Abstract
We describe an ST-elevation acute myocardial infarction involving the left main coronary artery in a middle-aged man who was treated by primary angioplasty with the use of sirolimus-eluting stents. To our knowledge, this is the 1st report of survival after sirolimus-eluting stent implantation in a patient with acute occlusion of the left main coronary artery. We discuss the case and review the literature.
Key words: Angioplasty, transluminal, percutaneous coronary; arterial occlusive diseases/complications; coronary angiography; human; male; middle-aged; myocardial infarction/etiology/therapy; stents, drug-eluting
We describe the case of a middle-aged man who had an ST-elevation acute myocardial infarction involving the left main coronary artery. He was treated by primary angioplasty with the use of sirolimus-eluting stents. To our knowledge, this is the 1st report of survival after sirolimus-eluting stent implantation in a patient with acute occlusion of the left main coronary artery.
Case Report
In December 2003, a 57-year-old man with no history of cardiac problems presented at the emergency department of our institution with a 1-hour history of chest discomfort and shortness of breath. There were no traditional cardiac risk factors identifiable, although his lipid profile was unknown. Evaluation in the emergency room revealed the patient to be hypotensive with a systolic blood pressure of 80 to 90 mmHg and in respiratory distress. The initial electrocardiogram revealed sinus rhythm with bifascicular block. The J-point was slurred with no definite ST-segment elevation but was suggestive of an anterior current of injury pattern with inferior ST-depression. Chest radiography confirmed pulmonary edema. The patient was intubated, mechanically ventilated, and given a 60-U/kg bolus of unfractionated intravenous heparin, followed by 12 U/kg per hour infusion, and 325 mg aspirin by nasogastric tube. He was taken emergently to the catheterization laboratory.
The 1st injection of contrast material revealed total occlusion of the left main coronary artery (LMCA) with TIMI grade 0 flow (Fig. 1). Intravenous heparin was continued with an additional bolus to achieve an activated clotting time of 200 to 250 seconds. A periprocedural abciximab bolus and infusion were used in conjunction with clopidogrel, 75 mg, by nasogastric tube. Mechanical reperfusion was initiated, and a 0.014″ coronary guidewire was initially passed into the left anterior descending coronary artery. A TIMI-2 to -3 flow was now established into the left coronary system, and the culprit lesion—a high-grade stenosis with a filling defect suggestive of thrombus—was identified in the LMCA. Coronary intervention was then performed with placement of a 3.5- × 13-mm sirolimus-eluting stent (SES) (CYPHER™, Cordis Corporation, a Johnson and Johnson company; Miami Lakes, Fla) in the LMCA, and TIMI-3 flow was established and maintained (Fig. 2). A 3.75-mm, high-pressure, noncompliant balloon was used for post-stent dilation. Because there was residual stenosis in the proximal left anterior descending coronary artery, a 2nd 2.75- × 23-mm SES (Cordis) was delivered. The right coronary artery (RCA) was then evaluated by angiography and was deemed to be a dominant vessel with no obstructive disease and with no angiographic collateral vessels to the left coronary system; an intra-aortic balloon pump (IABP) was placed for hemodynamic support. The time from onset of symptoms until the establishment of TIMI-3 flow was 120 minutes, with a “door-to-balloon” time of approximately 60 minutes. The patient was transferred to the cardiovascular intensive care unit for further care.
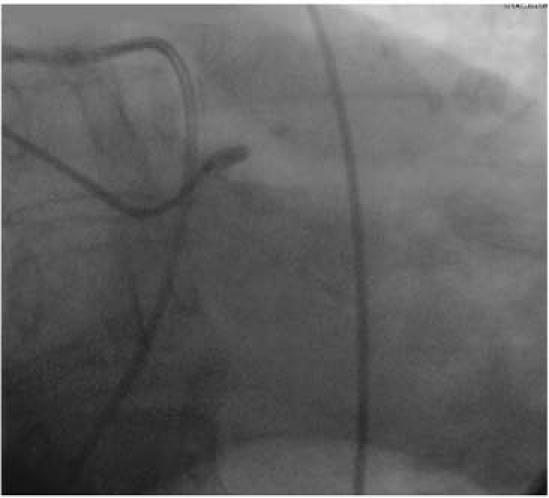
Fig. 1 Coronary angiogram of the left main coronary artery, right anterior oblique projection. A “stump” is visible, with TIMI-0 flow and no filling of either the left anterior descend-ing or circumflex coronary arteries.
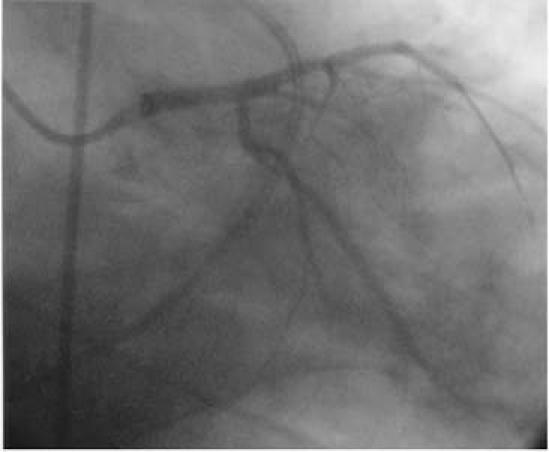
Fig. 2 After deployment of 2 sirolimus-eluting stents in the left main and left anterior descending coronary arteries, TIMI-3 flow can be seen in the left coronary system.
Two days later, transesophageal echocardiography, performed because of poor transthoracic acoustic windows, revealed extensive anterior wall hypokinesis with moderately severe left ventricular dysfunction, and an estimated ejection fraction of 0.25. Vessel patency with normal coronary flow velocities, as shown by color and pulsed-wave Doppler, was noted in the LMCA (Fig. 3). The cardiac index remained 2.5 to 3.0 L/min/cm2; therefore, the IABP was removed at 72 hours. After a difficult course due to prolonged intubation and nosocomial pneumonia, the patient was discharged on hospital day 37 to a rehabilitation facility in stable condition.

Fig. 3 A transesophageal echocardiogram showing the aortic valve in the short-axis view confirms diastolic flow into the ostium and the proximal portion of the left main coronary artery.
Discussion
Total occlusion of the LMCA is an uncommon finding at cardiac catheterization, presumably due to its lethal nature.1 The left coronary system supplies circulation to most of the left ventricular myocardium; therefore, acute occlusion of the left coronary system in the absence of collateral circulation leads to cardiogenic shock and is usually rapidly fatal.2 The prevalence of LMCA total occlusion in patients undergoing coronary angiography is low (0.04%–0.06%) and is extremely rare in patients with acute ST-elevation myocardial infarction undergoing coronary angiography.3 Survival, although uncommon, has been linked to a large and dominant RCA, especially if collateral circulation supplies the left coronary system. In the reported patient, the RCA was large and dominant, but no collateral vessels were identified angiographically. No further conclusion can be made, because it is possible that the collateral vessels functionally regressed once the left main lesion was revascularized. Goldberg and colleagues1 postulated that survival after LMCA occlusion is dependent on the rate of occlusion and the development of right-to-left collateral blood flow.
A 1989 review in the English-language medical literature cited 24 previous cases of acute ST-elevation myocardial infarction caused by total occlusion of the LMCA.4 Treatment options for acute LMCA occlusion have ranged from thrombolytic therapy5 to percutaneous coronary intervention (PCI)6,7 to emergency coronary artery bypass grafting (CABG). Further, there have been several reports that described percutaneous cardiopulmonary bypass in preparation for revascularization.8 Iwasaki and co-authors9 reported a series of 8 patients who had acute LMCA obstruction with myocardial infarction, and discussed reperfusion strategies and the clinical and angiographic outcomes. Those patients were all men between the ages of 55 and 70 years. Seven of the 8 patients presented in cardiogenic shock. Intracoronary thrombolysis (urokinase) was attempted initially in 5 patients and was unsuccessful in 3. Five of the 8 patients underwent PCI, and successful revascularization was achieved in all 5 patients. The use of an IABP was required in all 8 patients. Two patients died in the catheterization laboratory from pump failure, and a 3rd patient died later of congestive heart failure.9 Once again, factors favoring survival were the presence of a dominant RCA and a well-developed collateral circulation.
A review of this topic by Fabbiocchi and coworkers in 199910 cited 5 other cases of LMCA occlusion, and these were treated with emergency stent placement. The authors supported the use of this interventional approach as the quickest and most effective way to achieve reperfusion in these critically ill patients. However, they warned against the use of this method as a “definitive” therapy due to the risks of subacute stent thrombosis and late in-stent restenosis. They concluded that surgical revascularization should be considered, after stabilization of the patient with emergency stenting, as the treatment of choice.10 A report by Spiecker and associates7 expressed similar thoughts: emergency revascularization was carried out with thrombolysis and PCI as the 1st step to stabilize the patient, but surgical revascularization was the definitive treatment.
The use of glycoprotein IIb/IIIa inhibitors has been found to cause a marked reduction of subacute stent thrombosis, especially when combined with high-pressure, noncompliant balloons. To the best of our knowledge, ours is the 1st published report of the use of an SES in a case of acute LMCA occlusion. With the combined lower risk of subacute stent thrombosis (initial reported rate of 0.06% in the United States with SESs) and in-stent restenosis, our belief is that the management strategy presented here will update that proposed by Fabbiocchi's group10 and allow SESs to serve as the definitive revascularization strategy for many patients with acute LMCA occlusion.
There are scattered reports concerning the use of emergency CABG treatment for total LMCA occlusion.11,12 The surgical approach provides revascularization for all areas involved, but the time delay and logistics make this an option that is less than ideal. Lojoi and colleagues11 reported 2 cases of successful emergency CABG in patients with acute myocardial infarction and LMCA occlusion. In both patients, extensive right-to-left collateral vessels were present, and cardiopulmonary bypass was initiated within 2 hours of the onset of symptoms. Although possible, this efficiency is difficult to duplicate, and, if delays are anticipated, support can be provided with either IABP or percutaneous cardiopulmonary support. The investigators are to be congratulated on their success.
In conclusion, acute LMCA occlusion is extremely rare and is usually fatal. Survival has been linked to dominant RCA systems with well-developed collateral circulation. In addition, early reperfusion with revascularization is possible and improves survival. The use of modern interventional techniques such as glycoprotein IIb/IIIa inhibitors and SESs may provide definitive revascularization for many of these patients.
Footnotes
Address for reprints: Howard S. Bush, MD, Department of Cardiology, Desk A23, Cleveland Clinic Florida, 2950 Cleveland Clinic Blvd., Weston, FL 33331
E-mail: bushh@ccf.org
References
- 1.Goldberg S, Grossman W, Markis JE, Cohen MV, Baltaxe HA, Levin DC. Total occlusion of the left main coronary artery. A clinical, hemodynamic and angiographic profile. Am J Med 1978;64:3–8. [DOI] [PubMed]
- 2.de Feyter PJ, Serruys PW. Thrombolysis of acute total occlusion of the left main coronary artery in evolving myocardial infarction. Am J Cardiol 1984;53:1727–8. [DOI] [PubMed]
- 3.Shahian DM, Butterly JR, Malacoff RF. Total obstruction of the left main coronary artery. Ann Thorac Surg 1988;46: 317–20. [DOI] [PubMed]
- 4.Cohen MC, Ferguson DW. Survival after myocardial infarction caused by acute left main coronary artery occlusion: case report and review of the literature. Cathet Cardiovasc Diagn 1989;16:230–8. [DOI] [PubMed]
- 5.Lew AS, Weiss AT, Shah PK, Fishbein MC, Berman DA, Maddahi J. Extensive myocardial salvage and reversal of cardiogenic shock after reperfusion of the left main coronary artery by intravenous streptokinase. Am J Cardiol 1984;54: 450–2. [DOI] [PubMed]
- 6.Itoh T, Fukami K, Oriso S, Umemura J, Nakajima J, Obonai H, Hiramori K. Survival following cardiogenic shock caused by acute left main coronary artery total occlusion. A case report and review of the literature. Angiology 1997;48:163–71. [DOI] [PubMed]
- 7.Spiecker M, Erbel R, Rupprecht HJ, Meyer J. Emergency angioplasty of totally occluded left main coronary artery in acute myocardial infarction and unstable angina pectoris—institutional experience and literature review. Eur Heart J 1994;15:602–7. [DOI] [PubMed]
- 8.Wanner WR, Peterson SC, Blankenship WR, Roman TP. Emergency portable cardiopulmonary bypass for abrupt left main occlusion during coronary angioplasty. Excellent long-term survival. Chest 1992;101:869–70. [DOI] [PubMed]
- 9.Iwasaki K, Kusachi S, Hina K, Nishiyama O, Kondo J, Kita T, et al. Acute left main coronary artery obstruction with myocardial infarction—reperfusion strategies, and the clinical and angiographic outcome. Jpn Circ J 1993;57:891–7. [DOI] [PubMed]
- 10.Fabbiocchi F, Trabattoni D, Galli S, Bartorelli AL. Emergency stenting of totally occluded left main coronary artery in acute myocardial infarction. J Invasive Cardiol 1999;11: 309–12. [PubMed]
- 11.Lijoi A, Della Rovere F, Passerone GC, Dottori V, Scarano F, Bo M, et al. Emergency surgical treatment for total left main coronary artery occlusion. A report of 2 cases. Tex Heart Inst J 1993;20:55–9. [PMC free article] [PubMed]
- 12.Capdeville M, Lee JH. Emergency off-pump coronary artery bypass grafting for acute left main coronary artery dissection. Tex Heart Inst J 2001;28:208–11. [PMC free article] [PubMed]


