Abstract
The time-kill effect of moxifloxacin on 20 genetically distinct isolates of Stenotrophomonas maltophilia resistant to trimethoprim-sulfamethoxazole was studied. The majority (80%) were killed by a concentration equivalent to four times the MIC; the MIC induced a transient decrease in bacterial counts at 4 h, followed by regrowth. No effect was detected in four isolates. These results merit further clinical consideration.
Stenotrophomonas maltophilia is a pathogen affecting immunocompromised and debilitated patients (4). Trimethoprim-sulfamethoxazole is considered the treatment of choice (2), but resistant isolates emerge (8). Although newer fluoroquinolones have been shown to possess a considerable in vitro inhibitory effect on that species (3, 10), studies involved only isolates susceptible to co-trimoxazole. The present study focused on the in vitro killing effect of moxifloxacin on genetically distinct isolates of S. maltophilia resistant to co-trimoxazole.
Twenty diverse clinical isolates of S. maltophilia were used, with the following selection criteria: (i) isolation from seven different hospitals in the Athens region and from different patients with nosocomial infections, (ii) genetic diversity as defined by pulsed-field gel electrophoresis (PFGE) of their DNA, and (iii) multidrug resistance to trimethoprim-sulfamethoxazole, ciprofloxacin, and amikacin. The biological specimens from which they were isolated and the numbers of isolates obtained were as follows: sputum, 8; urine, 8; pus, 2; blood, 2. In two specimens, S. maltophilia was a copathogen, with Pseudomonas aeruginosa in one and with Klebsiella pneumoniae in the other. Identification of isolates was done by the API 20E system (bioMérieux, Marcy l' Etoile, France).
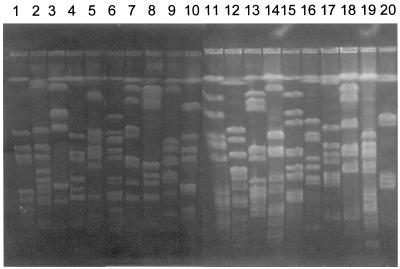
For PFGE, agarose plugs containing high-molecular-weight DNA were prepared as already described (1). DNA was digested with 30 U of SpeI restriction endonuclease (New England BioLabs, Göttingen, Germany), and electrophoresis was performed with 1% agarose gels with a Gene-Navigator system (Pharmacia, Uppsala, Sweden) for 20 h at 10°C with 5- to 50-s linear ramping at 6 V/cm.
Resistance to trimethoprim-sulfamethoxazole, ciprofloxacin, and amikacin was assessed after determination of MICs by a microdilution technique on commercially available plates (Becton Dickinson, Cockeysville, Md.) in a final volume of 0.1 ml with an overnight inoculum of 5 × 105 CFU/ml. MICs of moxifloxacin (Bayer, Leverkusen, Germany) were determined on freshly prepared plates. All determinations were performed in duplicate, and the MIC was considered the lowest antimicrobial concentration inhibiting visible bacterial growth after 18 h of incubation at 35°C.
An overnight inoculum of 106 CFU of each isolate per ml was exposed to moxifloxacin at concentrations equal to one and four times the MIC and to 2 and 38 μg, respectively, of trimethoprim-sulfamethoxazole per ml, i.e., the susceptibility breakpoint. One growth control was used per isolate tested. Exposure was performed in tubes of a 10-ml final volume in Mueller-Hinton broth. All tubes were incubated at 37°C in a shaking water bath to achieve optimal bacterial growth conditions. Bacterial growth was determined before and after 2, 4, 6, and 24 h of incubation by diluting an aliquot of 0.1 ml five times serially 1:10 in sterile water. A 0.1-ml aliquot of each dilution was plated onto MacConkey agar (Becton Dickinson). This method limited any probable antibiotic carryover effect and presented a lower detection limit of 10 CFU/ml. Each determination was performed twice.
Log10 changes in viable cell counts at any time of growth from the baseline were expressed as the mean ± the standard deviation. Comparisons were performed by analysis of variance. A killing effect was defined as any decrease of greater than 3 log10 from the beginning of the experiment (5). Comparisons of the killing effects of the drug concentrations used were performed by Fisher' s exact test. P values of ≤0.05 were considered significant.
DNA electrophoresis of the isolates tested is shown in Fig. 1. The MICs of moxifloxacin for 50 and 90% of the isolates tested (MIC50 and MIC90, respectively) were 2 and 4 μg/ml, respectively. At 2 μg/ml (9), moxifloxacin inhibited 13 isolates (65%). The time-kill effect of moxifloxacin is shown in Table 1. The mean log10 changes in viable cell counts caused by trimethoprim-sulfamethoxazole were +0.17, +0.28, +0.51, and +0.79 after 2, 4, 6, and 24 h of growth, respectively.
FIG. 1.
PFGE of the 20 isolates of S. maltophilia tested in this study.
TABLE 1.
Effects of the MIC of moxifloxacin and a concentration equal to four times the MIC on viable counts of 20 S. maltophilia multidrug-resistant nosocomial isolates
| Isolate | MIC (μg/ml) | Concn testeda | Individual or mean ± SD log10 change in viable cell count (CFU/ml) at indicated time of growth
|
|||
|---|---|---|---|---|---|---|
| 2 h | 4 h | 6 h | 24 h | |||
| 1 | 0.25 | 1 × MIC | −0.40 | −0.22 | −0.15 | +1.90 |
| 4 × MIC | −0.40 | −1.30 | −1.52 | −0.15 | ||
| 2 | 0.03 | 1 × MIC | −0.20 | −0.60 | −1.00 | +0.57 |
| 4 × MIC | −0.88 | −0.30 | −3.78 | −4.30 | ||
| 3 | 4 | 1 × MIC | 0.00 | −0.52 | −2.00 | −1.40 |
| 4 × MIC | −2.11 | −2.78 | −5.00 | −5.00 | ||
| 4 | 1 | 1 × MIC | −0.60 | −1.43 | −1.82 | +0.10 |
| 4 × MIC | −1.82 | −4.18 | −5.00 | −4.18 | ||
| 5 | 4 | 1 × MIC | −2.12 | −2.70 | −3.76 | −2.12 |
| 4 × MIC | −3.30 | −4.90 | −6.90 | −6.30 | ||
| 6 | 4 | 1 × MIC | −0.15 | −3.00 | −3.00 | −2.70 |
| 4 × MIC | −4.20 | −6.20 | −6.20 | −6.20 | ||
| 7 | 0.5 | 1 × MIC | −0.54 | −0.89 | −2.94 | 0.00 |
| 4 × MIC | −2.90 | −5.00 | −5.00 | −2.90 | ||
| 8 | 4 | 1 × MIC | −2.10 | −5.00 | −5.00 | −2.22 |
| 4 × MIC | −5.00 | −5.00 | −5.00 | −5.00 | ||
| 9 | 2 | 1 × MIC | −0.10 | −3.00 | −2.52 | −1.15 |
| 4 × MIC | −5.00 | −5.00 | −5.00 | −5.00 | ||
| 10 | 4 | 1 × MIC | −1.00 | −2.40 | −3.00 | −3.84 |
| 4 × MIC | −5.00 | −5.00 | −5.00 | −5.00 | ||
| 11 | 4 | 1 × MIC | −3.00 | −2.70 | −3.22 | −3.22 |
| 4 × MIC | −5.00 | −5.00 | −5.00 | −5.00 | ||
| 12 | 2 | 1 × MIC | −2.90 | −4.90 | −5.00 | −1.60 |
| 4 × MIC | −5.00 | −5.00 | −5.00 | −5.00 | ||
| 13 | 1 | 1 × MIC | −0.48 | −0.88 | −2.00 | +1.43 |
| 4 × MIC | −1.00 | −2.30 | −4.30 | −1.60 | ||
| 14 | 4 | 1 × MIC | −0.73 | −2.90 | −3.30 | 0.00 |
| 4 × MIC | −4.90 | −4.90 | −4.90 | −3.90 | ||
| 15 | 0.25 | 1 × MIC | −1.00 | −1.22 | −2.10 | 0.00 |
| 4 × MIC | −4.00 | −4.10 | −5.00 | −2.00 | ||
| 16 | 2 | 1 × MIC | −0.30 | −0.43 | −0.60 | +0.57 |
| 4 × MIC | −2.06 | −2.06 | −2.43 | +1.10 | ||
| 17 | 2 | 1 × MIC | −2.60 | −4.78 | −5.00 | −2.76 |
| 4 × MIC | −5.00 | −5.00 | −5.00 | −5.00 | ||
| 18 | 0.25 | 1 × MIC | +1.00 | +1.00 | +1.00 | +1.00 |
| 4 × MIC | −1.00 | −1.00 | −1.52 | −2.30 | ||
| 19 | 0.5 | 1 × MIC | −0.12 | −1.12 | −2.30 | +1.40 |
| 4 × MIC | −0.70 | −3.60 | −5.00 | +0.90 | ||
| 20 | 0.06 | 1 × MIC | +0.30 | 0.00 | +0.85 | +2.00 |
| 4 × MIC | −0.12 | −0.06 | −0.06 | +2.00 | ||
| 1-20 | 1 × MIC | −0.86 ± 1.11 | −1.89 ± 1.71 | −2.39 ± 1.82 | −0.73 ± 2.11 | |
| 4 × MIC | −3.45 ± 2.49b | −4.22 ± 2.41c | −4.83 ± 2.17d | −3.78 ± 2.99e | ||
Moxifloxacin was used at the MIC (1 × MIC) and at a concentration equivalent to four times the MIC (4 × MIC).
P = 0.001.
P = 0.029.
P = 0.002.
P = 0.004.
Isolates 2, 3, and 4 were not significantly affected by the MIC, but they were killed after 2 to 4 h by a concentration equivalent to four times the MIC. A ≥3-log10 decrease in viable counts was achieved by the MIC after 4 to 6 h for isolates 5, 6, 8, 9, 10, 11, and 12, but regrowth was found at 24 h; all isolates were killed after 2 h by a concentration equivalent to four times the MIC. Isolates 7, 15, and 19 were not affected by the MIC, but ≥3-log10 decreases in viable counts were caused after 4 h by a concentration equivalent to four times the MIC and were followed by regrowth at 24 h. Finally, isolates 1, 16, 18, and 20 remained completely indifferent to the effect of either of the concentrations tested.
The present study revealed a considerable time-kill effect of moxifloxacin on genetically distinct isolates of S. maltophilia resistant to trimethoprim-sulfamethoxazole. That effect involved 80% of the isolates tested, being most prominent when the concentration used was four times the MIC (Table 2). Bacterial killing by a concentration equivalent to four times the MIC was observed mainly over the first 2 or 4 h of exposure. The effect of the MIC was transient, and it was accompanied by bacterial regrowth after 24 h, whereas bacterial regrowth was observed in only three isolates exposed to a concentration equivalent to four times the MIC. In the majority of isolates, a concentration of moxifloxacin equivalent to four times the MIC prevented regrowth. Four isolates remained indifferent to the effect of moxifloxacin.
TABLE 2.
Killing effect of moxifloxacin at one and four times the MIC on 20 multidrug-resistant nosocomial isolates of S. maltophilia
| Drug concna | No. (%) of isolates killed at indicated time of growth
|
|||
|---|---|---|---|---|
| 2 h | 4 h | 6 h | 24 h | |
| 1 × MIC | 1 (5) | 5 (25) | 8 (40) | 2 (10) |
| 4 × MIC | 10 (50)b | 12 (60)c | 16 (80)d | 12 (60)b |
Moxifloxacin was used at the MIC (1 × MIC) and at a concentration equivalent to four times the MIC (4 × MIC).
P = 0.002
No significant difference between the drug concentrations tested.
P = 0.022.
Concentrations of moxifloxacin in serum rarely exceed 4 μg/ml after oral administration of a single 400-mg dose, but they are 31% higher after intravenous administration of a single 400-mg dose (7). These pharmacokinetic data, in correlation with the MICs for the isolates tested (Tables 1 and 2), render the reported results of clinical significance. However, for respiratory tract infections with strains for which the MIC is >2 μg/ml, the clinical relevance is limited because of accumulation of moxifloxacin in the bronchial epithelial lining fluid and in the alveolar macrophages (6). In the latter case, monotherapy with moxifloxacin might select for resistant mutants.
The growth of all of the isolates tested was not similarly affected after exposure to moxifloxacin. One probable explanation for this might be the underlying mechanism of resistance. Multidrug resistance of S. maltophilia is often attributed to the existence of the SmeDEF efflux pump in the outer membrane (11). Isolates for which the MIC of moxifloxacin is >2 μg/ml may carry that pump (12).
The results presented here reveal that moxifloxacin possesses a considerable time-kill effect on multidrug-resistant S. maltophilia that makes it suitable for use as a therapeutic alternative for infections by that species. These results merit further study in both the animal model and the clinical setting.
REFERENCES
- 1.Berg, G., N. Roskot, and K. Smalla. 1999. Genotypic and phenotypic relationships between clinical and environmental isolates of Stenotrophomonas maltophilia. Antimicrob. Agents Chemother. 37:3594-3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Betriu, C., A. Sánchez, L. Palau, M. Gǒmez, and J. J. Picazo. 2001. Antibiotic resistance surveillance of Stenotrophomonas maltophilia, 1993-1999. J. Antimicrob. Chemother. 48:152-154. [DOI] [PubMed] [Google Scholar]
- 3.Biedenbach, D. J., M. A. T. Croco, T. J. Barrett, and R. N. Jones. 1999. Comparative in vitro activity of gatifloxacin against Stenotrophomonas maltophilia and Burkholderia species isolates including evaluation of disk diffusion and E test methods. Eur. J. Clin. Microbiol. Infect. Dis. 18:428-431. [DOI] [PubMed] [Google Scholar]
- 4.Gales, A. C., R. N. Jones, K. R. Forward, J. Liòares, H. S. Sader, and J. Verhoef. 2001. Emerging importance of multidrug-resistant Acinetobacter species and Stenotrophomonas maltophilia as pathogens in seriously ill patients: geographic patterns, epidemiological features, and trends in the SENTRY antimicrobial surveillance program (1977-1999). Clin. Infect. Dis. 32(Suppl. 2):104-113. [DOI] [PubMed] [Google Scholar]
- 5.Hindler, J. 1992. Tests to assess bactericidal activity, p. 5.16.14-5.16.24. In H. D. Eisenberg (ed.), Clinical microbiology procedures handbook. American Society for Microbiology, Washington, D.C.
- 6.Soman, A., D. Honeybourne, J. Andrews, G. Jevons, and R. Wise. 1999. Concentrations of moxifloxacin in serum and pulmonary compartments following a single 400 mg oral dose in patients undergoing fibre-optic bronchoscopy. J. Antimicrob. Chemother. 44:835-838. [DOI] [PubMed] [Google Scholar]
- 7.Stass, H., and D. Kubitza. 1999. Pharmacokinetics and elimination of moxifloxacin after oral and intravenous administration in man. J. Antimicrob. Chemother. 43(Suppl. B):83-90. [DOI] [PubMed] [Google Scholar]
- 8.Tsiodras, S., D. Pittet, Y. Carmeli, G. Eliopoulos, H. Boucher, and S. Harbarth. 2000. Clinical implications of Stenotrophomonas maltophilia resistant to trimethoprim-sulfamethoxazole: a study of 69 patients at 2 university hospitals. Scand. J. Infect. Dis. 32:651-656. [DOI] [PubMed] [Google Scholar]
- 9.Valdezate, S., A. Vindel, E. Loza, F. Baquero, and R. Cantõn. 2001. Antimicrobial susceptibilities of unique Stenotrophomonas maltophilia clinical isolates. Antimicrob. Agents Chemother. 45:1581-1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiss, K., C. Restieri, E. De Carolis, M. Laverdière, and H. Guay. 2000. Comparative activity of new quinolones against 326 clinical isolates of Stenotrophomonas maltophilia. J. Antimicrob. Chemother. 45:363-365. [DOI] [PubMed] [Google Scholar]
- 11.Zhang, L., X. Z. Li, and K. Poole. 2001. SmeDEF multidrug efflux pump contributes to intrinsic multidrug resistance in Stenotrophomonas maltophilia. Antimicrob. Agents Chemother. 45:3497-3503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang, L., X. Z. Li, and K. Poole. 2001. Fluoroquinolone susceptibilities of efflux-mediated multidrug-resistant Pseudomonas aeruginosa, Stenotrophomonas maltophilia and Burkholderia cepacia. J. Antimicrob. Chemother. 48:549-552. [DOI] [PubMed] [Google Scholar]