Abstract
THERE HAS BEEN SIGNIFICANT PROGRESS in the area of mood disorders over the last 2 decades, encompassing advances in our knowledge of epidemiology, diagnosis, pathogenesis and treatment. This article presents a clinically oriented update and review on the diagnosis and management of major depressive disorder.
Mood disorders are among the most common afflictions that bring patients to doctors. Almost 20% of adults will have a mood disorder requiring treatment during their lifetime, and about 8% of adults will have a major depressive disorder during their lives.1
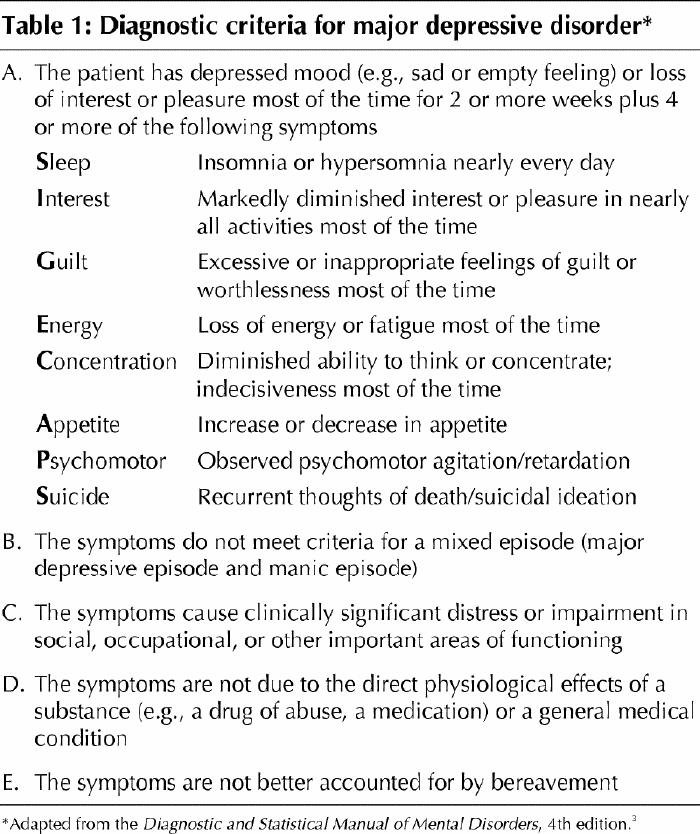
There are no pathognomonic markers of depression, although this is an area of active research.2 Diagnosis both in clinical practice and in clinical research studies is based on a set of specific signs and symptoms (Table 1). These criteria have helped distinguish various mood disorders that may have different causes and that certainly require different clinical management.
Table 1
In this review I focus on major depressive disorders. Closely related illnesses that are not discussed are dysthymic disorders and bipolar illnesses, which have lifetime rates of occurrence in the North American population of 8% and 2% respectively.6 As well, I do not discuss depressive syndromes induced by substance abuse or associated with a general medical condition. Useful review articles are available.7
Epidemiologic characteristics
As noted above, depressive disorders are common. Most clinicians will be involved in the care of these patients. Depression is twice as common in women as in men.1,8 The risk of a major depression increases 1.5 to 3.0 times if the illness is present in a first-degree relative as compared with no such illness in a first-degree relative.4,5
Surprisingly, for such a common disease there is little agreement on the association between age and onset. This is due to the fact that research is hampered by the absence of an unambiguous and universally agreed on set of diagnostic criteria and the fact that many of the studies have included patients already in the medical care system. It is well known that many people who meet the diagnostic criteria for depression do not seek treatment. A recent Canadian study using data from the National Population Health Survey suggests that the highest rates of first onset of depression (1.4%–9.1% of the population) occur among young adults (aged 12 to 24), and lower rates (1.3%–1.8%) occur among people 65 years of age or more.9
Depressive illnesses carry significant risks of death and disability. About 15% of patients with a mood disorder die by their own hand,10 and at least 66% of all suicides are preceded by depression. Rates of suicide in Canada are higher than those in the United States.11
Depressive disorders are associated with poor work productivity, as indicated by a 3-fold increase in the number of sick days in the month preceding the illness for workers with a depressive illness compared with coworkers who did not have such an illness.12,13 Depressive illnesses also affect family members and caregivers,14 and there is increasing evidence that children of women with depression have increased rates of problems in school and with behaviour, and have lower levels of social competence and self-esteem than their classmates with mothers who do not have depression.15 Depression is the leading cause of disability and premature death among people aged 18 to 44 years, and it is expected to be the second leading cause of disability for people of all ages by 2020.16,17
Depressive illnesses have also been shown to be associated with increased rates of death and disability from cardiovascular disease.18,19,20,21 Among 1551 study subjects without a history of heart disease who were followed for 13 years, the odds ratio for acute myocardial infarction among the subjects who had a major depressive episode was 4.5 times higher than among those who did not have a depressive episode.19 Among consecutive patients admitted to hospital with an acute myocardial infarction who had their mood measured with a standard depression rating scale, even those with minimal symptoms of depression had evidence of higher subsequent risk of death following their infarction and over the next 4 months.20 This risk was independent of other major risk factors, including age, ventricular ejection fraction and the presence of diabetes mellitus.
These and other findings are intriguing and are the subject of much ongoing research. Although the association was initially considered to be spurious, current mechanistic explanations include impaired platelet functioning, decreased heart rate variability (perhaps a consequence of imbalance in autonomic tone), and immune system activation and hypercortisolemia as stressor responses to depression.21 An unhealthy lifestyle may also be more common among depressed people.21 Whatever the cause, the accumulating data strongly suggest that clinicians should be alert to depression occurring in the context of other acute and chronic diseases. There is as yet no evidence that treatment of mild, clinically unapparent depressive symptoms in these settings will alter the clinical course of the underlying disease. Nonetheless, when depression is diagnosed in the presence of other diseases, treatment should be considered and discussed with the patient.
Etiology
Depression is thought to result from disruption of the normal brain neurochemistry. Work in this area has led to the development of new drugs to treat depression. These drugs appear to affect a number of central monoamine neurotransmitters. Central norepinephrine neural pathways are likely involved in activities of vigilance, motivation and general levels of energy. These pathways share a role with serotonin neural pathways in affecting anxiety and irritability. Serotonin neural pathways appear to control or have a role in controlling impulsivity and share a role with the dopamine pathways in appetite, sex and aggression. Our growing knowledge in this area helps us understand the etiology and pharmacotherapy of mood disorders.
Current theories of depression are complex and beyond the scope of this review.22,23,24 Fig. 1 outlines some of these theories. We are now aware that “long-term” (i.e., 30 days) antidepressant treatment results in sustained activation of cyclic adenosine 3-5-monophosphate (cAMP) in specific brain regions. Protein kinase A, which is stimulated by cAMP, phosphorylates the cAMP regulatory element binding protein. This protein then regulates and activates specific target genes, including brain-derived neurotrophic factor (BDNF), a neuroprotective factor that results in hippocampal nerve growth (Fig. 1). Psychological stress, important in the pathogenesis of depression, can decrease the production of BDNF and result in hippocampal neuronal atrophy.23,24 Furthermore, a series of brain-imaging studies consistently showed reduced neuronal activity in the dorsolateral prefrontal cortex that covaried with the severity of the depression (i.e., the more severe the depression, the larger the prefrontal deficits).25 Thus, an updated hypothesis on the development of a depressive disorder might posit that stress-induced vulnerability in genetically susceptible people may induce a cascade of intracellular neuronal mechanisms that increase or decrease specific neurotrophic factors necessary for the survival and function of specific brain neurons. Furthermore, not only antidepressants but also electroconvulsive therapy26 and depression-focused psychotherapy27 can affect neuronal growth and regional brain metabolism.
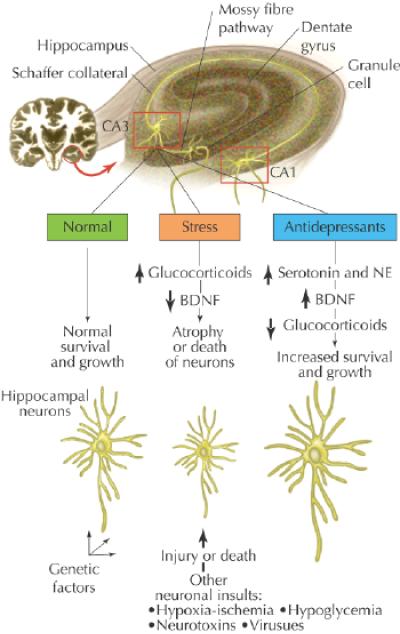
Fig. 1: A molecular and cellular model for the action of antidepressant treatments and the pathophysiology of stress-related disorders. This model of the hippocampus shows the major cell types in the hippocampus and how stress and antidepressant treatments may influence CA3 pyramidal cells. The 3 major subfields of the hippocampus (CA3 and CA1 pyramidal cells and dentate gyrus granule cells) are connected by the mossy fibre and Schaffer collateral pathways. Recent studies demonstrate that chronic stress decreases the expression of brain-derived neurotrophic factor (BDNF) in the hippocampus. This may contribute to the atrophy or death of neurons in the CA3 pyramidal cell layer of the hippocampus. Long-term elevation of glucocorticoid levels is also known to decrease the survival of these neurons. Other types of neuronal insult, such as hypoxia–ischemia, hypoglycemia, neurotoxins and viral infections, may also cause atrophy or damage of neurons and thereby make a person vulnerable to subsequent insults. These types of interaction may underlie the observations of decreased function and volume of hippocampus in patients with affective disorders and may explain the selective vulnerability of certain people to become depressed. Long-term antidepressant treatments increase the expression of BDNF as well as tyrosine kinase receptor B (trkB) and prevent the down-regulation of BDNF elicited by stress. This may increase the growth or survival of neurons, or help repair or protect neurons from further damage. Increased expression of BDNF and trkB seems to be mediated by the sustained elevation of the serotonin and norepinephrine (NE) systems and the cyclic adenosine monophosphate cascade. Normalization of glucocorticoid levels by long-term antidepressant treatments may also contribute to the recovery of CA3 neurons. (Adapted from Duman et al22 with permission of the publisher.) Photo: Paulette Dennis
Some of the neurotransmitters that are thought to be involved in the etiology of depression are outlined in Fig. 2, which emphasizes the interactions or “cross talk” that probably occur.28
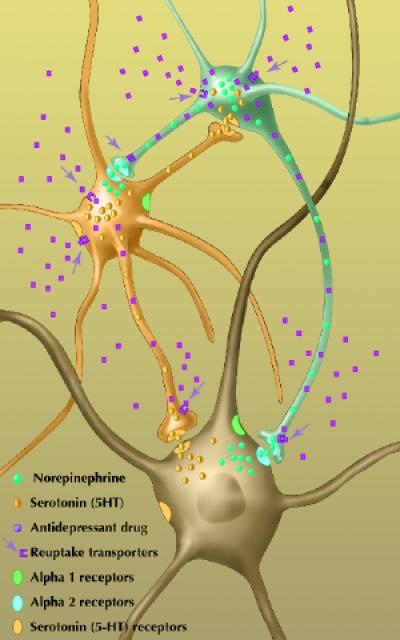
Fig. 2: Schematic of the “cross talk” and purported interactions in the brain between norepinephrine (NE), serotonin (5-HT) and the postsynaptic neurons. (Adapted from Blier28 with permission of the publisher.) Photo: Paulette Dennis
Principles of management
Recognition of the disease
Despite its high prevalence, only one-third of all patients with depression receive adequate treatment.29 The following are 4 common clinical errors that lead to diagnostic or treatment failures associated with depressive disorders:
· Insufficient questioning. Diagnostic failures occur when the patient is not asked questions that may elicit the symptoms of a mood disorder despite what should be a high index of suspicion based on its prevalence. The mnemonic “SIGECAPS” (sleep, interest, guilt, energy, concentration, appetite, psychomotor, suicide) (Table 1) may be a useful clinical adjunct (i.e., 4 or more SIGECAPS for major depression, 2 or 3 SIGECAPS for dysthymia).
· Failure to consult a family member. Owing to the cognitive distortions associated with the disease, it is not unusual for patients to minimize or exaggerate their symptoms. Thus, in patients who are relatively new to one's practice, it is risky at best to make (or exclude) a diagnosis of depression without collateral information from a relative, such as a spouse or parent.
· Acceptance of a diagnosis of a mood disorder despite lack of diagnostic criteria (e.g., starting treatment for depression when only a “depressed mood” is present without the concomitant mental and physical symptoms [i.e., SIGECAPS]).
· Exclusion of a diagnosis or failure to start treatment for depression despite the associated symptom complex (e.g., “Of course you're depressed. Who wouldn't be depressed if these events were occurring in their life?” In other words, “explaining” the diagnosis rather than considering treatment options).
These clinical errors, coupled with the stigma associated with psychiatric conditions,30 result in the underdiagnosis of major mood disorders. Clinicians should keep a high index of suspicion for this common disorder, question the patient about the constellation of symptoms (not just a mood change) associated with depression (i.e., SIGECAPS), and consider obtaining collateral information from a relative if they do not know the patient well or if the diagnosis is unclear.
Do no harm
The patient's thoughts of suicide should be taken seriously. The clinician should broach this topic in the first visit and regularly monitor for a change in the patient's intent and lethality. The priority is always the patient's (and others') safety. Detailed lethal plans, social isolation, substance abuse, previous suicide attempts and a family history of suicide all increase the risk, which may increase the need for careful and close monitoring (frequent visits, having the patient reside with friends or family, or hospital care).31
Therapeutic alliance
Treatment requires a compassionate, nonjudgemental attitude on the part of the physician. Initially, physicians need to educate patients about the illness concept of depression and to specifically tell them of their expectations for significant or full recovery (instillation of hope). Patients should be encouraged to ask questions and to let the doctor know if they cannot adhere to the treatment regimen rather than stopping treatment unilaterally. Family members are essential allies in supporting the depressed patient to comply with treatment, and their involvement is encouraged.
Biologic treatment
Antidepressant drug therapy
Therapy with an antidepressant agent is the preferred treatment in cases of moderate to severe major depression. The rate of response to an antidepressant trial is about 60% and is close to 80% if therapy with a second drug is tried after an initial antidepressant drug failure.32,33
Patients should learn that the physiologic symptoms of depression (disturbances of sleep, appetite, energy and motor activity) may resolve before the patient subjectively senses improvement (hence the rationale for “objective” reports from family members). Symptoms typically do not start to resolve until the patient has received an adequate dosage of medication for 2 to 4 weeks. Full remission (i.e., back to baseline and resolution of all SIGECAPS) — the goal of treatment — may take up to 4 months. There is an increasing risk of recurrence or chronicity, or both,34 if residual symptoms persist.
Reminding the patient that recovery is typically a “sawtooth curve” rather than a linear progression may reassure the patient and family when a few “bad” days occur. Patients need to be aware that side effects are typically transient and that they should not stop therapy, even if they are feeling better, without discussing it with the doctor.
Choosing an antidepressant agent
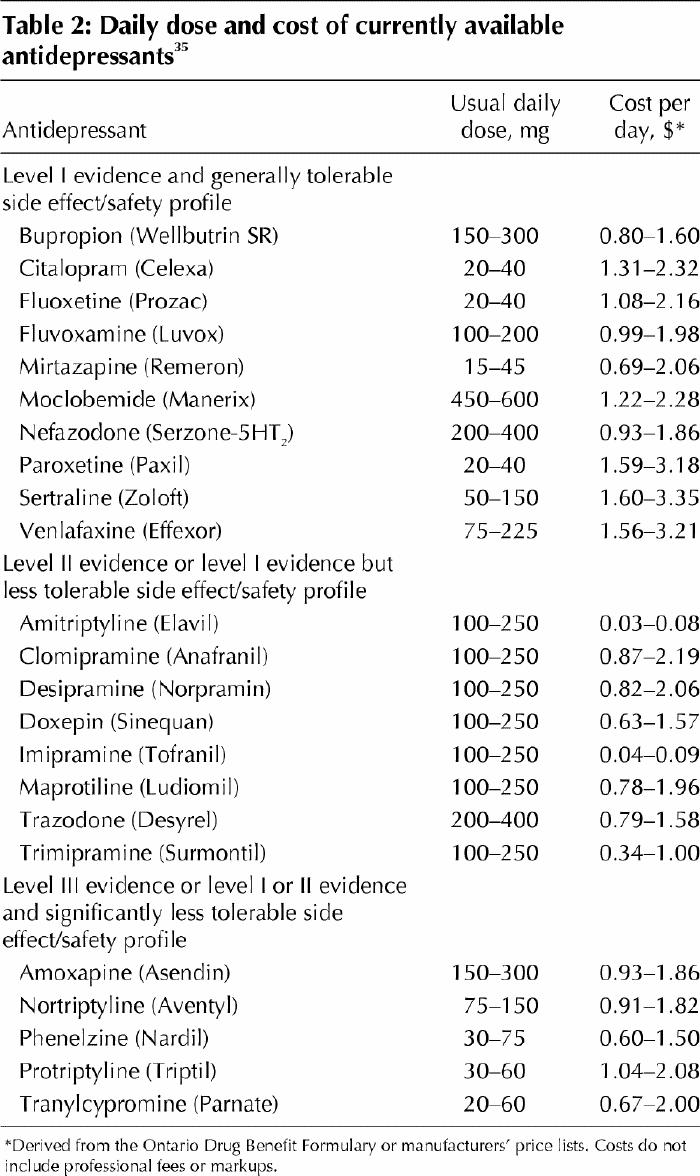
Over 20 antidepressants are commercially available in Canada (Table 2), and this number will certainly increase. Thus, the choice can be daunting in our commercial era, in which television advertisements, gift-laden industry representatives and distinguished professors at elegant dinners each extol the virtues of a different antidepressant.
Table 2
The following are basic concepts to consider in choosing an antidepressant:
· If the patient has had a previous positive response to a specific antidepressant, it would be prudent to initiate a trial with this drug. If a family member has had a previous good response with a certain antidepressant, the patient may feel more comfortable starting treatment with that drug. Likewise, if a family member has had an untoward response to a specific drug (or if the popular press is giving a specific drug a great deal of negative attention), one should consider other drug alternatives.
· Safety considerations should be reviewed. In suicidal patients at risk of overdose, the older-generation antidepressants (i.e., tricyclics and monoamine oxidase inhibitors [MAOIs]) can be lethal, whereas the newer-generation selective serotonin reuptake inhibitors (SSRIs) and others are relatively safe in overdose.36
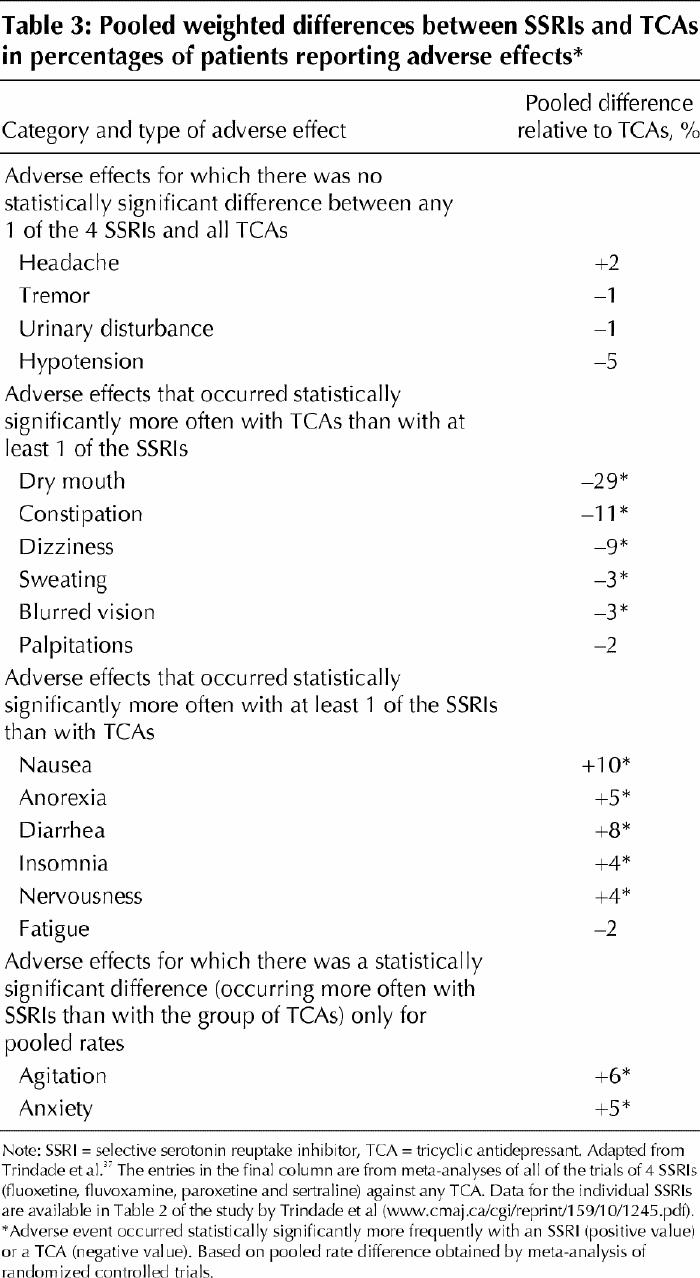
· Side effect tolerability should be matched to the individual patient. No antidepressant is devoid of side effects, but common class side effects, such as orthostatic hypotension (tricyclics), sedation (trazodone, fluvoxamine, paroxetine), stimulation (bupropion), weight gain (tricyclics, phenelzine, mirtazapine) and sexual dysfunction (SSRIs), may be more or less problematic for a specific patient should that side effect develop. Trindade and colleagues37 conducted a comprehensive systematic review and meta-analysis of side effects of SSRIs and tricyclic antidepressants. Table 3 shows the major class differences in the pooled analysis of 84 randomized controlled trials comparing SSRIs and tricyclic antidepressants.
Table 3
· Drug interactions are possible due to induction or inhibition of liver enzymes. In patients with coexisting medical disorders who are taking a number of other medications, an antidepressant with few drug–drug interactions (e.g., citalopram, sertraline, venlafaxine, mirtazapine) would be appropriate.38
· Unfortunately, physicians seldom consider the cost of drugs for our patients; however, cost is often one of the primary factors influencing a patient's decision to continue to take a prescribed medication. Substantial cost differences remain between tricyclic antidepressants, MAOIs, the generic SSRI fluoxetine and the newer antidepressant agents (Table 2).
Monotherapy versus augmentation
Sixty percent of patients with major depression or a dysthymic disorder will have a clinical response to an adequate trial (3–6 weeks) of an antidepressant.32,33 However, if there is no response (i.e., no change in SIGECAPS) after 3 weeks, the likelihood of a response is less than 20%,39 and a switch to an antidepressant of a different chemical class should be contemplated.
If, after 3–6 weeks, there is a partial response (i.e., some change in SIGECAPS) but not full resolution of symptoms, the physician should consider either raising the antidepressant dose if the patient can tolerate a higher dose with minimal side effects, or augmentation. The addition of a small dose of lithium,40 liothyronine sodium41 or a psychostimulant42 will quickly (i.e., within 1–2 weeks) convert a partial response to a full response in 25% of patients.
Switching antidepressants
If there is no or limited response to an adequate antidepressant trial and increasing the dose or augmentation is either unsuccessful or not appropriate, then switching to a different antidepressant is the appropriate strategy. Current thinking is to switch to a different SSRI or a newer antidepressant, or both. Most clinicians will defer a trial of a tricyclic antidepressant or MAOI until at least 2 trials of newer medications have failed. In general, there is no need to stop one antidepressant before starting a second drug trial, and typically the dosage of the first drug is tapered as the new antidepressant is started. Classic MAOIs are the exception, requiring a 2-week washout period before therapy with another antidepressant can be initiated. If the patient has not tolerated the first drug well, then a washout period may be prudent to dissipate side effects before a second drug trial.
Special considerations
There are few significant drug–drug interactions with the newer non-tricyclic/non-MAOI antidepressants. All antidepressants are metabolized by one or more of the cytochrome P450 (CYP450) hepatic isoenzymes. For depressive patients taking a number of other medications, antidepressants that have minimal CYP450 inhibitions (e.g., citalopram, venlafaxine, mirtazapine) should be considered.
In elderly people, pregnant women and breast-feeding women, one should be aware of certain factors. Antidepressants are effective in elderly people.43 The tenant “start low, go slow” applies, and the use of the newer agents, in particular those with minimal CYP450 inhibition, is appropriate and safer than the use of tricyclic antidepressants or MAOIs. There is growing evidence that antidepressants are safe during pregnancy, that they do not increase the risk of teratogenesis and that the risk of depressive relapse may be as high as 75% in pregnant women who stop their antidepressant therapy.44,45 These data should be incorporated into discussions with pregnant women as they review the benefits and risks of ongoing antidepressant chemotherapy. Data on the use of antidepressants during breast-feeding are limited, and long-term developmental effects are unknown. Preliminary safety data do not contraindicate the use of several tricyclic antidepressants and SSRIs.46
Maintenance therapy
Over 70% of patients experience a recurrence of depression during their lifetime.47 Most physicians (and their patients) stop antidepressant therapy too early, without discussion as to the risk of relapse and the subsequent risk of disability and death. Current guidelines suggest that, after recovery occurs, antidepressant therapy should be continued at the therapeutic dosage for at least 6 months to significantly lessen the chance of relapse.35,36 Indefinite antidepressant maintenance therapy should be discussed with patients with additional risk factors (2 or more episodes of depression in 5 years, episodes after the age of 50 and difficult-to-treat episodes).48 The clinician should review with the patient the benefits (prevention of recurrence) and risks (e.g., cost, side effects, inconvenience of taking medication) of treatment. If antidepressant therapy is stopped, the dosage should be tapered gradually to avoid discontinuation symptoms.49
Electroconvulsive therapy
Electroconvulsive therapy (ECT) has been and continues to be the most effective treatment for major depression.50,51 Between 60% and 80% of all depressed patients who receive a course of ECT respond to this treatment.50,51 A typical course of ECT is 6 to 12 treatments, with 2 to 3 treatments given per week. Improvement is typically noted after the fourth treatment. ECT should be considered a first-line treatment in depressed patients with psychotic features, actively suicidal patients and patients who have not responded to or cannot tolerate antidepressant chemotherapy. Although the mechanism of efficacy of ECT remains unclear, electroencephalography typically shows slowing in the prefrontal cortex (which likely reflects a more fundamental neurobiologic process) in patients who respond to ECT.52
Light therapy
Phototherapy is an established and effective treatment for major depression with a seasonal variation, particularly fall/winter depressions. Its efficacy in nonseasonal depression is not established. Phototherapy is an alternative treatment intervention to antidepressant therapy in mild to moderate seasonal depression. The reader is encouraged to refer to published Canadian guidelines.53 The usual treatment is at least 30 minutes per day of light therapy with a standard phototherapy device (delivering 10 000 lx of full-spectrum white light) throughout the fall/winter episode. Phototherapy devices can now be purchased or rented at many medical supply and equipment stores.
St. John's wort
St. John's wort (hypericin) is a popular alternative treatment for depression. Despite European studies demonstrating the efficacy of St. John's wort,54 a recent North American controlled study showed the compound to be no more effective than placebo in major depressive disorder.55 Although patients with mild mood symptoms (i.e., not major depression) may receive some benefit from hypericin, and the herb is relatively benign in terms of side effects and drug–drug interactions, physicians should encourage more standardized treatments in patients with moderate to severe mood disorders.
Other interventions
Although current data are limited, potential new or novel interventions for the treatment of mood disorders may include exercise regimens,56 sleep deprivation,57 psychosurgery,58 vagus nerve stimulation59 and transcranial magnetic stimulation.60
Psychological treatment
In addition to supportive and psychoeducational techniques, specific psychotherapeutic interventions are as effective as antidepressant therapy in mild to moderate major depression and dysthymic disorders.61,62,63
Cognitive behavioural therapy64,65 and interpersonal therapy66 are the treatment interventions with documented efficacy. Both therapies require specialized training, can be administered individually or in a group setting, and typically require 8 to 16 weekly sessions for efficacy.
The choice of psychotherapy or chemotherapy should be based on patient preference, clinician judgement and cost as well as the practical issue of availability of psychotherapy. Furthermore, patients who have not responded to their preferred treatment modality should be encouraged to try other interventions.
Although combined pharmacotherapy–psychotherapy is widely practised in the psychiatric community, the evidence of additive effects remains limited.67
Conclusion
There has been significant progress in the area of mood disorders over the last 2 decades, encompassing advances in our knowledge of epidemiology, diagnosis, pathogenesis and treatment. As clinicians we must enhance our efforts to recognize this illness in our patients and ensure that the myriad of effective treatments are offered and used. Furthermore, by espousing a medical model of this disease, we lessen the pervasive stigma that is associated with all mental disorders.
Acknowledgments
I thank Dr. Raymond W. Lam for his helpful and constructive critiques of the manuscript.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Correspondence to: Dr. Ronald A. Remick, Department of Psychiatry, St. Paul's Hospital, 1081 Burrard St., Vancouver BC V6Z 1Y6; rremick@shaw.ca
References
- 1.Murphy JM, Laird NM, Monson RR, Sobel AM, Leighton AH. A 40-year perspective on the prevalence of depression: the Stirling County Study. Arch Gen Psychiatry 2000;57:209-15. [DOI] [PubMed]
- 2.Duffy A. Towards effective early intervention and prevention strategies for major affective disorders: a review of antecedents and risk factors. Can J Psychiatry 2000;45:340-8. [DOI] [PubMed]
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: The Association; 1994.
- 4.Bland RC. Epidemiology of affective disorders: a review. Can J Psychiatry 1997;42(4):367-77. [DOI] [PubMed]
- 5.Sadovnick AD, Remick RA, Lam RW, Zis AP, Yee IM, Huggins NJ, et al. Mood Disorder Service Genetic Database: morbidity risks for mood disorders in 3,942 first-degree relatives of 671 index cases with single depression, recurrent depression, bipolar I, or bipolar II. Am JMed Genet 1994;54:132-40. [DOI] [PubMed]
- 6.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry 1994;51:8-19. [DOI] [PubMed]
- 7.Enns MW, Swenson JR, McIntyre RS, Swinson RP, Kennedy SH, and the CANMAT Depression Work Group. Clinical guidelines for the treatment of depressive disorders. VII. Comorbidity. Can J Psychiatry 2001;46(Suppl 1):77S-90S. [PubMed]
- 8.Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu HG, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA 1996;276:293-9. [PubMed]
- 9.Patten SB. Incidence of major depression in Canada. CMAJ 2000;163:714-5. [PMC free article] [PubMed]
- 10.Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a re-examination. Am J Psychiatry 2000;157:1925-32. [DOI] [PubMed]
- 11.Sakinofsky I, Leenaars AA. Suicide in Canada with special reference to the difference between Canada and the United States. Suicide Life Threat Behav 1997;27:112-26. [PubMed]
- 12.Parikh SV, Wasylenki D, Goerung P, Wong J. Mood disorders: rural/urban differences in prevalence, health care utilization, and disability in Ontario. J Affect Disord 1996;38:57-65. [DOI] [PubMed]
- 13.Kessler RC, Barber C, Birnbaum HG, Frank RG, Greenberg PE, Rose RM, et al. Depression in the workplace: effects on short-term disability. Health Aff(Millwood) 1999;18:163-71. [DOI] [PubMed]
- 14.Denihan A, Bruce I, Coakley D, Lawlor BA. Psychiatry morbidity in cohabitants of community-dwelling elderly depressives. Int J Geriatr Psychiatry 1998;13:691-4. [DOI] [PubMed]
- 15.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev 1999;106:458-90. [DOI] [PubMed]
- 16.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. Lancet 1997;349:1498-504. [DOI] [PubMed]
- 17.Gredon JF. The burden of disease in treatment-resistant depression. J Clin Psychiatry 2001;62:26-31. [PubMed]
- 18.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18 month prognosis after myocardial infarction. Circulation 1995;91:999-1005. [DOI] [PubMed]
- 19.Pratt LA, Ford DE, Crum RM, Armenian HK, Gallo JJ, Eaton WW. Depression, psychotropic medication, and risk of myocardial infarction. Prospective data from the Baltimore ECA follow-up. Circulation 1996;94:3123-9. [DOI] [PubMed]
- 20.Bush DE, Ziegelstein RC, Tayback M, Richter D, Stevens S, Zahalsky H, et al. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol 2001;88:337-41. [DOI] [PubMed]
- 21.Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease. Arch Gen Psychiatry 1998;55:580-92. [DOI] [PubMed]
- 22.Duman RS, Heninger GR, Nestler EJ. A molecular and cellular theory of depression. Arch Gen Psychiatry 1997;54:597-608. [DOI] [PubMed]
- 23.Stahl SM. Essential psychopharmacology of depression and bipolar disorder. New York: Cambridge University Press; 2000. p. 20-63.
- 24.Manji HK, Moore GJ, Rajkowska G, Chen G. Neuroplasticity and cellular resilience in mood disorders. Mol Psychiatry 2000;5:578-93. [DOI] [PubMed]
- 25.Drevets WC. Functioning neuroimaging studies of depression: the anatomy of melancholia. Annu Rev Med 1998;49:341-61. [DOI] [PubMed]
- 26.Vaidya VA, Sivciak JA, Du F, Dumnan RS. Hippocampal mossy fiber sprouting induced by chronic electroconvulsive seizures. Neuroscience 1999;89:157-66. [DOI] [PubMed]
- 27.Thase ME. Neuroimaging profiles and the differential therapies of depression. Arch Gen Psychiatry 2001;58:651-2. [DOI] [PubMed]
- 28.Blier P. Crosstalk between the norepinephrine and serotonin systems and its role in the antidepressant response. J Psychiatry Neurosci 2001;26(Suppl):S3-10. [PMC free article] [PubMed]
- 29.Judd LL, Paulus MP, Wells KB, Rapaport MH. Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. Am J Psychiatry 1996;153:1411-7. [DOI] [PubMed]
- 30.Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Friedman SJ, Meyers BS. Stigma as a barrier to recovery. Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv 2001; 52: 1615-20. [DOI] [PubMed]
- 31.Nemeroff CB, Compton MT, Berger J. The depressed suicidal patient. Assessment and treatment. Ann N Y Acad Sci 2001;932:1-23. [DOI] [PubMed]
- 32.Joffe R, Sokolov S, Streiner D. Antidepressant treatment of depression: a meta-analysis. Can J Psychiatry 1996;41:613-6. [DOI] [PubMed]
- 33.Moller HJ, Fuger J, Kasper S. Efficacy of new generation antidepressant: meta-analysis of imipramine-controlled studies. Pharmacopsychiatry 1994; 27: 215-23. [DOI] [PubMed]
- 34.Judd LL, Paulus MJ, Schettler PJ, Akiskal HS, Endicott J, Leon AC, et al. Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? Am J Psychiatry 2000;157:1501-4. [DOI] [PubMed]
- 35.Kennedy SH, Lam RW, Cohen NL, Ravindran AV, and the CANMAT Depression Work Group. Clinical guidelines for the treatment of depressive disorders. IV. Medications and other biological treatments. Can J Psychiatry 2001;46(Suppl 1):38S-58S. [PubMed]
- 36.American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder (revision). Am J Psychiatry 2000;157(4 Suppl):1-45. [PubMed]
- 37.Trindade E, Menon D, Topfer LA, Coloma C. Adverse effects associated with selective serotonin reuptake inhibitors and tricyclic antidepressents: a meta-analysis. CMAJ 1998;159(10):1245-52. [PMC free article] [PubMed]
- 38.Jefferson JW. Drug interactions — Friend or foe? J Clin Psychiatry 1998;59 (Suppl 4):37-47. [PubMed]
- 39.Nierenberg AA, McLean NE, Alpert JG, Worthington JJ, Rosenbaum JF, Fava M. Early non-response to fluoxetine as a predictor of poor 8 week outcome. Am J Psychiatry 1995;152:1500-3. [DOI] [PubMed]
- 40.Bauer M, Dopfiner S. Lithium augmentation in treatment-resistant depression: meta-analysis of placebo-controlled studies. J Clin Psychopharmacol 1999; 19:427-34. [DOI] [PubMed]
- 41.Altshuler LL, Bauer M, Frye MA, Gitlin MJ, Mintz J, Szuba MP, et al. Does thyroid supplementation accelerate tricyclic antidepressant response? A review and meta-analysis of the literature. Am J Psychiatry 2001;158:1617-22. [DOI] [PubMed]
- 42.Warneke L. Psychostimulants in psychiatry. Can J Psychiatry 1990;35:3-10. [DOI] [PubMed]
- 43.Gerson S, Belin TR, Kaufman A, Mintz J, Jarvik L. Pharmacological and psychological treatments for depressed older patients: a meta-analysis and overview of recent findings. Harv Rev Psychiatry 1999;7(1):1-28. [PubMed]
- 44.Stewart DE. Antidepressant drugs during pregnancy and lactation. Int Clin Psychopharmacol 2000;15(Suppl 3):S19-24. [PubMed]
- 45.Cohen LS, Rosenbaum JF. Psychotropic drug use during pregnancy: weighing the risks. J Clin Psychiatry 1998;59(Suppl 2):18-28. [PubMed]
- 46.Misri S, Kostaras D, Kostaras X. The use of selective serotonin reuptake inhibitors during pregnancy and lactation: current knowledge. Can J Psychiatry 2000;45(3):285-7. [DOI] [PubMed]
- 47.Mueller TI, Leon AC, Keller MB, Solomon DA, Endicott J, Coryell W, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry 1999;156(7):1000-6. [DOI] [PubMed]
- 48.Remick RA. Long term pharmacological treatment of mood disorders. In: Ancill R, Lader M, Tindall B, editors. Pharmacological management of chronic psychiatric disorders. London: Balliere Tindall; 1995. p. 553-63.
- 49.Haddad P. The SSRI discontinuation syndrome. J Psychopharmacol 1998;12: 305-13. [DOI] [PubMed]
- 50.Potter WZ, Rudorfer MV. Electroconvulsive therapy — a modern medical procedure [editorial]. N Engl J Med 1993;328:882-3. [DOI] [PubMed]
- 51.Kraus RP, Chandarana P. “Say, are you psychiatrists still using ECT?” CMAJ 1997;157:1375-7. [PMC free article] [PubMed]
- 52.Sackeim HA, Luber B, Katzman GP, Moeller JR, Prudic J, Devanand DP, et al. The effects of electroconvulsive therapy on quantitative electroencephalograms. Relationship to clinical outcome. Arch Gen Psychiatry 1996;53:814-24. [DOI] [PubMed]
- 53.Lam RW, Levitt AJ. Canadian consensus guidelines for the treatment of seasonal affective disorder. Vancouver: Clinical & Academic Publishing; 1999.
- 54.Linde K, Ramirez G, Mulrow CD, Pauls A, Weidenhammer W, Melchart D. St. John's wort for depression — an overview and meta-analysis of randomised clinical trials. BMJ 1996;313:253-8. [DOI] [PMC free article] [PubMed]
- 55.Shelton RC, Keller MB, Gelenberg A, Dunner DL, Hirschfeld R, Thase ME, et al. Effectiveness of St John's wort in major depression: a randomized controlled trial. JAMA 2001;285:1978-86. [DOI] [PubMed]
- 56.Lawlor DA, Hopker SW. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta-regression analysis of randomised controlled trials. BMJ 2001;322:763-7. [DOI] [PMC free article] [PubMed]
- 57.Wirz-Justice A, van den Hoofdakker RH. Sleep deprivation in depression: What do we know, where do we go? Biol Psychiatry 1999;46:445-53. [DOI] [PubMed]
- 58.Bridges PK, Bartlett JR, Hale AS, Poynton AM, Malizia AL, Hodgkiss AD. Psychosurgery: stereotactic subcaudate tractomy. An indispensable treatment. Br J Psychiatry 1994;165:599-611. [DOI] [PubMed]
- 59.George MS, Sackeim HA, Marangell LB, Husain MM, Nahas Z, Lisanby SH, et al. Vagus nerve stimulation. A potential therapy for resistant depression? Psychiatr Clin North Am 2000;23:757-83. [DOI] [PubMed]
- 60.Hasey G, Joffe R, Ivanski C. Managing neuropsychiatic disease with transcranial magnetic stimulation. CMAJ 2000;162:78-80. [PMC free article] [PubMed]
- 61.Keller MB, McCullough JP, Klein DN, Arrow B, Dunner DL, Gelenberg AJ, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med 2000;342:1462-70. [DOI] [PubMed]
- 62.Ravindran AV, Anisman H, Merali Z, Charbonneau Y, Telner J, Bialik RJ, et al. Treatment of primary dysthymia with group cognitive therapy and pharmacotherapy: clinical symptoms and functional impairments. Am J Psychiatry 1999;156:1608-17. [DOI] [PubMed]
- 63.Frank E, Grochocinski VJ, Spanier CA, Buysse DJ, Cherry CR, Houck PR, et al. Interpersonal psychotherapy and antidepressant medication: evaluation of a sequential treatment strategy in women with recurrent major depression. J Clin Psychiatry 2000;61:51-7. [PubMed]
- 64.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979.
- 65.Greenberg D, Padesky CA. Mind over mood. New York: Guilford Press; 1995.
- 66.Weissman MM, Markowitz JC, Klerman GL. A comprehensive guide to interpersonal psychotherapy. New York: Basic Books; 2000.
- 67.Segal ZV, Kennedy SH, Cohen NL, and the CANMAT Depression Work Group. Clinical guidelines for the treatment of depressive disorders. V. Combining psychotherapy and pharmacotherapy. Can J Psychiatry 2001;46(Suppl 1):59S-62S. [PubMed]


