Abstract
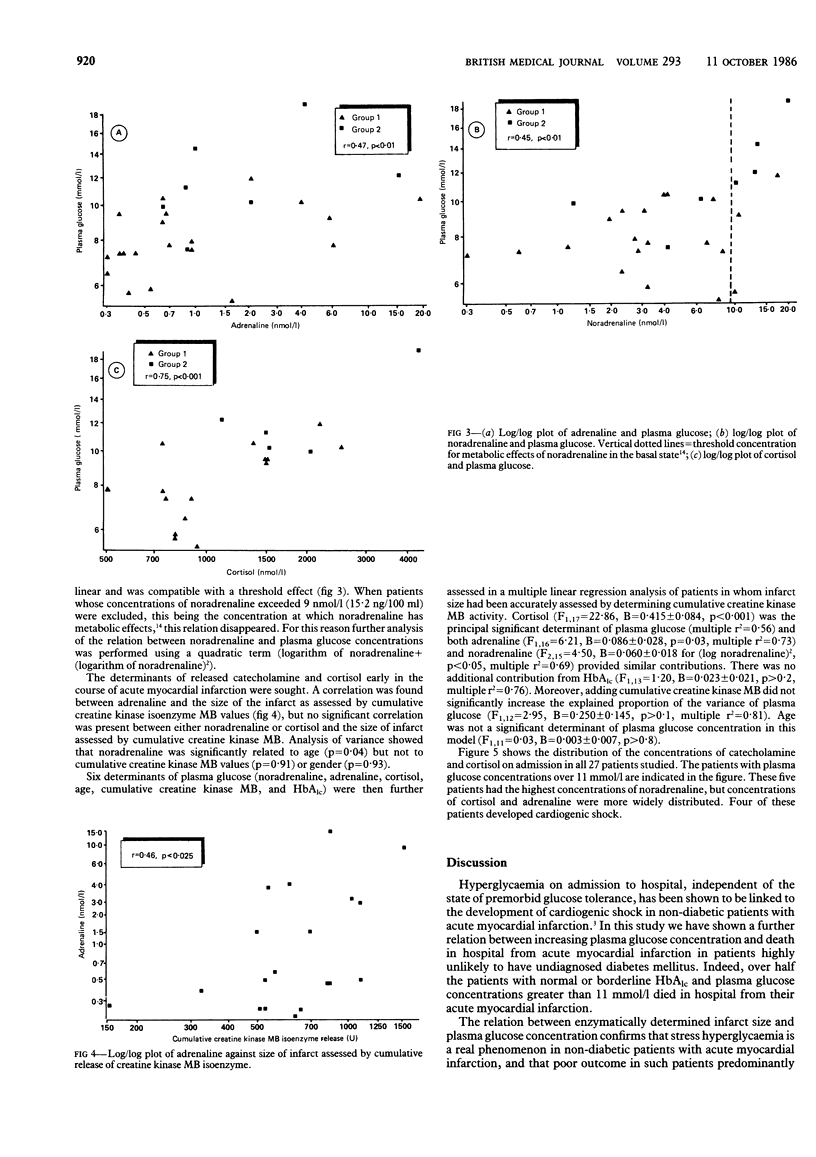
Determinants of plasma glucose concentrations were studied in patients on admission to hospital with confirmed acute myocardial infarction but without previous glucose intolerance as evidenced by raised concentrations of glycosylated haemoglobin (HbAlc). Mortality in hospital increased significantly with increasing plasma concentrations of glucose in patients with both normal (p less than 0.0001, n = 311) and borderline (p less than 0.02, n = 70) concentrations of HbAlc. There was a weak relation between plasma glucose concentrations and infarct size as estimated by peak aspartate transaminase activity in both HbAlc groups (rs = 0.26, n = 101 and rs = 0.41, n = 35 respectively). A correlation was found between adrenaline and plasma glucose concentrations (r = 0.47, n = 27) and cortisol and plasma glucose concentrations (r = 0.75, n = 19), but the relation of plasma noradrenaline and plasma glucose suggested a threshold effect. Concentrations of adrenaline, but not those of noradrenaline or cortisol, correlated with infarct size as measured both by peak aspartate transaminase activity and cumulative release of creatine kinase MB isoenzyme. Multiple regression analysis showed that concentrations of cortisol, adrenaline, and noradrenaline (but not the concentration of HbAlc, infarct size, or age) are the main determinants of plasma glucose concentration measured in non-diabetic patients when admitted to hospital after acute myocardial infarction.
Full text
PDF




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Benedict C. R., Grahame-Smith D. G. Plasma adrenaline and noradrenaline concentrations and dopamine-beta-hydroxylase activity in myocardial infarction with and without cardiogenic shock. Br Heart J. 1979 Aug;42(2):214–220. doi: 10.1136/hrt.42.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle D. M., Barber J. M., McIlmoyle E. L., Salathia K. S., Evans A. E., Cran G., Elwood J. H., Shanks R. G. Effect of very early intervention with metoprolol on myocardial infarct size. Br Heart J. 1983 Mar;49(3):229–233. doi: 10.1136/hrt.49.3.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burckhardt P., Felber J. P., Perret C. Adrenocortical, insulin and metabolic changes in response to acute myocardial infarction. Helv Med Acta. 1972;36(4):277–293. [PubMed] [Google Scholar]
- Christensen N. J., Videbaek J. Plasma catecholamines and carbohydrate metabolism in patients with acute myocardial infarction. J Clin Invest. 1974 Aug;54(2):278–286. doi: 10.1172/JCI107763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R. S., English M., McNeill G. P., Newton R. W. Effect of intravenous infusion of insulin in diabetics with acute myocardial infarction. Br Med J (Clin Res Ed) 1985 Aug 3;291(6491):303–305. doi: 10.1136/bmj.291.6491.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn J. N., Levine T. B., Olivari M. T., Garberg V., Lura D., Francis G. S., Simon A. B., Rector T. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med. 1984 Sep 27;311(13):819–823. doi: 10.1056/NEJM198409273111303. [DOI] [PubMed] [Google Scholar]
- Gwilt D. J., Petri M., Lamb P., Nattrass M., Pentecost B. L. Effect of intravenous insulin infusion on mortality among diabetic patients after myocardial infarction. Br Heart J. 1984 Jun;51(6):626–630. doi: 10.1136/hrt.51.6.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husband D. J., Alberti K. G., Julian D. G. Methods for the control of diabetes after acute myocardial infarction. Diabetes Care. 1985 May-Jun;8(3):261–267. doi: 10.2337/diacare.8.3.261. [DOI] [PubMed] [Google Scholar]
- Karlsberg R. P., Cryer P. E., Roberts R. Serial plasma catecholamine response early in the course of clinical acute myocardial infarction: relationship to infarct extent and mortality. Am Heart J. 1981 Jul;102(1):24–29. doi: 10.1016/0002-8703(81)90408-7. [DOI] [PubMed] [Google Scholar]
- Little R. A., Frayn K. N., Randall P. E., Stoner H. B., Yates D. W., Laing G. S., Kumar S., Banks J. M. Plasma catecholamines in patients with acute myocardial infarction and in cardiac arrest. Q J Med. 1985 Feb;54(214):133–140. [PubMed] [Google Scholar]
- Longstreth W. T., Jr, Diehr P., Inui T. S. Prediction of awakening after out-of-hospital cardiac arrest. N Engl J Med. 1983 Jun 9;308(23):1378–1382. doi: 10.1056/NEJM198306093082302. [DOI] [PubMed] [Google Scholar]
- McMillan D. E. The effect of diabetes on blood flow properties. Diabetes. 1983 May;32 (Suppl 2):56–63. doi: 10.2337/diab.32.2.s56. [DOI] [PubMed] [Google Scholar]
- Mortensen H. B. Quantitative determination of hemoglobin A1c by thin-layer isoelectric focusing. J Chromatogr. 1980 Jun 13;182(3-4):325–333. doi: 10.1016/s0378-4347(00)81481-4. [DOI] [PubMed] [Google Scholar]
- Oswald G. A., Corcoran S., Yudkin J. S. Prevalence and risks of hyperglycaemia and undiagnosed diabetes in patients with acute myocardial infarction. Lancet. 1984 Jun 9;1(8389):1264–1267. doi: 10.1016/s0140-6736(84)92447-4. [DOI] [PubMed] [Google Scholar]
- Proctor D. F., Adams G. K., Andersen I., Man S. F. Nasal mucociliary clearance in man. Ciba Found Symp. 1978;(54):219–234. doi: 10.1002/9780470720356.ch11. [DOI] [PubMed] [Google Scholar]
- Shapiro L. M., Howat A. P., Calter M. M. Left ventricular function in diabetes mellitus. I: Methodology, and prevalence and spectrum of abnormalities. Br Heart J. 1981 Feb;45(2):122–128. doi: 10.1136/hrt.45.2.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverberg A. B., Shah S. D., Haymond M. W., Cryer P. E. Norepinephrine: hormone and neurotransmitter in man. Am J Physiol. 1978 Mar;234(3):E252–E256. doi: 10.1152/ajpendo.1978.234.3.E252. [DOI] [PubMed] [Google Scholar]
- Smith C. C., Curtis L. D., Delamothe A. P., Prichard B. N., Betteridge D. J. The distribution of catecholamines between platelets and plasma in normal human subjects. Clin Sci (Lond) 1985 Jul;69(1):1–6. doi: 10.1042/cs0690001. [DOI] [PubMed] [Google Scholar]
- Sobel B. E., Shell W. E. Serum enzyme determinations in the diagnosis and assessment of myocardial infarction. Circulation. 1972 Feb;45(2):471–482. doi: 10.1161/01.cir.45.2.471. [DOI] [PubMed] [Google Scholar]
- Staszewska-Barczak J. The reflex stimulation of catecholamine secretion during the acute stage of myocardial infarction in the dog. Clin Sci. 1971 Nov;41(5):419–439. doi: 10.1042/cs0410419. [DOI] [PubMed] [Google Scholar]
- Thomas J. A., Marks B. H. Plasma norepinephrine in congestive heart failure. Am J Cardiol. 1978 Feb;41(2):233–243. doi: 10.1016/0002-9149(78)90162-5. [DOI] [PubMed] [Google Scholar]
- Thompson P. L., Fletcher E. E., Katavatis V. Enzymatic indices of myocardial necrosis: influence on short- and long-term prognosis after myocardial infarction. Circulation. 1979 Jan;59(1):113–119. doi: 10.1161/01.cir.59.1.113. [DOI] [PubMed] [Google Scholar]
- Videbaek J., Christensen N. J., Sterndorff B. Serial determination of plasma catecholamines in myocardial infarction. Circulation. 1972 Nov;46(5):846–855. doi: 10.1161/01.cir.46.5.846. [DOI] [PubMed] [Google Scholar]
- Willerson J. T., Hutcheson D. R., Leshin S. J., Faloona G. R., Unger R. H. Serum glucagon and insulin levels and their relationship to blood glucose values in patients with acute myocardial infarction and acute coronary insufficiency. Am J Med. 1974 Nov;57(5):747–752. doi: 10.1016/0002-9343(74)90848-1. [DOI] [PubMed] [Google Scholar]


