience was more common in older offspring and in working-class families. Although a few families had lost touch, virtually all offspring correctly reported the fact of death, and 90% the cause of death.31
We were interested in how this experience had affected them, and asked whether there were any conditions, weaknesses, or illnesses that ran in their family and, if so, what these were. Interestingly, only a third of daughters and a quarter of sons with the experience of a parent dying from heart disease felt that this meant ‘a family weakness’. The group least at risk of heart disease — affluent daughters — were most likely to perceive this as a family weakness, while the group at most risk — working-class sons — were least likely.31
If, in the future, we are going to advise patients about their genetic risks of cardiovascular disease, we need to understand why so few people feel affected by coronary deaths in their family.
We interviewed sons and daughters at length using a map based on questions in a general survey to divide sons and daughters into those with and without the experience of a parent dying from coronary disease, with and without the feeling that this affected them personally, and comparing offspring from working-class and middle-class backgrounds.32
Clinicians tend to define family histories of heart disease in terms of the fact, cause, and age of clinical events in rel-atives. Ordinary people recognise such definitions, but when considering whether the information applies to them personally, also take into account which ‘side’ of the family they take after, and whether there are any reasons, positive or negative, that make it possible to detach themselves from the experience of an affected relative. Stereotypes are common. For example:
‘One of my friends was a taxi driver, a big chap, overweight, always perspiring and always eating fries and I thought to myself, he's heading for a, you know, heart attack, and sad to say he did, and has since died’.
However, there are exceptions:
‘For every one fit … you think there's another bloke going about, smoking and beer belly out to here, and living for ever and ever and seeming to have no adverse effects anyone can see. What's going on?’
This figure, who has been called Uncle Norman, looms large in public consciousness as the person who defies medical advice and lives to tell the tale. On the other hand:
‘I know a few people that have had heart problems and they'd be the last people you'd think of, you read in the paper about people that's out jogging and athletes that have heart problems, one of the fittest men you would look at on television is Graeme Souness, he's had a triple bypass operation, he'd be the last person on earth you'd think’.
The ‘last person you'd think’ is another powerful image in the public mind. Epidemiologists recognise these stereotypes as false positive and false negative characterisations of risk.
In the MIDSPAN Family Study we looked at coronary and stroke mortality in 4002 fathers divided into five quintiles of the distribution of blood pressure, measured at baseline and each containing about 800 men (Table 1). Men in the top quintile (Q5) were at greatest risk of dying from coronary heart disease (CHD) or stroke during the next 15 years (true positive identification of risk). Men in the bottom quintile (Q1) were most likely to avoid a CHD or stroke death (true negative identification of risk). But most men in the top quintile avoided a CHD or stroke death (false positives), and some men in the bottom quintile nevertheless died of CHD or a stroke (false negatives). Uncle Norman is a common character.33
Table 1.
Fifteen-year mortality follow-up by blood pressure quintile: results from the Renfrew and Paisley MIDSPAN study.a
| Q1 | Q2 | Q3 | Q4 | Q5 | |
|---|---|---|---|---|---|
| Number of men | 800 | 802 | 799 | 801 | 800 |
| Coronary deaths | 75 | 102 | 133 | 136 | 153 |
| Stroke deaths | 17 | 17 | 22 | 30 | 57 |
a4002 men were divided into 5 quintiles of the distribution of blood pressure, measured at baseline and each containing about 800 men.28
The truly last person is very rare, because there is usually some risk factor, although perhaps not a visible one, to explain the clinical event. Much more common is the person who succumbs despite having only moderate risk factor levels that are too low to merit treatment.
Therapeutically, we should like to stop treating the false positives and to start treating the false negatives, but to do this we need more precise methods of predicting outcomes in individuals. Simple case-control studies are of limited value, because the cases are a mixture of true positives and false negatives, while the controls are a mixture of true negatives and false positives. Sorting this out needs long-term studies in the community.
The social challenge of family-based studies
At Glyncorrwg in South Wales, we used routine practice blood pressure data to identify groups of offspring at contrasting risk, who then took part in a community experiment to test their susceptibility to dietary change. At Ladywell, in Edinburgh, we used a map based on screening blood pressure data to test the idea that important differences in the pathophysiology of high blood pressure could be observed between carefully defined groups of families within the general population. They can, and there are many such maps to explore.
The MIDSPAN study in the west of Scotland shows the value of longitudinal data, not only in defining family medical histories and individual responses to them, but also in ident-ifying exceptions to the rule — the false positive and false negative characterisations — who have ‘escaped the shackles of inheritance’. MIDSPAN also shows the multifaceted nature of a family study population. We do not need separate primary care research networks for cancer, heart disease, mental health, and so on.34 Generalist primary care research networks can contribute to research in all of these areas.
Such studies require closer collaboration between family doctors; epidemiologists; and clinical, laboratory, and social scientists. A greater challenge concerns our social imagination. Can we develop the sustained relationships with families and communities on which these types of study depend?
Many of the early attempts to capitalise on new technol-ogies for genetic research can be likened, in their simplicity, naivety, and hopefulness, to early prospectors panning for gold. Colleagues with expertise in laboratory techniques and clinical measurement seem to lose all sophistication when they venture outside the teaching hospital and consider the implications of carrying out research in the community, where people are people, not patients; wear clothes not pyjamas; and have real lives and jobs and families. Some prospectors will be lucky, but this is not the way forward. Whether digging for treasure or mining for gold, serious investigators equip themselves with a map and the best technology.
The goldmine analogy is appropriate. There are riches to be found, but the necessary technology is analogous to deep mining, not panning in a river. Resources have to be invested in the right place. I have described several types of map that can indicate where best to target resources.
Archie Cochrane is not usually thought of as a Welsh miner, but his team successfully mined community reserves of helpfulness and goodwill for scientific ends in a way that may still turn out to be his most important legacy. By working in South Wales he was able to take advantage of the natural cohesion and solidarity of mining communities. Glyncorrwg was such a place. Ladywell, however, is in Corstorphine, an affluent, traditional Edinburgh suburb, while Renfrew and Paisley are post-industrial, urban environments, with high levels of all-cause mortality and socioeconomic deprivation. There is nothing special or unique about these settings.
General practice is the obvious setting for this work because of the good relationships that exist between primary healthcare teams and the communities they serve, and the facility with which contact can be maintained over long periods. Compared with any other way of carrying out long-term studies, continuity is our trump card, because of the facility of keeping in touch with families via parents.
In a mining village, all the passing visitor sees is the pithead. A visitor does not see the countless interdependent social relationships at work, at play, and at home, on which a mining community depends. One would need to stay longer, to look beyond the landscape, behind the curtain, to see the richness of the society that is hidden from view.
I like to think that a general practice population has many of these features, and that the three studies I have described illustrate the potential for collective action in such a setting. Such research is still possible, but only if we invest in maps, in people, and in relationships. Following the deep mining analogy, we need substantial investment in a few settings, rather than minor investment in many. There is also a need for more academics who can approach these issues from a general practice perspective.
Improving our understanding of the epidemiology of health and disease in families, and applying this information in clinical practice needs GPs who know their communities well. For William Pickles and Julian Tudor Hart, this part of their professional life began after the age of 40 years. I hope that this will encourage others to build in this way on their know-ledge and experience as generalist medical practitioners.
Acknowledgments
I wish to acknowledge and thank the large number of colleagues who have contributed to this series of family studies: Julian Tudor Hart, Mary Hart, Catherine Edwards, Pam Walton, Evelyn Thomas, Georgina Bingham, and Chris Foy at Glyncorrwg; Fred Epstein and Millicent Higgins of the Tecumseh Community Health Study, Michigan; David Holton, Hugh Edwards, Stephen Harrap, Brian Walker, Boyd Moir, Gillian Davidson, Margaret McMillan, Jessie Rutherford, and Tony Lever for their contributions to the Ladywell family blood pressure study, Edinburgh; and Victor Hawthorne, Charles Gillis, David Hole, Carole Hart, Mark Upton, Catherine Ferrell, Jane Goodfellow, Claire Bidwell, Alex McConnachie, Kate Hunt, Carol Emslie, and Niveen Abu-Rmeileh for their contributions to the MIDSPAN Family Study, Renfrew and Paisley.
Footnotes
This text is based on the William Pickles Lecture, which was delivered at the Spring Symposium of the Royal College of General Practitioners at the Royal Bath Hotel, Bournemouth, on 25 April 2004.
References
- 1.Pickles WN. Epidemiology in the Yorkshire Dales. Practitioner. 1955;174:76–87. [PubMed] [Google Scholar]
- 2.Berger J. A fortunate man. London: Penguin; 1969. [Google Scholar]
- 3.Pickles WN. Epidemiology in country practice. London: Royal College of General Practitioners; 1984. [Google Scholar]
- 4.Fry J. Common diseases: their nature, incidence and care. Lippincott: Philadelphia; 1979. [Google Scholar]
- 5.Hodgkin K. Towards earlier diagnosis: a guide to primary care. Edinburgh: Churchill Livingstone; 1985. [Google Scholar]
- 6.Huygen FJA. Family medicine. The medical life history of families. London: RCGP; 1990. [Google Scholar]
- 7.Pemberton J. Will Pickles of Wensleydale. The life of a country doctor. London: RCGP; 1984. [Google Scholar]
- 8.Pickles WN. A rheumatic family. Lancet. 1943;2:241. [Google Scholar]
- 9.Hart JT, Smith GD. Response rates in South Wales 1950-96; changing requirements for mass participation in human research. In: Maynard A, Chalmers I, editors. Non-random reflections on health services research. London: BMJ Publishing Group; 1997. [Google Scholar]
- 10.Miall WE, Oldham PE. The hereditary factor in arterial blood pressure. BMJ. 1963;i:75–80. doi: 10.1136/bmj.1.5323.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watt GCM. The example of Dr Julian Tudor Hart. Br J Gen Pract. 1999;35:503. [Google Scholar]
- 12.Hart JT. Semicontinuous screening of a whole community for hypertension. Lancet. 1970;ii:223–226. doi: 10.1016/s0140-6736(70)92582-1. [DOI] [PubMed] [Google Scholar]
- 13.Watt GCM, Foy CJW. Dietary sodium and arterial pressure: problems of studies within a single population. J Epidemiol Community Health. 1982;36:197–201. doi: 10.1136/jech.36.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watt G. Design and interpretation of studies comparing individuals with and without a family history of high blood pressure. J Hypertens. 1986;4:1–7. doi: 10.1097/00004872-198602000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Watt GCM, Foy CJW, Hart JT. Comparison of blood pressure, sodium intake and other variables in offspring with and without a family history of high blood pressure. Lancet. 1983;i:1245–1248. doi: 10.1016/s0140-6736(83)92697-1. [DOI] [PubMed] [Google Scholar]
- 16.Watt GCM, Foy CJW, Hart JT, et al. Dietary sodium and arterial blood pressure: evidence against genetic susceptibility. BMJ. 1985;291:1525–1528. doi: 10.1136/bmj.291.6508.1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deutscher S, Epstein FH, Kjelsberg MO. Familial aggregation of factors associated with coronary heart disease. Circulation. 1966;33:911–924. doi: 10.1161/01.cir.33.6.911. [DOI] [PubMed] [Google Scholar]
- 18.Cormack JJC. Family portraits — a method of recording family history. J R Coll Gen Pract. 1975;25:520–526. [PMC free article] [PubMed] [Google Scholar]
- 19.MRC Working Party on Mild to Moderate Hypertension. BMJ. Vol. 1. 1977. Randomised controlled trial of treatment for mild hypertension: design and pilot trial; pp. 1437–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harrap SB, Fraser R, Inglis GC, et al. Abnormal epinephrine release in young adults with high personal and high parental blood pressures. Circulation. 1997;96:556–561. doi: 10.1161/01.cir.96.2.556. [DOI] [PubMed] [Google Scholar]
- 21.Harrap SB, Cumming AD, Davies DL, et al. Glomerular hyperfiltration, high renin and low-extracellular volume in high blood pressure. Hypertension. 2000;35:952–957. doi: 10.1161/01.hyp.35.4.952. [DOI] [PubMed] [Google Scholar]
- 22.Noon JP, Walker BR, Webb DJ, et al. Impaired microvascular dilatation and capillary rarefaction in young adults with a predisposition to high blood pressure. J Clin Invest. 1997;99:1873–1879. doi: 10.1172/JCI119354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Watt GCM, Harrap SB, Foy CJW, et al. Abnormalities of glucocorticoid metabolism and the renin–angiotensin system: a four corners approach to the identification of genetic determinants of blood pressure. J Hypertens. 1992;10:473–482. doi: 10.1097/00004872-199205000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Walker BR, Phillips DIW, Noon JP, et al. Increased glucocorticoid activity in men with cardiovascular risk factors. Hypertension. 1998;31:891–895. doi: 10.1161/01.hyp.31.4.891. [DOI] [PubMed] [Google Scholar]
- 25.Bell J. The new genetics in clinical practice. BMJ. 1998;316:618–620. doi: 10.1136/bmj.316.7131.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harrap SB, Watt GCM. Genetics and the risk of coronary heart disease. Med J Aust. 1992;156:594–596. doi: 10.5694/j.1326-5377.1992.tb121451.x. [DOI] [PubMed] [Google Scholar]
- 27.Hawthorne VM, Watt GCM, Hart CL. Cardiorespiratory disease in men and women in urban Scotland. Baseline characteristics of the Renfrew/ Paisley (MIDSPAN) study population. Scot Med J. 1995;40:102–107. doi: 10.1177/003693309504000402. [DOI] [PubMed] [Google Scholar]
- 28.Watt GCM, Hart CL, Hole DJ, et al. Risk factors for cardiorespiratory and all cause mortality in men and women in urban Scotland: 15 year follow up. Scot Med J. 1995;40:108–112. doi: 10.1177/003693309504000403. [DOI] [PubMed] [Google Scholar]
- 29.Hole DJ, Watt GCM, Smith GD, et al. Impaired lung function is the strongest clinical indicator or mortality risk in men and women; findings from the Renfrew/Paisley study. BMJ. 1996;313:711–715. doi: 10.1136/bmj.313.7059.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Upton MN, Smith GD, McConnachie A, et al. Maternal smoking and personal cigarette smoking synergise to increase airflow limitation in adults. Am J Respir Crit Care Med. 2004;169:479–487. doi: 10.1164/rccm.200211-1357OC. [DOI] [PubMed] [Google Scholar]
- 31.Watt G, McConnachie A, Upton M, et al. How acurately do adult sons and daughters report and perceive parental deaths from coronary disease? J Epidemiol Community Health. 2000;54:859–863. doi: 10.1136/jech.54.11.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hunt K, Emslie C, Watt G. Lay constructions of a ‘family history’of heart disease: potential for misunderstandings in the clinical encounter? Lancet. 2001;357:1168–1171. doi: 10.1016/S0140-6736(00)04334-8. [DOI] [PubMed] [Google Scholar]
- 33.McConnachie A, Hunt K, Emslie C, et al. ‘Unwarranted survivals’ and ‘anomalous deaths’ from coronary heart disease: prospective survey of the general population. BMJ. 2001;323:1487–1491. doi: 10.1136/bmj.323.7327.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Academy of Medical Sciences. Strengthening clinical research. London: Academy of Medical Sciences; 2003. http://www.acmed sci.ac.uk/p_scr.pdf (accessed 3 Nov 2004.) [Google Scholar]


