Abstract
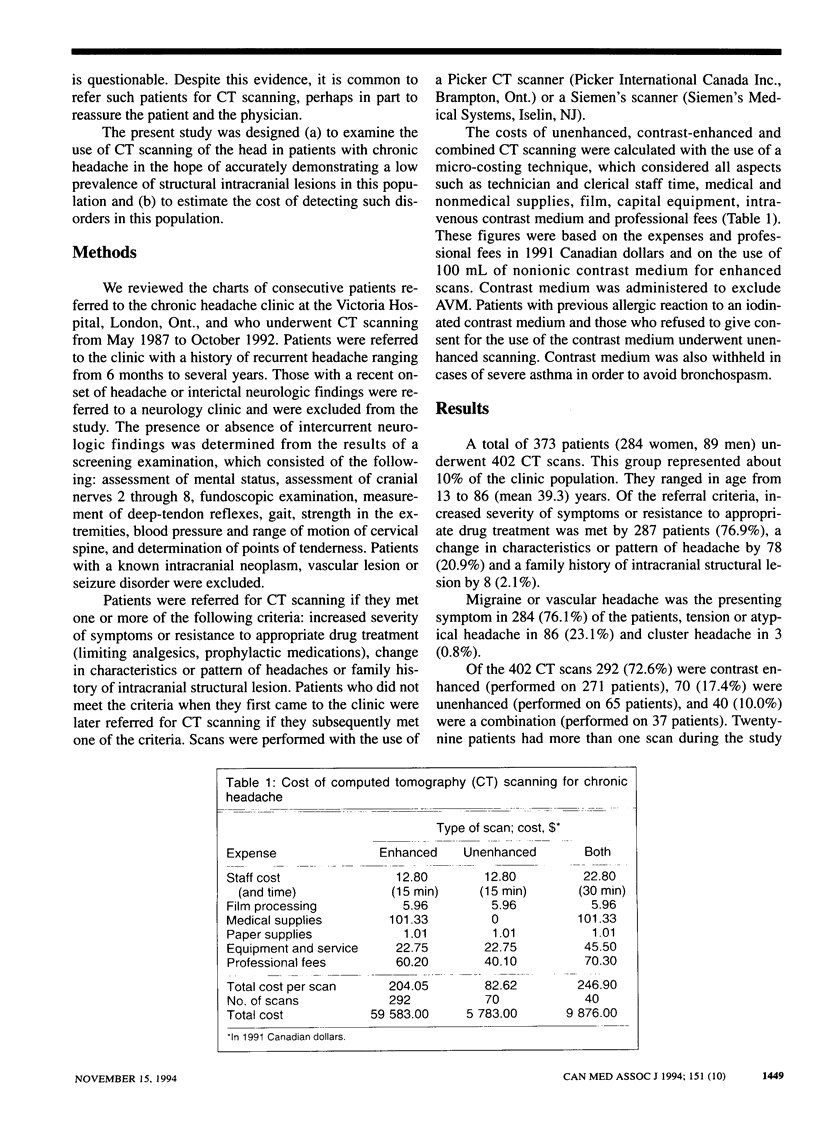
OBJECTIVE: To determine whether the rate of detecting a tumour, arteriovenous malformation (AVM) or aneurysm with the use of enhanced or unenhanced computed tomography (CT) is significant in patients with chronic headache and to calculate the cost. DESIGN: Case series. SETTING: Chronic headache clinic at a tertiary care referral centre. PATIENTS: All 373 consecutive patients with chronic headache (284 women, 89 men) referred for CT scanning from May 1987 to October 1992 who met one or more of the following criteria: increased severity of symptoms or resistance to appropriate drug therapy (287 patients [76.9%]), change in characteristics or pattern of headache (78 [20.9%]) or family history of intracranial structural lesion (8 [2.1%]). INTERVENTIONS: CT scans of the head were enhanced with nonionic contrast medium (292 scans), were unenhanced (70) or involved both methods (40). OUTCOME MEASURES: Number and nature of minor and major findings, and total price per scan. RESULTS: Of the 402 CT scans 14 (95% confidence interval [CI] 7 to 21) revealed minor findings that did not alter patient management: infarct (9 scans), cerebral atrophy (2), cavum vergae (1), hyperostosis frontalis interna (1) and communicating hydrocephalus (1). Four scans (95% CI 0 to 8) showed significant lesions: osteoma (2), low-grade glioma (1) and aneurysm (1); only the aneurysm was treated. There were no cases of AVM. An unenhanced scan cost $82.63 and an enhanced scan $204.05. The cost per significant finding was over $18,000. In all, it cost $74,243 to find one treatable vascular lesion. CONCLUSIONS: The detection rate of CT scanning in patients with chronic headache is similar to that expected in the general population, provided the neurologic findings are normal. The cost of detecting intracranial lesions in this patient population is high [corrected].
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baker H. L., Jr Cranial CT in the investigation of headache: cost-effectiveness for brain tumors. J Neuroradiol. 1983;10(2):112–116. [PubMed] [Google Scholar]
- Bannerman R. M., Ingall G. B., Graf C. J. The familial occurrence of intracranial aneurysms. Neurology. 1970 Mar;20(3):283–292. doi: 10.1212/wnl.20.3.283. [DOI] [PubMed] [Google Scholar]
- Bruyn G. W. Intracranial arteriovenous malformation and migraine. Cephalalgia. 1984 Sep;4(3):191–207. doi: 10.1046/j.1468-2982.1984.0403191.x. [DOI] [PubMed] [Google Scholar]
- Cuetter A. C., Aita J. F. CT scanning in classic migraine. Headache. 1983 Jul;23(4):195–195. doi: 10.1111/j.1526-4610.1983.hed2304195.x. [DOI] [PubMed] [Google Scholar]
- Debruyne J., Crevits L., Vander Eecken H. Migraine-like headache in intraventricular tumours. Clin Neurol Neurosurg. 1982;84(1):51–57. doi: 10.1016/0303-8467(82)90110-x. [DOI] [PubMed] [Google Scholar]
- Grosskreutz S. R., Osborn R. E., Sanchez R. M. Computed tomography of the brain in the evaluation of the headache patient. Mil Med. 1991 Mar;156(3):137–140. [PubMed] [Google Scholar]
- Herzeberg L., Lenman J. A., Victoratos G., Fletcher F. Cluster headaches associated with vascular malformations. J Neurol Neurosurg Psychiatry. 1975 Jul;38(7):648–649. doi: 10.1136/jnnp.38.7.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindfelt B., Olivecrona H. Cerebral arteriovenous malformation and cluster-like headache. Headache. 1991 Sep;31(8):514–517. doi: 10.1111/j.1526-4610.1991.hed3108514.x. [DOI] [PubMed] [Google Scholar]
- Joseph R., Cook G. E., Steiner T. J., Clifford Rose F. Intracranial space-occupying lesions in patients attending a migraine clinic. Practitioner. 1985 May;229(1403):477–481. [PubMed] [Google Scholar]
- Kuritzky A. Cluster headache-like pain caused by an upper cervical meningioma. Cephalalgia. 1984 Sep;4(3):185–186. doi: 10.1046/j.1468-2982.1984.0403185.x. [DOI] [PubMed] [Google Scholar]
- MCKISSOCK W., PATERSON J. H. A clinical survey of intracranial angiomas with special reference to their mode of progression and surgical treatment: a report of 110 cases. Brain. 1956 Jun;79(2):233–266. doi: 10.1093/brain/79.2.233. [DOI] [PubMed] [Google Scholar]
- Mani S., Deeter J. Arteriovenous malformation of the brain presenting as a cluster headache--a case report. Headache. 1982 Jul;22(4):184–185. doi: 10.1111/j.1526-4610.1982.hed2204184.x. [DOI] [PubMed] [Google Scholar]
- OZER M. N., SENCER W., BLOCK J. A CLINICAL STUDY OF CEREBRAL VASCULAR MALFORMATIONS. (THE SIGNIFICANCE OF MIGRAINE). J Mt Sinai Hosp N Y. 1964 Sep-Oct;31:403–423. [PubMed] [Google Scholar]
- Reutens D. C., Stewart-Wynne E. G. Factors influencing the yield of cranial CT scanning in a private neurological practice. Clin Exp Neurol. 1989;26:169–175. [PubMed] [Google Scholar]
- Sargent J. D., Solbach P. Medical evaluation of migraineurs: review of the value of laboratory and radiologic tests. Headache. 1983 Mar;23(2):62–65. doi: 10.1111/j.1526-4610.1983.hed2302062.x. [DOI] [PubMed] [Google Scholar]
- Schlake H. P., Grotemeyer K. H., Husstedt I. W., Schuierer G., Brune G. G. "Symptomatic migraine": intracranial lesions mimicking migrainous headache--a report of three cases. Headache. 1991 Nov;31(10):661–665. doi: 10.1111/j.1526-4610.1991.hed3110661.x. [DOI] [PubMed] [Google Scholar]
- Schoenberg B. S. Epidemiology of primary nervous system neoplasms. Adv Neurol. 1978;19:475–495. [PubMed] [Google Scholar]
- Sotaniemi K. A., Rantala M., Pyhtinen J., Myllylä V. V. Clinical and CT correlates in the diagnosis of intracranial tumours. J Neurol Neurosurg Psychiatry. 1991 Jul;54(7):645–647. doi: 10.1136/jnnp.54.7.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa D., Frediani F., Bussone G. Cluster headache-like syndrome due to arteriovenous malformation. Headache. 1988 Feb;28(1):36–38. doi: 10.1111/j.1365-2524.1988.hed2801036.x. [DOI] [PubMed] [Google Scholar]
- Thomas A. L. Periodic migrainous neuralgia associated with an arteriovenous malformation. Postgrad Med J. 1975 Jul;51(597):460–462. doi: 10.1136/pgmj.51.597.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troost B. T., Newton T. H. Occipital lobe arteriovenous malformations. Clinical and radiologic features in 26 cases with comments on differentiation from migraine. Arch Ophthalmol. 1975 Apr;93(4):250–256. doi: 10.1001/archopht.1975.01010020260002. [DOI] [PubMed] [Google Scholar]
- Waltimo O., Hokkanen E., Pirskanen R. Intracranial arteriovenous malformations and headache. Headache. 1975 Jul;15(2):133–135. doi: 10.1111/j.1526-4610.1975.hed02133.x. [DOI] [PubMed] [Google Scholar]
- West P., Todman D. Chronic cluster headache associated with a vertebral artery aneurysm. Headache. 1991 Apr;31(4):210–212. doi: 10.1111/j.1526-4610.1991.hed3104210.x. [DOI] [PubMed] [Google Scholar]



