Abstract
We describe a case of subacute left ventricular free wall rupture during acute myocardial infarction in a 68-year-old man. The diagnosis was confirmed by echocardiography. The patient was supported by an intra-aortic balloon pump until the ruptured wall could be successfully repaired by suturing and gluing a pericardial patch over the defect and bypassing the left anterior descending coronary artery with a vein graft. This case demonstrates that left ventricular free wall rupture is not always fatal and that early diagnosis and institution of intra-aortic balloon pump support in such patients can allow successful bridging to definitive emergency surgical therapy.
Key words: Echocardiography; heart catheterization; heart rupture, post-infarction/diagnosis/surgery/ultrasonography; heart ventricle/pathology/surgery; humans; intra-aortic balloon pumping; male; myocardial infarction/complications/therapy; ventricular septal rupture
Left ventricular free wall rupture (LVFWR) is a rare complication of acute myocardial infarction (AMI), occurring in approximately 2% of cases1 but even less frequently when primary percutaneous intervention can be performed.2 This complication is often fatal. We describe the presentation and successful treatment of a subacute LVFWR during an AMI in an elderly man.
Case Report
A 68-year-old man was seen in a local emergency room for severe retrosternal chest pain accompanied by dyspnea and sweating. A presumed diagnosis of anterior-wall acute myocardial infarction (AMI) with S-T segment elevation was made. Treatment with reteplase was started. The patient continued to have chest pain, however, and the S-T segment elevations did not resolve. Consequently, the patient was transferred to a tertiary care center, where he underwent percutaneous coronary intervention to deploy a stent in the proximal left descending coronary artery. Abciximab and clopidogrel were administered during this procedure. The rest of the epicardial coronary arteries were found to be normal. The patient's postoperative course over the next 24 hours was uneventful, with no arrhythmia or symptoms of heart failure, until his blood pressure suddenly dropped and he became confused. Dopamine was started, and the patient was transferred to our hospital.
On arrival, the patient was in a state of hemodynamic collapse. He was sweating and lethargic. His blood pressure was 60/45 mmHg, his heart rate was 110 beats/min, and an electrocardiogram showed sinus tachycardia. Auscultation revealed no audible rub or S3 gallop and no new murmurs. Signs of systemic hypoperfusion and cardiogenic shock were noted, and intra-aortic balloon pump (IABP) support was begun immediately. Further electrocardiography revealed sinus tachycardia, low-voltage QRS complexes with diffuse S-T segment elevations, and no electrical alternans. Right heart catheterization showed equalization of diastolic pressures. Echocardiography revealed a large pericardial effusion and manifestations of cardiac tamponade but no signs of myocardial tear, mitral regurgitation, or ventricular septal defect. Once IABP support had sufficiently improved the patient's hemodynamic status, the patient was transported to the operating room. The heart was approached through a sternotomy; then 500 mL of bloody fluid was drained from the pericardium. A pericardial patch was sutured and glued in place over the apical tear, and a vein graft was sutured to the left anterior descending coronary artery. The patient recovered quickly from surgery. After several weeks, he was fully ambulatory and was discharged from the hospital.
At the 3-month follow-up visit, the patient was taking statins, diuretics, β-blockers, angiotensin-converting enzyme inhibitors, and warfarin. Follow-up echocardiography revealed a left ventricular systolic function of 25% to 30%, mild enlargement of the left ventricle in the presence of a moderately large apical aneurysm, and no pericardial effusion.
Discussion
Myocardial rupture is a complication of AMI that directly causes death in 8% of patients.3 A rare but catastrophic form of this complication is LVFWR, the incidence of which is lowered when primary percutaneous intervention can be performed.2 The traditional risk factors of LVFWR are older age, female sex, previous hypertension, and a 1st lateral or anterior-wall AMI.2–7 Contrary to several reports, steroid use and late thrombolysis do not appear to increase the risk of LVFWR.8,9
Classic LVFWR usually produces symptoms within the first 24 hours after an AMI and almost always by the end of the 1st week.10 Clinical manifestations depend on the amount and rate of pericardial bleeding. In most cases, sudden hemodynamic collapse is followed quickly by electromechanical dissociation and death. In some cases, a blood clot will seal pericardial leaks and form a left ventricular pseudoaneurysm.11 A subacute variant of LVFWR, marked by slow repetitive bleeding, occurs in approximately one third of cases.6,12 Unlike patients with classic LVFWR, patients with the subacute variant may survive until emergency surgery can be performed.
Several studies have tried to identify the premonitory signs and symptoms of fatal LVFWR.5,6,12,13 Prodromal manifestations reported so far include persistent chest pain (often erroneously attributed to ischemia), intractable vomiting, restlessness, persistent S-T segment elevation, and positive T wave deflection that persists for 72 hours after the onset of chest pain.6,13 Other classic signs of cardiac tamponade, including pulsus paradoxus and diastolic pressure equalization, are usually absent.12 Electromechanical dissociation may occur but has limited diagnostic value.5
Echocardiography is the considered the best choice for definitive diagnosis of LVFWR. The main echocardiographic findings in patients with LVFWR are pericardial effusion and intrapericardial echoes; occasionally, right-heart collapse or the actual tear itself can be seen. Echocardiography has a diagnostic sensitivity of 100% and a specificity of 93%.12,14 Although hemopericardium may result from thrombolytic and glycoprotein IIb/IIIa inhibitor therapy, LVFWR should always be considered the leading diagnosis in a patient with AMI who is hypotensive and has pericardial effusion.
The definitive treatment for LVFWR is emergency surgical repair; most often, pericardial patch placement is performed with either biological glue or epicardial sutures.15,16 Other surgical techniques include infarctectomy with patch placement and ventricular wall reconstruction.15,17 Temporary therapeutic measures include rapid fluid infusion, administration of positive inotropic agents, and pericardiocentesis.17
Intra-aortic balloon pump support is a widely accepted treatment for ventricular septal rupture complicating AMI.18 However, its role in patients with LVFWR is less clear. Although Pifarre and colleagues suggested long ago that IABP support is a necessary step in achieving postsurgical survival,19 IABP support is not included in current treatment protocols and is used infrequently in patients with LVFWR.10,20 In our opinion, IABP support should be a routine part of initial hemodynamic stabilization. In the present case, we believe that reducing both afterload and wall tension through the use of IABP support significantly improved our patient's chances of survival until surgical treatment could be performed (Fig. 1).
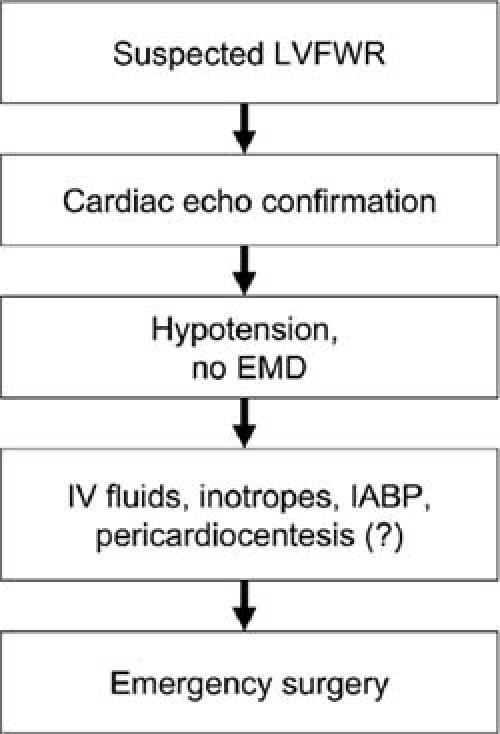
Fig. 1 Algorithm for clinical management of left ventricular free wall rupture in acute myocardial infarction.
EMD = electromechanical dissociation; IABP = intra-aortic balloon pump; IV = intravenous; LVFWR = left ventricular free wall rupture
Some authors have suggested that medical therapy might be appropriate in patients with LVFWR and pseudoaneurysm formation21 or in patients whose hemodynamic recovery is rapid.20 Although off-pump repair has been described,22 the combination of surgical repair with coronary artery bypass grafting is most often advocated. This approach is very practical, because 80% of patients who experience LVFWR have multivessel coronary artery disease.17
In the case reported here, the patient presented with symptoms that suggested subacute LVFWR. Although the slow leakage of blood did cause hemodynamic instability, the leakage was not severe enough to cause complete hemodynamic collapse and massive hemopericardium. Because the patient was receiving IABP support during the period of slow deterioration, we were able to proceed quickly and successfully with combination surgical repair and coronary artery bypass grafting. Moreover, since the patient had very recently undergone coronary catheterization, we were not faced with the dilemma of whether to perform emergency coronary angiography preoperatively in order to determine which coronary arteries to bypass, or whether to proceed directly to surgery and perform empirically based bypassing of all of the major epicardial coronary arteries.7
In summary, the present case demonstrates that left ventricular free wall rupture is not always fatal and that early diagnosis and the institution of IABP support in patients with subacute left ventricular free wall rupture can allow successful bridging to definitive emergency surgical therapy.
Footnotes
Address for reprints: Frank W. Smart, MD, Texas Heart Institute, 6770 Bertner Ave., Suite C355N, Houston, TX 77030
E-mail: smartcardio@hotmail.com
Dr. Amir is now at the Department of Cardiology, Lady Davis Hospital, Carmel Medical Center, 7 Michal Street, Haifa, 34362 Israel.
References
- 1.Moreno R, Lopez de Sa E, Lopez-Sendon JL, Garcia E, Soriano J, Abeytua M, et al. Frequency of left ventricular free-wall rupture in patients with acute myocardial infarction treated with primary angioplasty. Am J Cardiol 2000;85: 757–60, A8. [DOI] [PubMed]
- 2.Yip HK, Wu CJ, Chang HW, Wang CP, Cheng CI, Chua S, Chen MC. Cardiac rupture complicating acute myocardial infarction in the direct percutaneous coronary intervention reperfusion era. Chest 2003;124:565–71. [DOI] [PubMed]
- 3.Reddy SG, Roberts WC. Frequency of rupture of the left ventricular free wall or ventricular septum among necropsy cases of fatal acute myocardial infarction since introduction of coronary care units. Am J Cardiol 1989;63:906–11. [DOI] [PubMed]
- 4.Batts KP, Ackermann DM, Edwards WD. Postinfarction rupture of the left ventricular free wall: clinicopathologic correlates in 100 consecutive autopsy cases. Hum Pathol 1990;21:530–5. [DOI] [PubMed]
- 5.Figueras J, Curos A, Cortadellas J, Soler-Soler J. Reliability of electromechanical dissociation in the diagnosis of left ventricular free wall rupture in acute myocardial infarction. Am Heart J 1996;131:861–4. [DOI] [PubMed]
- 6.Raitt MH, Kraft CD, Gardner CJ, Pearlman AS, Otto CM. Subacute ventricular free wall rupture complicating myocardial infarction. Am Heart J 1993;126:946–55. [DOI] [PubMed]
- 7.Sutherland FW, Guell FJ, Pathi VL, Naik SK. Postinfarction ventricular free wall rupture: strategies for diagnosis and treatment. Ann Thorac Surg 1996;61:1281–5. [DOI] [PubMed]
- 8.Giugliano GR, Giugliano RP, Gibson CM, Kuntz RE. Meta-analysis of corticosteroid treatment in acute myocardial infarction. Am J Cardiol 2003;91:1055–9. [DOI] [PubMed]
- 9.Becker RC, Charlesworth A, Wilcox RG, Hampton J, Skene A, Gore JM, Topol EJ. Cardiac rupture associated with thrombolytic therapy: impact of time to treatment in the Late Assessment of Thrombolytic Efficacy (LATE) study. J Am Coll Cardiol 1995;25:1063–8. [DOI] [PubMed]
- 10.Purcaro A, Costantini C, Ciampani N, Mazzanti M, Silenzi C, Gili A, et al. Diagnostic criteria and management of subacute ventricular free wall rupture complicating acute myocardial infarction. Am J Cardiol 1997;80:397–405. [DOI] [PubMed]
- 11.Mahilmaran A, Nayar PG, Sheshadri M, Sudarsana G, Abraham KA. Left ventricular pseudoaneurysm caused by coronary spasm, myocardial infarction, and myocardial rupture. Tex Heart Inst J 2002;29:122–5. [PMC free article] [PubMed]
- 12.Lopez-Sendon J, Gonzalez A, Lopez de Sa E, Coma-Canella I, Roldan I, Dominguez F, et al. Diagnosis of subacute ventricular wall rupture after acute myocardial infarction: sensitivity and specificity of clinical, hemodynamic and echocardiographic criteria. J Am Coll Cardiol 1992;19:1145–53. [DOI] [PubMed]
- 13.Oliva PB, Hammill SC, Edwards WD. Cardiac rupture, a clinically predictable complication of acute myocardial infarction: report of 70 cases with clinicopathologic correlations. J Am Coll Cardiol 1993;22:720–6. [DOI] [PubMed]
- 14.Mittle S, Makaryus AN, Mangion J. Role of contrast echocardiography in the assessment of myocardial rupture. Echocardiography 2003;20:77–81. [DOI] [PubMed]
- 15.Mantovani V, Vanoli D, Chelazzi P, Lepore V, Ferrarese S, Sala A. Post-infarction cardiac rupture: surgical treatment. Eur J Cardiothorac Surg 2002;22:777–80. [DOI] [PubMed]
- 16.Padro JM, Mesa JM, Silvestre J, Larrea JL, Caralps JM, Cerron F, Aris A. Subacute cardiac rupture: repair with a sutureless technique. Ann Thorac Surg 1993;55:20–4. [DOI] [PubMed]
- 17.Reardon MJ, Carr CL, Diamond A, Letsou GV, Safi HJ, Espada R, Baldwin JC. Ischemic left ventricular free wall rupture: prediction, diagnosis, and treatment. Ann Thorac Surg 1997;64:1509–13. [DOI] [PubMed]
- 18.Birnbaum Y, Fishbein MC, Blanche C, Siegel RJ. Ventricular septal rupture after acute myocardial infarction. N Engl J Med 2002;347:1426–32. [DOI] [PubMed]
- 19.Pifarre R, Sullivan HJ, Grieco J, Montoya A, Bakhos M, Scanlon PJ, Gunnar RM. Management of left ventricular rupture complicating myocardial infarction. J Thorac Cardiovasc Surg 1983;86:441–3. [PubMed]
- 20.Figueras J, Cortadellas J, Evangelista A, Soler-Soler J. Medical management of selected patients with left ventricular free wall rupture during acute myocardial infarction. J Am Coll Cardiol 1997;29:512–8. [DOI] [PubMed]
- 21.Moreno R, Gordillo E, Zamorano J, Almeria C, Garcia-Rubira JC, Fernandez-Ortiz A, Macaya C. Long term outcome of patients with postinfarction left ventricular pseudoaneurysm. Heart 2003;89:1144–6. [DOI] [PMC free article] [PubMed]
- 22.Park WM, Connery CP, Hochman JS, Tilson MD, Anagnostopoulos CE. Successful repair of myocardial free wall rupture after thrombolytic therapy for acute infarction. Ann Thorac Surg 2000;70:1345–9. [DOI] [PubMed]


