When the new Johns Hopkins Hospital opened its ward on 15 May 1893, the first patient was a man with an aortic aneurysm. The inaugural Physician-in-Chief was William Osler, the eminent young professor from McGill University, Montreal. William Halsted, then 40 years old, was appointed Acting Surgeon, and a Temporary Matron, Miss Louisa Parsons, was recruited from the Florence Nightingale School of St. Thomas's Hospital, London. As a student, Osler had already spent an elective period at University College, London, in the laboratory of John Burdon Sanderson, where he worked on platelets. Osler subsequently founded the Medical School at Hopkins in 1899, using as a model the curriculum of Cambridge University. It was Sir John, now the retiring Regius Professor of Medicine at Oxford, who shaped Osler's destiny in 1904 by persuading Prime Minister Balfour to appoint his old student as successor to the Chair at Oxford. Osler had just received a Doctorate of Science from Oxford, and he surprised his North American colleagues by accepting the position. He had previously remarked to friends at dinner, “Do you think I am sufficiently senile to become Regius Professor at Oxford?”
Osler appreciated the capability of young people. In his valedictory lecture at Johns Hopkins (1905), he alluded to this. “In the science and art of medicine, young or comparatively young men have made every advance of the first rank. Vesalius, Harvey, Hunter, Dichat, Laennec, Virchow, Lister, Koch, the green years were yet upon their heads when their epoch-making studies were made. To modify an old saying, a man is sane morally at thirty, rich mentally at forty, wise spiritually at fifty—or never.” He went on to bemoan the uselessness of men above 60 years of age and the incalculable benefit in commercial, political, and professional life if, as a matter of course, men stopped work at 60. Clearly, this sentiment would not be well received in Houston or Oxford at the present time.
Many of Osler's clinical aphorisms were collected by his students during the Johns Hopkins years. Notable amongst these are “Medicine is learnt at the bedside and not in the class room,” “There is no disease more conducive to clinical humility than aneurysm of the aorta,” “Angina pectoris may be precipitated by muscular exertion, violent mental state, stomach upsets or cold weather,” and “A physician who treats himself has a fool for a patient.” The term “ward round” originated from the progression of bedside teaching by Osler and Halsted around the circular building of the Johns Hopkins Hospital.
Even before the advent of air travel, Osler recognized the importance of travel and international fellowship in medicine. “The all important matter is to get a breadth of view as early as possible and this is difficult without travel. To walk the wards of Guy's or St. Bartholomew's, to see the work at St. Louis and the Salpêtrière, to put in a few quiet months of study at one of the German University towns will store the young man's mind with priceless treasures.” Osler went on to become the doyen of Oxford medicine whilst Halsted and Harvey Cushing carried the flag for Johns Hopkins. When Osler's only son was wounded during World War I, Cushing operated but failed to save him.
The Beginnings of Cardiac Surgery
Cardiac surgery had little profile in 1905. Diagnosis was based entirely on clinical findings and was imprecise. Roentgen had discovered x-rays in 1895. The first time x-rays were used for diagnosis was in 1896 when a drunken sailor was admitted to a London hospital with a stab wound in the back. He was paraplegic, and x-rays of the spine showed the tip of the knife blade wedged between 2 vertebrae and encroaching on the spinal canal. Removal of the blade cured the paraplegia.
The first successful cardiac operation occurred in September 1896 when Ludwig Rehn of Frankfurt operated on 22-year-old man stabbed in a drunken brawl. Cardiac tamponade was relieved and a 1.5-cm wound of the right ventricle was closed with 3 interrupted sutures. The first cardiac operation in the United States took place in September 1902 when Luther Hill of Montgomery, Alabama, was called to the home of a 13-year-old boy who had been stabbed 5 times in the chest. The boy was dyspneic, restless, and in shock, with a barely palpable pulse and inaudible heart sounds. Hill recognized cardiac tamponade and proceeded to perform a thoracotomy on the kitchen table, by the light of oil lamps. Chloroform anesthesia was used, the tamponade was relieved, and a right ventricular wound was closed with cat gut. Theodore Tuffier used x-rays to locate a bullet in the chest of a wounded soldier in 1903. The x-rays showed the bullet in the region of the left atrium, and Tuffier removed it from within the pericardial cavity.
In the meantime, Rudolph Matas (a founding fellow of the American College of Surgeons and Honorary Fellow of the Royal College of Surgeons of England) pioneered many of the fundamental aspects of vascular surgery. Matas described intravenous transfusion for the treatment of hemorrhage and shock (1888). He developed the Matas-Smythe pump for artificial respiration (1901) and used the Fell-O'Dwyer apparatus for anesthesia directly into the trachea (1902). He was the first to describe the use of the nasogastric tube and the gastroduodenal tube in intestinal obstruction. He was best known for his work on aneurysms, having described a limb-preserving brachial endoaneurysmorrhaphy in 1888. During Matas's surgical career, which continued until the age of 78, he performed over 260 aneurysm operations.
With little more than the chest x-ray and clinical signs for diagnosis, basic ventilatory care, and fluid infusion, elective cardiac surgery was first attempted in France in 1912. Alexis Carrel and Theodore Tuffier had collaborated on experimental surgery of the heart and thoracic aorta. One of their procedures was to connect the apex of the left ventricle to the descending thoracic aorta with a preserved aortic homograft, to bypass the aortic valve. An opportunity to apply their techniques presented when a 26-year-old patient was admitted with severe aortic stenosis. On 13 July 1912, Tuffier used the recently described median sternotomy incision to expose the patient's heart. He intended to incise the aorta and palpate the valve directly but, in a state of anxiety, he attempted to invaginate the aortic wall and bluntly dilated the valve instead. This disappointing start was followed by a more ambitious procedure by Eugene Doyen. When presented with a critically ill young woman with right ventricular outflow tract obstruction, Doyen passed a tenotome through the wall of the right ventricle, to blindly cut the obstruction. There was little improvement and the girl died a few hours later.
With the French otherwise occupied during World War I, interest in cardiac surgery shifted to the United States. In St. Louis, Evarts Graham and Duff Alan decided that diseased heart valves could be repaired only under direct vision. They designed a cardioscope with a lens at the tip, which would come into direct contact with the intended structure. A valvuloplasty knife was carried inside the tube with its blade set at a right angle to the lens. They planned to use the device in August 1923 on a 31-year-old woman with mitral stenosis. Unfortunately, the patient died before the cardioscope was introduced, and they were unable to solicit another patient.
Mitral Valvotomy – Grounds for Optimism
It fell to Elliott Cutler from Cushing's lab at Harvard to operate successfully for the first time at the Peter Bent Brigham Hospital in Boston (1923). The patient was a bedridden 12-year-old girl, terribly short of breath and with alarming hemoptysis. The child was expected to die soon, and the parents were keen for Cutler to proceed. The operation lasted 1½ hours and utilized a modification of Milton's sternotomy known as the Duval-Barasty approach. The sternal split gave excellent exposure to the heart and enabled the pleura to be dissected away from the pericardium without causing pneumothorax. Cutler inserted a valvulotome into the apex of the left ventricle and attempted to cut both cusps of the stenotic valve. The girl survived surgery, but signs of mitral stenosis persisted and her activity remained restricted. She survived for another 4½ years, and the hemoptysis abated. Ultimately, autopsy examination proved that the mitral orifice had been partly enlarged by the incision. Cutler operated twice more during the next few months but both patients died soon afterwards.
Following Osler's aphorism “In science, the credit goes to the man who convinces the world, not the man to whom the idea first occurred,” it was an Oxford man who is accredited with the breakthrough in mitral valve surgery. Henry Souttar (Fig. 1) was educated at Oxford High School and then Queen's College, Oxford. He became a clinical student at the London Hospital in 1903 and then Staff General Surgeon at the London Hospital in 1915. An innovative surgeon, Souttar was awarded the CBE in 1919 for treatment of war wounds. He had an engineering workshop over his Harley Street house and stored his surgical instruments in a fine mahogany breakfront bookcase in the operating theater at the London Hospital. Although Souttar was convinced that rheumatic mitral stenosis was principally a mechanical problem, the cardiologists regarded surgery as both reckless and unjustified. Sir James McKenzie had said, “The only heart disease I know of is that of the muscle, and no operation will correct it.” Accordingly, Souttar waited until McKenzie died before operating. His patient, Lily Hine from Bethnal Green, was one of 6 children of a tuberculous laborer and had suffered 3 attacks of rheumatic fever. At the age of 10, she had been admitted under Lord Dawson of Penn to the London Hospital, with Sydenham's chorea and rheumatic carditis. At the age of 19, she was again admitted with mitral stenosis, hemoptysis, orthopnea, and heart failure. On 6 May 1925, she was given an anesthetic of ether vapor by tracheal insufflation. Positive pressure was increased as necessary to keep the left lung expanded when the pleural cavity was opened. Souttar entered the chest through the fourth left intercostal space and divided the ribs above to produce a rectangular flap. The atrial appendage was clamped and incised between stay sutures. On removal of the clamp, Souttar easily inserted his index finger into the valve orifice. Although he intended to use an instrument on the valve, his finger separated the leaflets and produced mitral regurgitation. As he withdrew the finger, the lower stay suture tore out and he was faced with a “voluminous gush of blood.” Souttar gripped the appendage and applied an atrial clamp to suture the defect. The procedure was completed in 1 hour without further incident, and the patient improved symptomatically. Although the operation was successful, Souttar was never referred another patient. Mitral valvotomy was not attempted again in the United Kingdom for more than 20 years.

Fig. 1 Henry Souttar
Michael DeBakey trained at Tulane University, New Orleans, while Rudolph Matas was still operating there. Alton Ochsner was head of the department of surgery. After internship at Charity Hospital, DeBakey took a fellowship at Strasbourg University under René Leriche. Leriche had considered that the best treatment for aortic occlusive disease of the abdominal aorta would be excision of the diseased segment and its replacement with a graft (30 years later, DeBakey brought this prediction to reality). After a further period at the University of Heidelberg under Martin Kirschner, DeBakey developed a blood transfusion pump (1934). This was eventually employed in Gibbon's heart–lung machine. Dr. DeBakey returned to Europe during World War II as Director of the Surgical Consultants Division and was eventually discharged from the United States Army as a colonel in 1946. He left the Ochsner Clinic and Tulane University in 1948, to take an appointment as Professor and the first Chairman of Surgery at Baylor University College of Medicine in Houston.
Ductus Arteriosus
In March 1937, an extremely sick 22-year-old woman presented in Boston with Streptococcus viridans bacterial endocarditis on a patent ductus arteriosus. In pre-antibiotic times, recovery was unlikely, and medical management had little to offer. Endotracheal intubation and positive pressure ventilation had only recently been described in the UK by the anesthetists McGill and Rowbottom, and the principles of open-chest surgery were barely established. The surgeon John Streider nevertheless decided to attempt surgical ductus closure and partially achieved this with a series of transfixion sutures. The patient died on the fifth postoperative day from acute dilatation of the stomach.
Eighteen months later, Robert Gross successfully ligated a ductus in a 7-year-old girl at Boston Children's Hospital. Interestingly, Harvey Cushing's biography of Sir William Osler, given to Gross as a Christmas present in his senior college year, so impressed him that he applied to study medicine under Cushing at Harvard Medical School. While still a resident, Gross had worked out the procedure in the autopsy room using a single heavy braided silk ligature. Then 33 years old, he performed the operation despite the orders of his Chief, William Ladd, as he left for his holidays, “Don't try to operate on that little girl's patent ductus. She will die.” When Ladd returned from his vacation, the two met at a tennis match. Ladd asked Gross, “Anything new, Bob?” The laconic chief resident replied, “Nothing much.” Oswald Tubbs performed the first ligation of an infected patent ductus on 5 December 1939 at the Brompton Hospital. In his Hunterian Lecture at the Royal College of Surgeons in April 1943, Tubbs reported 9 operations on infected ductus arteriosus, with 6 survivors.
The War Years
During World War II, there were desperate efforts to develop a reliable antibiotic. At the Dunn School of Pathology in Oxford, Howard Florey, a young Australian pathologist, took on Ernst Chain (a Jewish biochemist who had escaped from Nazi Germany) to help him develop an antibiotic. Scouring the literature, they found a report from Alexander Fleming (1928), who serendipitously had discovered a mould that he had named Penicillium notatum, which could destroy colonies of virulent bacteria. Frustrated by his failure to isolate the substance, Fleming had published only 1 short manuscript about penicillin (1929) and had lost interest. Florey found Fleming's report, obtained a sample of penicillin and, with the biochemist Norman Heatley, succeeded in purifying it. In May 1940, they infected 8 mice with a lethal dose of streptococci, 4 of which were given penicillin. The following day, the treated mice were all well, whereas the others were dead. The Oxford team described “penicillin as a chemotherapeutic agent” in the Lancet on 24 August 1940. Soon afterwards, the substance was tested in human beings. Unsupported in the UK, efforts to develop penicillin were relocated to the United States. As a result, many wounded servicemen were saved between 1943 and 1945.
Alfred Blalock (1899–1965) qualified in medicine at Johns Hopkins in 1922. When internship did not lead to chief residency, he accepted a surgical post at Vanderbilt University, where his research led to a new understanding of the pathophysiology of shock. In 1938, Blalock worked in Sanford Leeds's laboratory on the production of pulmonary hypertension. They joined the subclavian artery to the pulmonary artery. On the strength of his work on shock, Blalock returned to Johns Hopkins as Professor of Surgery in 1941. The following year, he presented his work on subclavian artery bypass to Edward Park and the pediatric department as a solution for coarctation of the aorta. Helen Taussig then asked Blalock if he would create an artificial ductus arteriosus to increase blood flow to the lungs of patients with tetralogy of Fallot. This might provide the means to increase pulmonary blood flow and relieve cyanosis. At the same time, there was increasing interest in other laboratories in the palliation of congenital anomalies. For example, Gross and Hufnagel at Harvard planned to excise coarctation of the aorta and to reconnect the ends by end-to-end anastomosis. Clarence Crafoord, who had visited the Harvard Research Laboratory, beat Gross to the first clinical application with an operation performed on 19 October 1944 in Stockholm. The first patient was a 12-year-old boy and the second, 12 days later, was a 27-year-old farmer.
On the 29 November 1944, Blalock performed the first subclavian-to-pulmonary artery anastomosis at the Halsted Clinic. The chief resident, William Longmire, was first assistant and Denton Cooley, a 24-year-old junior resident, administered fluids. Blalock's experienced technician, Vivien Thomas (who had pioneered the procedure in the laboratory) stood by while Merel Harmel administered an anesthetic of ether and oxygen. Taussig watched the operation from the head of the table. The deeply cyanosed child with tetralogy of Fallot improved in color immediately when the clamps were removed. Although the postoperative course was stormy, the child survived, with excellent symptomatic relief.
Following the first blue baby operations, Blalock and Taussig were invited to tour Europe to demonstrate the procedure. Blalock was accompanied by Henry Bahnson, another junior resident, as Cooley was in Italy on war service. Russell Brock (Fig. 2) invited Blalock to operate at Guy's Hospital, where the shunt procedure was performed successfully on 10 children with tetralogy. Taussig and Blalock presented their experience in the Great Hall of the British Medical Association. At the conclusion of Blalock's lecture, the hall remained dark after the projection of slides when suddenly a long searchlight beam traversed the length of the Hall. The spotlight fell on a Guy's nursing sister who was dressed in a dark blue uniform and holding a small but vivacious blonde 2-year-old girl with tetralogy. The little patient was now pink, after surgery 1 week before. The effect was theatrical and provoked tumultuous applause from the audience. The “blue baby” tour probably changed the course of thoracic surgery in Europe. The potential for heart surgery was soon to be reinforced by the cardiotomy procedures of Dwight Harken for missile wounds (1946) and by the mitral valvotomies of Charles Bailey (1947).

Fig. 2 Lord Brock
Brock and Cooley
At Guy's Hospital, Brock had studied autopsy hearts that were affected by right ventricular outflow tract obstruction. Having observed the pinhole orifice of the pulmonary valve with secondary muscular hypertrophy, he considered a direct surgical attack on the obstruction as an alternative to Blalock's bypass procedure. Brock designed a valvulotome and, after failed attempts to reach the valve from the pulmonary artery, he changed to a transventricular approach. On 16 February 1948, he was able to pass the curved instrument effortlessly into the pulmonary artery of an 18-year-old woman. Before cardiac catheterization, it was difficult to distinguish between the membrane type of pulmonary valve stenosis and the infundibular narrowing of tetralogy of Fallot. For infundibular stenosis, Brock designed a transventricular blunt-nosed punch to core out the obstructed muscle. He used this instrument successfully in 1949 and introduced it to the United States on an exchange visit to Johns Hopkins.
Just as Blalock had profoundly impressed the surgeons of Europe, Brock's impact in Baltimore was no less dramatic. He arrived at Johns Hopkins while Blalock was presenting patients at a case conference at the medical school. Brock appeared in the rear of the auditorium wearing a grey topcoat and Homburg hat, and carrying his own suitcase. Blalock introduced him to the audience and invited him to examine the patient under consideration. Brock put down his suitcase and, without removing hat or coat, stepped onto the stage, took a stethoscope from his pocket, examined the child and the x-ray and stated, “Coarctation of the aorta, surgical correction advised.” It was on this visit that Brock invited the young Denton Cooley to be visiting chief resident at the Brompton Hospital.
Dr. Cooley had already established a formidable reputation at Hopkins. One weekend over the Christ-mas period of 1945, he had been asked to see a patient who had undergone excision of a malignant tumor of the sternum by Grant Ward. The sternum had been replaced with a stellite (Vitalium) plate 10 days before, and Cooley found the man in shock. Ward and Cooley returned the patient to the operating room, but removal of the implant caused profuse hemorrhage. The metal prosthesis had eroded the aorta, causing a false aneurysm. Ward stemmed the bleeding with a finger but was himself incapacitated as a consequence of surgery for a spinal cord tumor. Cooley was obliged to take over. He excised a piece of muscle from the patient's chest wall and sutured it to cover the bleeding point. It was soon clear that the muscle patch would give way. When Ward asked what could be done next, Cooley replied, “I believe I would put a clamp on the side of the aorta and oversew it.” This succeeded, the patient survived, and Cooley won great acclaim.
Dr. Cooley's second aneurysm operation took place at Hopkins after his return from World War II, in the spring of 1949. Blalock was on vacation and Cooley took over the Cardiac Service. One of Blalock's coarctation patients was readmitted with severe chest pain. The chest x-ray showed a massive false aneurysm at the root of the right subclavian artery. Cooley had performed coarctation resection before and decided to excise the aneurysm. Again, the operation proved successful. On his return to Baltimore, Blalock remarked, “If you are confronted with a serious surgical problem that has no proven solution, take a trip to Hawaii and your Resident will handle it.” On 15 January 1949, Dr. Cooley married Louise Thomas (Fig. 3), head nurse of Halsted 5, the main surgical floor at Hopkins.

Fig. 3 Denton and Louise Cooley, 15 January 1949
Cooley at the Brompton Hospital
By now, Michael DeBakey was chairman of surgery at Baylor College of Medicine. Foreseeing the rising interest in cardiovascular surgery, he invited Cooley to join the Baylor staff. Dr. Cooley still wished to take up the fellowship at the Brompton Hospital with Sir Russell Brock, whose heart and lung service was arguably the most exciting in the world. Dr. DeBakey was willing to postpone the Houston appointment, and, in August of 1950, Dr. Cooley, Louise, and their new-born daughter Mary set sail for England on the Queen Elizabeth. Later in life, Lord Brock, then President of the Royal College of Surgeons of England (1969), recalled Dr. Cooley's arrival.
Denton Cooley came to Brompton Hospital as a result of my visit to Johns Hopkins in 1949. As a young man, I recall, with the great advantage of physique. A very good looking young man with charming manners and a nice way of expressing himself, all of which were undeniable attributes. It was immediately apparent that his practical performance as a surgeon was in keeping with the high standard suggested by his physical attributes. His title was Senior Surgical Registrar—the equivalent of Senior Resident in the United States—and he was an extremely active worker operating all the time. A very rapid and able operator with lung as well as heart surgery. I was struck by his extreme restlessness, his pronounced eagerness to do more and better things than anyone else.
Two months after Cooley arrived at Brompton Hospital, Oswald Tubbs developed pulmonary tuberculosis and required a lobectomy. Tubbs requested that Cooley be Brock's first assistant. Two hours before the surgery, Tubbs called Cooley to the bedside and outlined the way he wished the operation to be performed. In exchange for Cooley's persuading Brock to perform a phrenic nerve crush, Tubbs would put Cooley in charge of his practice until he was fit. In fact, Cooley did the phrenic crush himself after Brock had removed the lobe.
Dr. Cooley went on to leave his mark on the Brompton. A prolific and skilled operator, on one occasion he was called to help one of the senior surgeons, “Pasty” Barrett, who had torn the left atrial appendage during an attempted mitral valvotomy. When Cooley walked into the operating room, there was blood all over the floor and a frustrated Barrett exclaimed, “Cooley, this operation should be awfully simple but I've made it simply awful.” On another occasion, Cooley was having difficulty with a rigid bronchoscopy when one of the experienced operating room technicians remarked, “Dr. Cooley, if you hold the bronchoscope still, I will thread the patient over it for you.” Eager to begin his own practice in Houston, Cooley left London earlier than expected, in June 1951.
The Post-War Years
At the beginning of the 1950s, the stage was set for the great advances in cardiovascular surgery. Surgeons such as Harken and Bigelow returned from World War II with ideas and clinical experience on which to base future developments. The closed cardiac operations had already caught the imagination of ambitious young men such as Walton Lillehei, John Kirklin, Donald Ross, Viking Björk, Brian Barratt-Boyes and many others who would mould cardiac surgery into a specialty. John Gibbon was already working towards the development of a pump oxygenator that would allow direct vision during cardiac repair. Key areas of support—such as safe anesthesia, cardiac catheterization, electrocardiography, and defibrillation—were now available, as were antibiotics and anticoagulants.
John Gibbon had started work on the heart-lung machine at Jefferson Medical College in 1937, using roller pumps that had recently been improved upon by Michael DeBakey. After returning from war service, he worked on a larger and more efficient pump oxygenator and obtained some heparin, which had been isolated by Best at the University of Toronto. By 1947, Gibbon was able to perform complete heart– lung bypass in dogs with a low mortality rate.
Wilfred Bigelow explored the use of therapeutic hypothermia in ischemic limbs while serving with the Canadian Army in England, in preparation for the Normandy landings. On returning to the Toronto General Hospital, Bigelow was soon seconded to a fellowship with Blalock at Johns Hopkins Hospital. Learning of John Gibbon's efforts in Philadelphia, Bigelow considered that a simpler option would be to cool the whole body and reduce oxygen requirements. It would then be possible to interrupt the circulation and open the heart. This approach gained support from others. In the late summer of 1952, Floyd Lewis and colleagues at the University of Minnesota used topical cooling with ice to close an atrial septal defect in a 5-year-old girl. The core temperature was reduced to 28 °C, after which the chest was opened and venous inflow to the heart was occluded for 5.5 minutes. During this time, the right atrium was opened and a 2-cm-diameter defect was closed by direct suture. The child recovered and was discharged from hospital 11 days after the operation.
Gibbon's first operation with a pump oxygenator also took place in 1952, on a 15-month-old baby who was believed to have an atrial septal defect. At operation, no hole was found and the postmortem disclosed a large patent ductus arteriosus. Further attempts with the pump oxygenator were made in two 5-year-old girls. One had a multiply fenestrated atrial septum, while the other had multiple cardiac anomalies. Both were failures, but Gibbon's moment of success came on 6 May 1953. An 18-year-old girl was supported by the machine for 26 minutes while a secundum atrial septal defect was closed by direct suture. The operation note was handwritten by Robert K. Finley, “With the patient under Pentothal and oxygen endo-anesthesia, Dr. Gibbon opened the chest through the fourth interspaces bilaterally. The right atrium was large and, by invaginating the appendage, a large intra auricular defect could be felt. The patient was then placed on the oxygenating apparatus (26 minutes on total substitution of heart and lungs), the right auricle opened and the defect sutured closed with 5/0 silk. The patient tolerated the procedure well.” That night, Gibbon telephoned Alfred Blalock and Clarence Crafoord at the Karolinska Institute to tell them the news. When further infants died, Gibbon declared a moratorium on bypass surgery and never attempted a further heart operation.
Gibbon attributed his failure to human error, an issue reinforced by John Kirklin's successful application of the modified Gibbon machine soon afterwards. Kirklin wrote, “In the deepest recesses of my heart, I felt that those four patients died in part because of his lack of appreciation of some of the technical aspects of cardiac surgery.”
Open Heart Surgery in Minnesota
In March 1954, Walton Lillehei adopted a very different approach, that of donor cross-circulation. Against considerable opposition, the Minnesota Group used an infant's parent to sustain the circulation while a ventricular septal defect was closed under direct vision. Lillehei's first operation was undertaken on 26 March 1954 and used a Sigma motor pump to control the flow rate between donor and patient at an average of 40 mL/kg/min at normothermia. The 6.9-kg 1-year-old boy died from severe pulmonary vascular disease 11 days after surgery. Undaunted, Lillehei and colleagues operated successfully on a 4-year-old child on the 20 April 1954 and, by the end of August 1954, had performed 8 operations to close ventricular septal defects, with only 2 deaths. In the months that followed in Minneapolis, a number of surgical firsts were achieved in rapid succession for correction of defects previously deemed inoperable. There was no donor mortality in the 45 cross-circulation operations, and 28 of the infants survived to be discharged from hospital. None of the deaths was attributable to cross-circulation. Notwithstanding, Lillehei abandoned the technique and adopted the DeWall-Lillehei bubble oxygenator in preference.
In 1955, Kirklin and his team at the Mayo Clinic began to use a modified form of Gibbon's pump oxygenator to repair atrioventricular canal defects under direct vision. Kirklin wondered if the artificial oxygenator would be as damaging to the blood as Richard Varco declared it to be in Time magazine (1955). Paradoxically, Kirklin was under pressure from inside and outside the Mayo Clinic to abort these efforts, and to use instead Lillehei's controlled cross-circulation method—which did not cause blood damage, or the so-called postperfusion syndrome. Nevertheless, between March and October 1955, Kirklin produced a successful series of intracardiac operations using the Mayo-Gibbon machine. This work established cardiopulmonary bypass as a safe and reproducible platform for open heart surgery.
Developments in Houston
Dr. Cooley's introduction to Houston was no less eventful than his latter days at Hopkins. Although they had met briefly during World War II, the first clinical encounter between Drs. DeBakey and Cooley was during a staff round at the old Jefferson Davis County Hospital when presented with a patient who had a syphilitic saccular aortic arch aneurysm. As Dr. DeBakey examined the patient, he paused to ask his new colleague how he would approach this problem. Cooley's reply that he would excise the aneurysm produced a stunned silence, until DeBakey asked Cooley to elaborate. Cooley explained that he would put a clamp across the neck of the aneurysm, remove and oversew it, and that this was the patient's only chance for survival. DeBakey asked if he had done this before and, to everyone's amusement, Cooley responded that he had done it twice. Cooley carried out the operation successfully 2 days later. On 5 January 1953, DeBakey and Cooley resected a descending thoracic aneurysm that had caused severe pain through its erosion of the vertebral bodies. An aortic homograft was used as the vascular graft. These early operations established Baylor as the leading center for vascular surgery in the United States and a mecca for those with aneurysmal disease throughout the world. The Duke of Windsor, encouraged by his American wife Wallis Simpson, was operated by DeBakey for a 4.5-cm abdominal aortic aneurysm. While Dr. DeBakey concentrated on aneurysm surgery and the development of vascular grafts, it was Dr. Cooley who pushed forward with cardiac surgery. He used hypothermia to repair 12 atrial septal defects, with only 1 death from coronary embolism.
In the mid 1950s, there were 2 hospitals in the world that routinely performed open heart surgery—the Mayo Clinic and the University of Minnesota Medical Center—and these were only 90 miles apart. Visitors from all parts of the world traveled to both to observe their methods. Dr. Cooley was an early observer in June 1955 and was later to write, “The contrast between the two institutions and the two surgeons was striking. We observed Lillehei and the team composed mostly of house staff correcting a ventricular septal defect using cross-circulation. During the visit, we also saw an oxygenator developed by Richard DeWall at the University of Minnesota. The next day, we observed John Kirklin and his impressive team in Rochester that was made up of physiologists, biochemists, cardiologists and others as they performed operations using the Mayo-Gibbon apparatus. Such a device was beyond my organizational capacity and financial reach. I was deeply disappointed on our return to Houston when Dr. McNamara stated that he would not permit me to operate on his patients unless I had a Mayo-Gibbon apparatus.”
The first operation to employ a pump oxygenator in the UK was at the Hammersmith Hospital, on 9 December 1953. The Melrose machine was a modification of Viking Björk's rotating disk oxygenator; it was first used by Ian Aird and Bill Cleland to support the circulation (rather than to bypass the heart) during a closed aortic valvotomy. Denis Melrose went on to develop cardioplegia. Potassium citrate injected directly into the aortic root produced flaccid diastolic cardiac arrest, which allowed the operation to be carried out in a dry, motionless heart, with less risk of air embolism. To deliberately cause cardiac arrest was enormously controversial at the time and provided an ethical dilemma similar to that of cardiac transplantation. The coroner was present in the operating room for the first use of elective cardiac arrest, and permission was obtained from the leaders of the Anglican, Catholic, and Presbyterian Churches.
Cooley progressed from using the DeWall-Lillehei apparatus to Vincent Gott's simple plastic collapsible oxygenator and from low flow rates (3–4 L/min) to the high-volume perfusion advocated by Kirklin. In 1957, Cooley produced a reusable stainless steel bubble oxygenator, and, by 1961, he had incorporated a bloodless prime (5% dextrose and water). This allowed open cardiac surgery for the first time on Jehovah's Witness patients, hundreds of whom came to Houston.
Artificial Hearts
In tandem with developments in cardiac repair, others were evaluating the prospects for cardiac replacement with a mechanical system. Vladimir Demikhov had designed an artificial heart in Moscow in 1937. His device consisted of 2 membrane pumps side by side, primed with physiological saline. In canine models, the inflow cannulae were inserted into both atrial appendages, and the outflow cannulae were introduced into the aorta and pulmonary artery with clamps. With the dog's ventricles excised, the device sustained life for up to 5½ hours. In 1958, Atsumi and colleagues of Tokyo School of Medicine developed a hydraulically driven plastic heart. Atsumi soon identified the complex mechanical problems of achieving a physiological balance between systemic and pulmonary circulations. In the United States, Willem Kolff, the pioneer of renal dialysis, worked on a pendulum type of artificial heart with his Japanese colleagues Akutsu and Nose.
In Argentina, Domingo Liotta developed an implantable artificial heart with plastics obtained from an aeroplane factory run by immigrant German generals. They undertook hundreds of experiments on dogs and calves, and their third prototype was so successful that the work was presented to the American Society for Artificial Organs. Kolff was impressed by these developments and invited Liotta to join him at the Cleveland Clinic. When Kolff had difficulty in attracting research funds, DeBakey offered Liotta financial backing and laboratory facilities to develop an artificial heart program at Baylor.
Dr. DeBakey recognized that complete cardiac replacement would be excessively problematic and preferred to concentrate on left ventricular support with an implantable device. A substantial grant was obtained from the American Heart Association for Dr. Liotta to work with Drs. Cooley and Beall on left ventricular assist. Their first prototype took blood from the left atrium to the ascending aorta. The second model took blood from the left atrium to the descending aorta, using a tube-type pump that was both safer and easier to insert. The device consisted of a silastic tube reinforced with Dacron, and with ball-type valves at each end to direct flow. Surrounding this tube was a second tube connected to an external source of compressed air. The volume of air pumped into the outside tube could be adjusted from 0 to 60 mL per stroke, and the pump console was driven electrically in synchrony with the R wave of the electrocardiogram. Compressed air in the outside tube squeezed the blood forward in synchrony with the cardiac cycle.
In 1963, Stanley Crawford implanted this device into a 42-year-old man who had received a Starr Edwards valve for calcific aortic stenosis and left ventricular failure. The morning after valve replacement, he had suffered a cardiac arrest, which required internal cardiac massage. The pump performed continuously over the next 4 days, but the patient did not recover from severe cerebral injury. However, 3 years later, on 8 August 1966, a pulsatile pump was implanted in a 37-year-old woman who was critically ill with rheumatic aortic and mitral valve disease. After double valve replacement, she could not be weaned from cardiopulmonary bypass, but the left ventricular assist device (LVAD) sustained her for 10 days, until left ventricular function improved. The device was subsequently explanted and she was discharged from the hospital 18 days after explantation of the LVAD. Encouraged by the result, the team next supported a 16-year-old woman for 4 days after mitral valve replacement. During the late 1950s and early 1960s, the Baylor cardiovascular program expanded. Dr. Cooley developed a large pediatric cardiac practice at Texas Children's Hospital and a massive adult service at St. Luke's Episcopal Hospital. The program outgrew the facilities, and Cooley's ambition was to create a dedicated cardiovascular center independent of the Methodist Hospital and Baylor. Support for this came from the University of Texas, which wished to build a medical school adjacent to St. Luke's. Dr. Cooley recruited architects to design an additional wing to St. Luke's adjacent to Texas Children's Hospital and set about the task of raising funds for the building himself. In practice, Dr. Cooley separated from Dr. DeBakey with the development of the Texas Heart Institute in 1963 (shortly before Crawford implanted Liotta's LVAD). Further developments in Houston took place against a background of intense competition between the 2 teams, which was fueled by media attention. At the Pan Pacific Surgical Congress of 1963, Cooley predicted the advent of heart transplantation and implantable artificial hearts.
Cardiac Transplantation
From 1957, Norman Shumway and his colleague Richard Lower had worked on the 3 most crucial problems in cardiac transplantation. They had worked out a suitable operative technique, established the basis of immunosuppression, and studied the performance of a transplanted heart when cut off from the central nervous system. The outstanding issue now was the timing of donor heart removal.
This problem had frustrated the first attempted transplant (1964) at the University of Mississippi. James Hardy had planned to obtain a donor heart from a young patient dying of brain damage, whose circulation would then be maintained by femoro-femoral bypass. Hardy had already performed the first human lung transplant (June 1963) and had gained experience with immunosuppression, through the use of both drugs and cobalt radiotherapy. At the time, Hardy had confidence that a chimpanzee heart would provide suitable back-up, should an allotransplant fail. Eventually, a 68-year-old man with hypertension and lower-leg gangrene was admitted pulseless and comatose with heart failure, but was resuscitated with tracheostomy, mechanical ventilation, femoral embolectomy, and below-the-knee amputation. There was a young prospective donor in the medical center, but his brain injury did not cause death quickly enough for the transplant. Consequently, the recipient was placed on cardiopulmonary bypass, and a chimpanzee's heart was implanted. The patient died approximately 1 hour after separation from the heart– lung machine, and the outcome was never widely discussed.
Christiaan Barnard's success on 3rd December 1967 came as a surprise to everyone, although he had visited Shumway's laboratory beforehand. Louis Waskansky survived for only 18 days, but Barnard's second patient, the 58-year-old Cape Town dentist Phillip Blaiberg, operated on 2 January 1968, survived for 18 months before dying of chronic rejection. Transplantation began in Houston in May 1968 and would soon overtake the combined experience of all other centers.
By the middle of August 1968, Cooley had performed 9 transplants, but, despite large numbers of accidents and homicides in Houston, donors were scarce. St. Luke's Hospital and the surrounding hotels soon filled with patients awaiting transplants, and, on 1 occasion, Cooley in desperation transplanted a sheep's heart into a 48-year-old man. On 17 August, Dr. Cooley transplanted the heart of an 8-year-old boy (with severe head injuries) into a 5-year-old girl with congenital heart disease. This was the first pediatric transplant, but the recipient survived for less than a week.
At Methodist Hospital, Dr. DeBakey's colleague Ted Diethrich orchestrated a multiple transplantion from a single teenage suicide victim. On 31 August 1968, the donor heart, a single lung, and both kidneys were harvested and transplanted into 4 separate recipients. The newspaper headlines read, “DeBakey team of sixty performs multiple transplant.” During the 12 months after Barnard's first operation, over 100 transplants were performed in almost 50 centers. The results were discouraging, for almost 60 patients were dead by the eighth postoperative day, and the mean survival was less than 30 days. Enthusiasm in the medical profession waned rapidly. Dr. Shumway's first operation, on 6 January 1968 (4 days after the Blaiberg transplant), was unsuccessful. Misfortune hounded the operation from the start. The diseased heart was so large that, after excision, the pericardial cavity was almost 3 times the size of the donor heart. Five hours after the operation, the patient was returned to the operating room with bleeding and tamponade. He received 288 pints of blood and died from hepatic coma. The hospital bill for this operation was $28,845, almost $2,000 per day for the 15 postoperative days. During 1968, Dr. Cooley attempted the first pediatric heart-lung transplant, on a 2½-month-old child with an atrioventricular canal defect and pulmonary hypertension. The infant died within 24 hours.
The Total Artificial Heart
Against this background of failure in biological cardiac replacement came the impetus to succeed with a mechanical artificial heart. Liotta had a design for an implantable total artificial heart driven by carbon dioxide gas pulsed through tubes from a control console. The pumping mechanism consisted of 2 air-driven diaphragm-type reciprocating pumps constructed from Dacron-impregnated silastic with a reticular Dacron fabric lining. Cooley obtained Wada-Cutter valves to provide unidirectional flow. On 30 January 1969, Liotta began a series of total artificial heart implantions in calves and, by the end of March, Haskell Karp, who had a large left ventricular aneurysm, was already identified as a prospective candidate. The device was implanted on Good Friday, 4 April, as a postcardiotomy bridge to cardiac transplantation. By Easter Sunday, Karp's condition had deteriorated and attempts to find a donor heart intensified. A potential donor was located in Massachusetts but the Lear jet dispatched from Houston to bring back the ventilated donor and family suffered a hydraulic system failure. The pilot was forced to make an emergency landing in Louisiana. By the time the second Lear jet reached Houston, the donor had suffered a cardiac arrest and the transplant failed 32 hours later. The sequelae to this operation are well known and are still not resolved today. Kolff wrote in the Hospital Tribune on 14 July 1968, “The implantation of an artificial heart in Houston, Texas on April 4th was a step forward in medical history. Dr. Denton Cooley, Dr. Domingo Liotta and others kept a patient alive for 64 hours with a mechanical heart before he received a natural heart transplant. While the patient eventually died of complications from having the second operation, the important fact is that the Houston doctors proved that an artificial heart can indeed replace a natural one in man.”
Ray C. Fish and the Texas Heart Institute
Although the Texas Heart Institute was founded in 1962, progress towards a dedicated building was restricted by funding. In 1966, Dr. Cooley met the newly appointed president of the Ray C. Fish Foundation, who agreed to provide $500,000 per year for 10 years to support the development. The Foundation was established in memory of Ray Fish, a wealthy pipeline contractor who had died of coronary disease 4 years earlier. As a result of this generosity, the new Texas Heart Institute building opened in 1972; and the first Ray C. Fish Foundation Award for Scientific Achievement was presented to Norman Shumway for his pioneering work in cardiac transplantation. Around this time, Cooley performed his 10,000th heart operation.
Progression in the 1960s
The 1960s were a very exciting time for heart surgery. In 1962, Mason Sones (a later recipient of the Ray C. Fish Award) achieved direct and reproducible catheterization of the coronary arteries, which established the basis for coronary bypass surgery. In May 1967, René Favaloro resected an occluded portion of the right coronary artery and interposed a saphenous vein graft. The following year, this group performed aortocoronary bypass with saphenous vein conduit to the left coronary artery.
In Oxford, Alfred Gunning and Carlos Duran worked to provide a reliable method for aortic homograft harvesting and preparation. As a result of this work, Donald Ross performed the first subcoronary homograft aortic valve replacement on 20 June 1962. Later in life, Mr. Ross reflected on this advance, “Such was our state of unpreparedness that in June 1962 an aortic valve that I was decalcifying disappeared down the sucker tubing at a time when Starr valves were only a distant rumor. We had no alternative but to reconstitute one of our freeze-dried aortic homograft valves and sew it in with a single suture layer—a technique which fortunately had already been suggested to us by our colleagues Gunning and Duran of Oxford. You can imagine our delight when the first valve was not rejected and continued to function in that patient for 4 years. We forgot about the newly available mechanical valves—a state of amnesia which I must confess persists to this day.” In 1967, Ross performed the first pulmonary autograft operation.
Back in Oxford, Duran and Gunning transferred their attention to the preservation of heterograft valves. On 23 September 1964, they performed the first human implantation of a stent-mounted porcine valve. Stent-mounted tissue prostheses were developed further by Carpentier, Ionescu, Hancock, and others in the late 1960s. Cooley, who was not a pig-valve enthusiast, reflected on a case of rapid degeneration of a porcine xenograft in a 12-year-old boy. “About six months earlier, this patient had had a porcine graft placed in the aortic annulus in a city in Louisiana. The poor, bewildered mother, knowing that her son had received a pork graft, asked me what type of valve we would use now. I told her we would use a Björk valve. She said, “What kind of animal is a Björk?”
In August of 1962, George Morris at Methodist Hospital performed the first repair of acute type A dissection. The patient was a senior fellow in Dr. Kirklin's unit at the Mayo Clinic. Morris commented at the time, “Dr. Kirklin, whom I consider the greatest gentleman in American surgery, was the Speaker at the Houston Surgical Society several days after the operation and made rounds with me to visit his assistant.” William Mustard first performed his atrial baffle correction of transposition of the great arteries in 1963. Mustard was an ebullient character. At a meeting in Houston where Lord Brock was the guest speaker, Mustard, who had a passion for diving and spent most of his time in the pool at conferences, recognized the dark suited man, climbed out and said, “Hello Sir. I did enjoy your lecture today.” Brock replied, “Thank you, Dr. Mustard. It is tomorrow morning.”
Westaby in Alabama and Texas
Stephen Westaby was born in a northern English steel town in the year of closed mitral valvotomies (1948). His parents acquired a black-and-white television set in 1955, and Westaby learned about the first open heart operations from news reports. Westaby decided to be a cardiac surgeon at the age of 7, went to Charing Cross Hospital Medical School in London (1966), then qualified in medicine in 1972, after 6 years of competitive rugby and cricket. Keen to gain exposure to cardiac surgery as soon as possible, Westaby obtained the post of resident surgical officer with Oswald Tubbs at the Brompton Hospital shortly before Tubbs's retirement in 1974. Lord Brock had already retired but had left his operating boots in a dusty cupboard in the operating theater suite. Westaby discovered these and adopted them.
Thrown in at the deep end with no previous experience, Westaby performed his first median sternotomy for a right ventricle repair, which was successful. After surgical training at Addenbrooke's Hospital, Cambridge, Westaby returned to cardiac surgery with Hugh Bentall at the Hammersmith Hospital, then with Donald Ross at the Middlesex Hospital. A compulsive operator, Westaby spent little time on paperwork and was dispatched to the University of Alabama (1981) for exposure to Dr. Kirklin's disciplined approach. Westaby spent most of his time in the operating room with Drs. Kirklin, Kouchoukos, Pacifico, and Karp, gaining extensive experience of complex adult and congenital cardiac surgery. His research project was to study, with James Kirklin, the molecular mechanisms of the damaging effects of cardiopulmonary bypass. The interaction between complement anaphylatoxins, white cells, and the whole body inflammatory response was defined by this work, which led to a master's thesis.
On 23 July 1981, Cooley implanted a second total artificial heart, which had been developed by Akutsu, from Kolff's laboratory. The patient had undergone coronary bypass but suffered intractable ventricular fibrillation postoperatively and could not be resuscitated. He was returned to the operating room and placed again on cardiopulmonary bypass. The fibrillating heart was excised and replaced with the total artificial heart until cardiac transplantation 2 days later. On this occasion, Dr. Cooley was assisted by his Texan colleague O.H. Frazier, back from his overseas fellowship as a flight surgeon in Vietnam and a more stressful period as a resident with Dr. DeBakey at the Methodist Hospital. News of the operation traveled fast, and Westaby decided to go to Houston with the hope of meeting Dr. Cooley and seeing the total artificial heart. The trip was a success. Cooley entertained the young English fellow (Fig. 4) with tea in his office and explained the workings of the device. For Westaby, this was the beginning of an enduring interest in mechanical circulatory support, and of his relationship with the Texas Heart Institute. Flushed with success, Westaby went to Methodist Hospital the following day, where Gerald Lawrie took him to watch Michael DeBakey operate.

Fig. 4 The author (left) meets Dr. Cooley.
Houston and the University of Alabama had a profound effect on Westaby's approach to cardiac surgery and inspired an unwillingness to accept the limitations of a cash-strapped National Health Service. Westaby returned to the Hammersmith Hospital as a senior registrar (1982) and continued to study the inflammatory response to bypass. It seemed that post-bypass lung injury and the adult respiratory distress syndrome followed complement activation, sequestration of neutrophils in the pulmonary vasculature, then release of protease enzymes and free radicals, which damaged the alveolar capillary barrier. At the time, the only available protease enzyme inhibitor was aprotinin, which was used in the treatment of pancreatitis. Westaby decided to use aprotinin in an attempt to attenuate the post-perfusion syndrome and, with others, began a clinical trial at the Hammersmith Hospital. It was soon clear that the surgical field appeared unusually dry in patients who received aprotinin. The further development of aprotinin as a hemostatic agent in cardiac surgery is well known.
The Jarvik Heart
In December 1982, after more than $160 million had been invested in the development of an artificial heart, the University of Utah team led by William DeVries implanted a Jarvik-7 total artificial heart as a permanent solution for end-stage heart failure. The patient, 61-year-old dentist Barney Clark, survived for 112 days, but with numerous adverse events. Clark's quality of life was poor and the venture massively expensive. In the midst of controversy, DeVries realized that further implants at the University of Utah were unlikely and moved to a private facility in Louisville, Kentucky. Only 3 further permanent implants were undertaken, although 1 patient survived for 2 years. Dr. Jarvik wrote in Scientific American, “If the artificial heart is ever to achieve its objective, it must be more than a pump. It must be more than functional, reliable, and dependable. It must be forgettable.”
By the 1980s, cardiac transplantation had reached a watershed. After notable advances in immunosuppression and the impressive results of Bailey and colleagues in the pediatric age group, progress decelerated through a lack of donor organs. Many patients died on the waiting list, and outcomes were limited by the side-effects of chronic immunosuppression, by opportunistic infection, and by the development of allograft coronary artery disease. Accordingly, the National Heart, Lung, and Blood Institute invited submissions towards the development of an implantable electrically powered left heart assist system as a possible alternative to transplantation. The major goals were durability exceeding 2 years and mechanical reliability, with a tether-free system. Designs for the Thermo Cardiosystems, Inc. (TCI, now Thoratec) and Novacor LVADs were supported by this initiative and were developed at the Texas Heart Institute and Stanford University, respectively.
The first successful bridge to cardiac transplantation was performed by Oyer at Stanford University using the electric Novacor system in a 51-year-old man with ischemic cardiomyopathy. O.H. Frazier at the Texas Heart Institute implanted the pneumatic TCI LVAD in 1986, followed by the first electric modification in 1991. In September 1991, the electric TCI device was used in a young cardiomyopathy patient who was supported successfully for 505 days. Under the terms of the investigational agreement, the patient was restricted to the hospital grounds, and, depressed by confinement, he abruptly discontinued his warfarin and suffered a massive stroke. When the LVAD was switched off, the patient's own heart continued to support the circulation, thereby revealing a remarkable degree of recovery. This alerted Frazier to the potential for bridge-to-myocardial recovery in idiopathic dilated cardiomyopathy patients.
Back to Oxford
In 1986, Westaby was appointed to develop cardiac surgery in Oxford. His predecessor, Alfred Gunning, had worked single-handedly and with poor support—a few beds on the general surgical ward and no dedicated intensive care facilities. There was a single perfusionist, and a dated heart–lung machine supplied by short-lived gas cylinders. Up to that time, most adults and all children had been sent to London for cardiac surgery. Although Oxford University was founded in the 13th century and the University of Texas in the 19th, there was a stark contrast between their medical facilities. Only radical change could establish a worthwhile cardiac center for Oxford.
With a small group of dedicated nursing staff, Westaby operated all day every weekday, and no further patients were referred elsewhere. Five months later, after resources for 18 months had been spent, the cardiac beds and operating theatres were closed by the administration and Westaby left to operate in Saudi Arabia. When the political smoke had cleared 6 weeks later, he took over a second operating room and made plans for the Oxford Heart Centre. Because competition for intensive care beds was the critical limiting factor, Westaby withdrew cardiac surgery from the general intensive care unit and established a small cardiac recovery area within the operating suite. “Fast-track recovery” began in this unit, where patients who had been operated upon in the morning were returned to the surgical floor in the afternoon. Anesthetic and perfusion techniques were modified to enable 6 patients per day to pass through 3 recovery beds. Rapid recovery prompted early hospital discharge on the fifth or sixth postoperative day. The fast-track approach dramatically reduced the cost of cardiac surgery, enabling many more patients to undergo operation within the allocated budget. With progressive economic constraints in Europe and the United States, the “cardiac surgery without intensive care” approach caused great interest and attracted many overseas fellows and visitors. The activity rate grew rapidly, due partly to a comprehensive pediatric program and an expanding thoracic aortic surgery practice. Within 10 years of Westaby's arrival in Oxford, the surgical volume had expanded from 100 to 1,800 patients per year. The year 1993 provided a new challenge when Westaby met Robert Jarvik at the Society for Thoracic Surgeons meeting in San Antonio. Jarvik showed Westaby the prototype of an axial-flow impeller pump and was persuaded to establish an Oxford laboratory research program in parallel with Frazier's work at the Texas Heart Institute. At the time, there were no large animal facilities in Oxford, so these were developed with charitable donations.
Oxford had been frustrated by the difficulties of having patients accepted onto a transplant waiting list and quite possibly dying before an organ became available. Accordingly, Westaby focused on providing permanent mechanical circulatory support. To overcome the risk of driveline infection, a system was devised to introduce power via a carbon pedestal screwed to the outer table of the skull, a technique adopted from artificial hearing technology. A sheep model was chosen to afford longer testing than could be achieved in the calf.
By 1995, Frazier considered that the electric TCI LVAD could provide a suitable alternative to medical management in end-stage heart failure patients who were not eligible for transplantation. Because the Food and Drug Administration restricted LVAD use to bridge-to-transplant applications, Frazier suggested that the first long-term implants could be performed in Oxford. Against the background of the Jarvik laboratory program, 2 electric TCI implants were performed in idiopathic dilated cardiomyopathy patients, with survival to 6 months. Both patients died of device-related complications, although the second patient left the hospital 4 weeks after implantation and for a few months had an excellent quality of life in the community. Because these patients were not destined for transplantation, native heart function was carefully monitored, and marked improvement was documented. The Oxford LVAD and thoracic aortic surgery programs were supported by first-rate Japanese and Australian fellows, including Takahiro Katsumata, Satoshi Saito, and Matthew Horton, the son of David Horton, who was an overseas fellow with Dr. Cooley at the time of the Haskell Karp operation.
Saving Julie's Heart
In 1997, Professor Richard Clarke from the National Institutes of Health took a new implantable centrifugal pump, the AB-180, to Oxford. This had been used in Pittsburgh on 3 occasions for post-cardiotomy support, but without a survivor. Within 3 days, a 19-year-old student named Julie was sent from the Middlesex Hospital in London with acute viral myocarditis. On a ventilator and with a balloon pump, she had a systolic pressure of 50 mmHg and was anuric and close to death. She was taken directly to an operating theatre at 4 AM and placed on cardiopulmonary bypass for resuscitation. The AB-180 was then implanted into the right pleural cavity and she was weaned onto the LVAD. After 4 days of treatment, the heart showed signs of recovery, and the pump was removed at 7 days. This young woman had virtually normal myocardial function 8 days after pump removal.
Two weeks later, an 8-year-old child was admitted to the pediatric intensive care unit with severe biventricular failure. Again, viral myocarditis was suspected, but the AB-180 was too large. On this occasion, Westaby telephoned Roland Hetzer in Berlin, and a pediatric Berlin Excor system was flown to Oxford on the same day. This reversed the heart failure and the child was extubated. However, the myocardial biopsy showed chronic idiopathic dilated cardiomyopathy, with little likelihood of recovery. The child therefore underwent a cardiac transplant and remains well today. This was the first pediatric bridge to cardiac transplantation in the UK.
In 1998, Terumo brought its new magnetically suspended centrifugal LVAD to Oxford for laboratory testing. The sophisticated Japanese feedback and monitoring equipment allowed detailed study of the effects of long-term circulation without pulse pressure. While end-organ function and histology remained normal out to 12 months of pulseless circulation, significant changes were noted in the morphology of the aortic wall. Absence of pulse pressure caused the smooth muscle of the medial layer to atrophy. However, increasing evidence from Houston and Oxford suggested that continuous flow pumps could be as effective as the pulsatile LVADs. With awareness of the potential for myocardial recovery in the unloaded heart, the stage was set for long-term LVAD therapy. Dr. DeBakey, now in his 10th decade, had also developed an axial-flow pump with engineers of the NASA Space Agency. This was taken to Europe for clinical testing. The prolific work of the German and Austrian centers—particularly at Berlin, Bad Oyenhausen, and Vienna—caused an envious Englishman to remark, “There are three stages in the development of an LVAD —bench work, animal testing, and implantation into Germans!”
By autumn of 1999, the FDA had approved a clinical trial of the Jarvik 2000 as a bridge to cardiac transplantation. In the UK, the Medical Devices Agency sanctioned the first study of “destination therapy” with a continuous-flow pump. A combined Houston-Oxford team carried out the first bridge and permanent implants soon afterwards. All funding (£1.5 million) for the Oxford research and first clinical implants had been obtained on a charitable basis. The first 3 human Jarvik 2000 implants in the UK were funded by the National Heart Research Fund, which, in similar circumstances, had funded the first 3 cardiac transplants by Terence English in Cambridge 30 years before.
The Peter Houghton Story
At age 59, Peter Houghton had reached the end of his natural life. For 10 years, his idiopathic dilated cardiomyopathy become increasingly symptomatic, and he was now housebound, with pitting edema to the thighs and ascites, despite maximum medical therapy. A religious man, psychologist, and counselor for patients dying of AIDS, Peter himself had already received the last rites, after being turned down for cardiac transplantation on grounds of renal dysfunction. A medical friend at the Middlesex Hospital had heard of the Oxford LVAD program and threw Peter a lifeline. After detailed assessment by an independent cardiologist, Philip Poole-Wilson of the Royal Brompton Hospital, everyone agreed that Peter was within weeks of death and had nothing to lose. Westaby had reservations about whether Peter could survive the operation, but in the skeptical and perhaps hostile environment in the UK, only a terminally ill patient could be considered for this novel approach. On 20 June 2000, the operation was carried out in the left lateral position to gain access to the apex of the left ventricle and the descending thoracic aorta. The skull-mounted power system was implanted first, followed by the outflow graft anastomosis to the descending thoracic aorta. The pump was then inserted into the apex of the left ventricle during cardiopulmonary bypass. The postoperative course was difficult. Coagulopathy required re-entry for further hemostasis, and Dr. Frazier's enormous experience was invaluable in achieving survival. Inotropic support was needed to boost right ventricular function, but the elevated afterload decreased pump flow. After initial recovery, the electric cable protruded through one of the neck incisions and had to be revised under local anesthesia. Remarkably, there was no subsequent infection.
Recovery from end-stage heart failure is a slow process irrespective of the improved blood flow. For the first time, the implantable components of an LVAD were imperceptible to the patient, and the external power system was easily portable and simple to use. Houghton was eager to make the best use of what he termed “extra life.” He published a book about his experience titled On Death, Dying, and Not Dying. Another of Houghton's roles was to relieve Westaby of the time-consuming effort to raise funds to keep the program afloat. He sought to inform other heart failure patients of the possibility of extra life and traveled to the USA to help Jarvik and Frazier persuade the Food and Drug Administration to consider destination therapy with continuous flow devices. In a supermarket in Birmingham (UK), the leather bag holding the controller and battery was mistaken for a camera bag and snatched by a teenager. The external power cable was pulled from the percutaneous pedestal, thus triggering the alarm. Fearing a trap, the teenager dropped the bag and Peter, assisted by members of the public, was able to plug himself in and continue shopping. He is now close to the 5th anniversary of the implant and is fitter than ever (Fig. 5). There is a symbiotic relationship between an improving left ventricle and the device that provides unloading and augments cardiac output. Peter Houghton, with Westaby and others, established the charitable Heart Failure Foundation with the intention of providing blood pumps on a widespread basis in the UK.
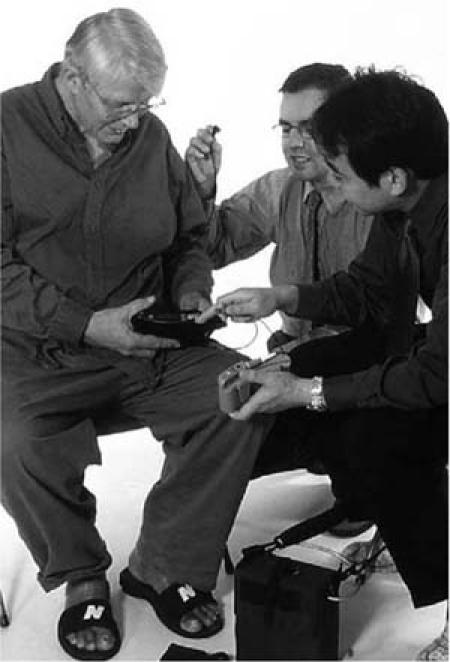
Fig. 5 Peter Houghton (left), recipient of the first permanent implant of a continuous-flow pump (June 2000).
Epilogue
The pursuit of long-term mechanical circulatory support and relief from heart failure has inextricably linked Oxford with Houston. On the 100th anniversary of Osler's arrival in Oxford, the value of international fellowship between the United States and Europe remains as strong as ever. Regrettably, the pressurized modern training programs on both sides of the Atlantic fail to encourage or allow time for international exchange as they once did. Nor are the rich historical aspects of our specialty adequately presented. Why else would off-pump myocardial revascularization be regarded as innovative?
Dr. Cooley has always been a champion of international fellowship. He said, “You must make your Residents and Fellows feel that they are an integral part of the program, members of the team. I believe in sportsmanship in surgery. As captain of the team, the Chief Surgeon should have the confidence and support of his people. If some of these tyrannical surgeons were captain of a rugger team, Lord help them if they ever got into a good scrum; their own men would kick their brains out.”
International fellowship provides a wider perspective on the surgical world, teaches humility, and reduces the likelihood of becoming a tyrannical surgeon. On the subject of humility, Dr. Cooley also said, “A successful cardiovascular surgeon should be a man who, when asked to name the 3 best surgeons in the world, would have difficulty in deciding on the other two!”
A Note on the Author
Always intrigued by the development of cardiac surgery and the great characters behind the advances, Westaby published Landmarks in Cardiac Surgery in 1997, after 5 years of research. In addition to receiving the Cooley Society's International Recognition Award for 2004, he was the proud recipient of the Texas Heart Institute's Ray C. Fish Award for Scientific Achievement that same year.
Footnotes
Address for reprints: Stephen Westaby, MD, Consultant Cardiac Surgeon, Oxford Heart Centre, John Radcliffe Hospital, Headley Way, Headington, Oxford OX3 9DU, United Kingdom
E-mail: swestaby@AHF.org.uk
Presented at the 14th International Meeting of the Denton A. Cooley Cardiovascular Surgical Society, 6–10 October 2004, Houston, Texas


