An 82-year-old man with a history of hypertension and prostatectomy for benign hypertrophy was admitted with left flank pain of sudden onset. He had no bowel or bladder symptoms, and findings on physical examination were normal. Results of laboratory tests revealed the following elevated values: erythrocyte sedimentation rate 32 (normal < 20) mm/h, C-reactive protein level 124 (normal < 6) mg/dL, leukocyte count 18.8 (normal 5–10) х 109/L, serum calcium level 2.72 (normal < 2.58) mmol/L, and γ-glutamyl transferase (GGT) level 77 (normal < 50) U/L. His serum albumin level, renal function, other liver function test results and chest radiograph were normal.
Prolonged fever (> 38.3°C), lassitude, anorexia and weight loss (> 10% of body weight) developed over the following 4 weeks, with neither localizing symptoms nor abnormal findings on examination. A leukemoid reaction developed: the patient's leukocyte count was 64.3 х 109/L, with a marked left shift and mild monocytosis (neutrophils 67%, bands 18%, lymphocytes 2%, monocytes 13%), but otherwise the blood smear was normal. His alkaline phosphatase level rose to 525 (normal < 126) IU/L and GGT level to 620 U/L, with normal bilirubin and aminotransferase levels. His serum calcium level increased to 3.29 mmol/L, with normal levels of serum parathyroid hormone, angiotensin-converting enzyme and vitamin D; the hypercalcemia responded to hydration and 60 mg of pamidronate.
Blood and urine cultures and lumbar puncture results were negative. Echocardiography, to rule out endocarditis, revealed normal findings. A tuberculin skin test was positive at 20 mm. Abdominal ultrasonography and CT scanning revealed multiple hypodense lesions up to 1.5 cm in size in the spleen and liver (Fig. 1). Osteolytic lesions in a few thoracic vertebrae were consistent with bone metastases or granulomatous disease, but bone marrow biopsy was inconclusive. A chest CT scan showed emphysema but no acute disease or enlarged lymph nodes. Liver biopsy showed fatty liver and nonspecific granulomas and stained negative for acid-fast bacteria. With a differential diagnosis of splenic lymphoma or disseminated tuberculosis, 4 antituberculous drugs were prescribed, but with no effect. Thrombocytopenia developed, which prevented guided splenic biopsy or splenectomy.1 The patient died 5 weeks after admission.

Fig. 1: CT scan showing hypodense lesions in spleen and liver.
The spleen and liver showed multiple well-demarcated nodules at autopsy consisting of grey hemorrhagic tissue with areas of necrosis. Histologic examination revealed irregular vascular spaces lined by atypical pleomorphic endothelial cells showing a focal papillary pattern of proliferation as well as widespread necrotic areas and hemorrhages (Fig. 2). These findings were consistent with primary angiosarcoma of the spleen.
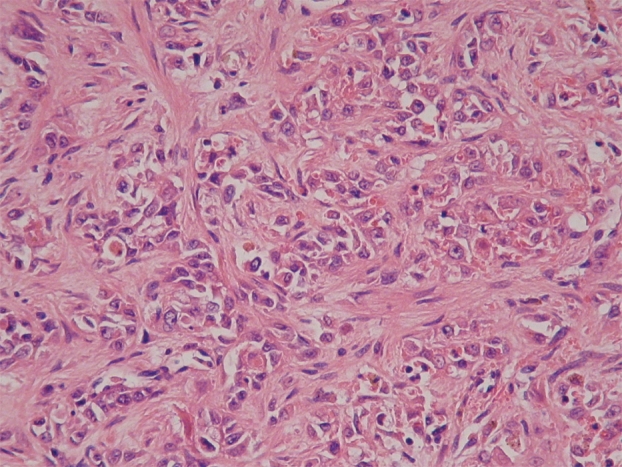
Fig. 2: Spleen tissue, showing irregular vascular spaces lined by atypical pleomorphic endothelial cells and widespread areas of necrosis and hemorrhage.
Primary angiosarcoma of the spleen is a highly aggressive malignant disease with a median survival of 5 months irrespective of treatment. It arises from the endothelial lining of the splenic blood vessels, and hence the malignant cells express both endothelial (e.g., CD34 and CD31) and histiocytic (e.g., CD68 and lysozyme) markers.2 Men and women are affected equally, and the disease usually occurs in people over age 60 years. Common presenting symptoms include upper abdominal pain (in 66% of cases), fever, anorexia and weight loss. Splenomegaly is the most common finding (in 75%), and splenic rupture can occur. As in the case we describe, imaging is characteristic, showing masses in an enlarged spleen.3 Metastatic spread is common to the liver (in 60%), causing cholestatic disease, and to the spine (in 20%), causing hypercalcemia.2,3 Other laboratory abnormalities include a leukemoid reaction, possibly related to the production of granulocyte colony-stimulating factor by the tumour cells. Diagnosis can be confirmed by liver biopsy, but a “sampling error” may occur, as happened in our case. There are no current therapies of benefit, and treatment remains palliative.
Ami Schattner Alon Bassevitch Department of Medicine Judith Diment Department of Pathology Kaplan Medical Centre Rehovot, Israel Hebrew University Hadassah Medical School Jerusalem, Israel
REFERENCES
- 1.Kraus MD, Fleming MD, Vonderheide RH. The spleen as a diagnostic specimen: a review of 10 years' experience at two tertiary care institutions. Cancer 2001;91:2001-9. [DOI] [PubMed]
- 2.Neuhauser TS, Derringer GA, Lester DR, et al. Splenic angiosarcoma: a clinicopathologic and immunophenotypic study of 28 cases. Mod Pathol 2000;13:978-87. [DOI] [PubMed]
- 3.Thompson WM, Levy AD, Aguilera NS, et al. Angiosarcoma of the spleen: imaging characteristics in 12 patients. Radiology 2005;235:106-15. [DOI] [PubMed]


