Abstract
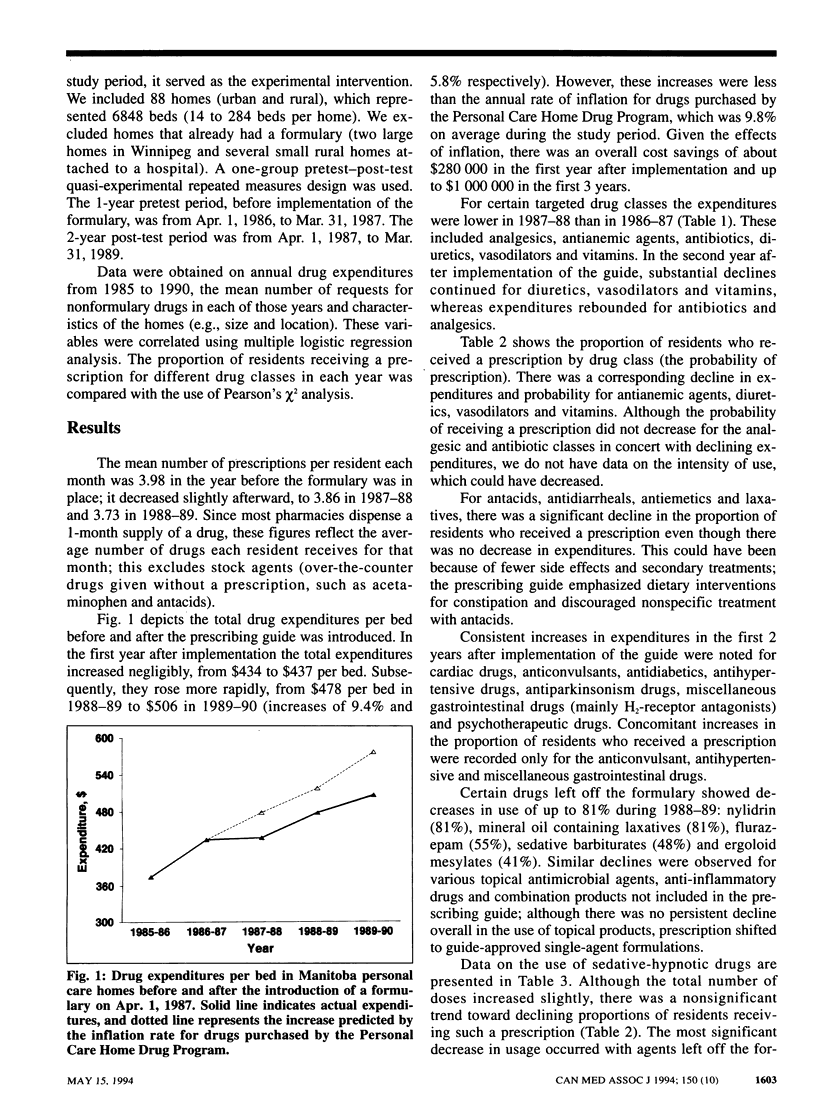
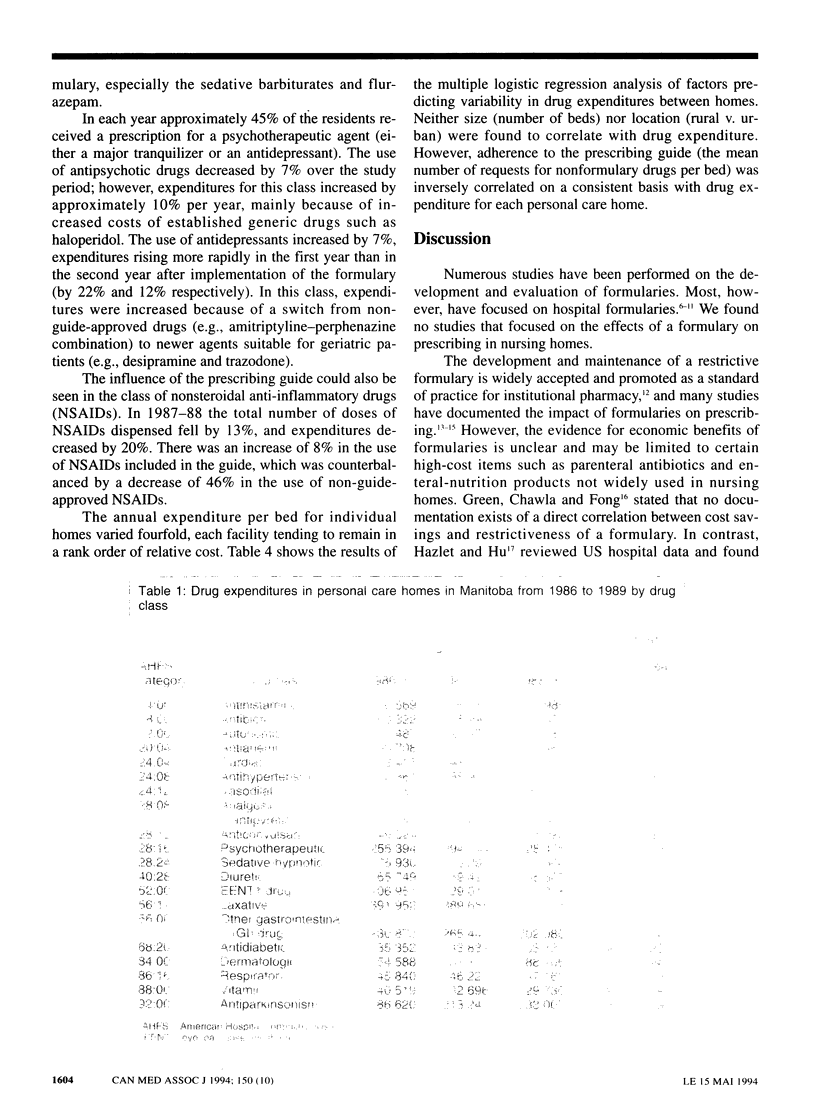
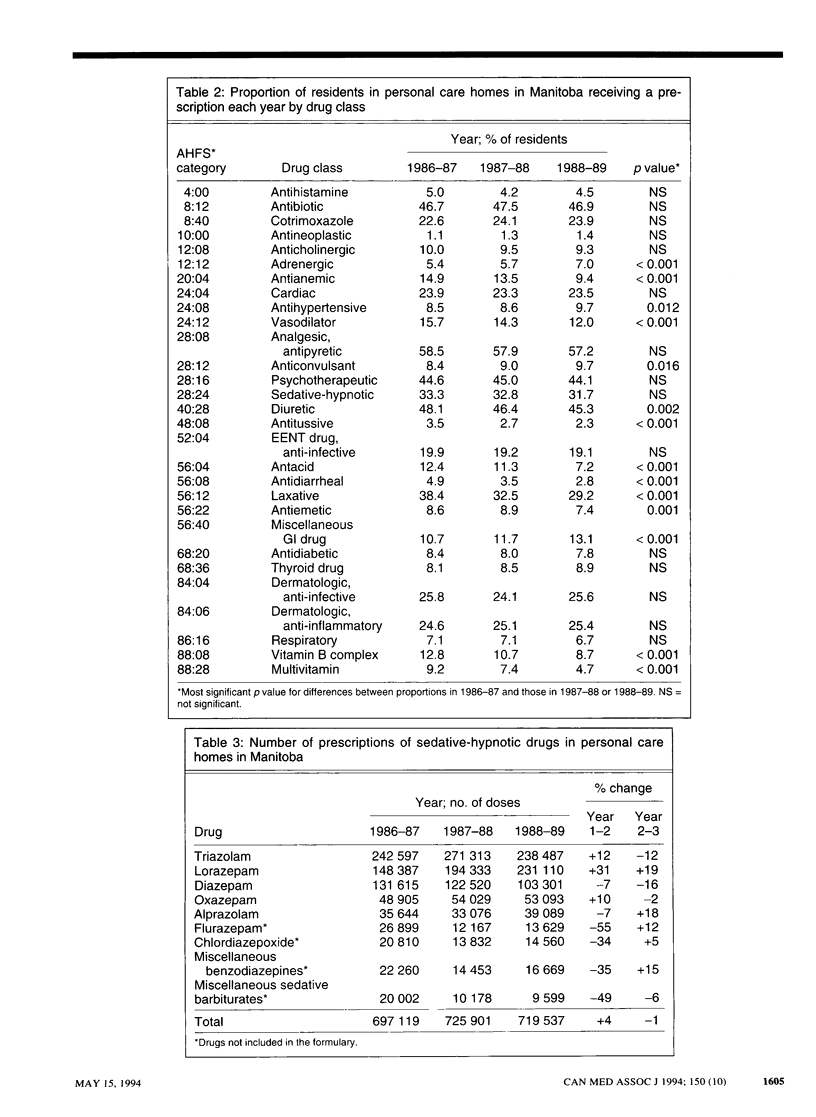
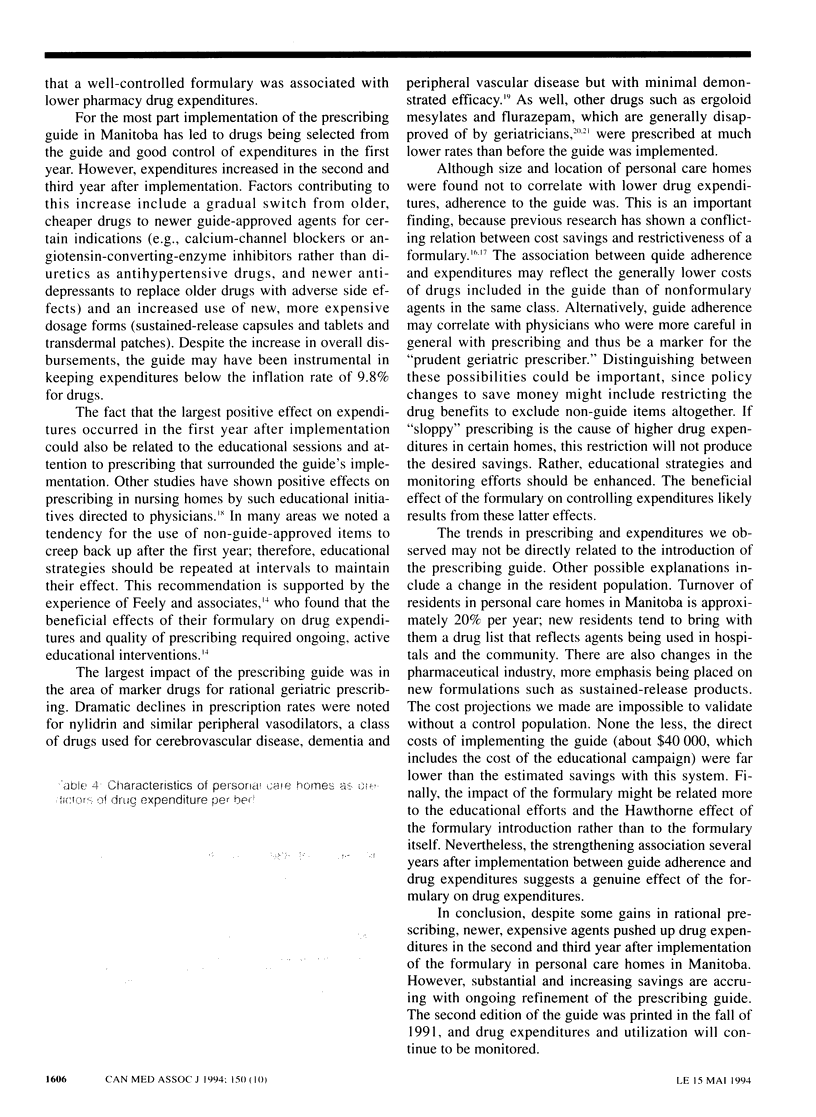
OBJECTIVE: To assess the impact of a formulary on drug expenditures and prescribing trends in personal care homes (nursing homes). DESIGN: Quasi-experimental analysis of a drug prescription database before and after implementation of the formulary. SETTING: Personal care homes in Manitoba. PATIENTS: Residents occupying the 6848 beds of the 88 personal care homes that did not already have a formulary. INTERVENTION: Formulary, introduced Apr. 1, 1987. MAIN OUTCOME MEASURES: Drug expenditures from Apr. 1, 1985, to Mar. 31, 1990; proportion of residents receiving a prescription by drug class and rate of prescriptions of nonformulary drugs in the year before and 2 years after the formulary was introduced. MAIN RESULTS: The total drug expenditures per bed remained constant during the first year after the formulary was implemented, even though the annual drug inflation rate was 9.8% on average during the study period. Expenditures 2 and 3 years after implementation rose by 9.4% and 5.8% respectively. Those for specific agents and drug classes targeted as being inappropriate for long-term care decreased greatly because of reduced prescribing. Expenditures for some other drug classes increased mainly because newer, more expensive agents were used. The mean drug expenditure per bed varied widely between homes; neither size nor location were found to correlate with drug expenditure, but adherence to the formulary did predict personal care homes with decreased expenditures. CONCLUSIONS: A formulary in personal care homes can improve therapeutic management. The impact on cost containment was not as strong after the first year, although expenditures remained less than the rate of inflation for drug costs.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anandan J. V. Reducing the number of formulary theophylline preparations. Am J Hosp Pharm. 1981 Apr;38(4):511–513. [PubMed] [Google Scholar]
- Avorn J., Soumerai S. B., Everitt D. E., Ross-Degnan D., Beers M. H., Sherman D., Salem-Schatz S. R., Fields D. A randomized trial of a program to reduce the use of psychoactive drugs in nursing homes. N Engl J Med. 1992 Jul 16;327(3):168–173. doi: 10.1056/NEJM199207163270306. [DOI] [PubMed] [Google Scholar]
- Barriere S. L. Controversies in antimicrobial therapy: formulary decisions on third-generation cephalosporins. Am J Hosp Pharm. 1986 Mar;43(3):625–629. [PubMed] [Google Scholar]
- Branch R. A., Johnston P. E., Koestner J. A., Bluhm R., Stratton C. W., Knight J. R. The formulary: an educational tool for clinical pharmacology. Clin Pharmacol Ther. 1992 May;51(5):481–488. doi: 10.1038/clpt.1992.51. [DOI] [PubMed] [Google Scholar]
- Carty M. A., Everitt D. E. Basic principles of prescribing for geriatric outpatients. Geriatrics. 1989 Jun;44(6):85-8, 90-2, 97-8. [PubMed] [Google Scholar]
- Daniels C. E., Wertheimer A. I. Analysis of hospital formulary effects on cost control. Top Hosp Pharm Manage. 1982 Aug;2(2):32–49. [PubMed] [Google Scholar]
- Durfee D. D., Skinner-Domet V. M. Cost effectiveness of an enteral products formulary. Am J Hosp Pharm. 1984 Nov;41(11):2352–2354. [PubMed] [Google Scholar]
- Feely J., Chan R., Cocoman L., Mulpeter K., O'Connor P. Hospital formularies: need for continuous intervention. BMJ. 1990 Jan 6;300(6716):28–30. doi: 10.1136/bmj.300.6716.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J. A., Chawla A. K., Fong P. A. Evaluating a restrictive formulary system by assessing nonformulary-drug requests. Am J Hosp Pharm. 1985 Jul;42(7):1537–1541. [PubMed] [Google Scholar]
- Hazlet T. K., Hu T. W. Association between formulary strategies and hospital drug expenditures. Am J Hosp Pharm. 1992 Sep;49(9):2207–2210. [PubMed] [Google Scholar]
- Morgan D. J., Sutters C. A., Pugh S. Medical audit and formulary management: a policy for rational use of thrombolytic drugs. Postgrad Med J. 1991 Feb;67(784):165–169. doi: 10.1136/pgmj.67.784.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosner M. M. The financial effects of formularies in hospitals. Am J Hosp Pharm. 1966 Dec;23(12):673–675. [PubMed] [Google Scholar]
- Sylvester K. L., Wudds T. W. Cost savings through formulary implementation and group purchasing in four therapeutic categories. Hosp Formul. 1986 Mar;21(3):357-60, 369-70. [PubMed] [Google Scholar]
- Thompson T. L., 2nd, Filley C. M., Mitchell W. D., Culig K. M., LoVerde M., Byyny R. L. Lack of efficacy of hydergine in patients with Alzheimer's disease. N Engl J Med. 1990 Aug 16;323(7):445–448. doi: 10.1056/NEJM199008163230704. [DOI] [PubMed] [Google Scholar]


