Abstract
Marginal-zone (MZ) B cells represent a first line of defense against particulate blood-borne antigens. Together with the B1 cells, they are responsible for the early response against type II T-independent antigens. The molecular pathways controlling the development of MZ B cells are only poorly understood. We found that these cells are virtually absent in mice deficient in the BOB.1/OBF.1 coactivator. Loss of these B cells was demonstrated by the lack of cells showing the appropriate cell surface phenotype but also by histological analyses and tri-nitro-phenol-Ficoll capturing. The lack of these cells is a B-cell-intrinsic defect, as shown by bone marrow complementation experiments. We also show that the expression of BOB.1/OBF.1 in peripheral B cells is required for the development of MZ B lymphocytes. Our analysis of BOB.1/OBF.1-deficient splenic B cells reveals alterations in cell motility, tumor necrosis factor receptor expression, and B-cell receptor (BCR) signaling. These changes could contribute to the loss of MZ B lymphocytes by altering the maturation of the cells. Interestingly, development of and BCR signaling in B1 B cells are completely normal in BOB.1/OBF.1 mutant mice.
Three sets of peripheral effector B lymphocytes have been described. B1 cells are largely confined to the peritoneal cavities. Conventional B cells, also called recirculating follicular B cells or B2 cells, are present in the secondary lymphoid organs like the spleen, lymph nodes, and tonsils, and they also recirculate in the blood. A third kind of effector B cells are the marginal-zone (MZ) B cells. MZ B cells are specifically present in the region surrounding the marginal sinuses of the lymphoid follicles in the spleen (27, 38, 41). Because of their special location, they are involved in filtering of the blood on its way from the arterial sinuses to the venous sinuses. They therefore have immediate contact with blood-borne antigens, and recent experiments suggest that they are involved in the mounting of a primary immune response against such blood-borne antigens, in particular, particulate antigens (42).
Several other features also characterize MZ B cells in addition to their specific location. They express high levels of immunoglobulin M (IgM) and low levels of IgD on their surface, and they are CD21high, CD1high, and CD23low (3, 40). Like B1 B cells, they appear to be poised and, as a consequence, react rapidly upon antigen encounter (47, 48). They share a second similarity with B1 B lymphocytes; namely, they prefer to react against simple microbial antigens (42). MZ B cells have received some attention recently because their development is affected by a variety of mutations (9, 10, 17, 21, 56, 66). Although there is still no common picture emerging of how the development of this cell lineage is regulated, it is likely that signals from a variety of receptors are involved. A simple model of B-cell development proposes that strong B-cell receptor (BCR) signals favor the development of B1 B lymphocytes, intermediate-strength signals result in B2 B-cell development, and weak signals favor the development of MZ B lymphocytes (10).
BOB.1/OBF.1 (other names are Bob1, OBF1, and OCA-B) is a transcriptional coactivator specifically expressed in lymphocytes (20, 36, 62). This coactivator specifically interacts with the POU domain of the Oct1 and Oct2 transcription factors present in B and T cells (11, 12, 19). Expression of BOB.1/OBF.1 is constitutive in B lymphocytes, albeit at variable levels, and can be induced in T cells upon coactivation (18, 53, 57, 58, 61, 71). BOB.1/OBF.1 seems to play a critical role in mediating the transcriptional activity of the Oct1 and Oct2 transcription factors (31, 34, 35, 49, 51).
A mutation of BOB.1/OBF.1 in the mouse germ line resulted in various defects in the B-lymphocyte lineage. The most striking defect is the complete absence of germinal-center formation (24, 46, 61). As a consequence, these mice are highly susceptible to various infections because they are unable to mount a strong secondary immune response (14, 24, 46, 61). In addition to the defects in germinal-center development, BOB.1/OBF.1-deficient animals also show defects in earlier stages of B-cell development, most notably, at the stage of transitional B lymphocytes that have completed the bone marrow phase of development and are on the way to the periphery (22). Interestingly, development of the B1 B-cell lineage is normal in these mutant mice (46).
When primary immune responses against various types of antigens were analyzed in BOB.1/OBF.1-deficient mice, a defect in the response to type II T-cell-independent antigens was observed, especially at earlier stages of immunization (61). Given that recent data suggest that this response is, to a large extent, mediated by the MZ B cells in combination with the B1 lineage (38), we analyzed whether MZ B-cell development is effected in BOB.1/OBF.1-deficient mice. In contrast to an earlier report that briefly stated that development of MZ B cells is normal in BOB.1/OBF.1-deficient mice (53), we found that, in our mice, development or survival of MZ B cells is dramatically reduced. BOB.1/OBF.1-deficient splenic B cells show alterations in signaling and motility that could interfere with the production of MZ B cells.
MATERIALS AND METHODS
Mice.
C57BL/6 wild-type and BOB.1/OBF.1-deficient mice on the same genetic background were obtained from our breeding facility. The transgenic mice used in this study, expressing the tetracycline-regulated transactivator (tTA) under the control of the intronic μ heavy-chain enhancer (μE) and a minimal promoter or expressing transgenic BOB.1/OBF.1 and a luciferase reporter gene under the control of a bidirectional tetracycline operator sequence (tetO), were previously described (22). Mice were analyzed 8 to 10 weeks after birth. All animal studies were approved by an institutional review board.
Fluorescence-activated cell sorter (FACS) analysis.
Single-cell suspensions of Lympholyte-M (Cedarlane Laboratories Ltd., Hornby, Ontario, Canada)-purified splenocytes (5 × 105) were incubated for 30 min at 4°C with different combinations (as indicated in Results) of the following antibodies: anti-B220-biotin, anti-CD21-fluorescein isothiocyanate (FITC), anti-CD23-phycoerythrin (PE), anti-IgM-PE, anti-IgD-biotin, anti-CD1-FITC, anti-B220-PerCP and anti-tri-nitro-phenol-biotin (all produced by Pharmingen, San Diego, Calif.). Stainings were performed in phosphate-buffered saline (PBS) containing 0.1% bovine serum albumin (BSA; Roche Diagnostics, Mannheim, Germany), 0.1% Na-azide, and a saturating concentration of anti-CD16/CD32 (Pharmingen) to block Fcγ III/II receptors. Biotin-labeled antibodies were revealed by streptavidin-Cy-Chrom (Pharmingen) or, in four-color analyses, by streptavidin-allophycocyanin (Pharmingen). Cell surface marker expression was analyzed by using a four-color flow cytometer (FACScalibur) and Cell Quest software (Becton Dickinson, Heidelberg, Germany). Antibodies used for sorting of splenic follicular and MZ B cells were anti-B220-biotin, anti-CD21-FITC, and anti-CD23-PE. Cells were sorted with a FACSORT plus cytometer (Becton Dickinson).
TNP-Ficoll treatment.
Ten-week-old wild-type and BOB.1/OBF.1−/− mice were injected intravenously with 100 μg of TNP-Ficoll (Biosearch Technologies, Inc.) dissolved in 500 μl of PBS. Control animals received the same amount of PBS only. Thirty minutes after injection, mice were sacrificed and spleens were isolated. One-half of the spleen was used for histological examinations, while the other half was used for FACS analysis.
Histological analysis.
Spleens were embedded in Tissue-Tek O.C.T. compound (Sakura), snap-frozen in liquid nitrogen, and stored at −80°C. Cryostat sections of 4 μm were prepared, air dried, and fixed in acetone (10 min at room temperature). Slides were incubated for 45 min with staining buffer (PBS containing 0.1% BSA, 0.1% Na-azide, and anti-CD16/CD32) and then stained for 45 min with a 1:100 dilution of both anti-IgM-PE (Pharmingen) and MOMA-1-FITC (Serotec) or IgM-PE and IgD-FITC antibodies (both from Pharmingen). Sections from TNP-Ficoll-treated animals were stained with a combination of anti-TNP-biotin (Pharmingen) and anti-MOMA-1-FITC antibodies. Biotinylated antibodies were revealed with streptavidin-Cy-Chrom (Pharmingen). Slides were mounted in Mowiol containing the nucleic acid-specific fluorescent dye 4′,6′-diamidino-2-phenylindole (DAPI; 0.1 μg/ml; Roche).
For analysis of BOB.1/OBF.1 protein expression in the spleen, sections were fixed with 4% paraformaldehyde in PBS and permeabilized with 1% Triton X-100. Afterward, samples were stained with rabbit anti-mouse BOB.1/OBF.1 antibody, raised against the N terminus, and then stained with donkey anti-rabbit horseradish peroxidase-conjugated antibody (Santa Cruz). Binding of horseradish peroxidase-labeled antibody was revealed with 3-amino-9-ethylcarbazo compound.
All slides were analyzed with a Leica microscope (DMIRB/E) and OpenLab software (version 2.2.5). The excitation wavelength for FITC was 494 nm, that for PE was 576 nm, that for Cy-Chrom was 581 nm, and that for DAPI was 359 nm.
Repopulation.
For the bone marrow reconstitution experiments, BOB.1/OBF.1−/− and wild-type donors, as well as μMT (26) recipients, on a BALB/c background were bred under specific-pathogen-free conditions at our institute. μMT mice were irradiated with 250 and then 200 rads (with a 3-h interval between irradiations). After a rest period of 18 to 20 h, the mice were injected intravenously with 2 × 106 bone marrow cells in the tail vein. The donor bone marrow cells were prepared by pooling total cells isolated from both femurs of a donor and then treated with 2 ml of Gey's hypotonic solution for 5 min at 4°C. Cells were than centrifuged through a 1-ml 100% fetal calf serum cushion, washed twice with PBS, and counted. Two separate wild-type and BOB.1/OBF.1-deficient donor mice each were used to inject three recipients each. At day 32 after repopulation, the animals were sacrificed and the spleen, peritoneum, and bone marrow were harvested for FACS and histological analyses.
Migration assay.
Lympholyte-M-purified splenocytes (106) and peritoneal lavage cells were assayed for transmigration with 5-μm-pore-size Transwell culture inserts (Costar). The medium used for the experiments was RPMI 1640 medium (Gibco) supplemented with 0.25% of bovine serum albumin (Sigma). To assay chemotaxis, the bottom chambers were filled with 1 μg of MIP-3β per ml, 0.5 μg of BLC per ml, or 0.1 μg of SDF-1α per ml (all were from R&D). The migration occurred at 37°C in a humidified atmosphere with 5% CO2 over 4 h. After incubation, cells that had migrated to the lower chamber were harvested, stained with anti-B220-PerCP (Pharmingen), and counted by FACScalibur and analyzed by CellQuest software.
Calcium influx measurement.
Peritoneal exudate cells obtained by conventional methods and Lympholyte-M-separated splenocytes from both wild-type and BOB.1/OBF.1−/− animals were incubated with 4 μg of Fluo-3-AM per ml and 10 μg of FuraRed per ml (both were from Molecular Probes) in RPMI 1640 medium for 45 min at 37°C. Thereafter, the cells were washed thoroughly and stained with anti-B220-PE and anti-heat-stable antigen (HAS) (splenocytes) or anti-B220-PE and anti-Mac-1-biotin antibodies (peritoneal cells). After washing, cells were resuspended at 106/ml of RPMI medium. After a 15-min incubation at 37°C, cells were stimulated with 30 μg of anti-IgM-F(ab′)2 (Jackson ImmunoResearch) per ml and the resultant variation in intracellular Ca2+ was monitored by flow cytometry. Data were analyzed with FlowJo software.
Analysis of mRNA expression levels.
For analysis of chemokine receptor mRNA expression, total RNA isolated from wild-type and BOB.1/OBF.1−/− splenocytes, peritoneal cells, and cultivated pre-B cells of both genotypes was used. Pre-B-cell lines were established by culturing bone marrow cells from mice of the indicated genotype under the stimulatory influence of irradiated adherent stromal ST2 cells and interleukin-7. The culture medium used was IMDM (PAN) supplemented with 2% fetal calf serum, antibiotics (penicillin and streptomycin), 50 μM β-mercaptoethanol, and 2% supernatant from an interleukin-7-producing J558 transfectant. Expression of BOB.1/OBF.1 RNA was investigated in FACSortplus-sorted follicular (B220pos CD21med CD23high) and MZ (B220pos CD21high CD23low/neg) wild-type splenocytes. RNA was isolated with a High Pure RNA isolation kit (Roche) and reverse transcribed with Moloney murine leukemia virus reverse transcriptase (Promega) and random hexamer primers. For reverse transcription (RT)-PCR, the PCR primers used were BOB.1/OBF.1 (5′-CAA GCT CCT GCC CCA CCA AGG-3′ and 5′-GAG GTT GAT ACT GCA GGC TGG AGG TG-3′), BAFFR (5′-GCA ATC AGA CCG AGT GCT TCG-3′ and 5′-CTA TTG CTC TGG GCC AGC TGT-3′), BCMA (5′-TCT TTC AGT GAT CCA GTC CC-3′ and 5′-CAC TTT GCA AAG CAG TTG GC-3′), TACI (5′-ATG GCT ATG GCA TTC TGC CC-3′ and 5′-TCA GAT CCC TGG TGC CTT CC-3′), LT-α (5′-ATG ACA CTG CTC GGC CGT CT-3′ and 5′-CCC TTA CTG AGC AGG AAC AC-3′), and β-actin (5′-GGT CAG AAG GAC TCC TAT GTG-3′ and 5′-AGA GCA ACA TAG CAC AGC TTC-3′).
Quantification of the BAFFR mRNA expression level in the pre-B cells was performed by real-time PCR. The PCR was performed in a Roche LightCycler with the LightCycler-FastStart DNA Master SYBR Green I system (Roche). The cDNAs were serially diluted (4:2:1) to check the efficiency of the PCR. Each PCR was performed with each dilution at least three times. Porphobilinogen deaminase (PBGD) primers (5′-CAG ACC GAC ACT GTG GTG GC-3′ and 5′-CTT CCG AAG GCG GGT GTT GAG-3′) were used as a control for a housekeeping gene. Calculations were performed with the LightCycler software, version 3.39. Quantification was performed relative to the expression levels of wild-type cells (7).
Western blot.
Sorted MZ and follicular B cells from wild-type mice were lysed with RIPA buffer (50 mM Tris-HCl [pH 8], 150 mM NaCl, 0.1% sodium dodecyl sulfate, 0.5% deoxycholic acid, 1% NP-40 with 1 mM dithiothreitol and 1 mM phenylmethylsulfonyl fluoride), and the proteins were separated on sodium dodecyl sulfate-12.5% polyacrylamide gels. Antibodies used for Western blot assays were polyclonal anti-BOB.1/OBF.1 (50) and anti-RelA (Santa Cruz).
In vitro stimulation of B cells.
B cells were enriched from spleens of wild-type and BOB.1/OBF.1-deficient mice by incubation of Gey's-treated splenocytes with anti-CD43 antibodies coupled to paramagnetic beads (MACS; Miltenyi Biotech, Cologne, Germany) as recommended by the supplier. The nonbound cells were then stimulated by incubation with 27 μg of goat anti-mouse IgM per ml for the times indicated. Cells were then harvested, and whole-cell extracts were made and analyzed for tyrosine phosphorylation as previously described (67).
For electrophoretic mobility shift assays, wild-type and BOB.1/OBF.1−/− splenocytes and peritoneal cells were incubated for 2 h in the presence or absence of 30 μg of anti-IgM-F(ab)2 per ml. Afterward, cells were lysed with Dignam C buffer (20 mM HEPES [pH 7.9], 0.42 M NaCl, 1.5 mM MgCl, 0.2 mM EDTA, 25% glycerol, 1 mM dithiothreitol, 1 mM phenylmethylsulfonyl fluoride), and the protein concentrations were determined with the Bradford reagent. The electrophoretic mobility shift assay with NF-κB was performed as described before (32) with 5 μg of total protein extracts.
RESULTS
Reduced numbers of MZ B cells in BOB.1/OBF.1−/− mice.
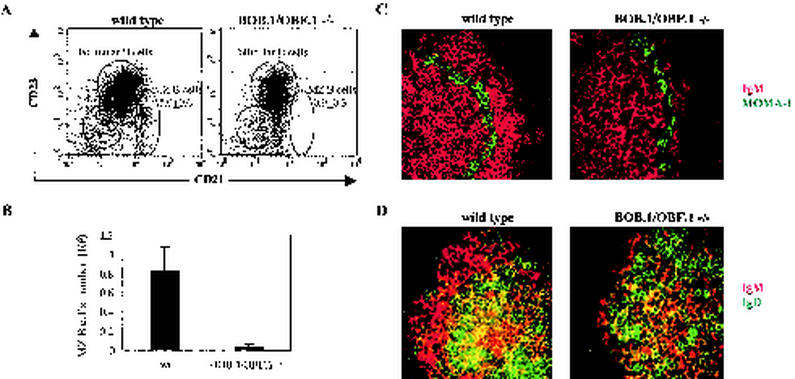
In order to investigate whether BOB.1/OBF.1 deficiency affects the size of the MZ B-cell compartment, we performed a flow cytometry analysis of splenocytes isolated from wild-type and BOB.1/OBF.1−/− mice. As previously reported (40), analysis of CD21 and CD23 expression among B cells (B220/CD45R+) allowed us to discriminate between newly formed (CD21neg CD23neg), follicular (CD21med CD23high), and MZ (CD21high CD23low/neg) B cells (Fig. 1A). Consistent with previous data, BOB.1/OBF.1−/− mice showed a reduced number of total B cells (46, 61). However, while the reduction in the total number of B cells was in the range of two to threefold, we observed a much more pronounced reduction in the number of MZ B cells. In wild-type mice, about 5% of the total splenic B cells had an MZ B-cell phenotype (CD21high CD23low/neg). In contrast, the proportion of cells with this cell surface phenotype was below 1% in BOB.1/OBF.1-deficient mice (Fig. 1A). Analysis of absolute cell numbers showed that MZ B cells in BOB.1/OBF.1−/− mice were reduced by about 20-fold (Fig. 1B). This reduction of the MZ B-cell population was further confirmed by the absence of CD21high and CD1high cells within the IgMhigh IgDlow population in BOB.1/OBF.1−/− animals (data not shown). The lack of CD1high cells excludes the possibility that these results were just a consequence of a specific reduction of CD21 expression in BOB.1/OBF.1−/− MZ B cells.
FIG. 1.
The MZ B-cell compartment is reduced in BOB.1/OBF.1−/− mice. (A) Splenocytes isolated from wild-type (wt) and BOB.1/OBF.1−/− mice were stained with a combination of anti-B220, anti-CD21, and anti-CD23 antibodies. Within the B220pos cell gate, MZ, follicular (FO), and newly formed (NF) B cells are indicated. Mean percentages of MZ B cells (with standard deviations) in 20 analyzed animals of both genotypes are given. (B) Absolute numbers of MZ B cells in wild-type and BOB.1/OBF.1−/− mice obtained by analysis of five animals of both genotypes are given. Data are presented as the mean plus the standard deviation. Spleen sections from wild-type and BOB.1/OBF.1-deficient mice were stained with a combination of PE-labeled anti-IgM (red) and FITC-labeled anti-MOMA-1 (green) antibodies (C) or anti-IgM-PE (red) and anti-IgD-FITC (green) antibodies (D). Representative results obtained with spleen sections of 10 animals of both genotypes are shown. Sections were viewed at an original magnification of ×400.
We performed a histological examination of spleens from wild-type and BOB.1/OBF.1−/− mice to examine whether there were B cells present in the MZ. We used the MOMA-1 antibody, a specific marker for metallophilic macrophages (28), to visualize the border between the follicle and the MZ. Spleen sections from wild-type mice clearly show IgM-positive cells outside of the metallophilic (MOMA-1+) macrophage rim (MZ) (Fig. 1C). However, such IgM-positive cells were virtually absent from this splenic region in BOB.1/OBF.1-deficient mice (Fig. 1C). We also stained spleen sections of wild-type and BOB.1/OBF.1−/− mice with a combination of anti-IgM and anti-IgD antibodies. Staining of wild-type spleens showed the presence of cells positive for both IgM and IgD (follicular B cells) surrounded by only IgM-positive MZ B cells (Fig. 1D). In concordance with the results obtained in the IgM/MOMA-1 stainings, rims of IgM single-positive cells were almost completely absent in spleen sections of BOB.1/OBF.1−/− mice (Fig. 1D).
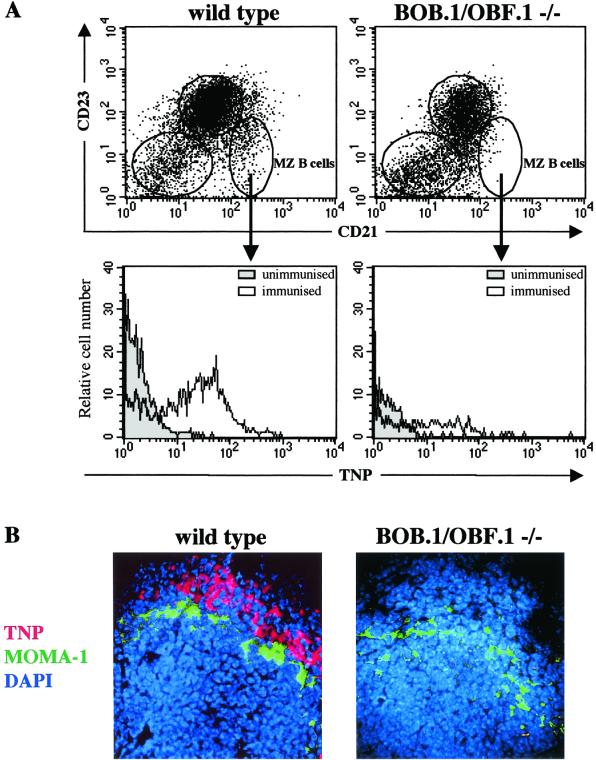
TNP-Ficoll capturing is reduced in BOB.1/OBF.1−/− mice.
It has been shown that intravenously injected TNP-Ficoll is initially recognized and captured by MZ B cells but not by follicular B cells (9, 21, 30). In order to check for the presence of functional MZ B cells in the spleen, wild-type and BOB.1/OBF.1−/− mice were injected intravenously with TNP-Ficoll and then analyzed 30 min later for the presence of antigen in the spleen with an anti-TNP antibody. In wild-type animals, TNP-Ficoll capturing was detected in the gate of CD21high CD23low B cells (MZ B cells) (Fig. 2A) but not in the gate of follicular and newly formed B cells (data not shown). Histological analysis also showed binding of anti-TNP antibody in the MZ, outside the rim of metallophilic macrophages (Fig. 2B). In contrast, both flow cytometric and histological analyses revealed that in BOB.1/OBF.1−/− mice, almost no TNP-Ficoll-capturing cells were present in the MZ, confirming the absence of functional MZ B cells in BOB.1/OBF.1-deficient animals (Fig. 2).
FIG. 2.
T-cell-independent type II antigen capturing in wild-type and BOB.1/OBF.1−/− mice. (A) Splenocytes from TNP-Ficoll-immunized wild-type and BOB.1/OBF.1−/− mice were stained with a combination of anti-B220, anti-CD21, anti-CD23, and anti-TNP antibodies. MZ B cells (B220pos CD21high CD23low) were gated, and histograms presenting anti-TNP staining of immunized and unimmunized animals are shown. The data shown are representative of three sets of experiments. (B) Spleen sections from TNP-Ficoll-immunized animals were stained with biotin-labeled anti-TNP (red) and FITC-labeled anti-MOMA-1 (green) antibodies. Sections were mounted with Mowiol containing the DNA-specific fluorescent dye DAPI (blue), which stained all nucleated cells. Magnification, ×400.
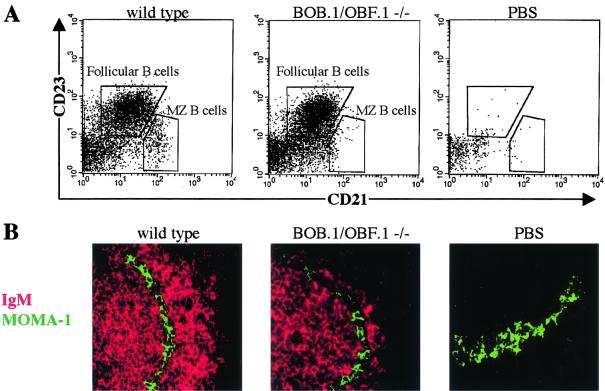
The lack of MZ B cells in BOB.1/OBF.1-deficient mice is due to an intrinsic defect in the B-cell lineage.
To investigate whether the lack of MZ B cells in BOB.1/OBF.1-deficient mice is due to an intrinsic defect in the B-cell lineage, bone marrow reconstitution experiments were performed. Sublethally irradiated μMT mice were used as recipients for intravenous injections of total bone marrow isolated from either wild-type or BOB.1/OBF.1-deficient donors. μMT mice lack B cells but otherwise show normal traits, including normal numbers of T cells (25). Injections of wild-type bone marrow resulted in the generation of both follicular and MZ B cells (Fig. 3A and B). BOB.1/OBF.1-deficient mouse-derived bone marrow gave rise to follicular but not MZ B cells (Fig. 3A and B). Control μMT recipients injected with PBS lacked IgM-positive cells in the spleen. We also investigated the overall MZ architecture for the presence of reticular fibroblasts and MZ macrophages. We found that the BOB.1/OBF.1 deficiency affects neither the general splenic MZ architecture nor the distribution of MZ macrophages (data not shown). Together, these data strongly suggest that the lack of MZ B cells in BOB.1/OBF.1−/− mice is due to the lack of BOB.1/OBF.1 in the B cells themselves.
FIG. 3.
Lack of MZ B cells in BOB.1/OBF.1-deficient mice is due to an intrinsic defect in the B-cell lineage. (A) Wild-type and BOB.1/OBF.1−/− bone marrow cells were injected into μMT mice. Control mice were injected with PBS. After 32 days of repopulation, spleens were analyzed for the presence of CD21high CD23low (MZ) B cells. (B) One part of the spleen was used for histological examinations. Sections were stained with anti-IgM-PE and anti-MOMA-1-FITC antibodies.
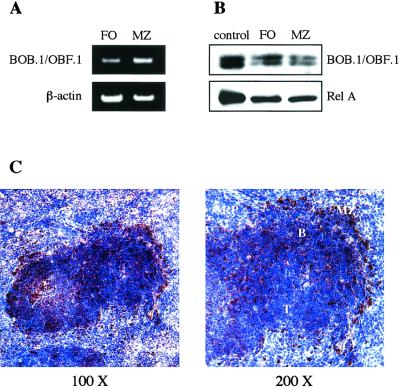
BOB.1/OBF.1 is expressed in MZ B cells.
From earlier studies, it was known that germinal center B cells, which are also lacking in BOB.1/OBF.1-deficient mice, express high levels of the BOB.1/OBF.1 protein (18). Therefore, we analyzed whether the BOB.1/OBF.1 protein is expressed in MZ B cells and, if so, to what extent. We sorted MZ and follicular B cells from wild-type mice and analyzed both mRNA and protein levels. BOB.1/OBF.1 mRNA was present in both follicular and MZ B cells. mRNA expression levels appeared slightly higher in MZ B cells (Fig. 4A). Western blots also showed the presence of virtually identical BOB.1/OBF.1 protein levels in both B-cell subpopulations (Fig. 4B). Furthermore, histological analysis of spleen sections showed the binding of a BOB.1/OBF.1-specific antibody to B cells on both sides of the marginal sinus (Fig. 4C). These results show that BOB.1/OBF.1 is expressed in MZ B cells and that the expression level is comparable to that in follicular B cells.
FIG. 4.
BOB.1/OBF.1 is expressed in MZ B cells. Wild-type splenic B cells were sorted on the basis of the expression of CD21 and CD23 to follicular (FO) (CD21med CD23high) and MZ (CD21high CD23low/neg) B cells. (A) Total RNA was isolated, and RT-PCR with primers specific for BOB.1/OBF.1 and β-actin was performed. (B) Western blot analysis of whole-cell extracts was performed with antibodies specific for the BOB.1/OBF.1 and RelA proteins. As a positive control, a whole-cell extract of PD31 cells was used. (C) Wild-type spleen sections were stained with anti-BOB.1/OBF.1 antibody (brown), counterstained with hematoxylin, and viewed at original magnifications of ×100 and ×200. B- and T-cell zones (B and T, respectively) and red pulp (RP) are indicated.
MZ B-cell development is dependent on BOB.1/OBF.1 expression in the spleen.
We recently demonstrated that BOB.1/OBF.1-deficient B cells exhibit defects in the early developmental stages in the bone marrow (22). We were therefore interested in determining whether the observed defect in MZ B cells might be a consequence of problems acquired during bone marrow differentiation. We have established a double-transgenic rescue system for BOB.1/OBF.1 deficiency in the bone marrow (22). The first line (μE-tTA) contains a transgene that encodes a tetracycline-regulated transactivator (tTA) under the control of the intronic μ heavy-chain enhancer (μE) and a minimal promoter. The second line (tetO-BOB.1/OBF.1) contains a bidirectional tetracycline operator sequence (tetO) that simultaneously regulates the expression of transgenic BOB.1/OBF.1 and a luciferase reporter gene. This system allows us to reconstitute normal early B-cell development in the bone marrow while maintaining a lack of BOB.1/OBF.1 expression in the periphery (22). We performed FACS and histological analyses of the MZ B-cell compartment in the spleens of these mice. Expression of the BOB.1/OBF.1 protein in bone marrow but not in the spleen was not sufficient to rescue the MZ B-cell number in BOB.1/OBF.1−/− animals (Fig. 5), suggesting that BOB.1/OBF.1 protein expression in the spleen is necessary for MZ B-cell development.
FIG. 5.
Expression of BOB.1/OBF.1 limited to bone marrow does not rescue MZ B-cell development. Mice expressing a tetracycline-regulated transactivator (tTA) under the control of the intronic μ heavy-chain enhancer (μE) and a minimal promoter and BOB.1/OBF.1 under the control of a bidirectional tetracycline operator sequence (tetO) were crossed with BOB.1/OBF.1−/− or BOB.1/OBF.1+/− mice in order to obtain expression of the BOB.1/OBF.1 transgene on a BOB.1/OBF.1−/− background. (A) Splenocytes from double-transgenic (dtg) BOB.1/OBF.1+/−, single-transgenic (stg) BOB.1/OBF.1−/−, and double-transgenic BOB.1/OBF.1−/− animals were stained with anti-B220, anti-CD21, and anti-CD23 antibodies. Representative CD21/CD23 stainings of B220-positive cells and mean percentages of MZ B-cell numbers are shown. (B) Splenic cryosections from the same mice were stained with anti-IgM-PE (red) and anti-MOMA-1-FITC (green) antibodies and viewed at a magnification of ×400.
BOB.1/OBF.1−/− B cells show altered migration properties.
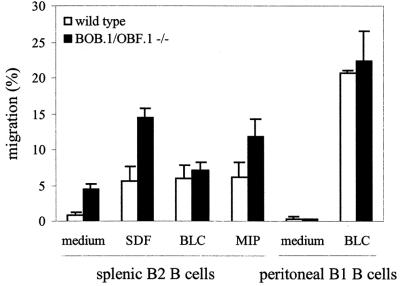
It has been suggested that proper migration and compartmentalization of B cells are critical for the development of MZ B cells (4, 5, 8, 17, 21, 23, 66). We therefore compared the migration properties of splenocytes isolated from wild-type and BOB.1/OBF.1−/− mice in an in vitro migration system. The basal migration level (in the absence of stimulation) was significantly higher for BOB.1/OBF.1−/− than for wild-type B cells (Fig. 6). We also compared the migration of BOB.1/OBF.1−/− and wild-type B cells stimulated with SDF-1α, MIP-3β, or BLC. Increased motility of BOB.1/OBF.1−/− B cells was also seen in the gradients of SDF-1α and MIP-3β (Fig. 6). In contrast, whereas BLC strongly induced migration of wild-type B cells, migration of BOB.1/OBF.1-deficient B cells toward this chemokine was not significantly induced over the basal level (Fig. 6). The weak response of BOB.1/OBF.1−/− B cells to BLC is most likely due to the fact that B cells from BOB.1/OBF.1−/− mice show reduced BLC receptor surface expression (reference 68 and our unpublished data). Since the BLC receptor plays an important role in the development and compartmentalization of B cells (15), this could indicate that hyporesponsiveness to BLC might contribute to the defects in B-cell development in BOB.1/OBF.1−/− mice.
FIG. 6.
Altered migration of BOB.1/OBF.1−/− splenocytes. Migration of Lympholyte-M-purified splenocytes or peritoneal exudate cells (106) from wild-type and BOB.1/OBF.1−/− mice was analyzed. Cells placed in 5-μm-pore-size Transwell inserts were incubated for 4 h in a gradient of SDF-1α, BLC, or MIP-3β. After incubation, cells that had migrated were harvested, stained with an anti-B220 antibody or anti-B220 and anti-Mac-1 antibodies for peritoneal B1 cells, counted, and analyzed by flow cytometry. The data presented are mean percentages of B cells that migrated, which were obtained by analysis of six animals per group.
Since the number of B1 cells is normal or slightly increased in BOB.1/OBF.1-deficient mice (46), we also analyzed the migration of these cells. In peritoneal B1 B cells, basal motility, as well as the chemotactic response to BLC, appeared to be unaffected by a BOB.1/OBF.1 deficiency (Fig. 6).
Reduced BAFF receptor (BAFFR) mRNA expression in BOB.1/OBF.1−/− B cells.
Recently, it has been shown that BAFF, a B-cell activation factor from the tumor necrosis factor family, is an important factor for B-cell homeostasis (6, 64). BAFF is produced by cells of myeloid origin and is the ligand for three receptors, BAFFR (BlyS), BCMA, and TACI (63). Disruption of the BAFF-BAFFR system leads to a strong reduction of MZ B cells (59). We checked BAFFR mRNA expression in follicular and MZ B-cell populations and noticed that BAFFR mRNA was detectable in both B-cell types (Fig. 7A). Next, we compared the expression of mRNA for BAFFR in BOB.1/OBF.1−/− and wild-type mice and observed that the BAFFR mRNA level is reduced in the spleens of BOB.1/OBF.1-deficient mice (Fig. 7B). The difference in the BAFFR mRNA expression level between wild-type and BOB.1/OBF.1-deficient mice was already detectable at the pre-B-cell stage. The relative expression of BAFFR mRNA in cultured BOB.1/OBF.1−/− pre-B cells was roughly twofold lower than that in wild-type pre-B cells, and this reduction was confirmed by quantitative real-time RT-PCR (LightCycler) (Fig. 7C).
FIG. 7.
Impaired BAFFR mRNA expression in BOB.1/OBF.1−/− B cells. RT-PCRs for the indicated mRNA molecules were performed with total RNA samples from sorted wild-type (wt) follicular (FO) and MZ B cells (A), wild-type and BOB.1/OBF.1−/− splenocytes (B), and wild-type and BOB.1/OBF.1−/− cultivated pre-B cells (C). Additionally, LightCycler analysis of wild-type and BOB.1/OBF.1−/− cultivated pre-B-cell cDNA with was performed primers for BAFFR and PBGD. The BAFFR/PBGD ratio, relative to the expression levels of wild-type cells, is presented.
We also compared the mRNA expression of other BAFFRs in BOB.1/OBF.1−/− and wild-type mice. The expression of TACI mRNA was not significantly altered in the absence of BOB.1/OBF.1, while the BCMA mRNA level was reduced in the spleens of BOB.1/OBF.1-deficient mice (Fig. 7B). Interestingly, the BAFFR and BCMA mRNAs were also reduced in BOB.1/OBF.1−/− peritoneal B1 B cells (Fig. 7B).
Another member of the tumor necrosis factor family, lymphotoxin alpha (LT-α), was reported to be important for MZ B-cell compartmentalization and maintenance (33, 45). We therefore investigated whether the reduction of MZ B cells in BOB.1/OBF.1−/− mice correlates with a reduction in the LT-α mRNA level in BOB.1/OBF.1-deficient mice. LT-α mRNA in BOB.1/OBF.1−/− spleen tissue was not reduced compared with that in wild-type spleen tissue. If anything, the expression of LT-α may be slightly increased in BOB.1/OBF.1 mutant mice (Fig. 7B).
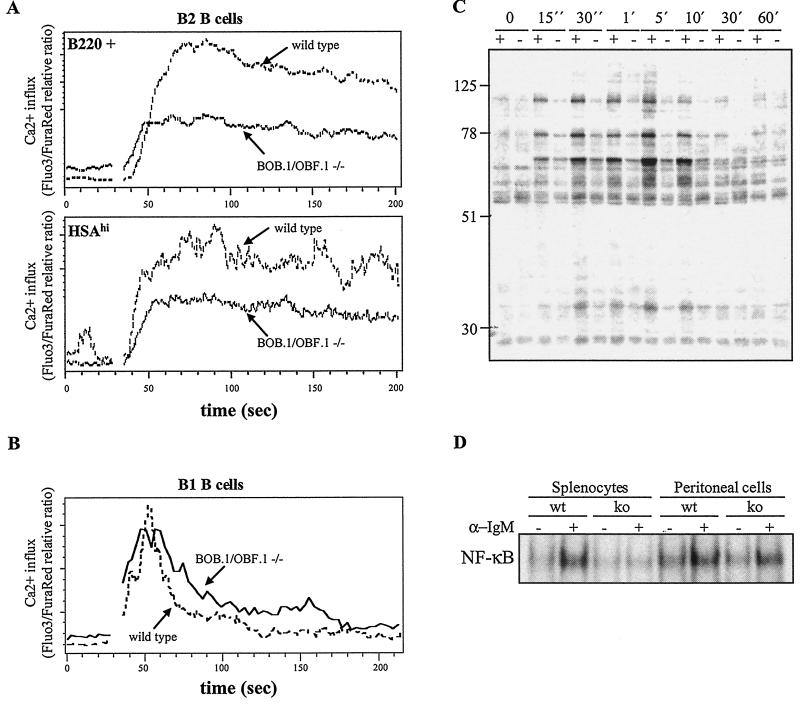
BOB.1/OBF.1−/− B cells show reduced BCR signaling.
Several recent papers suggest that MZ B-cell development is affected by the strength of the signal elicited at the B-cell receptor. According to this hypothesis, a weak signal favors development of MZ B cells while a strong signal favors development of follicular and B1 cells. Some of the support for this hypothesis is derived from the analysis of mouse mutants that show increased BCR signaling and a reduced MZ B-cell compartment (10, 21, 56). To test whether BOB.1/OBF.1−/− mice fit this theory, we monitored Ca2+ influx after IgM stimulation of splenic lymphocytes from wild-type and BOB.1/OBF.1−/− mice. Surprisingly, BOB.1/OBF.1-deficient B cells were much less responsive to BCR stimulation than were wild-type mice (Fig. 8A). The observed reduction of Ca2+ influx could not be simply attributed to the increased proportion of newly formed (HSAhigh) (1, 2) B cells in BOB.1/OBF.1−/− mice. Similar to the result obtained with total B220-positive cells, BCR-triggered Ca2+ influx into HSAhigh B cells from BOB.1/OBF.1−/− mice is reduced compared with that into wild-type HSAhigh B cells (Fig. 8A).
FIG. 8.
Effects of BOB.1/OBF.1 deficiency on BCR signaling in B2 and B1 B cells. Calcium influx after stimulation with anti-IgM F(ab)2 into wild-type and BOB.1/OBF.1−/− splenic total B cells (B220 positive) or newly formed B cells (B220 positive and HSAhigh) (A) and peritoneal B1 B cells (B220 and Mac-1 positive) (B) was monitored by flow cytometry. (C) Wild-type (+) and BOB.1/OBF.1−/− (−) splenic B cells were stimulated with anti-IgM F(ab)2 for the indicated times, and a Western blot assay with antiphosphotyrosine antibodies was performed. (D) Splenocytes and peritoneal cells isolated from wild-type (wt) and BOB.1/OBF.1 knockout (ko) mice were incubated for 2 h in the presence of anti-IgM F(ab)2, and an electrophoretic mobility shift assay with an NF-κB probe was performed. The data shown are representative of three independent experiments.
This result led us to explore in more detail the effect of BCR stimulation in splenocytes from BOB.1/OBF.1−/− mice. To do this, we enriched B cells from the spleens of BOB.1/OBF.1-deficient and wild-type mice by incubating the splenocytes with antibodies directed against CD43 and subsequently separating them with magnetic beads. Unbound cells, enriched for B cells, were then stimulated for various times with anti-IgM antibody, and whole-cell protein extracts were prepared for polyacrylamide gel electrophoresis, Western blotting, and reaction with antiphosphotyrosine antibodies. The pattern of phosphorylated substrates in stimulated, BOB.1/OBF.1-deficient splenic B cells was identical to the pattern obtained in wild-type cells (Fig. 8C). However, the response was much weaker and the time course was delayed in BOB.1/OBF.1-deficient cells. Concordant with this, IgM-stimulated NF-κB activation in BOB.1/OBF.1−/− splenocytes was significantly reduced (Fig. 8D).
These results demonstrate that the reduction of the MZ B-cell compartment in BOB.1/OBF.1−/− mice is not due to increased signal strength from the BCR. Thus, BOB.1/OBF.1-deficient mice do not fit the simple version of the above-mentioned hypothesis of MZ B-cell development.
B1-cell signaling is not reduced in BOB.1/OBF.1-deficient mice.
According to the signal strength hypothesis, B1 cells are believed to require strong BCR signals (10). We therefore investigated whether the reduced BCR signal strength is specific for follicular B cells or whether this reduction can also be observed in B1 B cells. We analyzed Ca2+ influx after IgM stimulation of the B220+Mac-1+ population (B1 B cells) of peritoneal cells from wild-type and BOB.1/OBF.1−/− mice. In contrast to that in B2 cells, Ca2+ influx was not decreased in BOB.1/OBF.1−/− B1 B cells (Fig. 8B). Furthermore, the NF-κB activation upon BCR engagement is normal in BOB.1/OBF.1−/− B1 B cells (Fig. 8D). These results suggest that BOB.1/OBF.1 specifically affects BCR-mediated signaling in follicular B cells but not in the B1 B-cell lineage.
DISCUSSION
The definition of MZ B cells is based on three parameters: location, surface marker expression, and function in T-independent humoral response (27, 38, 42). BOB.1/OBF.1-deficient mice contain almost no cells that fulfill any of these parameters.
Earlier analyses of B-lymphocyte development in a BOB.1/OBF.1 (OCA-B)-deficient mouse mutants revealed only a partial reduction of MZ B cells (53). One explanation for this discrepancy could be a difference in the mouse strain background. Our mice were generated on a C57BL/6 background, whereas the mice used in the other study were backcrosses of the 129 strain to C57BL/6. We have analyzed the MZ B-cell population in BOB.1/OBF.1−/− mice on a BALB/c background, as well as on a C57BL/6 × NMRI mixed background and found that the MZ B-cell compartment was also dramatically reduced (Fig. 5A and B and 7). To clarify this issue, we obtained spleens from 129 × C57BL/6 BOB.1/OBF.1-deficient mice from P. Matthias (61). Indeed, these mice showed a much less pronounced reduction of MZ B cells. This indicates that modifier genes exist that influence the consequences of the BOB.1/OBF.1 gene mutation.
Reduction of MZ B-cell numbers in BOB.1/OBF.1−/− mice is a B-cell-intrinsic defect. Histological analysis showed that the general structure of the MZ is not changed in these mice. BOB.1/OBF.1−/− bone marrow cells transferred into μMT mice still are not able to develop into MZ B cells. Since the microenvironment in μMT mice could be considered normal (25), these data further confirm that development of MZ B cells is dependent on BOB.1/OBF.1 expression in B lymphocytes. This finding is in line with the results obtained in the analyses of the other defects of BOB.1/OBF.1-deficient B cells, which all turned out to be B cell intrinsic (22, 53). Moreover, it seems that the MZ B-cell compartment is dependent on BOB.1/OBF.1 protein expression in the late stages of development since expression of the BOB.1/OBF.1 protein limited to early stages of B-cell development (22) could not rescue MZ B-cell numbers.
The MZ B-cell compartment could be affected by defective B-cell migration to or defective retention at the correct microenvironmental site. B-cell compartmentalization depends on cell motility and chemotactic responses (4, 5, 23). Altered migration and reduction of MZ B-cell number were also observed in Pyk-2-, Lsc-, and CD22-deficient mice (17, 21, 56). Interestingly, the alterations in cell motility in these three mutants show distinct patterns. Migration of Pyk-2-deficient B cells is reduced (21). In contrast, B cells isolated from CD22−/− and Lsc−/− mice show enhanced motility (17, 56), as do BOB.1/OBF.1-deficient B cells. The expression of Blr-1, a receptor for the chemokine BLC, is reduced in BOB.1/OBF.1−/− mice (68). Since BLC plays an important role in the processes of splenic organization (15, 68), hyporesponsiveness to BLC could contribute to the incorrect B-cell compartmentalization in BOB.1/OBF.1−/− mice. If disturbed homing was responsible for the lack of MZ B cells, one must conclude that the levels of surface markers characteristic of MZ B cells requires this compartmentalization since FACS analysis of total splenocytes did not reveal B cells with this phenotype in BOB.1/OBF.1−/− mice.
Several recent papers have described the importance of the BAFF for B-cell homeostasis and MZ B-cell development (6, 63, 64). The mRNA expression levels of two out of three BAFFRs, BAFFR and BCMA, are reduced in BOB.1/OBF.1−/− splenocytes. However, while disruption of the BAFF-BAFFR system resulted in a strong reduction in the number of MZ B cells (59, 60), an analysis of BCMA-deficient mice did not reveal any obvious B-cell phenotype (60, 69). We cannot exclude the possibility that the reduction of BCMA expression accompanied by a BOB.1/OBF.1 deficiency and/or a reduction of BAFFR expression contributes to a reduction of MZ B-cell numbers. However, the reduction of BAFFR mRNA expression seems to be the more substantial factor in the mechanism by which the BOB.1/OBF.1 deficiency affects the MZ B-cell compartment. BAFF was noted as being important for the survival and maturation of B cells (6, 37, 52, 54, 55). Thus, reduced BAFFR levels could contribute to the effect of BOB.1/OBF.1 deficiency on the MZ B-cell compartment by affecting the survival of these cells. Interestingly, while numbers of follicular and, especially, MZ B cells are strongly reduced by disruption of the BAFF-BAFFR system, it seems that B1 B-cell survival is not dependent on these molecules (60). In agreement with this, the number of B1 B cells is not decreased in BOB.1/OBF.1−/− mice although our data show that the expression of BAFFR mRNA in these cells is reduced. How the BOB.1/OBF.1 deficiency affects BAFFR mRNA expression is not clear. It is not known whether BAFFR is a direct target gene for BOB.1/OBF.1. We found no obvious binding site for Oct proteins when inspecting the mouse BAFFR promoter sequence.
The role of LT-α in MZ B-cell development was confirmed by several publications showing a reduction in the number of MZ B cells in the absence of LT or the LT receptor (33, 45). In BOB.1/OBF.1−/− splenocytes, we observed a slight increase in the expression of LT-α mRNA. This excludes the possibility that the absence of MZ B cells in BOB.1/OBF.1 mutant mice is due to LT-α insufficiency. Primary B-cell follicles in BOB.1/OBF.1−/− mice also have normal numbers and distribution of follicular dendritic cells (53). Since the role of LT in the maintenance of follicular dendritic cells is well established (16, 43-45), this finding could be indirect evidence that LT action most probably is not impaired in BOB.1/OBF.1−/− mice.
B cells require BCR signaling for development and survival. B1 and MZ B cells are specialized B-cell populations selected for by antigenic stimulation (29, 39, 41). Several recent studies have suggested that BCR signal strength is a major regulator of lineage decision. It has been shown that Aiolos−/− mice have a reduced MZ B-cell compartment and increased Ca2+ influx upon BCR stimulation (10). Recently, we observed that the same holds true for CD22−/− mice (56). In contrast, mice with reduced signal strength, such as phospholipase Cγ2- and Btk-deficient mice, have an increased proportion of MZ B cells (10, 65). Further support was derived from BCR transgenic mice showing different signaling strengths (29, 42). Consequently, it was postulated that a strong signal leads to the development of follicular B (or B1) cells while weak signals favor MZ B-cell development. It could be expected that BOB.1/OBF.1-deficient mice with a severe defect in the MZ B-cell compartment would also show enhanced BCR signaling. Surprisingly, our results clearly show that BOB.1/OBF.1−/− splenic B cells have significantly reduced BCR signaling, thus calling into question the simple version of the signal strength hypothesis of MZ B-cell generation.
How BOB.1/OBF.1 deficiency affects BCR signaling remains unclear. BOB.1/OBF.1 could regulate the expression of a gene(s) required in the BCR signal transduction pathway. No such gene is known. Alternatively, BOB.1/OBF.1 might have a direct role in BCR signaling. A potential direct function of BOB.1/OBF.1 in signal transduction was suggested recently by the discovery of a myristoylated membrane-associated BOB.1/OBF.1 isoform (70). However, it is not clear whether this protein isoform affects BCR signaling.
Interestingly, BOB.1/OBF.1 deficiency has different consequences for BCR signaling in B1 B cells versus B2 B cells. The number of B1 B cells is not changed in BOB.1/OBF.1-deficient mice, although B1 B cells also express BOB.1/OBF.1 (46). Thus, it appears that this protein is not required for B1 B-cell development and function. B1 B cells differ from conventional B cells both in origin and in BCR specificity and activation threshold (38, 39, 42). Again, it is speculated that the BCR activation threshold is the source of the most B1-B2 differences (13). However, the differences in signaling responsible for BCR-triggered activation of B1 and B2 cells are poorly understood. Our data suggest that at least some of the potential BOB.1/OBF.1 target genes (or even BOB.1/OBF.1 itself) are differentially required for BCR signaling in B1 and B2 B cells. Further work is necessary to clarify the molecular differences in BCR signaling between B1 and B2 B cells. One interesting possibility is the existence of a BOB.1/OBF.1-related gene that is specifically expressed in B1 B cells.
Acknowledgments
The first two authors contributed equally to this work.
We thank Patrick Matthias for supplying spleens from BOB.1/OBF.1-deficient mice and Peter Conradt for help with cell sorting by FACS.
This work is supported by a grant (DFG-SFB 497/C5) to Thomas Wirth.
REFERENCES
- 1.Allman, D. M., S. E. Ferguson, and M. P. Cancro. 1992. Peripheral B cell maturation. I. Immature peripheral B cells in adults are heat-stable antigenhi and exhibit unique signaling characteristics. J. Immunol. 149:2533-2540. [PubMed] [Google Scholar]
- 2.Allman, D. M., S. E. Ferguson, V. M. Lentz, and M. P. Cancro. 1993. Peripheral B cell maturation. II. Heat-stable antigen(hi) splenic B cells are an immature developmental intermediate in the production of long-lived marrow-derived B cells. J. Immunol. 151:4431-4444. [PubMed] [Google Scholar]
- 3.Amano, M., N. Baumgarth, M. D. Dick, L. Brossay, M. Kronenberg, L. A. Herzenberg, and S. Strober. 1998. CD1 expression defines subsets of follicular and marginal zone B cells in the spleen: beta 2-microglobulin-dependent and independent forms. J. Immunol. 161:1710-1717. [PubMed] [Google Scholar]
- 4.Ansel, K. M., and J. G. Cyster. 2001. Chemokines in lymphopoiesis and lymphoid organ development. Curr. Opin. Immunol. 13:172-179. [DOI] [PubMed] [Google Scholar]
- 5.Ansel, K. M., V. N. Ngo, P. L. Hyman, S. A. Luther, R. Forster, J. D. Sedgwick, J. L. Browning, M. Lipp, and J. G. Cyster. 2000. A chemokine-driven positive feedback loop organizes lymphoid follicles. Nature 406:309-314. [DOI] [PubMed] [Google Scholar]
- 6.Batten, M., J. Groom, T. G. Cachero, F. Qian, P. Schneider, J. Tschopp, J. L. Browning, and F. Mackay. 2000. BAFF mediates survival of peripheral immature B lymphocytes. J. Exp. Med. 192:1453-1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boehm, J., Y. He, A. Greiner, L. Staudt, and T. Wirth. 2001. Regulation of BOB.1/OBF.1 stability by SIAH. EMBO J. 20:4153-4162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bowman, E. P., J. J. Campbell, D. Soler, Z. Dong, N. Manlongat, D. Picarella, R. R. Hardy, and E. C. Butcher. 2000. Developmental switches in chemokine response profiles during B cell differentiation and maturation. J. Exp. Med. 191:1303-1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cariappa, A., H. C. Liou, B. H. Horwitz, and S. Pillai. 2000. Nuclear factor kappa B is required for the development of marginal zone B lymphocytes. J. Exp. Med. 192:1175-1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cariappa, A., M. Tang, C. Parng, E. Nebelitskiy, M. Carroll, K. Georgopoulos, and S. Pillai. 2001. The follicular versus marginal zone B lymphocyte cell fate decision is regulated by Aiolos, Btk, and CD21. Immunity 14:603-615. [DOI] [PubMed] [Google Scholar]
- 11.Cepek, K. L., D. I. Chasman, and P. A. Sharp. 1996. Sequence-specific DNA binding of the B-cell-specific coactivator OCA-B. Genes Dev. 10:2079-2088. [DOI] [PubMed] [Google Scholar]
- 12.Chasman, D., K. Cepek, P. A. Sharp, and C. O. Pabo. 1999. Crystal structure of an OCA-B peptide bound to an Oct-1 POU domain/octamer DNA complex: specific recognition of a protein-DNA interface. Genes Dev. 13:2650-2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fagarasan, S., N. Watanabe, and T. Honjo. 2000. Generation, expansion, migration and activation of mouse B1 cells. Immunol. Rev. 176:205-215. [DOI] [PubMed] [Google Scholar]
- 14.Fehr, T., C. Lopez-Macias, B. Odermatt, R. M. Torres, D. B. Schubart, T. L. O'Keefe, P. Matthias, H. Hengartner, and R. M. Zinkernagel. 2000. Correlation of anti-viral B cell responses and splenic morphology with expression of B cell-specific molecules. Int. Immunol. 12:1275-1284. [DOI] [PubMed] [Google Scholar]
- 15.Forster, R., A. E. Mattis, E. Kremmer, E. Wolf, G. Brem, and M. Lipp. 1996. A putative chemokine receptor, BLR1, directs B cell migration to defined lymphoid organs and specific anatomic compartments of the spleen. Cell 87:1037-1047. [DOI] [PubMed] [Google Scholar]
- 16.Fu, Y. X., H. Molina, M. Matsumoto, G. Huang, J. Min, and D. D. Chaplin. 1997. Lymphotoxin-alpha (LTalpha) supports development of splenic follicular structure that is required for IgG responses. J. Exp. Med. 185:2111-2120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Girkontaite, I., K. Missy, V. Sakk, A. Harenberg, K. Tedford, T. Potzel, K. Pfeffer, and K. D. Fischer. 2001. Lsc is required for marginal zone B cells, regulation of lymphocyte motility and immune responses. Nat. Immunol. 2:855-862. [DOI] [PubMed] [Google Scholar]
- 18.Greiner, A., K. Müller, J. Hess, K. Pfeffer, K. H. Müller-Hermelink, and T. Wirth. 2000. BOB.1/OBF.1 expression is upregulated in normal germinal center B cells and germinal center derived B cell lymphomas. Am. J. Pathol. 156:501-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gstaiger, M., O. Georgiev, H. van Leeuwen, P. van der Vliet, and W. Schaffner. 1996. The B cell coactivator Bob1 shows DNA sequence-dependent complex formation with the Oct-1/Oct-2 factors, leading to differential promoter activation. EMBO J. 15:2781-2790. [PMC free article] [PubMed] [Google Scholar]
- 20.Gstaiger, M., L. Knoepfel, O. Georgiev, W. Schaffner, and C. M. Hovens. 1995. A B-cell coactivator of octamer-binding transcription factors. Nature 373:360-362. [DOI] [PubMed] [Google Scholar]
- 21.Guinamard, R., M. Okigaki, J. Schlessinger, and J. V. Ravetch. 2000. Absence of marginal zone B cells in Pyk-2-deficient mice defines their role in the humoral response. Nat. Immunol. 1:31-36. [DOI] [PubMed] [Google Scholar]
- 22.Hess, J., P. J. Nielsen, K. D. Fischer, H. Bujard, and T. Wirth. 2001. The B lymphocyte-specific coactivator BOB.1/OBF.1 is required at multiple stages of B-cell development. Mol. Cell. Biol. 21:1531-1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim, C. H., and H. E. Broxmeyer. 1999. Chemokines: signal lamps for trafficking of T and B cells for development and effector function. J. Leukoc. Biol. 65:6-15. [DOI] [PubMed] [Google Scholar]
- 24.Kim, U., F.-F. Qin, S. Gong, S. Stevens, Y. Luo, M. Nussenzweig, and R. G. Roeder. 1996. The B-cell-specific transcription coactivator OCA-B/OBF-1/Bob-1 is essential for normal production of immunoglobulin isotypes. Nature 383:542-547. [DOI] [PubMed] [Google Scholar]
- 25.Kitamura, D., and K. Rajewsky. 1992. Targeted disruption of μ chain membrane exon causes loss of heavy-chain allelic exclusion. Nature 356:154-156. [DOI] [PubMed] [Google Scholar]
- 26.Kitamura, D., J. Roes, R. Kuhn, and K. Rajewsky. 1991. A B cell-deficient mouse by targeted disruption of the membrane exon of the immunoglobulin mu chain gene. Nature 350:423-426. [DOI] [PubMed] [Google Scholar]
- 27.Kraal, G. 1992. Cells in the marginal zone of the spleen. Int. Rev. Cytol. 132:31-74. [DOI] [PubMed] [Google Scholar]
- 28.Kraal, G., and M. Janse. 1986. Marginal metallophilic cells of the mouse spleen identified by a monoclonal antibody. Immunology 58:665-669. [PMC free article] [PubMed] [Google Scholar]
- 29.Lam, K. P., and K. Rajewsky. 1999. B cell antigen receptor specificity and surface density together determine B-1 versus B-2 cell development. J. Exp. Med. 190:471-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lane, P. J., D. Gray, S. Oldfield, and I. C. MacLennan. 1986. Differences in the recruitment of virgin B cells into antibody responses to thymus-dependent and thymus-independent type-2 antigens. Eur. J. Immunol. 16:1569-1575. [DOI] [PubMed] [Google Scholar]
- 31.Laumen, H., P. J. Nielsen, and T. Wirth. 2000. The BOB.1/OBF.1 coactivator is essential for octamer-dependent transcription in B cells. Eur. J. Immunol. 30:458-469. [DOI] [PubMed] [Google Scholar]
- 32.Lernbecher, T., U. Müller, and T. Wirth. 1993. Distinct NF-κB/Rel transcription factors are responsible for tissue-specific and inducible gene activation. Nature 365:767-770. [DOI] [PubMed] [Google Scholar]
- 33.Lu, T. T., and J. G. Cyster. 2002. Integrin-mediated long-term B cell retention in the splenic marginal zone. Science 297:409-412. [DOI] [PubMed] [Google Scholar]
- 34.Luo, Y., H. Fujii, T. Gerster, and R. G. Roeder. 1992. A novel B cell-derived coactivator potentiates the activation of immunoglobulin promoters by octamer-binding transcription factors. Cell 71:231-241. [DOI] [PubMed] [Google Scholar]
- 35.Luo, Y., H. Ge, S. Stevens, H. Xiao, and R. G. Roeder. 1998. Coactivation by OCA-B: definition of critical regions and synergism with general cofactors. Mol. Cell. Biol. 18:3803-3810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luo, Y., and R. G. Roeder. 1995. Cloning, functional characterization, and mechanism of action of the B-cell-specific transcriptional coactivator OCA-B. Mol. Cell. Biol. 15:4115-4124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mackay, F., and J. L. Browning. 2002. BAFF: a fundamental survival factor for B cells. Nat. Rev. Immunol. 2:465-475. [DOI] [PubMed] [Google Scholar]
- 38.Martin, F., and J. F. Kearney. 2000. B-cell subsets and the mature preimmune repertoire. Marginal zone and B1 B cells as part of a “natural immune memory.” Immunol. Rev. 175:70-79. [PubMed] [Google Scholar]
- 39.Martin, F., and J. F. Kearney. 2001. B1 cells: similarities and differences with other B cell subsets. Curr. Opin. Immunol. 13:195-201. [DOI] [PubMed] [Google Scholar]
- 40.Martin, F., and J. F. Kearney. 1999. CD21high IgMhigh splenic B cells enriched in the marginal zone: distinct phenotypes and functions. Curr. Top. Microbiol. Immunol. 246:45-50. [DOI] [PubMed] [Google Scholar]
- 41.Martin, F., and J. F. Kearney. 2000. Positive selection from newly formed to marginal zone B cells depends on the rate of clonal production, CD19, and btk. Immunity 12:39-49. [DOI] [PubMed] [Google Scholar]
- 42.Martin, F., A. M. Oliver, and J. F. Kearney. 2001. Marginal zone and B1 B cells unite in the early response against T-independent blood-borne particulate antigens. Immunity 14:617-629. [DOI] [PubMed] [Google Scholar]
- 43.Matsumoto, M., Y. X. Fu, H. Molina, and D. D. Chaplin. 1997. Lymphotoxin-alpha-deficient and TNF receptor-I-deficient mice define developmental and functional characteristics of germinal centers. Immunol. Rev. 156:137-144. [DOI] [PubMed] [Google Scholar]
- 44.Matsumoto, M., Y. X. Fu, H. Molina, G. Huang, J. Kim, D. A. Thomas, M. H. Nahm, and D. D. Chaplin. 1997. Distinct roles of lymphotoxin alpha and the type I tumor necrosis factor (TNF) receptor in the establishment of follicular dendritic cells from non-bone marrow-derived cells. J. Exp. Med. 186:1997-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mebius, R. E., S. van Tuijl, I. L. Weissman, and T. D. Randall. 1998. Transfer of primitive stem/progenitor bone marrow cells from LT alpha−/− donors to wild-type hosts: implications for the generation of architectural events in lymphoid B cell domains. J. Immunol. 161:3836-3843. [PubMed] [Google Scholar]
- 46.Nielsen, P. J., O. Georgiev, B. Lorenz, and W. Schaffner. 1996. B lymphocytes are impaired in mice lacking the transcriptional co-activator Bob1/OCA-B/OBF1. Eur. J. Immunol. 26:3214-3218. [DOI] [PubMed] [Google Scholar]
- 47.Oliver, A. M., F. Martin, G. L. Gartland, R. H. Carter, and J. F. Kearney. 1997. Marginal zone B cells exhibit unique activation, proliferative and immunoglobulin secretory responses. Eur J. Immunol. 27:2366-2374. [DOI] [PubMed] [Google Scholar]
- 48.Oliver, A. M., F. Martin, and J. F. Kearney. 1999. IgMhigh CD21high lymphocytes enriched in the splenic marginal zone generate effector cells more rapidly than the bulk of follicular B cells. J. Immunol. 162:7198-7207. [PubMed] [Google Scholar]
- 49.Pfisterer, P., A. Annweiler, C. Ullmer, L. Corcoran, and T. Wirth. 1994. Differential transactivation potential of Oct1 and Oct2 is determined by additional B cell-specific activities. EMBO J. 13:1654-1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pfisterer, P., S. Zwilling, J. Hess, and T. Wirth. 1995. Functional characterization of the murine homolog of the B-cell-specific coactivator BOB.1/OBF.1. J. Biol. Chem. 270.:29870-29880. [DOI] [PubMed]
- 51.Pierani, A., A. Heguy, H. Fujii, and R. G. Roeder. 1990. Activation of octamer-containing promoters by either octamer-binding transcription factor 1 (OTF-1) or OTF-2 and requirement of an additional B-cell-specific component for optimal transcription of immunoglobulin promoters. Mol. Cell. Biol. 10:6204-6215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pound, J. 2001. A key role for BAFF in maintaining peripheral B cells. Trends Immunol. 22:659.. [DOI] [PubMed] [Google Scholar]
- 53.Qin, X. F., A. Reichlin, Y. Luo, R. G. Roeder, and M. C. Nussenzweig. 1998. OCA-B integrates B cell antigen receptor-, CD40L- and IL 4-mediated signals for the germinal center pathway of B cell development. EMBO J. 17:5066-5075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rolink, A. G., and F. Melchers. 2002. BAFFled B cells survive and thrive: roles of BAFF in B-cell development. Curr. Opin. Immunol. 14:266-275. [DOI] [PubMed] [Google Scholar]
- 55.Rolink, A. G., J. Tschopp, P. Schneider, and F. Melchers. 2002. BAFF is a survival and maturation factor for mouse B cells. Eur. J. Immunol. 32:2004-2010. [DOI] [PubMed] [Google Scholar]
- 56.Samardzic, T., D. Marinkovic, C. P. Danzer, J. Gerlach, L. Nitschke, and T. Wirth. 2002. Reduction of marginal zone B cells in CD22-deficient mice. Eur. J. Immunol. 32:561-567. [DOI] [PubMed] [Google Scholar]
- 57.Sauter, P., and P. Matthias. 1997. The B cell-specific coactivator OBF-1 (OCA-B, Bob-1) is inducible in T cells and its expression is dispensable for IL-2 gene induction. Immunobiology 198:207-216. [DOI] [PubMed] [Google Scholar]
- 58.Sauter, P., and P. Matthias. 1998. Coactivator OBF-1 makes selective contacts with both the POU-specific domain and the POU homeodomain and acts as a molecular clamp on DNA. Mol. Cell. Biol. 18:7397-7409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schiemann, B., J. L. Gommerman, K. Vora, T. G. Cachero, S. Shulga-Morskaya, M. Dobles, E. Frew, and M. L. Scott. 2001. An essential role for BAFF in the normal development of B cells through a BCMA-independent pathway. Science 293:2111-2114. [DOI] [PubMed] [Google Scholar]
- 60.Schneider, P., H. Takatsuka, A. Wilson, F. Mackay, A. Tardivel, S. Lens, T. G. Cachero, D. Finke, F. Beermann, and J. Tschopp. 2001. Maturation of marginal zone and follicular B cells requires B cell activating factor of the tumor necrosis factor family and is independent of B cell maturation antigen. J. Exp. Med. 194:1691-1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schubart, D. B., A. Rolink, M. H. Kosco-Vilbois, F. Botteri, and P. Matthias. 1996. B-cell-specific coactivator OBF-1/OCA-B/Bob1 required for immune response and germinal centre formation. Nature 383:538-542. [DOI] [PubMed] [Google Scholar]
- 62.Strubin, M., J. W. Newell, and P. Matthias. 1995. OBF-1, a novel B cell-specific coactivator that stimulates immunoglobulin promoter activity through association with octamer proteins. Cell 80:497-506. [DOI] [PubMed] [Google Scholar]
- 63.Thompson, J. S., S. A. Bixler, F. Qian, K. Vora, M. L. Scott, T. G. Cachero, C. Hession, P. Schneider, I. D. Sizing, C. Mullen, K. Strauch, M. Zafari, C. D. Benjamin, J. Tschopp, J. L. Browning, and C. Ambrose. 2001. BAFF-R, a newly identified TNF receptor that specifically interacts with BAFF. Science 293:2108-2111. [DOI] [PubMed] [Google Scholar]
- 64.Thompson, J. S., P. Schneider, S. L. Kalled, L. Wang, E. A. Lefevre, T. G. Cachero, F. MacKay, S. A. Bixler, M. Zafari, Z. Y. Liu, S. A. Woodcock, F. Qian, M. Batten, C. Madry, Y. Richard, C. D. Benjamin, J. L. Browning, A. Tsapis, J. Tschopp, and C. Ambrose. 2000. BAFF binds to the tumor necrosis factor receptor-like molecule B cell maturation antigen and is important for maintaining the peripheral B cell population. J. Exp. Med. 192:129-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang, D., J. Feng, R. Wen, J. C. Marine, M. Y. Sangster, E. Parganas, A. Hoffmeyer, C. W. Jackson, J. L. Cleveland, P. J. Murray, and J. N. Ihle. 2000. Phospholipase Cγ2 is essential in the functions of B cell and several Fc receptors. Immunity 13:25-35. [DOI] [PubMed] [Google Scholar]
- 66.Weih, D. S., Z. B. Yilmaz, and F. Weih. 2001. Essential role of relb in germinal center and marginal zone formation and proper expression of homing chemokines. J. Immunol. 167:1909-1919. [DOI] [PubMed] [Google Scholar]
- 67.Wienands, J., O. Larbolette, and M. Reth. 1996. Evidence for a preformed transducer complex organized by the B cell antigen receptor. Proc. Natl. Acad. Sci. USA 93:7865-7870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wolf, I., V. Pevzner, E. Kaiser, G. Bernhardt, E. Claudio, U. Siebenlist, R. Forster, and M. Lipp. 1998. Downstream activation of a TATA-less promoter by Oct-2, Bob1, and NF-κB directs expression of the homing receptor BLR1 to mature B cells. J. Biol. Chem. 273:28831-28836. [DOI] [PubMed] [Google Scholar]
- 69.Xu, S., and K. P. Lam. 2001. B-cell maturation protein, which binds the tumor necrosis factor family members BAFF and APRIL, is dispensable for humoral immune responses. Mol. Cell. Biol. 21:4067-4074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yu, X., L. Wang, Y. Luo, and R. G. Roeder. 2001. Identification and characterization of a novel OCA-B isoform: implications for a role in B cell signaling pathways. Immunity 14:157-167. [PubMed] [Google Scholar]
- 71.Zwilling, S., A. Dieckmann, P. Pfisterer, P. Angel, and T. Wirth. 1997. Inducible expression and phosphorylation of coactivator BOB.1/OBF.1 in T cells. Science 277:221-225. [DOI] [PubMed] [Google Scholar]