Case
A 41-year-old man presents for assessment of severe hypertriglyceridemia. He has previously been well. His lipid levels were checked because his serum appeared milky on screening for dyslipidemia. He has no history of abdominal pains, his medical history is unremarkable (in particular, no diabetes mellitus, hypothyroidism, obesity or pancreatitis), and he has no family history of premature coronary artery disease. He does not drink alcohol excessively and is a nonsmoker. The physician records his height (180 cm), weight (80 kg) and abdominal circumference (86 cm). Other findings on physical examination are unremarkable. The fasting lipid profile reveals a total cholesterol level of 7.8 (normally < 5.2) mmol/L, a high-density lipoprotein (HDL) cholesterol level of 0.5 (normally > 0.9) mmol/L and a triglyceride level of 30.2 (normally < 2.3) mmol/L. The patient had previously received treatment with 2 statins, in increasing doses, without a decrease in triglycerides.
How should the patient's lipid profile be classified? What other investigations should be performed? How should the patient's dyslipidemia be managed?
North Americans consume 100 g of fat per day on average, or about one-third of their total daily energy intake. This fat is absorbed in the intestine as free fatty acids and combines with glycerol to form triglycerides. These lipids are assembled as chylomicrons (Fig. 1). Apolipoprotein B (apo B) is essential for the assembly and secretion of chylomicrons and very-low-density liprotein (VLDL). Chylomicrons exchange surface components with high-density lipoproteins (HDL) and acquire apo C-II and apo E in the process. Apolipoproteins are structural proteins that are noncovalently bound to the lipids. They contain either receptor binding sites, or activators or inhibitors of key enzymes of lipoprotein metabolism. Apo E is required for the normal removal of triglyceride-rich particles from the blood via hepatic apo E receptors. Apo C-II activates lipoprotein lipase, which hydrolyzes the core triglycerides and releases free fatty acids. The ratio of apo C-II (activator) to apo C-III (inhibitor) determines the activity of lipoprotein lipase, affecting the rate of clearance of chylomicrons and VLDL. The triglyceride component of chylomicrons is removed by lipoprotein lipase. The resulting chylomicron remnants are cleared by the liver via receptors that recognize apo E, which is a high-affinity ligand.

Fig. 1: Triglyceride pathway. The gut produces chylomicrons following the absorption of fat. The triglyceride (TG) component of chylomicrons is removed by lipoprotein lipase located on the vascular endothelium of muscle, myocardium and adipose tissue. The resulting chylomicron remnants are cleared from the circulation by hepatic receptors that recognize apolipoprotein E (apo E). The liver exports triglycerides into the circulation in the core of very-low-density lipoprotein (VLDL) particles. Photo: Paulette Dennis
Severe hypertriglyceridemia is of concern because it can predispose to pancreatitis. Mild to moderate hypertriglyceridemia is often associated with a metabolic syndrome that increases the risk of coronary artery disease. Use of inappropriate lipid-lowering agents to treat moderate to severe hypertriglyceridemia (fasting triglyceride levels > 5.0 mmol/L) is one of the most common pitfalls in the management of dyslipidemia. In this review, we will focus on the causes, diagnosis and management of hypertriglyceridemia.
Risks associated with hypertriglyceridemia
Although mild hypertriglyceridemia is often asymptomatic, severe primary hypertriglyceridemia (triglyceride level > 10.0 mmol/L) can be associated with several clinical manifestations (chylomicronemia syndrome), including abdominal pain, pancreatitis, difficulties with short-term memory and flushing with alcohol. The pathogenesis of acute pancreatitis in this setting is unclear. It is thought that extravascular chylomicrons in the pancreas cause the release of free fatty acids, which start the inflammation cascade.1 Physical findings include eruptive xanthomas, lipemia retinalis and hepatosplenomegaly. Plasma taken from people with severe hypertriglyceridemia appears milky. When refrigerated overnight, it separates into a creamy supernatant and clear infranatant.
Studies have shown that even mildly elevated triglyceride levels may be a predictor of coronary artery disease. In the Physicians' Health Study, triglyceride levels were found to be strongly correlated with the total cholesterol:HDL cholesterol ratio, inversely correlated with LDL size (small, dense LDL particles, LDL phenotype B) and inversely correlated with HDL cholesterol levels. After adjustment for lipid levels and other risk factors for coronary artery disease, triglyceride levels were significantly and linearly correlated with incident myocardial infarction.2
The reason why elevated triglyceride levels are associated with coronary artery disease is complex. Mild to moderate hypertriglyceridemia may increase the risk of premature coronary artery disease, in part because of several metabolic abnormalities that often accompany mild to moderate elevations in triglyceride levels (Box 1).
Box 1.
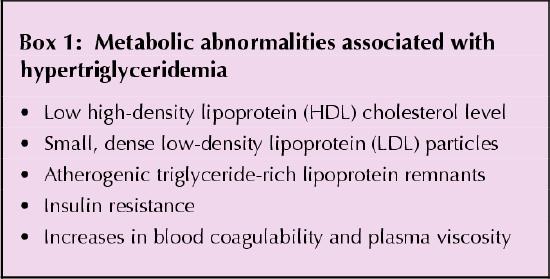
After adjustment for serum HDL cholesterol levels, high triglyceride concentrations have been shown to be a significant but modest independent predictor of cardiovascular disease in both men and women (relative risk 1.14 and 1.37 respectively).3 The relation of serum triglycerides to HDL cholesterol, particularly when expressed as log(triglyceride/HDL cholesterol), is called the atherogenic index of plasma (AIP) and correlates positively with the lipoprotein particle size and likelihood of coronary artery disease.4 Although people at low risk of coronary artery disease have AIP values in the negative range, those at higher risk have progressively increasing positive values.
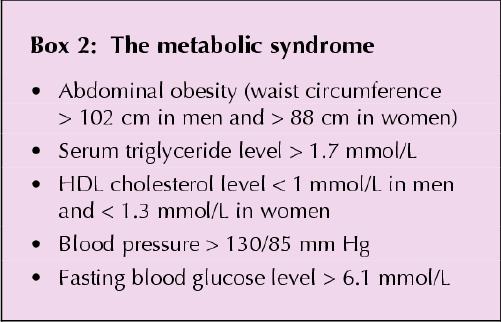
Clinically, the “hypertriglyceridemic waist,” which is often associated with the atherogenic metabolic syndrome (or syndrome X) (Box 2), may be the most helpful indicator of high risk for coronary artery disease. A waist measurement of more than 100–102 cm in men and 88–90 cm in women provides useful reference values to identify obese patients at high risk of the atherogenic metabolic syndrome.5 Patients with the syndrome have a greater rate of progression to coronary artery disease and a 2-fold higher frequency of clinical events (myocardial infarction, stroke, revascularization or death from coronary artery disease) over 15–20 years than those without the syndrome.6
Box 2.
Causes
Hypertriglyceridemia may be the result of either genetic defects (primary causes) or, more commonly, acquired factors (secondary causes) such as obesity, alcohol consumption, diabetes mellitus, hypothyroidism or the use of certain medications that increase triglyceride production or decrease its clearance or both (Table 1). The degree of triglyceride elevation may be helpful in predicting the likelihood that a genetic defect is involved.
Table 1
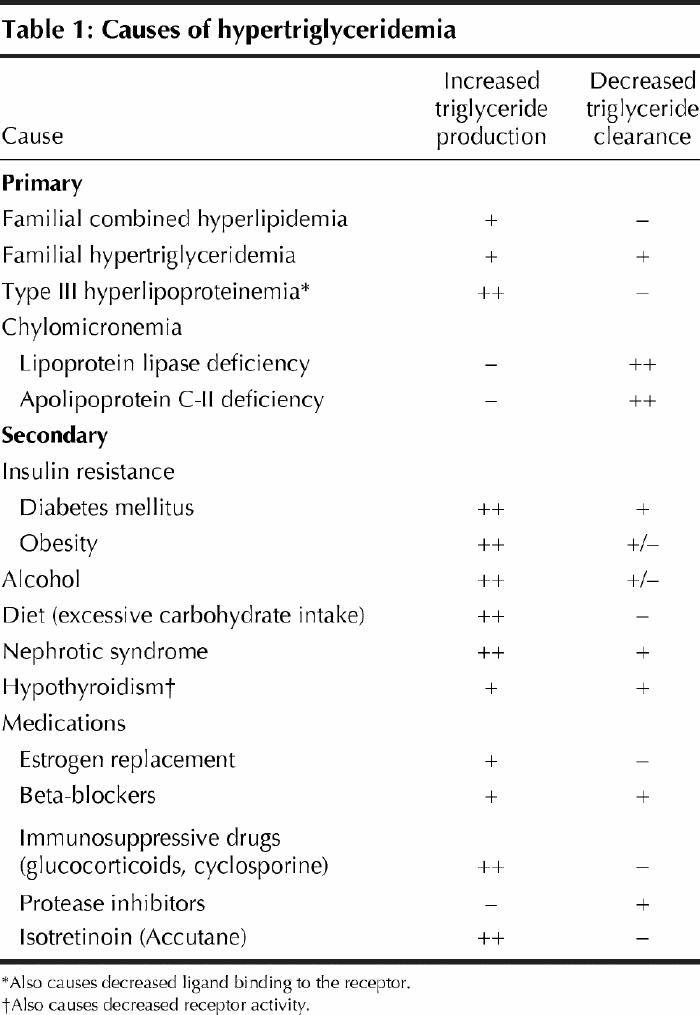
The 2 main genetic disorders that cause mild or moderate hypertriglyceridemia (triglyceride level 2.0–5.0 mmol/L or 5.0–10.0 mmol/L respectively) are familial combined hyperlipidemia and familial hypertriglyceridemia. Familial combined hyperlipidemia is the most common lipoprotein disorder, occurring in 1 in 150 adults.1 It results from the overproduction of hepatically derived apo B-100 associated with VLDL. The plasma apo B concentration is usually above 1.2 g/L. Familial combined hyperlipidemia is associated with a significant increase in risk of coronary artery disease and accounts for one-third to one-half of familial causes of coronary artery disease.7 Affected patients typically present with one or both of hypercholesterolemia and hypertriglyceridemia (triglyceride level usually 2.0–5.0 mmol/L). Familial hypertriglyceridemia is an autosomal dominant disorder associated with mild to moderate elevations in serum triglyceride levels (usually 2.0–10.0 mmol/L). Affected patients are usually heterozygous for inactivating mutations of the lipoprotein lipase gene and typically have low serum HDL cholesterol levels. Their serum apo-B levels are not elevated, and their risk for coronary artery disease is not greatly increased.
Severe hypertriglyceridemia (triglyceride level > 10.0 mmol/L) occurs in about 1 in 1000 adults, and much less frequently in children.1 Chylomicrons and VLDL compete for the same clearance mechanism, lipoprotein lipase. Severe hypertriglyceridemia is usually related to complete or partial lipoprotein lipase deficiency. The condition can also develop when an increase in hepatic VLDL production occurs in combination with a decrease in clearance. This combination may be due to either genetic or acquired factors such as obesity, diabetes, alcohol intake or estrogen use. Decreased triglyceride clearance may also be acquired or inherited (Table 1). Acquired causes (e.g., hypothyroidism, β-blocker use and diabetes) result in both an overproduction of VLDL and decreased lipoprotein lipase activity. The 2 main disorders associated with severe hypertriglyceridemia are dysbetalipoproteinemia (type III hyperlipoproteinemia) and chylomicronemia.
Dysbetalipoproteinemia is a multifactorial disorder that is inherited as an autosomal recessive trait. It is usually characterized by the presence of 2 apo E2 alleles. Remnant lipoprotein particles are the main triglyceride-rich particles in the plasma of these patients. An additional genetic or acquired factor that increases lipoprotein production or impairs lipoprotein clearance (e.g., diabetes, hypothyroidism or obesity) is typically required for full clinical expression. Premature coronary artery disease and peripheral vascular disease are common in affected patients. Physical findings include tuberoeruptive xanthomas and xanthomas of the palmar creases (xanthoma striatum palmare).
Chylomicronemia is characterized by fasting serum triglyceride levels greater than 10.0 mmol/L. Plasma samples from affected patients separate into a creamy supernatant and clear infranatant after refrigeration. The primary form of this condition is caused by a deficiency in lipoprotein lipase or its activator apo C-II, which results in complete absence of lipoprotein lipase activity. However, patients may have a secondary form in which some other dyslipidemia (e.g., familial hypertriglyceridemia due to partial lipoprotein lipase deficiency) is exacerbated by an acquired factor.
Hemorrhagic pancreatitis is the most serious, life-threatening complication of severe hypertriglyceridemia, particularly if it occurs in pregnancy.
Patients with elevated triglyceride levels should be investigated for secondary causes. The differential diagnosis for primary triglyceride disorders and associated degree of hypertriglyceridemia is summarized in Table 2.
Table 2

Diagnosis
Routine screening for dyslipidemia with a fasting lipid profile (total cholesterol, HDL cholesterol, triglyceride and calculated LDL cholesterol levels) is recommended in the following patients:8
· Men over 40 years of age
· Women over 50 years
· Adults with 2 or more risk factors for coronary artery disease
· People with clinical evidence of coronary artery disease, peripheral vascular disease or carotid artery disease
· People with diabetes mellitus
· People with xanthomas or other stigmas of dyslipidemia
· People with a family history of dyslipidemia or coronary artery disease
Laboratory investigations to exclude secondary disorders of lipid metabolism should include measurement of fasting blood glucose, serum creatinine, thyroid stimulating hormone and apo B levels. Apo B levels will help differentiate between the less atherogenic condition familial hypertriglyceridemia and the more atherogenic condition familial combined hypertriglyceridemia.9,10,11
Additional investigations may include assessment of lipoprotein lipase activity, apo C-II levels and apo E genotyping to confirm one of the inherited disorders. The results may be important for the management of patients and for family counselling. Specialized centres such as lipid clinics can be consulted to perform these tests and interpret the results.
Management
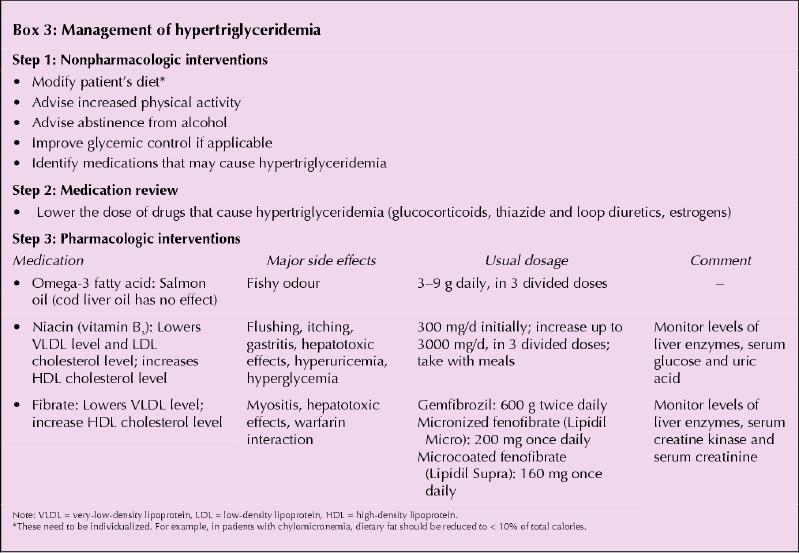
An approach to the management of hypertriglyceridemia is summarized in Box 3. All reversible causes should be treated. This may include improving glycemic control in patients with diabetes, treating hypothyroidism and stopping the use of medications that may cause elevated triglyceride levels. In addition, patients should be encouraged to increase their level of physical activity, decrease their waist circumference and achieve an ideal body mass index (20–27 kg/m2), decrease alcohol consumption and, if possible, abstain from alcohol, and follow a low-fat diet (fat intake less than 10% of total dietary energy intake per day). Referral to a nutritionist may be necessary to accomplish this goal.12
Box 3.
Drug therapy
The most effective triglyceride-lowering drugs are fibric acid derivatives and niacin. These drugs also raise HDL cholesterol levels, which are often reduced in patients with hypertriglyceridemia.
Fibrates
Fibrates are generally very well tolerated. They activate a class of nuclear receptors known as peroxisome proliferator-activated receptor alpha (PPAR-α).13 This results in increased production of lipoprotein lipase and of apo A-I and A-II, which are the 2 main proteins of HDL. LDL cholesterol levels may initially increase after fibrate therapy is started, but the average particle size also increases. Because of the concern regarding hepatic side effects and rhabdomyolysis, close follow-up with liver enzyme tests and creatine kinase measurement are recommended 6 weeks after starting fibrate therapy and every 3 to 6 months thereafter, or if symptoms appear. The need for this surveillance has been disputed but is currently recommended by the manufacturers of fibrates. The risk of side effects may be increased if fibrate therapy is combined with statin therapy.14,15
Niacin
Niacin is a member of the vitamin B family (vitamin B3). Its mechanism of action is illustrated in Fig. 2. Niacin inhibits the mobilization of free fatty acids from peripheral adipose tissue to the liver. Side effects of niacin include elevated liver enzyme levels, glucose intolerance and flushing. Follow-up liver enzyme tests are recommended 6 weeks after starting niacin therapy and every 3 to 6 months thereafter. Niacin is not contraindicated in patients with diabetes if there is cautious follow-up of glycemic control. Flushing can be diminished with the use of ASA 30 minutes to 1 hour before ingestion of niacin. Sustained-release preparations of niacin with improved flushing profiles are also available. Niacin is available over the counter. The starting dose is usually 100 mg 3 times daily, with meals, and should be gradually increased to the target dose or a maximum of 1000 mg 3 times daily.
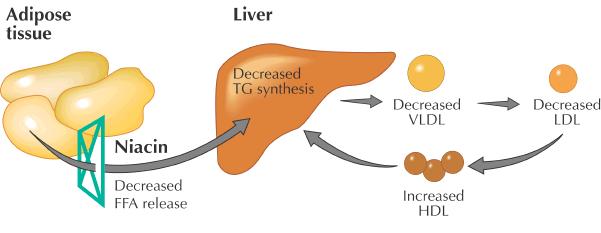
Fig. 2: Mechanism of niacin action. Niacin inhibits the release of free fatty acids from adipose tissue, which leads to decreased VLDL secretion by the liver. FFA = free fatty acids, TG = triglycerides, VLDL = very-low-density lipoprotein, LDL = low-density lipoprotein, HDL = high-density lipoprotein. Photo: Paulette Dennis
Omega-3 fatty acids
Some patients may benefit from omega-3 fatty acids16 (docosapentaenoic acid and eicosapentaenoic acid) found in salmon oil supplements. Omega-3 fatty acids reduce VLDL production and thus result in decreased serum triglyceride levels. Salmon oil is available over the counter in 1-g capsules. The starting dose is 1 g twice daily and can be increased to 3 g three times daily.
Bile acid sequestrants
Bile acid sequestrants should be avoided until triglyceride levels return to normal, since they can increase VLDL synthesis and exacerbate the hypertriglyceridemia.
A note regarding statins
Most patients with dyslipidemia considered for drug treatment will have a combined increase in cholesterol and usually a mildly elevated (< 5.0 mmol/L) triglyceride level (familial combined hypertriglyceridemia). In such patients, a statin may be used as the first-line treatment because of its cholesterol- and triglyceride-lowering effect and the strong evidence for prevention of coronary artery disease.
Treatment targets
For mild to moderate hypertriglyceridemia the current treatment target is a fasting triglyceride level below 3.0 mmol/L in low-risk patients (10-year risk < 10%) and below 2.0 mmol/L in all other patients.8 This degree of hypertriglyceridemia is seen commonly, usually as part of the metabolic syndrome that also includes insulin resistance, small dense LDL particles, decreased HDL cholesterol levels, and borderline to high blood pressure. It is associated with an increased risk of coronary artery disease. Management includes treatment of secondary causes, changes in diet and lifestyle and, depending on the degree of hypertriglyceridemia, use of statins, fibrates, niacin and salmon oil. Statins are not often prescribed for patients with elevated triglyceride levels, but they may be used if the LDL cholesterol level is also elevated.
For severe hypertriglyceridemia, patients are at increased risk of pancreatitis and, in the long term, may also be at increased risk of coronary artery disease. However, the conventional risk assessment based on Framingham data is not applicable in cases of severe dyslipidemias. Target triglyceride levels may not be achieved, but the initial goal should be to maintain fasting triglyceride levels below 10.0 mmol/L, and subsequently below 3.0 mmol/L.17 A very-low-fat diet (total fat intake < 10% of total daily energy intake), abstinence from alcohol and treatment with fibrates, niacin and salmon oil are recommended.
Case revisited
This patient's most serious risk is acute hemorrhagic pancreatitis. His long-term risk for vascular disease is relatively low, although higher than that in the general population. The multiple statin therapy had failed to improve his lipid profile and was discontinued. Although statins may reduce triglyceride levels, they are not appropriate for severe hypertriglyceridemia. Statins are rarely effective in normalizing triglyceride levels when the fasting level is greater than 5.0 mmol/L. The patient underwent testing for lipoprotein lipase activity. He was found to have chylomicronemia due to deficient lipoprotein lipase activity and was given a low-fat diet to follow. Therapy with a fibrate (micronized fenofibrate, 200 mg/d) was started. The fasting serum triglyceride level remained elevated, and so salmon oil (5 g/d) was added to the fibrate therapy. At follow-up his triglyceride level was decreased (2.0 mmol/L), the HDL cholesterol level was increased (0.9 mmol/L), and the total cholesterol level was decreased (5.1 mmol/L).
Footnotes
This article has been peer reviewed.
Contributors: Drs. Fung and Frohlich both contributed to the conception and design of the paper. Dr. Fung drafted the article. Dr. Frohlich revised it critically for important intellectual content. Both authors gave final approval of the version to be published.
Competing interests: None declared for Dr. Fung. Dr. Frohlich has participated in educational and research activities supported by manufacturers of lipid-lowering drugs.
Correspondence to: Dr. Jiri J. Frohlich, Healthy Heart Lipid Clinic, St. Paul's Hospital, 180–1081 Burrard St., Vancouver BC V6Z 1Y6; fax 604 806-8590
References
- 1.Lipids. In: Scriver CR, Beaudet AL, Sly WS, Valle D, editors. The metabolic and molecular basis of inherited disease. 8th ed. New York: McGraw-Hill; 2001. p. 2703-988.
- 2.Stampfer MJ, Krauss RM, Ma J, Blanche PJ, Holl LG, Sacks FM, et al. A prospective study of triglyceride level, low-density lipoprotein particle diameter, and risk of myocardial infarction. JAMA 1996;276:882. [PubMed]
- 3.Austin MA, Hokanson JE, Edwards KL. Hypertriglyceridemia as a cardiovascular risk factor. Am J Cardiol 1998;81:7B. [DOI] [PubMed]
- 4.Dobiasova M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FERHDL). Clin Biochem 2001:34:583-8. [DOI] [PubMed]
- 5.Zhao XQ, Morse J, Chait A, Fisher L, Dowdy A, Albers J, et al. Simvistatin plus niacin protect against atherosclerosis progression and clinical events in coronary artery disease patients with metabolic syndrome [abstract 1130-73]. J Am Coll Cardiol 2002;39(5, Suppl A).
- 6.Despres JP, Lemieux I, Prud'homme D. Treatment of obesity: need to focus on high risk abdominally obese patients. BMJ 2001;332:716-20. [DOI] [PMC free article] [PubMed]
- 7.Sniderman AD, Bergeron J, Frohlich J. Apolipoprotein B versus lipoprotein lipids: vital lessons from the AFCAPS/TexCAPS trial. CMAJ 2001:164(1):44-7. [PMC free article] [PubMed]
- 8.Fodor J, Frohlich J, Genest J, McPherson R, for the Working Group on Hypercholesterolemia and Other Dyslipidemias. Recommendations for the management and treatment of dyslipidemia. CMAJ 2000;162(10):1441-7. [PMC free article] [PubMed]
- 9.Cantin B, Gagnon F, Moorjani S, Despres JP, Lamarche B, Lupien PJ, Dagenais GR. Is lipoprotein(a) an independent risk factor for ischemic heart disease in men? The Quebec Cardiovascular Study. J Am Coll Cardiol 1998;31(3):519-25. [DOI] [PubMed]
- 10.Dagenais GR, Robitaille NM, Lupien PJ, Christen A, Gingras S, Moorjani S, et al. First coronary heart disease event rates in relation to major risk factors: Quebec cardiovascular study. Can J Cardiol 1990;6(7):274-80. [PubMed]
- 11.Dagenais GR, Ahmed Z, Robitaille NM, Gingras S, Lupien PJ, Christen A, et al. Total and coronary heart disease mortality in relation to major risk factors — Quebec cardiovascular study. Can J Cardiol 1990;6(2):59-65. [PubMed]
- 12.Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;16:285(19):2486-97. [DOI] [PubMed]
- 13.Fruchart JC. Duriez P. Staels B. Peroxisome proliferator-activated receptor-alpha activators regulate genes governing lipoprotein metabolism, vascular inflammation and atherosclerosis. Curr Opinion Lipidol 1999;10(3):245-57. [DOI] [PubMed]
- 14.Wooltorton E. Bayer pulls cerivastatin (Baycol) from market. CMAJ 2001; 165 (5):632. [PMC free article] [PubMed]
- 15.Herman RJ. Drug interactions and the statins. CMAJ 1999; 161(10):1281-6. [PMC free article] [PubMed]
- 16.Holub BJ. Clinical nutrition: 4. Omega-3 fatty acids in cardiovascular care. CMAJ 2002;166(5):608-15. [PMC free article] [PubMed]
- 17.Benlian P, De Gennes JL, Foubert L, Zhang H, Gagne SE, Hayden M. Premature atherosclerosis in patients with familial chylomicronemia caused by mutations in the lipoprotein lipase gene. N Engl J Med 1996;19:335(12):848-54. [DOI] [PubMed]


