Abstract
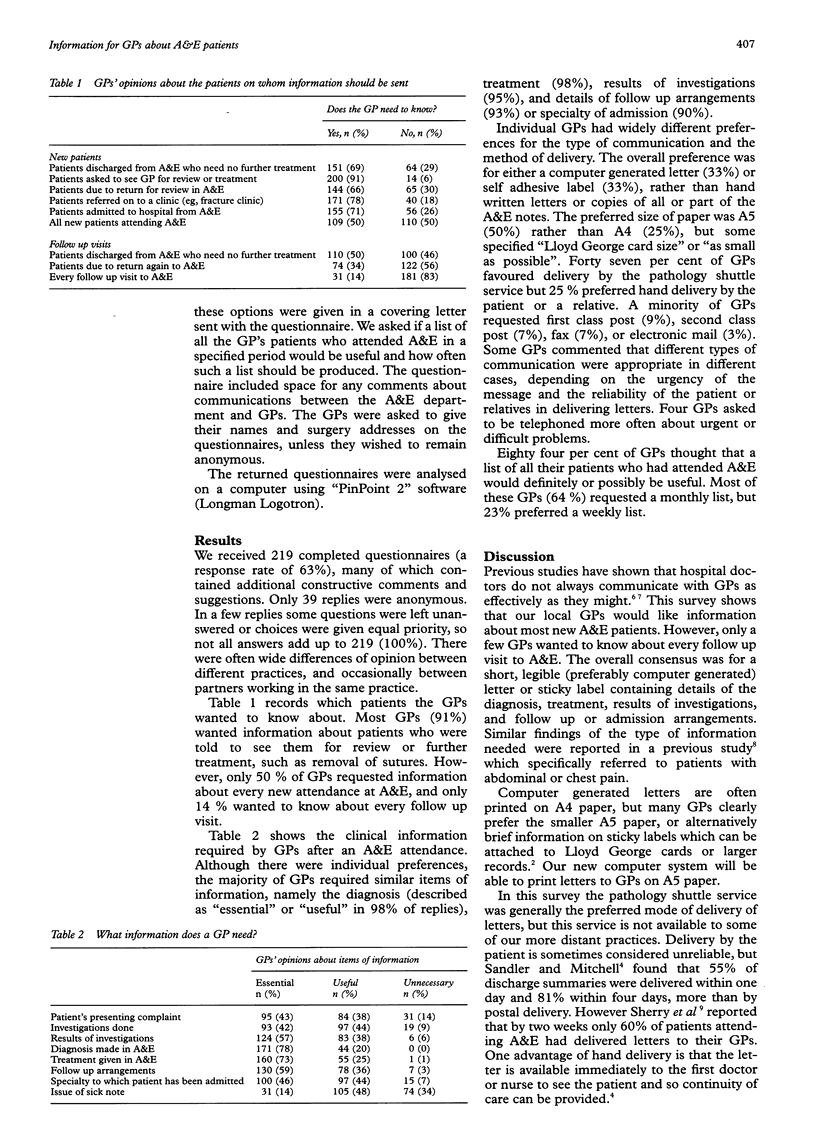
OBJECTIVES: To establish what information general practitioners (GPs) want about their patients who attend accident and emergency (A&E) departments and the GPs' preferences for the type of communication and method of delivery. METHODS: Analysis of questionnaire sent to all 350 GPs in the catchment area of one A&E department. RESULTS: 219 completed questionnaires (63%) were returned. GPs requested information about most new attendances at A&E, but only 50% of GPs wanted details of every new A&E patient. Most GPs preferred a small computer generated letter or sticky label which included details of investigation results, diagnosis, treatment, and follow up arrangements. 47% of GPs requested delivery of letters by the pathology specimen service, but 25% preferred hand delivery by the patient or a relative. Individual GPs often had widely different preferences, especially about the type of communication and method of delivery. Most GPs would value a monthly list of all their patients who have attended A&E. CONCLUSIONS: GPs need prompt and appropriate information about their patients who attend A&E. A computerised records system should be arranged so that relevant information can be produced easily and quickly in a format suitable for filing in GP records. Good communications with GPs would improve the continuity of care for A&E patients.
Full text
PDF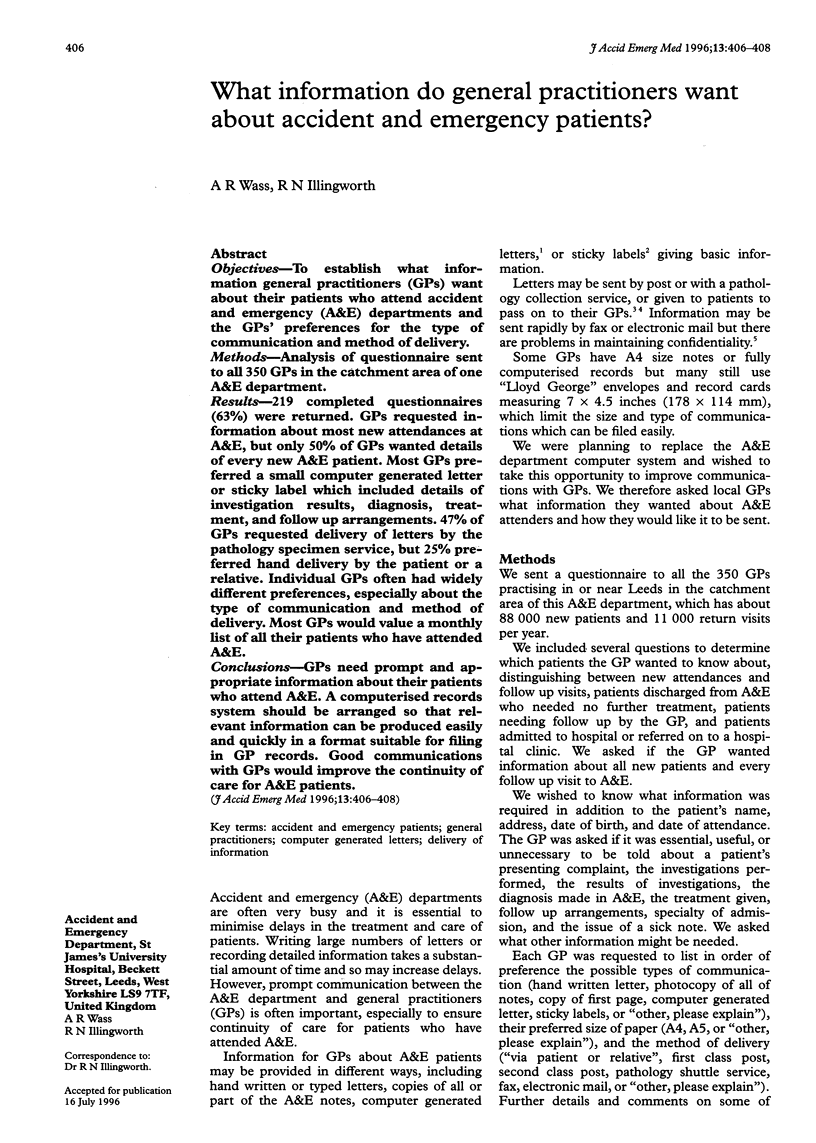

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson R. Clinical system security: interim guidelines. BMJ. 1996 Jan 13;312(7023):109–111. doi: 10.1136/bmj.312.7023.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dover S. B., Low-Beer T. S. The initial hospital discharge note: send out with the patient or post? Health Trends. 1984 May;16(2):48–48. [PubMed] [Google Scholar]
- Lloyd B. W., Barnett P. Use of problem lists in letters between hospital doctors and general practitioners. BMJ. 1993 Jan 23;306(6872):247–247. doi: 10.1136/bmj.306.6872.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mageean R. J. Study of "discharge communications" from hospital. Br Med J (Clin Res Ed) 1986 Nov 15;293(6557):1283–1284. doi: 10.1136/bmj.293.6557.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler D. A., Mitchell J. R. Interim discharge summaries: how are they best delivered to general practitioners? Br Med J (Clin Res Ed) 1987 Dec 12;295(6612):1523–1525. doi: 10.1136/bmj.295.6612.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherry M., Edmunds S., Touquet R. The reliability of patients in delivering their letter from the hospital accident and emergency department to their general practitioner. Arch Emerg Med. 1985 Sep;2(3):161–164. doi: 10.1136/emj.2.3.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams M. J., Haley P., Gosnold J. K. An improved method of communication between computerized accident and emergency departments and general practitioners. Arch Emerg Med. 1991 Sep;8(3):192–195. doi: 10.1136/emj.8.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoltie N., De Dombal F. T. Communication between GPs and consultants. BMJ. 1992 May 2;304(6835):1181–1182. doi: 10.1136/bmj.304.6835.1181-c. [DOI] [PMC free article] [PubMed] [Google Scholar]


