Abstract
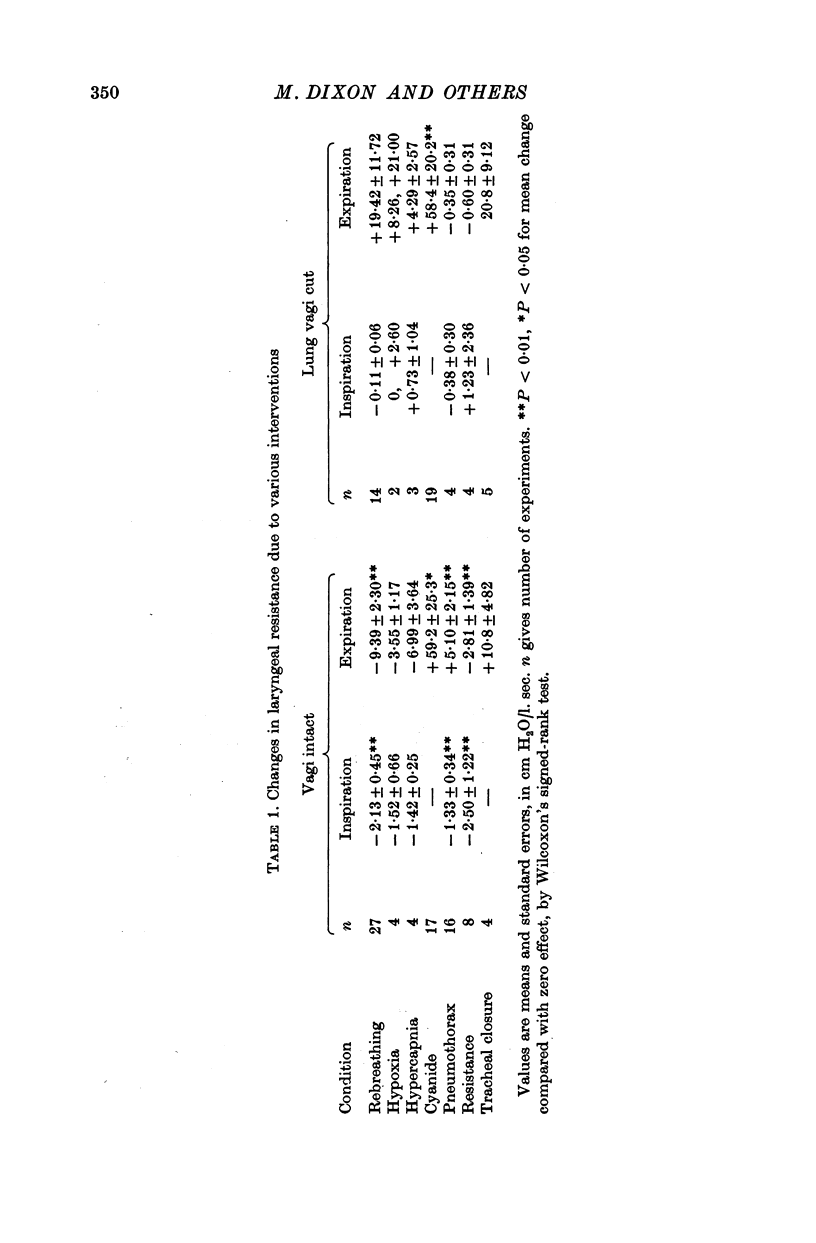
1. The effects of asphyxia, hypoxia, hypercapnia, stimulation of peripheral chemoreceptors, pneumothorax and breathing through resistances have been investigated on laryngeal resistance to airflow in anaesthetized cats, with and without bilateral vagotomy below the origin of the recurrent laryngeal nerves.
2. Resistance to airflow of the innervated larynx was usually measured with the larynx isolated in situ with constant flow from the trachea to a pharyngeal opening, and expressed by the relationship between translaryngeal pressure and airflow.
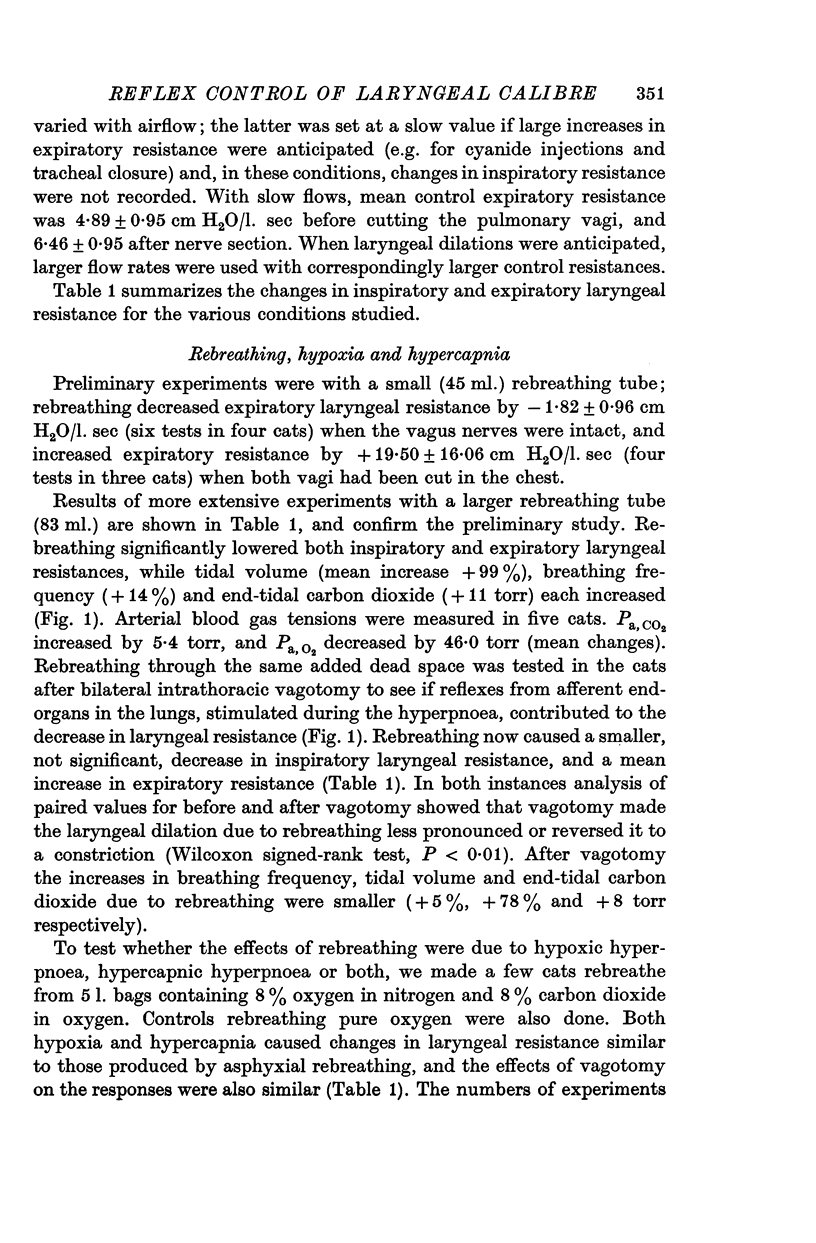
3. Asphyxia, hypoxia and hypercapnia each stimulated breathing and decreased laryngeal resistance to airflow, in both the inspiratory and expiratory phases. After vagotomy the effect was reduced, abolished or (usually) reversed to a laryngeal constriction, especially in expiration.
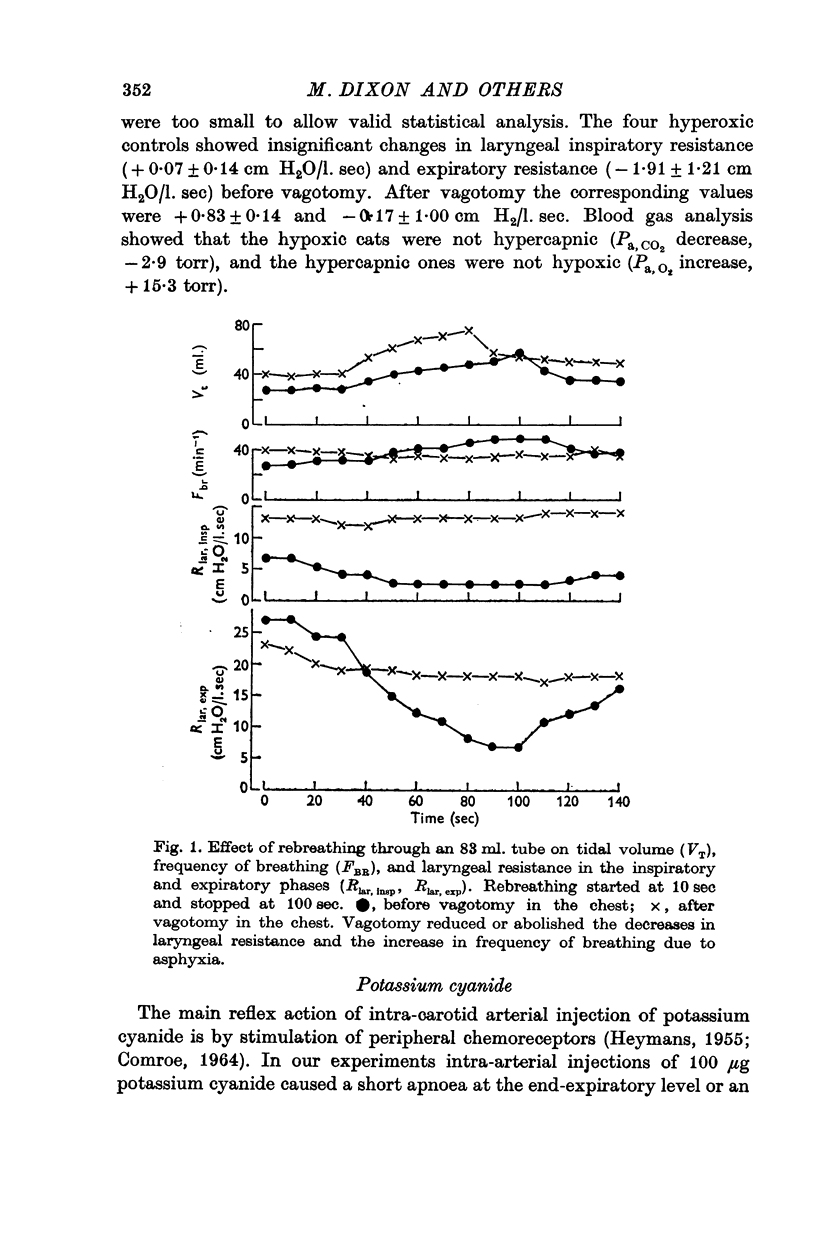
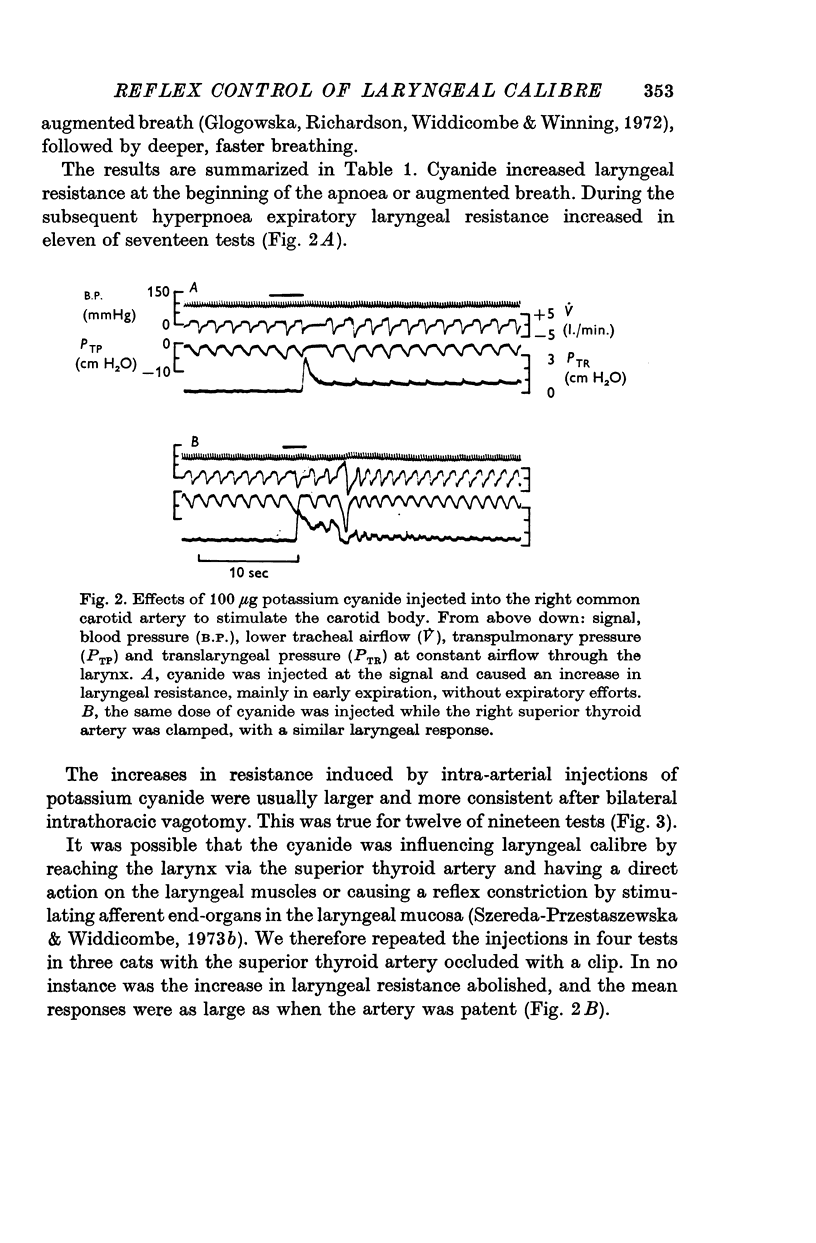
4. Intra-arterial injections of potassium cyanide (to stimulate carotid body chemoreceptors) caused a short apnoea or an augmented breath followed by hyperpnoea, concurrently with expiratory constrictions of the larynx. The responses were usually stronger after bilateral vagotomy.
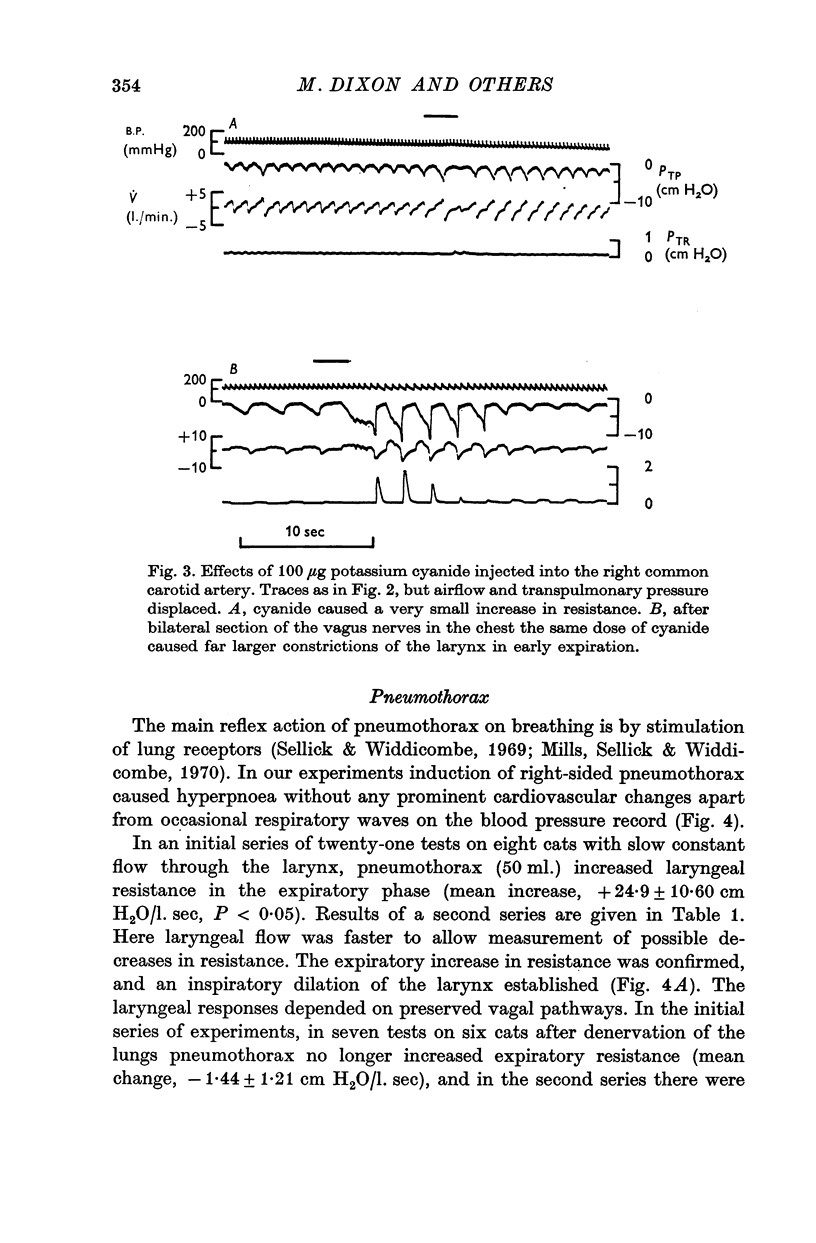
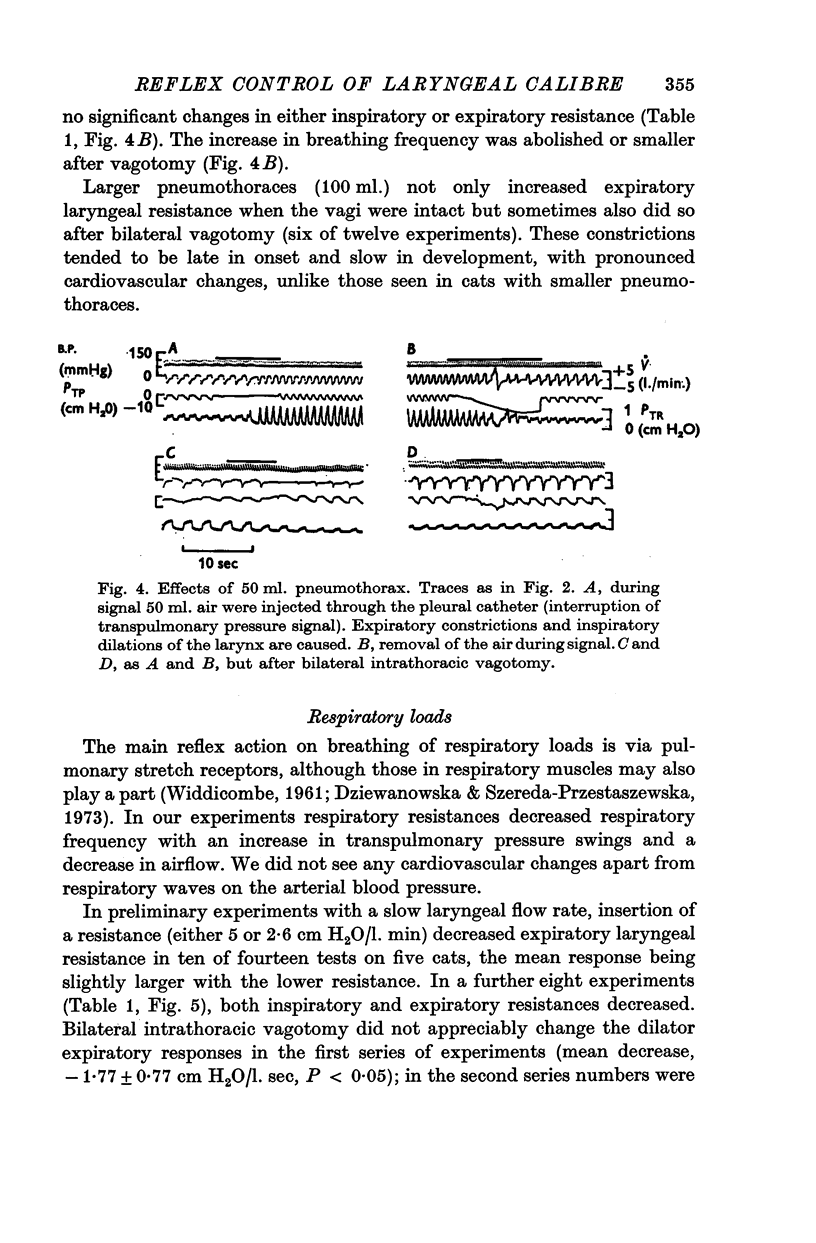
5. Pneumothorax caused tachypnoea, inspiratory dilatations and expiratory constrictions of the larynx. The responses were abolished by vagotomy.
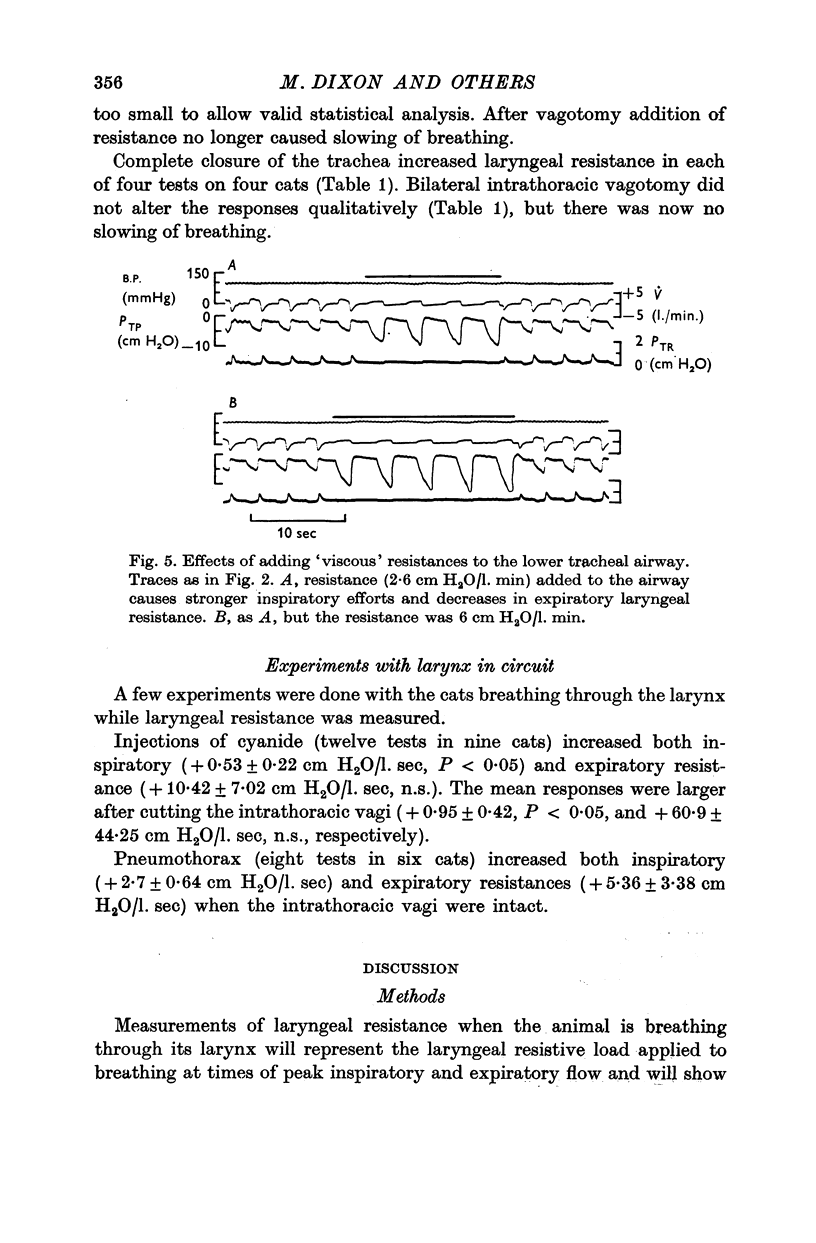
6. Imposition of respiratory resistances dilated the larynx, in inspiration and expiration, while complete closure of trachea caused expiratory constrictions of the larynx. These changes did not depend on intact vagal pathways.
7. The results are discussed in terms of nervous control of the larynx in the different conditions.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BLIDE R. W., KERR H. D., SPICER W. S., Jr MEASUREMENT OF UPPER AND LOWER AIRWAY RESISTANCE AND CONDUCTANCE IN MAN. J Appl Physiol. 1964 Nov;19:1059–1069. doi: 10.1152/jappl.1964.19.6.1059. [DOI] [PubMed] [Google Scholar]
- BORISON H. L., BRODIE D. A. Analysis of central control of respiration by the use of cyanide. J Pharmacol Exp Ther. 1956 Oct;118(2):220–229. [PubMed] [Google Scholar]
- Bartlett D., Jr, Remmers J. E., Gautier H. Laryngeal regulation of respiratory airflow. Respir Physiol. 1973 Jul;18(2):194–204. doi: 10.1016/0034-5687(73)90050-9. [DOI] [PubMed] [Google Scholar]
- COMROE J. H., Jr, MORTIMER L. THE RESPIRATORY AND CARDIOVASCULAR RESPONSES OF TEMPORALLY SEPARATED AORTIC AND CAROTID BODIES TO CYANIDE, NICOTINE, PHENYLDIGUANIDE AND SEROTONIN. J Pharmacol Exp Ther. 1964 Oct;146:33–41. [PubMed] [Google Scholar]
- Dziewanowska Z., Szereda-Przestaszewska M. Studies on extravagal control of respiration. Acta Physiol Pol. 1973;24(3):377–392. [PubMed] [Google Scholar]
- Eterradossi J., Benchetrit G., Idelman J., Poupot C., Lemarchands H. Sommation de chémo-reflexes ventilatoires par stimulation carotidienne par NaCN. J Physiol (Paris) 1967;59(4 Suppl):404–404. [PubMed] [Google Scholar]
- Fukuda H., Kirchner J. A. Changes in the respiratory activity of the cricothyroid muscle with intrathoracic interruption of the vagus nerve. Ann Otol Rhinol Laryngol. 1972 Aug;81(4):532–537. doi: 10.1177/000348947208100412. [DOI] [PubMed] [Google Scholar]
- Fukuda H., Sasaki C. T., Kirchner J. A. Vagal afferent influences on the phasic activity of the posterior cricoarytenoid muscle. Acta Otolaryngol. 1973 Feb-Mar;75(2):112–118. doi: 10.3109/00016487309139684. [DOI] [PubMed] [Google Scholar]
- GREEN J. H., NEIL E. The respiratory function of the laryngeal muscles. J Physiol. 1955 Jul 28;129(1):134–141. doi: 10.1113/jphysiol.1955.sp005342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautier H., Remmers J. E., Bartlett D., Jr Control of the duration of expiration. Respir Physiol. 1973 Jul;18(2):205–221. doi: 10.1016/0034-5687(73)90051-0. [DOI] [PubMed] [Google Scholar]
- Glogowska M., Richardson P. S., Widdicombe J. G., Winning A. J. The role of the vagus nerves, peripheral chemoreceptors and other afferent pathways in the genesis of augmented breaths in cats and rabbits. Respir Physiol. 1972 Oct;16(2):179–196. doi: 10.1016/0034-5687(72)90050-3. [DOI] [PubMed] [Google Scholar]
- HEMINGWAY A., SIMMONS D. H. Respiratory response to acute progressive pneumothorax. J Appl Physiol. 1958 Sep;13(2):165–170. doi: 10.1152/jappl.1958.13.2.165. [DOI] [PubMed] [Google Scholar]
- HEYMANS C. Action of drugs on carotid body and sinus. Pharmacol Rev. 1955 Mar;7(1):119–142. [PubMed] [Google Scholar]
- HYATT R. E., WILCOX R. E. The pressure-flow relationships of the intrathoracic airway in man. J Clin Invest. 1963 Jan;42:29–39. doi: 10.1172/JCI104693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neil E., O'Regan R. G. Efferent and afferent impulse activity recorded from few-fibre preparations of otherwise intact sinus and aortic nerves. J Physiol. 1971 May;215(1):33–47. doi: 10.1113/jphysiol.1971.sp009456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nye R. E., Jr Influence of the cyclical pattern of ventilatory flow on pulmonary gas exchange. Respir Physiol. 1970 Oct;10(3):321–337. doi: 10.1016/0034-5687(70)90052-6. [DOI] [PubMed] [Google Scholar]
- Peslin R., Hixon T., Mead J. Variations des résistances thoraco-pulmonaires au cours du cycle ventilatoire étudiées par méthode d'oscillation. Bull Physiopathol Respir (Nancy) 1971 Jan-Feb;7(1):173–188. [PubMed] [Google Scholar]
- RATTENBORG C. Laryngeal regulation of respiration. Acta Anaesthesiol Scand. 1961;5:129–140. doi: 10.1111/j.1399-6576.1961.tb00091.x. [DOI] [PubMed] [Google Scholar]
- SIMMONS D. H., HEMINGWAY A. Acute respiratory effects of pneumothorax in normal and vagotomized dogs. Am Rev Tuberc. 1957 Aug;76(2):195–214. doi: 10.1164/artpd.1957.76.2.195. [DOI] [PubMed] [Google Scholar]
- Sellick H., Widdicombe J. G. The activity of lung irritant receptors during pneumothorax, hyperpnoea and pulmonary vascular congestion. J Physiol. 1969 Aug;203(2):359–381. doi: 10.1113/jphysiol.1969.sp008868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spann R. W., Hyatt R. E. Factors affecting upper airway resistance in conscious man. J Appl Physiol. 1971 Nov;31(5):708–712. doi: 10.1152/jappl.1971.31.5.708. [DOI] [PubMed] [Google Scholar]
- Stransky A., Szereda-Przestaszewska M., Widdicombe J. G. Changes in laryngeal calibre due to vagal lung reflexes and peripheral chemoreceptor stimulation. J Physiol. 1972 Jul;224(2):88P–89P. [PubMed] [Google Scholar]
- Stransky A., Szereda-Przestaszewska M., Widdicombe J. G. The effects of lung reflexes on laryngeal resistance and motoneurone discharge. J Physiol. 1973 Jun;231(3):417–438. doi: 10.1113/jphysiol.1973.sp010241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stănescu D. C., Clément J., Pattijn J., van de Woestijne K. P. Glottis opening and airway resistance. J Appl Physiol. 1972 Apr;32(4):460–466. doi: 10.1152/jappl.1972.32.4.460. [DOI] [PubMed] [Google Scholar]
- Suzuki M., Kirchner J. A., Murakami Y. The cricothyroid as a respiratory muscle. Its characteristics in bilateral recurrent laryngeal nerve paralysis. Ann Otol Rhinol Laryngol. 1970 Oct;79(5):976–983. doi: 10.1177/000348947007900517. [DOI] [PubMed] [Google Scholar]
- Szereda-Przestaszewska M., Stransky A. The effect of changes in bronchial calibre on upper airway calibre. Bull Physiopathol Respir (Nancy) 1972 May-Jun;8(3):453–457. [PubMed] [Google Scholar]
- Szereda-Przestaszewska M., Widdicombe J. G. Reflex effects of chemical irritation of the upper airways on the laryngeal lumen in cats. Respir Physiol. 1973 Jun;18(1):107–115. doi: 10.1016/0034-5687(73)90026-1. [DOI] [PubMed] [Google Scholar]
- Szereda-Przestaszewska M., Widdicombe J. G. The effect of intravascular injections of veratrine on laryngeal resistance to airflow in cats. Q J Exp Physiol Cogn Med Sci. 1973 Oct;58(4):379–385. doi: 10.1113/expphysiol.1973.sp002231. [DOI] [PubMed] [Google Scholar]
- WIDDICOMBE J. G. The activity of pulmonary stretch receptors during bronchoconstriction, pulmonary oedema, atelectasis and breathing against a resistance. J Physiol. 1961 Dec;159:436–450. doi: 10.1113/jphysiol.1961.sp006819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Burgh Daly M. Interaction of cardiovascular reflexes. Sci Basis Med Annu Rev. 1972:307–332. [PubMed] [Google Scholar]


