Abstract
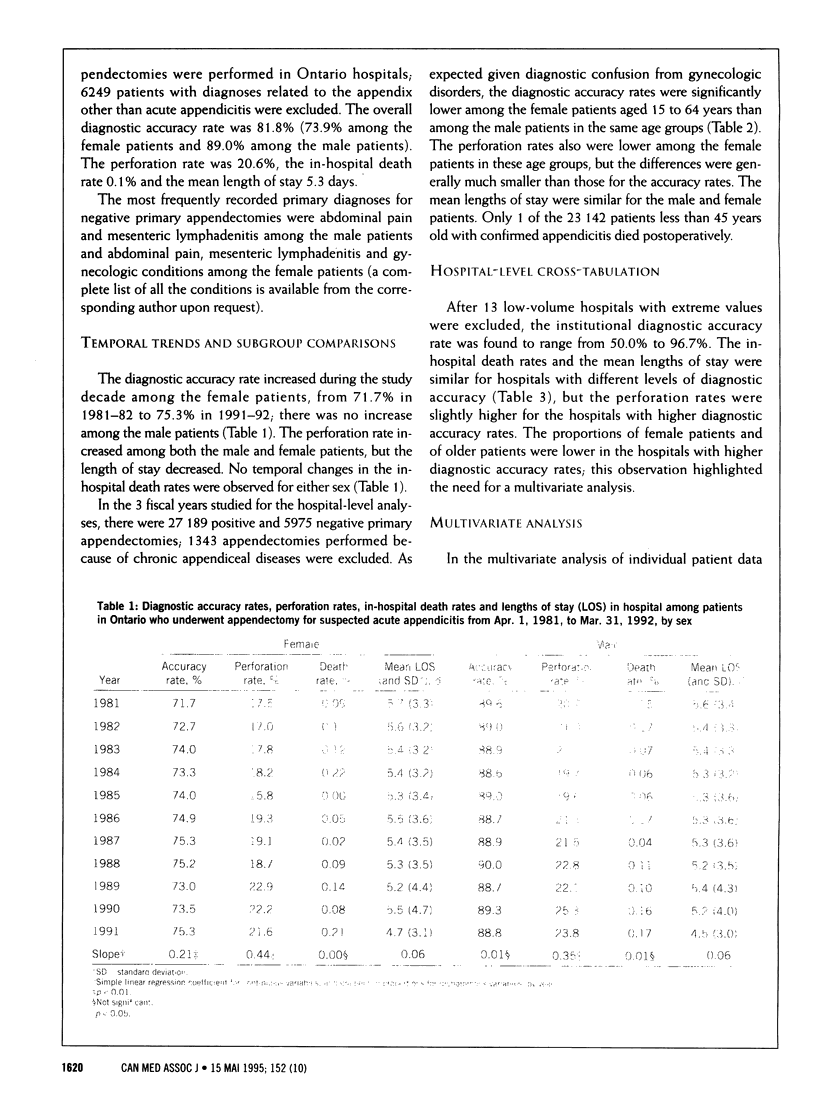
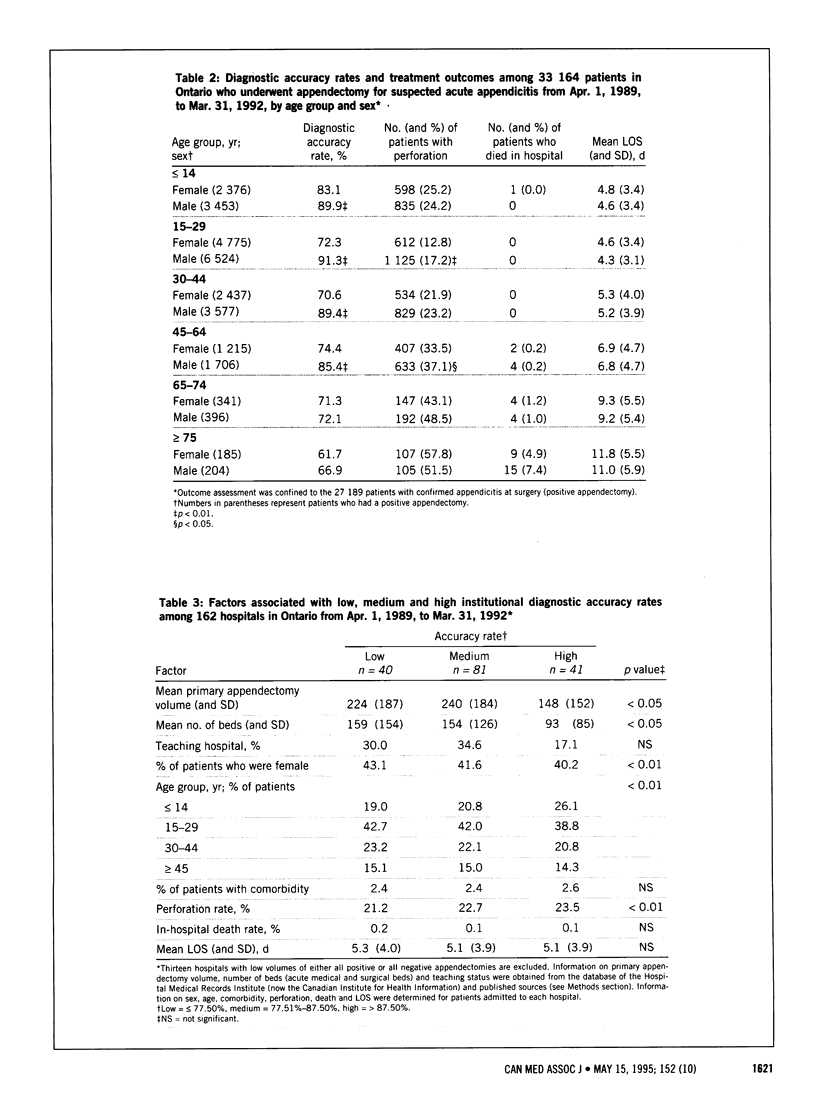
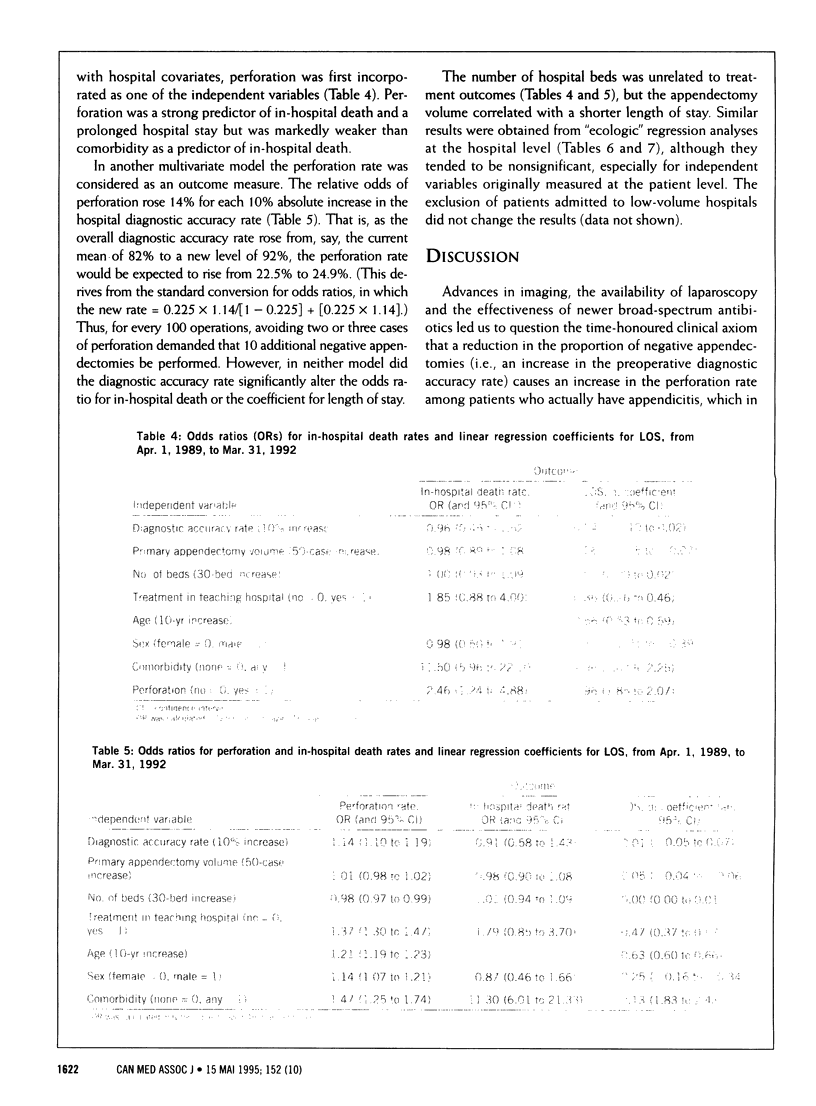
OBJECTIVE: To test the hypothesis that, with modern diagnostic methods and antibiotics, more conservative use of surgery in cases of suspected appendicitis would not result in increased rates of short-term complications in confirmed cases. DESIGN: Population-based observational study using administrative data. SETTING: All Ontario hospitals in which primary appendectomy was performed from Apr. 1, 1981, to Mar. 31, 1992. PATIENTS: All 126,815 patients admitted to hospital for a primary appendectomy during the study period. OUTCOME MEASURES: Diagnostic accuracy rate (acute appendicitis as the primary diagnosis), perforation rate, in-hospital death rate and length of stay. RESULTS: The diagnostic accuracy rate among the male patients was stable throughout the decade; among the female patients it rose significantly, from 71.7% in 1981 to 75.3% in 1991 (p < 0.01). The perforation rates increased significantly among both the female and male patients (p < 0.01), whereas the mean length of stay decreased (p < 0.05). Despite sex-related differences in the accuracy rates, the male and female patients had similar in-hospital death rates and mean lengths of stay. The institutional diagnostic accuracy rates, as determined from data for 1989-90 to 1991-92, ranged from 50.0% to 96.7%. Multivariate analyses of 27,189 confirmed cases of appendicitis at 175 hospitals revealed that perforation was a strong predictor of in-hospital death (odds ratio [OR] 2.46, 95% confidence interval [CI] 1.24 to 4.88), but comorbidity was the strongest predictor (OR 11.50, 95% CI 5.96 to 22.10). For each 10% increase in the diagnostic accuracy rate, the perforation rate increased 14% (OR 1.14, 95% CI 1.10 to 1.19), but the accuracy rate was not significantly related to the in-hospital death rate or the length of stay. CONCLUSION: A higher diagnostic accuracy rate is associated with more perforated appendixes. Although perforation itself leads to adverse outcomes, a higher accuracy rate does not. This suggests that hospitals with higher accuracy rates incur more perforations, but, with close observation, timely laparotomy and the use of modern antibiotics, these patients have favourable outcomes. This contrasts with adverse effects of perforation among patients at high risk for perforation (especially very young children and elderly people) in centres at all accuracy levels. The variation in hospitals' diagnostic accuracy rates suggests that some proportion of appendectomies could be safely avoided.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adams I. D., Chan M., Clifford P. C., Cooke W. M., Dallos V., de Dombal F. T., Edwards M. H., Hancock D. M., Hewett D. J., McIntyre N. Computer aided diagnosis of acute abdominal pain: a multicentre study. Br Med J (Clin Res Ed) 1986 Sep 27;293(6550):800–804. doi: 10.1136/bmj.293.6550.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addiss D. G., Shaffer N., Fowler B. S., Tauxe R. V. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990 Nov;132(5):910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- Andersson R. E., Hugander A., Thulin A. J. Diagnostic accuracy and perforation rate in appendicitis: association with age and sex of the patient and with appendicectomy rate. Eur J Surg. 1992 Jan;158(1):37–41. [PubMed] [Google Scholar]
- Chang F. C., Hogle H. H., Welling D. R. The fate of the negative appendix. Am J Surg. 1973 Dec;126(6):752–754. doi: 10.1016/s0002-9610(73)80063-7. [DOI] [PubMed] [Google Scholar]
- Charlson M. E., Pompei P., Ales K. L., MacKenzie C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Chen E., Naylor C. D. Variation in hospital length of stay for acute myocardial infarction in Ontario, Canada. Med Care. 1994 May;32(5):420–435. doi: 10.1097/00005650-199405000-00002. [DOI] [PubMed] [Google Scholar]
- Detmer D. E., Frisch C. Improved results in acute appendicitis care following areawide review. Med Decis Making. 1984;4(2):217–227. doi: 10.1177/0272989X8400400209. [DOI] [PubMed] [Google Scholar]
- Deyo R. A., Cherkin D. C., Ciol M. A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992 Jun;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Dunn E. L., Moore E. E., Elerding S. C., Murphy J. R. The unnecessary laparotomy for appendicitis-can it be decreased? Am Surg. 1982 Jul;48(7):320–323. [PubMed] [Google Scholar]
- Hannan E. L., Kilburn H., Jr, O'Donnell J. F., Bernard H. R., Shields E. P., Lindsey M. L., Yazici A. A longitudinal analysis of the relationship between in-hospital mortality in New York State and the volume of abdominal aortic aneurysm surgeries performed. Health Serv Res. 1992 Oct;27(4):517–542. [PMC free article] [PubMed] [Google Scholar]
- Jadallah F. A., Abdul-Ghani A. A., Tibblin S. Diagnostic laparoscopy reduces unnecessary appendicectomy in fertile women. Eur J Surg. 1994 Jan;160(1):41–45. [PubMed] [Google Scholar]
- Koepsell T. D., Inui T. S., Farewell V. T. Factors affecting perforation in acute appendicitis. Surg Gynecol Obstet. 1981 Oct;153(4):508–510. [PubMed] [Google Scholar]
- Luckmann R. Incidence and case fatality rates for acute appendicitis in California. A population-based study of the effects of age. Am J Epidemiol. 1989 May;129(5):905–918. doi: 10.1093/oxfordjournals.aje.a115224. [DOI] [PubMed] [Google Scholar]
- McLean A. D., Stonebridge P. A., Bradbury A. W., Rainey J. B., Macleod D. A. Time of presentation, time of operation, and unnecessary appendicectomy. BMJ. 1993 Jan 30;306(6873):307–307. doi: 10.1136/bmj.306.6873.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller B. A., Daling J. R., Moore D. E., Weiss N. S., Spadoni L. R., Stadel B. V., Soules M. R. Appendectomy and the risk of tubal infertility. N Engl J Med. 1986 Dec 11;315(24):1506–1508. doi: 10.1056/NEJM198612113152402. [DOI] [PubMed] [Google Scholar]
- Olsen J. B., Myrén C. J., Haahr P. E. Randomized study of the value of laparoscopy before appendicectomy. Br J Surg. 1993 Jul;80(7):922–923. doi: 10.1002/bjs.1800800744. [DOI] [PubMed] [Google Scholar]
- Velanovich V., Satava R. Balancing the normal appendectomy rate with the perforated appendicitis rate: implications for quality assurance. Am Surg. 1992 Apr;58(4):264–269. [PubMed] [Google Scholar]
- White J. J., Santillana M., Haller J. A., Jr Intensive in-hospital observation: a safe way to decrease unnecessary appendectomy. Am Surg. 1975 Dec;41(12):793–798. [PubMed] [Google Scholar]
- Zeger S. L., Liang K. Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986 Mar;42(1):121–130. [PubMed] [Google Scholar]


