The difficulty in life is the choice. — George Moore, The Bending of the Bough
Health care professionals caring for patients with cardiovascular disease are faced with an increasingly complex array of difficult choices. In this issue (page 1233), Madhu Natarajan and colleagues1 describe how they evaluated over 8000 patients waiting for cardiac catheterization within the Hamilton, Ont., region during a 2-year period ending in March 2000. Only 37% of the procedures were completed within the waiting times requested by the referring physicians. A disproportionately high fraction of the 50 deaths, 32 myocardial infarctions (MIs) and 156 episodes of unstable angina that occurred while patients were waiting for catheterization were in outpatients, who represented 59% of all requests. Not surprisingly, multivariate analysis showed that those at greatest risk were older and had symptoms suggesting more advanced disease. Aortic stenosis and depressed left ventricular ejection fraction were also powerful predictors of unfavourable events in outpatients. Although central booking existed and procedure waiting times were prioritized according to urgency, this approach applied only to inpatients, whose names were then added to the central catheterization list. In contrast, outpatients were triaged to individual angiographers. This process was presumably modulated by the angiographers' schedule, available laboratory time and their own prioritization.
Although some useful clues for practitioners are provided in this report, it is unclear whether the rather high proportion (33.5%) of patients with normal coronary arteries or mild coronary disease underwent appropriate risk stratification with noninvasive testing, what this revealed and how it was applied to the waiting time for cardiac catheterization. In contrast, those deemed to be at high risk on stress testing and those with low left ventricular ejection fraction, advanced symptoms or recent MI were proportionately more likely to wait beyond their requested waiting time. These findings seem somewhat paradoxical. This disconnect between the knowledge of factors associated with increased risk and the length of procedural delay provides insight into a more opportune use of a limited resource. Hence, patients identified through appropriate risk stratification to be at low risk should have the longest delay. We are also uncertain what proportion of inpatients had unstable angina or acute MI. Notwithstanding the priority for such patients, there exists, even within this subset, a genuine hierarchy of urgency that should influence procedure timing.
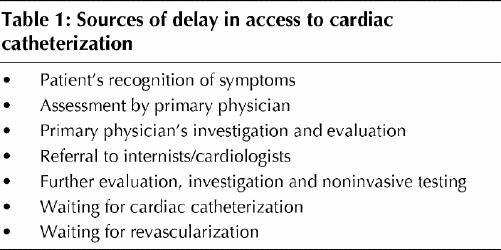
Are these Hamilton waiting times reasonable, and is the frequency of adverse events while waiting for catheterization acceptable? Arguably, any death of a patient on a waiting list is 1 death too many. Yet a median waiting time of 60 days for outpatient catheterization is likely to be representative of many other Canadian institutions. Sources of delay are unfortunately many (Table 1). For patients presenting with acute coronary syndromes, the need for timely urgent intervention can be sensibly guided by intelligent and contemporaneous risk assessment that continually assesses response to medical therapy. Depending on these factors, we should be aiming at intervention either immediately or within 48 hours of admission.2,3
Table 1
Natarajan and colleagues1 have done us a service by recalling the need for appropriate audit at individual centres concerning waiting times and adverse cardiac events. This experience again signals the need for national surveillance and standards to define and assess severity and urgency and to gauge expected benefit.4,5,6,7 Recent demonstration of improved outcomes among appropriately selected patients undergoing revascularization, as well as with the use of cardioverter/defibrillator devices for those at risk for or surviving sudden cardiac death, will only augment the already substantial pressure on Canadian cardiovascular resources.2,8,9 The need for systematic planning and cooperation among regional medical centres, provincial and federal governments, and national organizations, such as the Heart and Stroke Foundation of Canada and the Canadian Cardiovascular Society, has never been greater.
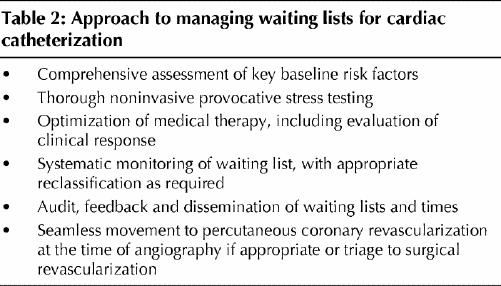
To be sure, the road ahead is filled with difficult choices, but an approach such as that outlined in Table 2 can assist in the evaluation of patients awaiting cardiac catheterization. Systematic monitoring that is open and disseminated, with audit and feedback driving timely and effective triage, is the preferred method for the engagement of high-quality professionals working among rationally distributed resources. Over 5 years ago, a Canadian Cardiovascular Society national consensus conference examined this issue and called urgently for a national registry to collect accurate prospective data on performance characteristics and waiting times.10 Both that time and some patients have since expired: the book is overdue.
Table 2
β See related article page 1233
Footnotes
Contributors: Both authors contributed substantially to the conception and design of the commentary. Dr. Ezekowitz laid out an initial plan, from which drafts of the article were constructed. Both authors approved the final version of the manuscript.
Competing interests: None declared.
Correspondence to: Dr. Paul W. Armstrong, 2-51 Medical Sciences Building, University of Alberta, Edmonton AB T6G 2H7; fax 780 492-9486; paul.armstrong@ualberta.ca
References
- 1.Natarajan MK, Mehta SR, Holder DH, Goodhart DR, Gafni A, Shilton D, et al. The risks of waiting for cardiac catheterization: a prospective study. CMAJ 2002;167(11):1233-40. [PMC free article] [PubMed]
- 2.FRagmin and Fast Revascularisation during InStability in Coronary Artery Disease Investigators. Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. Lancet 1999;354:708-15. [PubMed]
- 3.Fitchett D, Goodman S, Langer A. New advances in the management of acute coronary syndromes: 1. Matching treatment to risk. CMAJ 2001; 164(9):1309-16. [PMC free article] [PubMed]
- 4.Knudtson ML. Waiting list issues. Can J Cardiol 1997;13(Suppl D):67D-72D. [PubMed]
- 5.Hadorn DC, the Steering Committee of the Western Canada Waiting List Project. Setting priorities for waiting lists: defining our terms. CMAJ 2000;163(7):857-60. [PMC free article] [PubMed]
- 6.Sanmartin C, Shortt SE, Barer ML, Sheps S, Lewis S, McDonald PW. Waiting for medical services in Canada: lots of heat, but little light. CMAJ 2000;162(9):1305–10. [PMC free article] [PubMed]
- 7.Alter DA, Basinski ASH, Cohen EA, Naylor CD. Fairness in the coronary angiography queue. CMAJ 1999;161(7):813-7. [PMC free article] [PubMed]
- 8.Cannon CP, Weintraub WS, Demopoulos LA, Vicari R, Frey MJ, Lakkis N, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med 2001;344:1879-87. [DOI] [PubMed]
- 9.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346(12):877-83. [DOI] [PubMed]
- 10.Higginson LA, Naylor CD. Rates of cardiac catheterization, coronary angioplasty and coronary artery bypass surgery in Canada. Can J Cardiol 1997; 13(Suppl D):47D-52D. [PubMed]


