Abstract
Tuberculosis is not just a medical problem, but also a problem of social inequality and poverty
“Everything interacts with everything else: each single factor conspires with the others to crush a man, break him physically and mentally, and lay him wide open to disease.... Pack men together like herring in a barrel, deprive 'em of every last ounce of resistance, batten 'em below decks for days at a time, and what do you get? T.B. It's inevitable.”
This is how the novelist Alistair McLean described life on a British World War II cruiser on convoy duty in the North Atlantic in his novel HMS Ulysses. Compare this picture with the life of a passenger on board a luxury cruiseliner—well fed, enjoying the cruise, pampered by the stewards and being taken care of by the first-class health care on board. These two images pretty much describe the state of the world's population today—the 'haves' and the 'have-nots'. And most humans on this planet clearly belong to the have-nots, which brings us back to tuberculosis (TB). The poor will remain a breeding ground for the 'white plague' until we realize that it is not only the microbe Mycobacterium tuberculosis that is causing the disease, but also the abominable conditions under which hundreds of millions of people on this planet are forced to live.
M. tuberculosis was not a serious threat to humans when they were hunter–gatherers and lived in small groups. As they formed settlements and started growing crops, their population increased, as did contact between groups, and new opportunities for human pathogens emerged. An ancestral mycobacterial species occupied this new niche, and either infected humans first, to become M. tuberculosis, then possibly crossing the species barrier into bovids to evolve into M. bovis, or vice versa. Which of these scenarios accurately reflects history is disputed at present, but what is indisputable is the fact that ∼97% genomic similarity exists between M. tuberculosis and M. bovis. Nowadays, both Mycobacterium species have evolved into serious pathogens and still cross the species barrier. Unlike many human pathogens that appear in epidemic waves lasting only weeks or a few years—two years for measles, four years for influenza—epidemics of TB seem to occur over centuries. Historical evidence includes century-long epidemics in the Nile Valley in about 3000 BC, Greece during 750–500 BC, the Americas during about AD 700–1400 and modern Western Europe during AD 1700–1900 (Daniel, 1999). Unfortunately, we do not know why these epidemic waves eventually faded out, with the exception of the most recent one in Western Europe. Although an epidemic can last for centuries, the peak incidence might be only a few decades long. Thus, we can view the current epidemic of TB as another outbreak that will wane over time. However, the difference between previous epidemics and the current situation is the global extent of the problem, human density, globalization and extensive population movements, all coupled with the HIV epidemic. The incidence of TB might be higher in some locations, but in fact no population today is immune or isolated from risk. It is therefore no surprise that TB is a global emergency, with an estimated one-third of the world's population currently infected and an estimated 3 million deaths each year despite the availability of antibiotics that can cure this affliction.
The poor will remain a breeding ground for the 'white plague' until we realize that it is not only the microbe [...] that is causing the disease...
At least part of the problem lies in our failure to understand this complex disease. The early 'contagion theory' protagonists, including students of Hippocrates and other Greek scholars, were clearly on the right track. But the 'heredity' school, including the Paris Faculty from 1650, was influential as well, citing as evidence the observation that TB
The incidence of TB might be higher in some locations, but in fact no population today is immune or isolated from risk
was frequently familial, that no infectious agent had been identified, that there were different forms of the disease and that the disease can occur long after contact with infected persons. Only after 1882, when Robert Koch conclusively identified the bacterium, did the heredity theorists wane, although there is considerable evidence that host genetics does have a role in susceptibility. Today, we identify the cause of TB to be the bacterium M. tuberculosis, coupled with other factors including genetic susceptibility and the environment, such as HIV infection, stress, overcrowding, nutrition, substance abuse and other causes of immunosuppression. There is little we can do about genetic factors in the context of the population, but much can be learnt from history about how to deal with the bacterium and the environment. This article considers some of these factors and examines how they continue to limit any attempt to control TB in a global context.
Only 1 in 10 infected individuals is likely to progress to an active disease episode over their lifetime in the absence of immunosuppression. This subset of affected persons consists of two major subgroups: those who progress to an active disease episode soon after infection (recent transmission); and those who develop the disease many years or even decades later (reactivation; Lillebaek et al., 2002). Knowing the relative proportions of these two patient groups tells the epidemiologist a lot about the stage of the epidemic in any society: in developed countries with a low incidence of TB, most cases belong to the second group—86% in London, for instance—whereas in high-incidence societies most individuals are in the first group (van Helden, 2002). This information could, or should, influence how we handle the disease. Dealing swiftly and efficiently with active cases as they occur in low-incidence societies, such as Western Europe and the USA, will lead to a decline of the disease or will at least keep it under control at a low level. In high-incidence societies, however, extensive transmission will occur, and in all likelihood, the incidence of TB will increase. This is particularly true in an environment of immunosuppression (HIV), poverty and malnutrition, such as in subsaharan Africa today (Fig. 1). In a situation in which the reproductive rate of the pathogen is less than 1 (R0 < 1), the number of disease cases will remain constant at low levels or will decline. If R0 > 1, the disease caseload will increase. For example, an increase in TB infections of 2.8% a year can lead to a 16-fold increase in initial caseload within a century. An annual increase of 3.5% will lead to a doubling of the caseload after 20 years. These figures may seem unreasonable or unlikely, but there are plenty of examples in which such increases have occurred. In Zimbabwe, the incidence rate increased from about 100 per 100,000 in 1990 to 300 per 100,000 in 1996, which reflects an increase of ∼20% per annum. Under these conditions we can rapidly reach a situation last seen in the newly industrialized world in the eighteenth and nineteenth centuries, when ∼25% of all deaths were due to TB.
...the advent of antibiotics, although making a huge difference to individuals, had relatively little overall impact on the decline of TB in Europe
Figure 1.
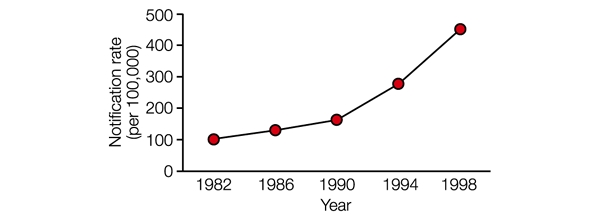
Notification rate for tuberculosis from 1982 to 1998 in sub-Saharan Africa. This is an illustration of the situation in sub-Saharan Africa and is a composite taken from notification rate information from various countries. It therefore does not necessarily reflect an accurate situation for any single country, but approximates that for the region as a whole.
As society changed from predominantly rural to industrialized, crowding and poverty in metropolitan areas increased markedly, creating an environment in which M. tuberculosis was able to flourish. It is estimated that 20% of all deaths in London were due to TB during the late seventeenth century. This situation worsened, peaking in the UK in about 1780, when the incidence rate reached 1,120 per 100,000 a year and 1.25% of the entire population died each year from TB. This alarming state of affairs led to many social changes, and the incidence of TB started to decline in England from the early 1800s, years before other infectious diseases, long before the discovery of M. tuberculosis and a century before the advent of antibiotics. This decline might have been due to an increased resistance in the population, better nutrition and improved housing and working conditions. In about 1870, food production exceeded population growth in Western Europe for the first time and higher wages from the industrial revolution allowed most citizens to purchase sufficient, nutritious food. The latter is a crucial factor, because it is known that a person who is 10% underweight has a threefold increased risk of developing TB after infection. Thus, the advent of antibiotics, although making a huge difference to individuals, had relatively little overall impact on the decline of TB in Europe.
The solutions have, therefore, been staring us in the face all along: alleviation of poverty and improved nutrition. If this is the formula to fight TB, does the converse apply in areas or nations where the disease is in ascendancy? Table 1 shows the differences in income and health expenditure per capita for various countries and regions. Differences in income per capita in the developed world exceed those in the developing world 60-fold, which parallels the more than 60-fold difference in TB incidence rates and the at least 60-fold difference in health expenditure.
Table 1. Health expenditure: a comparison.
| Expenditure | USA | Switzerland | Germany | UK | RSA | Developing countries |
|---|---|---|---|---|---|---|
| Per capita | 4,271 | 3,857 | 2,697 | 1,675 | 230 | 82 |
| % GDP | 12.9 | 10.4 | 10.5 | 6.9 | 7.2 | 5.5 |
| GNI per capita | 34,100 | 38,140 | 25,120 | 24,430 | 3,020 | 1,230 |
Figures are in US $ from 1998. GDP, gross domestic product; GNI, gross national income; RSA, Republic of South Africa.
The causes of these discrepancies are manifold, but they are worth considering: in Africa, for example, the population growth rate during the past few decades was ∼3% a year, whereas the change in gross domestic product (GDP) was less than 1% (Landes, 1999). A harsh climate, regular food shortages, political instability, wars, economic crises and largescale population movements have caused disruption in civil and social services, and this has been exacerbated by a skills drain. In many areas, people are forced to sell vital assets for short-term survival, after which economic recovery may be impossible. In such a severe crisis, the entire structure of society is affected and the availability and distribution of basics, such as food and drugs, is curtailed.
Table 2 shows clearly that millions of individuals are in dire need of assistance, but help is not always given where it is most needed, and what is given is seldom enough. Consequently, it is not surprising that eight out of ten of the countries with the highest rates of TB are not listed in the top ten countries in terms of aid received. In the Democratic Republic of Congo—formerly known as the Belgian Congo and as Zaire—for example, the collapse in civil services can be simply illustrated by the collapse of the infrastructure: in 1960, the country had 140,000 km of useable road, whereas by 1985 this had been reduced to 19,000 km, of which ∼2,000 km were paved. In 1997, rebels captured the diamond-mining areas, and as a consequence, the government was not able to pay its soldiers, which caused widespread unrest and pillaging (Landes, 1999). Under these conditions, poverty alleviation and health care are next to impossible. As stated by David Landes in 1994, “All the ills that have hurt Latin America and the Middle East are exponentially compounded in Subsaharan Africa: bad government, unexpected sovereignty, backward technology, inadequate education, bad climate, incompetent if not dishonest advice, poverty, hunger, disease, overpopulation—a plague of plagues.” Because of these problems, food production lags behind population growth and Africa does not have food security or even self-sufficiency. A large proportion of the population is malnourished, at least partly because bureaucrats make themselves richer at the expense of the population; under such circumstances, farmers give up, or hold back, and too little or the wrong kind of crop is grown. Although the situation in India is quite different in many ways, population growth and poverty nevertheless ensure that India now has the highest caseload of TB patients.
Table 2. Top ten countries that receive humanitarian aid compared with the top ten countries for tuberculosis incidence.
| Humanitarian aid received (2000) | (millions US $) | Tuberculosis incidence (1999) | (rate/100,000) |
|---|---|---|---|
| Serbia/Montenegro | 237 | Zimbabwe | 584 |
| Europe | 178 | Cambodia | 572 |
| Former Yugoslavia | 142 | South Africa | 526 |
| Ethiopia | 102 | Kenya | 484 |
| Mozambique | 95 | Mozambique | 433 |
| East Timor | 92 | Ethiopia | 397 |
| Iraq | 76 | Uganda | 351 |
| Sudan | 52 | Afghanistan | 321 |
| Angola | 48 | Democratic Republic of Congo | 320 |
| Bosnia | 43 | Vietnam | 189 |
Between 1973 and 1993, oil revenues in the oil-producing nations exceeded US $2 trillion (2 × 1012). Despite this income, the incidence of TB in many of these countries is still unacceptably high. Arguably, the income from oil exports has not been put to good use and these countries have sought compensation in religious fundamentalism and military aggression (Huntington, 1998; Diamond, 1998; Landes, 1999). Global regions can be classified into areas of relative peace and those of unrest—where unrest might be military, political or otherwise, such as extreme poverty—and we find that regions of unrest have a very high incidence of TB (Fig. 2).
Figure 2.
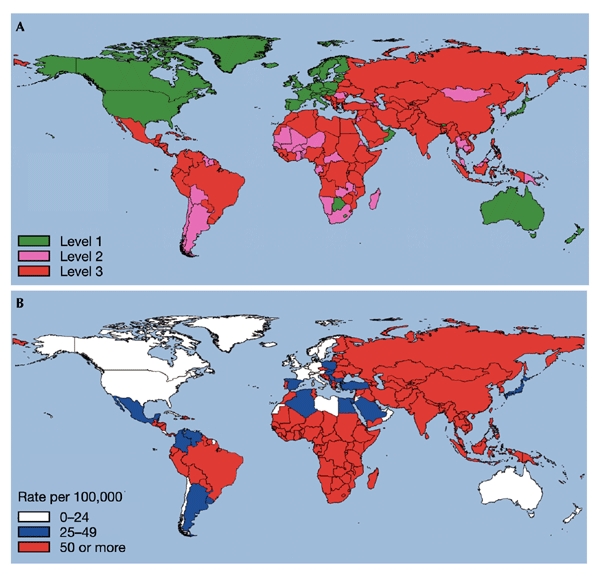
Tuberculosis incidence rates correlate with poor socio-economic conditions. (A) Estimated levels of global unrest, with level 1 indicating minimal or no unrest, level 2 some unrest and level 3 high-level unrest or potential for unrest. Adapted from a map by Albert Jongman, Leiden University. (B) Global tuberculosis incidence rates. Adapted from World Health Organization reports. (www.who.int/gtb).
Part of the solution and explanation also lies in differences in work ethos. In the developed world, the primary assets for income are the export of advanced products and high productivity by skilled workers instead of the sale of raw materials, which is the main income for many developing countries. In terms of economic success, the developed world's 'work culture'—the 'Davos' culture of the G7 countries (from Davos, Switzerland, where the G7 leaders meet regularly)—is extremely important, but it is not adopted by an adequate proportion of the world population to create the economic benefits that will eventually limit the spread of TB. Whether the advanced lifestyle of Europe and North America is globally sustainable in the long term is entirely another matter and quite debatable, however (Bond, 2002).
The real power blocks emerging in the world today are the 'haves' and the 'have-nots'. About two centuries ago, the gap between the richest and poorest nations or regions was between 2:1 and 5:1, whereas the gap now could be as large as 400:1 (Landes, 1999). This has occurred despite—or perhaps because of—increased international trade. Too many developing countries have become dependent on the sale of non-renewable resources, such as oil, gold or minerals, which makes them dependent on and vulnerable to technological developments elsewhere, and to other economic changes beyond their control. Many of these countries would, in fact, have a negative GDP without the sale of these important resources. In this sense, trade does not necessarily promote peace and stability. International trade peaked in 1913, followed by World War I in Europe. Increased trade was noted again in the 1960s and 1970s and was followed by the Cold War. Increased trade can therefore be divisive because of interdependence: if it is not expected to continue or does not continue, conflict can result.
As the gap between the haves and the have-nots becomes larger, a reaction is likely to occur, possibly in the form of conflict or large-scale population movements. Differences in living standards have caused large-scale migrations in previous centuries by Greeks, Jews, Turks, Russians, Chinese and others and, more recently, when about 55 million people migrated from Europe to the USA over a 100-year period starting in the early 1800s. The late twentieth century has seen even larger and more accelerated migrations. In 1990, ∼130 million people were on the move all over the world (Huntington, 1998), following the concentration gradient to perceived economic and political improvement. This often includes the movement of skilled workers—the 'brain drain'—further enhancing the abilities of the wealthy nations at the expense of their poorer neighbours. In South Africa, for example, hundreds of thousands of skilled people have emigrated since the 1980s and the proportion of South Africans below the poverty line increased from 50% to 62% between 1993 and 2001 (Bond, 2002). The official unemployment figure given by the government is about 30%, but it is more likely to be 45% (Bond, 2002). The country's unemployment rate has been the worst of any industrialized nation since about 1 million people—20% of the workforce—lost their formal employment in the 1990s. It is therefore not surprising that the Republic of South Africa now has the third highest incidence rate of TB, according to the World Health Organization.
The lessons from Britain and other industrialized countries from the nineteenth century and the first half of the twentieth century, coupled with an increase in TB even in developed countries starting in the early 1980s, suggests that medical intervention at the individual level alone will not solve the problem (Gandy & Zumla, 2002). Instead, there must be the political will to address the problems of poverty, inadequate health care and inequality. Thus, biomedical research needs to be combined with political, social, economic and cultural research in the search for answers. Specifically, we need to understand and reduce the poverty gap. Although this discourse alone could occupy several
“[Tuberculosis] is always the result of gross defects in social organization and in the management of individual lives. It is truly a social sin which can and must be stamped out”
volumes of any journal, some ideas are already clear. Not every country can or should adopt the lifestyle of the wealthy nations. These countries consume huge amounts of energy with considerable wastage, which is arguably not sustainable in the long-term. Thus, although the topic is perhaps overdone, we need to consider sustainable development and its three pillars, namely ecology, sociology (including factors such as employment and poverty) and economy (including considerations of trade restrictions, natural resources, consumption habits and conflicts). We need to consider simple things such as income tax. There is adequate evidence from many countries that as income tax is reduced unemployment decreases and long-term government revenue increases after an initial lag period. Tax reduction is an excellent method of stimulating the economy and stabilizing government revenue, which in turn is crucial for improving public health. For example, TB increased in Germany after World War I with the rapidly rising inflation at that time, and decreased again when the German economy stabilized. Furthermore, we could consider differential drug pricing, on the basis of per capita income of various countries (Lopert et al., 2002). Thus, a drug price in a poor country, such as Tajikistan, could be one-hundredth of that in a wealthy nation, such as Denmark. In this way, the wealthy can subsidize the poor and help to narrow the gap without prejudicing the interest of drug companies in developing and producing drugs. It is also important to review external aid incentives. For example, external aid funding for TB control was estimated to be US $8 for control activities (per activity) compared with US $137 for malaria and more than US $900 for AIDS (www.who.int). Finally, we should provide major incentives to form partnerships, such as the Global Alliance against Tuberculosis, to encourage companies and countries to control the disease and to embark on new programmes for drug and vaccine development.
Last, it is crucial that biomedical researchers and workers strengthen their interaction with public health services, because each discipline alone will not be able to provide sufficient impetus to control this disease. It is evident that active TB cases need to be diagnosed as fast, as accurately and as sensitively as possible. Research suggests that the current technology is inadequate, and a reliable alternative is urgently needed (Figs 3,4). Furthermore, we need to isolate TB patients as quickly as possible to prevent further transmission. It is no longer feasible or socially acceptable to isolate patients physically in a sanatorium or specialized hospital (Fig. 5), thereby causing stigmatization, but what is urgently needed is the immediate treatment of patients with antibiotics in order to sterilize them with respect to TB, and efficient drugs with minimal side effects. In addition, these drugs should not require a regimen of a minimum of six months, which is the case at present. Finally, we need social studies to help us to change our lifestyle so that we minimize risk and transmission, particularly in those communities where TB is abundant.
...biomedical research needs to be combined with political, social, economic and cultural research in the search for answers
Figure 3.
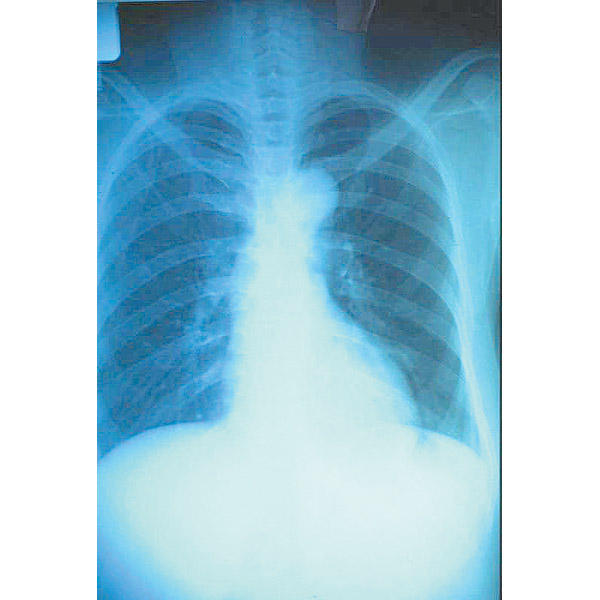
A chest X-ray of a tuberculosis patient. © WHO/TDR/Andy Crump.
Figure 4.
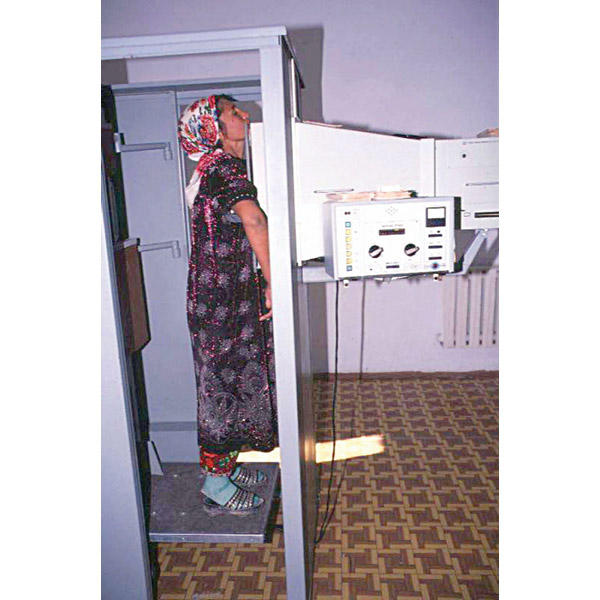
A tuberculosis patient at a hospital in Samarkand, Uzbekistan, undergoing an X-ray of her chest. The woman has been treated several times in the past but is presenting with reinfection. © WHO/TDR/Andy Crump.
Figure 5.
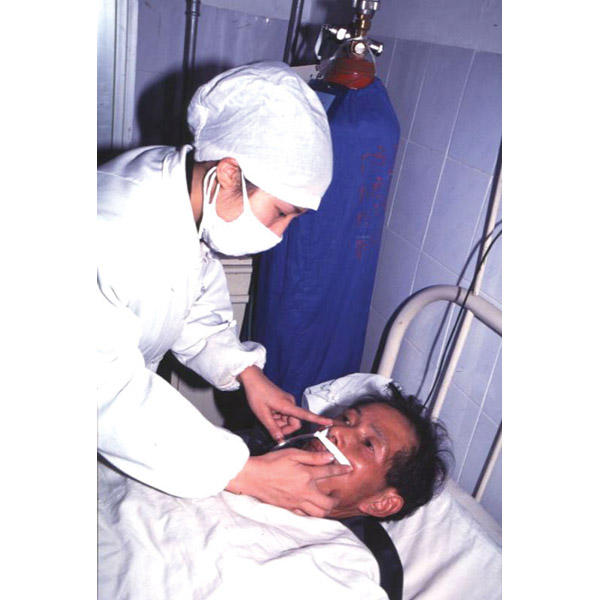
An elderly patient in the tuberculosis ward of a hospital in Changsha, Hunan Province, China, who is having difficulties breathing, receives oxygen through a nasal tube that is being secured by a nurse. © WHO/TDR/Andy Crump.
It is fitting that this is the 50th anniversary of an address given by René Dubos (Dubos & Dubos, 1992), who said, “The anti-TB movement synthesized in one single crusade the efforts of sociologists, humanitarians and hygienists to improve the fate of the destitute by social reforms; to strengthen the human body by advocating a healthy way of life; to control infection by tracking and destroying the tubercle cell.” What was said then is just as true today. Dubos went on to say that “magic bullets are not the most effective way to deal with pathogens” but that “the real keys came from ecology, human behaviour and a recognition that microbial and human populations are part of the same evolving biosphere.... Thus it is certain that TB is not an inescapable component of human society. It is always the result of gross defects in social organization and in the management of individual lives. It is truly a social sin which can and must be stamped out.” We now know that more than 50% of South Africans currently live below the poverty line defined by the United Nations and that hundreds of millions of people worldwide share their situation. However, it is also true that the worse the situation is, the better is the potential for improvement. In Mozambique and Uganda, for example, where previous conflicts and social unrest drastically curtailed economic activity, economic growth rates now exceed 5% per year. Clearly, it will be difficult to sustain very high growth rates indefinitely, but it is possible that these could be maintained for some years and exceed growth rates seen in Europe and the USA. As the basic requirements for controlling TB are the well-being of the population, good economics, the availability of antibiotics, effective diagnosis, a stable infrastructure and multidisciplinary health-care professionals, there must be stability first, followed by commitment from governments to provide better health care.

Acknowledgments
I thank R. Warren for a critical reading of this essay, and M. de Klerk for assistance with the maps. Funding for research was provided by GlaxoSmithKline, the Wellcome Trust and the Sequella Foundation.
References
- Bond P. (2002) Unsustainable South Africa. University of Natal Press, Scottsville, South Africa. [Google Scholar]
- Daniel T.M. (1999) Captain of Death: The Story of Tuberculosis. Boydell & Brewer, Rochester, New York, USA. [Google Scholar]
- Diamond J. (1998) Guns, Germs and Steel. Vintage, London. [Google Scholar]
- Dubos R. & Dubos J. (1992) The White Plague 2nd edn. Ruttgers University Press, New Brunswick, New Jersey, USA. [Google Scholar]
- Gandy M. & Zumla A. (2002) The resurgence of disease: social and historical perspectives on the 'new' tuberculosis. Soc. Sci. Med., 55, 385–396. [DOI] [PubMed] [Google Scholar]
- Huntington S.P. (1998) The Clash of Civilizations and the Remaking of World Order. Simon & Schuster, London, UK. [Google Scholar]
- Landes D.S. (1999) The Wealth and Poverty of Nations. Abacus, London. [Google Scholar]
- Lillebaek T. et al. (2002) Molecular evidence of endogenous reactivation of Mycobacterium tuberculosis after 33 years of latent infection. J. Infect. Dis., 185, 401–404. [DOI] [PubMed] [Google Scholar]
- Lopert R., Lang D.L., Hill S.R. & Henry D.A. (2002) Differential pricing of drugs: a role for cost-effective analysis? Lancet, 359, 2105–2107. [DOI] [PubMed] [Google Scholar]
- van Helden P.D. (2002) Molecular epidemiology of TB: challenging dogmas and asking new questions. IUBMB Life, 53, 219–223. [DOI] [PubMed] [Google Scholar]


