Abstract
Background
Waits for elective total hip arthroplasty for osteoarthritis are common in publicly funded health care systems, but they may lead to poorer postoperative outcomes and loss of health-related quality of life (HRQOL) through progressive pain and immobility during the wait. These issues have not been examined from the time of referral for surgery. Our primary objective was to test whether a longer wait was associated with poorer postoperative HRQOL.
Methods
Patients needing possible total hip arthroplasty for osteoarthritis were identified upon referral to a surgeon in London, Ont. Outcome measures, including the Western Ontario McMaster (WOMAC) Osteoarthritis Index and mobility in the 6-Minute Walk, were assessed at baseline and every 3–6 months thereafter until at least 3 months after the surgery.
Results
Of 553 potentially eligible patients referred for surgical assessment, 123 were placed on a waiting list for total hip arthroplasty; 114 underwent the procedure, and 99 of them returned for postoperative assessment. No significant differences in HRQOL or mobility were seen postoperatively between patients with short waits and those with long waits (a priori definitions ≤ 6 months and > 6 months respectively). At referral, however, patients with short waits had poorer HRQOL and were less mobile than those with long waits (p = 0.002 for WOMAC Osteoarthritis Index total score, 0.001 for pain, 0.009 for stiffness and 0.008 for function; p = 0.006 for 6-Minute Walk results). Patients with short waits experienced larger gains in these measures from the time of referral until the postoperative assessment than did patients with long waits (p = 0.002 for WOMAC Osteoarthritis Index total score, < 0.001 for pain, 0.005 for stiffness and 0.005 for function; p = 0.06 for 6-Minute Walk results). For patients with long waits, increases in the WOMAC Osteoarthritis Index total score exceeded 10% and losses in walking distance exceeded 30 m from the time of referral to surgery.
Interpretation
The length of wait for elective total hip arthroplasty is not associated with postoperative HRQOL and mobility. However, patients who undergo the procedure within 6 months after referral have greater disability at referral, and realize greater gains in HRQOL and mobility after surgery, than patients waiting more than 6 months. Clinically important losses in HRQOL and mobility occur in patients waiting more than 6 months.
Total hip arthroplasty for osteoarthritis improves health-related quality of life (HRQOL) and mobility.1,2,3 However, patients needing elective total hip arthroplasty in publicly funded health care systems often wait because resources do not match demand.4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20 Delays may cause losses in HRQOL from progressive pain and immobility and may lead to poorer outcomes because of more advanced hip disease when surgery is finally done. Also, it has been suggested that publicly funded systems lacking integrated systems to manage waiting lists cannot ensure that waits are matched to disability.21
Previous waiting-list studies4,10,11,12,13,14,15,16,17,18,19,20 have been conducted, but they did not start data collection from the time of patient referral, simultaneously measure HRQOL and mobility or prospectively assess the relation between the entire wait and postoperative outcome. Thus, declines in well-being before the surgeon's assessment, the relation between patient disability at referral and length of wait, and whether longer waits lead to poorer postoperative outcomes have not been fully addressed. We therefore prospectively followed HRQOL and mobility of patients from the time of their referral for total hip arthroplasty. Our primary objective was to test whether longer waits were associated with poorer postoperative HRQOL. As a secondary objective, we determined whether clinically important changes occurred in HRQOL and mobility between the time of referral and surgery.
Methods
Ethics approval for the study was obtained from the University of Western Ontario Human Ethics Committee.
All 7 surgeons performing elective total hip arthroplasty in London, Ont., participated. London provides tertiary care for 1.5 million people in 3 teaching hospitals, each of which has at least 200 acute care beds. Over 80% of elective total hip arthroplasty procedures in Ontario are done in teaching hospitals or in hospitals with 200 acute care beds.1
A study assistant (S.W.B.) reviewed consecutive referrals to the surgeons' offices for “hip disease” from 1994 to 1997. Potential subjects were mailed a letter describing the study. This was followed by a telephone call, during which a screening eligibility checklist was completed. Inclusion criteria were a suspected diagnosis by the referring physicians of osteoarthritis of one or both hips, age of 20 years or more and an ability to understand English. Exclusion criteria included a history of inflammatory arthritis, congenital hip dislocation, avascular necrosis of the femoral head, a condition likely to cause death within 2 years, simultaneous referral to more than 1 surgeon or a previous total hip arthroplasty. Patients in institutions (e.g., residents of mental health or rehabilitation facilities) were not excluded. Up to 3 telephone calls were made before subjects were classified as nonrespondents. All subjects provided signed informed consent. Consenting subjects meeting entry criteria at the screening call attended the outpatient department for baseline studies, which included the 6-Minute Walk22 and assessment of HRQOL by validated indices. Global HRQOL was measured by means of the Medical Outcomes Study Short-Form 36 (SF-36)23 and the Health Utilities Index Mark 3 (HUI 3) Multi- Attribute Health Status Classification System.24,25 Disease- specific measures were the Western Ontario McMaster (WOMAC) Osteoarthritis Index26 and the Harris Hip Scale.27 Intrinsic anxiety (trait anxiety) and anxiety levels at a single time (state anxiety) were assessed by means of the State-Trait Anxiety Inventory28 The SF-36 and the State-Trait Anxiety Inventory were self-administered questionnaires. All other indices and the 6-Minute Walk were supervised (S.W.B.).
Three months from baseline and every 6 months thereafter patients were mailed a package containing the SF-36 and the State Anxiety Scale for completion and return. At 6 months from baseline and every 6 months thereafter patients returned to the outpatient department to repeat the studies done at baseline. At the patient's first visit with the surgeon the diagnosis of osteoarthritis was confirmed. The surgeon's decision regarding the need for total hip arthroplasty and, if indicated, the next available date for surgery were recorded. Follow-up stopped if it was judged that total hip arthroplasty was not indicated. Patients for whom the procedure was recommended were placed on the waiting list, and follow-up continued as described earlier. These patients were also offered placement on a cancellation list. All patients who underwent total hip arthroplasty in London were asked to return to the outpatient department at least 3 months after surgery for a final assessment. Patients and referring physicians were told that involvement in the study would not affect waiting times, and surgeons were not given patients' study results.
For the primary analysis we included patients placed on the waiting list when they first saw the surgeon (“waiting list cohort”) and followed until after surgery. We planned in advance to relate postoperative HRQOL to the length of wait and set the cutoff point for short and long waits according to the mean time the waiting list cohort waited from referral to surgery (“total wait”). The sample size estimate was based in part on the WOMAC Osteoarthritis Index total score. We determined that 100 patients undergoing total hip arthroplasty would provide 80% power (2-tailed αerror probability 5%) to detect a difference in the WOMAC Osteoarthritis Index total score of at least 10% between the short- and long-wait groups after surgery, which is a difference judged to be clinically important.29 Waiting times were log-transformed to improve normality, p values were not adjusted for multiple comparisons, and missing items within otherwise completed questionnaires were replaced according to procedures in relevant scoring manuals. For the secondary analysis we explored further relations between waiting time and postoperative outcome by splitting the cohort into 4 groups according to the total wait. Cutoff points were decided in advance to define the groups (group 1: ≤3 months; group 2: 3–6 months; group 3: 6–12 months; group 4: > 12 months), and changes over time in HRQOL and 6-Minute Walk results were compared across groups by means of analysis of variance.
Results
Of 553 patients referred because of hip disease, 215 completed the baseline assessment (Fig. 1). Of the 338 patients who were excluded, 190 did not meet the eligibility criteria (diagnosis other than osteoarthritis, previous total hip arthroplasty or simultaneous referral to 2 surgeons), 34 could not be contacted, and 114 were eligible but declined entry (unwilling to travel to London, “too busy” or reason not specified). Of the 215 eligible patients, 123 saw a surgeon and were placed on the waiting list; the other patients were not placed on the waiting list because the surgeon deemed that total hip arthroplasty was not indicated (n = 62), the diagnosis was other than osteoarthritis (n = 20), the patient did not attend the appointment with the surgeon (n = 6), or total hip arthroplasty was recommended but the patient declined (n = 4).
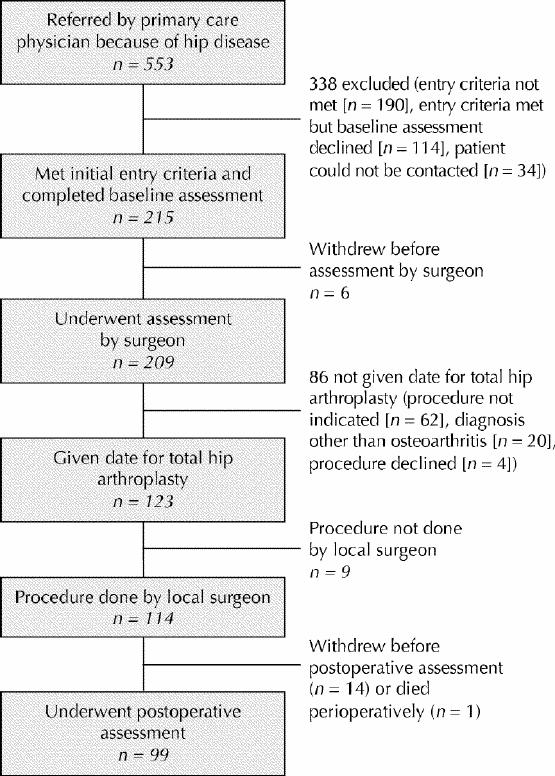
Fig. 1: Cohort ascertainment and follow-up of patients with osteoarthritis of the hip referred for possible total hip arthroplasty in London, Ont.
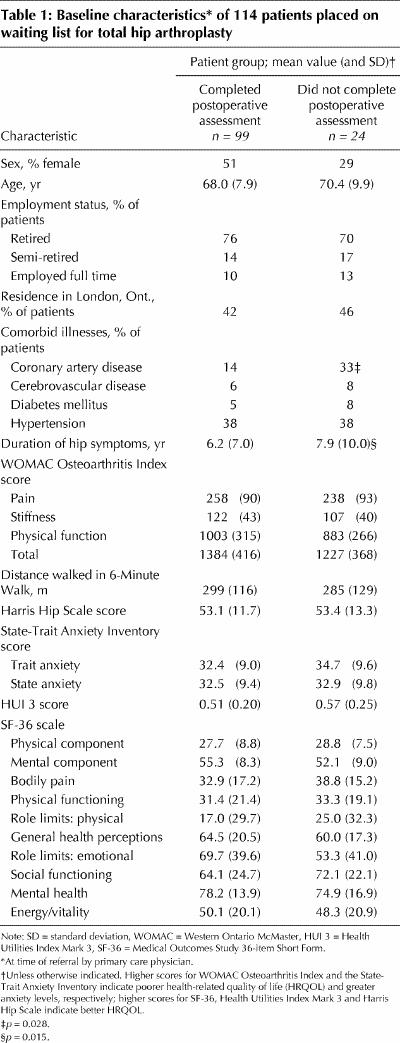
Of the 123 patients placed on the waiting list, 24 were subsequently withdrawn because the procedure was done outside London (n = 7), the surgery was cancelled because of coronary artery disease (n = 2), the procedure was done but the patient did not return for the postoperative assessment (n = 14) or the patient died perioperatively (n = 1). The remaining 99 patients underwent total hip arthroplasty in London, returned for the postoperative assessment (mean time from surgery to postoperative assessment 4.0 [standard deviation (SD) 1.7] months) and were included in the primary analysis. Table 1 shows the baseline characteristics of the waiting list cohort according to whether they provided postoperative data. Overall, the cohort was moderately to severely disabled based on published data for the WOMAC Osteoarthritis Index,26 the 6-Minute Walk30 and the SF-36.31
Table 1
Length of wait and postoperative outcomes
For the 123 patients on the waiting list the mean time from referral to the first appointment with the surgeon was 3.2 (SD 2.6) months (range 0.25–11.2 months). We saw no significant differences in this time between the 114 patients who underwent total hip arthroplasty in London and the 9 who did not (3.0 [SD 2.4] and 3.9 [SD 2.6] months respectively, p = 0.44). The mean total waiting time was 6.5 (SD 5.0) months (range 0.5–24.0 months) for the 114 patients who underwent the procedure in London; it did not differ significantly from the mean total waiting time for the 99 patients who returned for the postoperative assessment (6.0 [SD 4.8] months, range 0.5–24.0, p = 0.51). The waiting times were right skewed such that 25%, 50% and 75% of the patients underwent surgery within 3.2, 4.7 and 8.2 months after referral, respectively. The final 25% waited between 9 and 24 months.
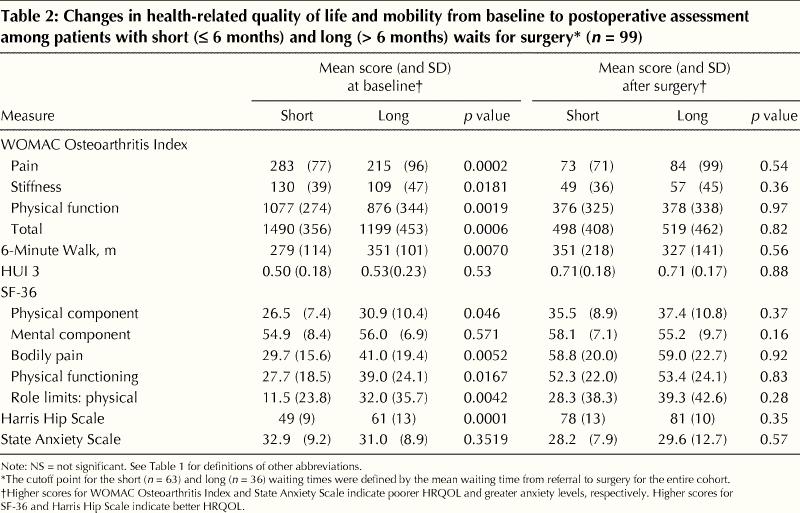
Table 2 shows the baseline and postoperative outcomes for patients with short waits (≤ 6 months) and those with long waits (> 6 months). Postoperatively, we observed no significant differences in HRQOL or 6-Minute Walk results between the 2 groups. At referral, however, patients with short waits had poorer HRQOL and were less mobile than those with long waits (p values for WOMAC Osteoarthritis Index components = 0.002 for total score, 0.001 for pain, 0.009 for stiffness and 0.008 for function; p = 0.006 for 6-Minute Walk results). Comparisons of changes from baseline until after surgery showed that, relative to patients with long waits, those with short waits experienced larger gains in HRQOL (p values for WOMAC Osteoarthritis Index components = 0.002 for total score, < 0.001 for pain, 0.005 for stiffness and 0.005 for function), and they had greater reductions in anxiety levels (p = 0.03). From baseline to after surgery the patients with a short wait experienced a mean increase in the 6-Minute Walk of 72 m, as compared with a mean decline of 24 m among those with a long wait (p = 0.06).
Table 2
Quality of life and mobility before and after surgery
Fig. 2 shows the HRQOL scores and 6-Minute Walk results for prespecified subgroups according to the total wait. For patients who waited at least 3 months (groups 2–4) their mobility and disease-specific HRQOL remained impaired or worsened relative to baseline levels. In general, anxiety levels were higher during the wait than at baseline levels across all subgroups (data not shown). Postoperatively, we saw improvements to levels better than those at baseline in all measures and in all subgroups except the 6-Minute Walk in group 4. For the WOMAC Osteoarthritis Index total score, the mean change relative to baseline from referral to surgery exceeded 10% in groups 2, 3 and 4. For the 6-Minute Walk, this change exceeded 30 m in groups 2 and 4.
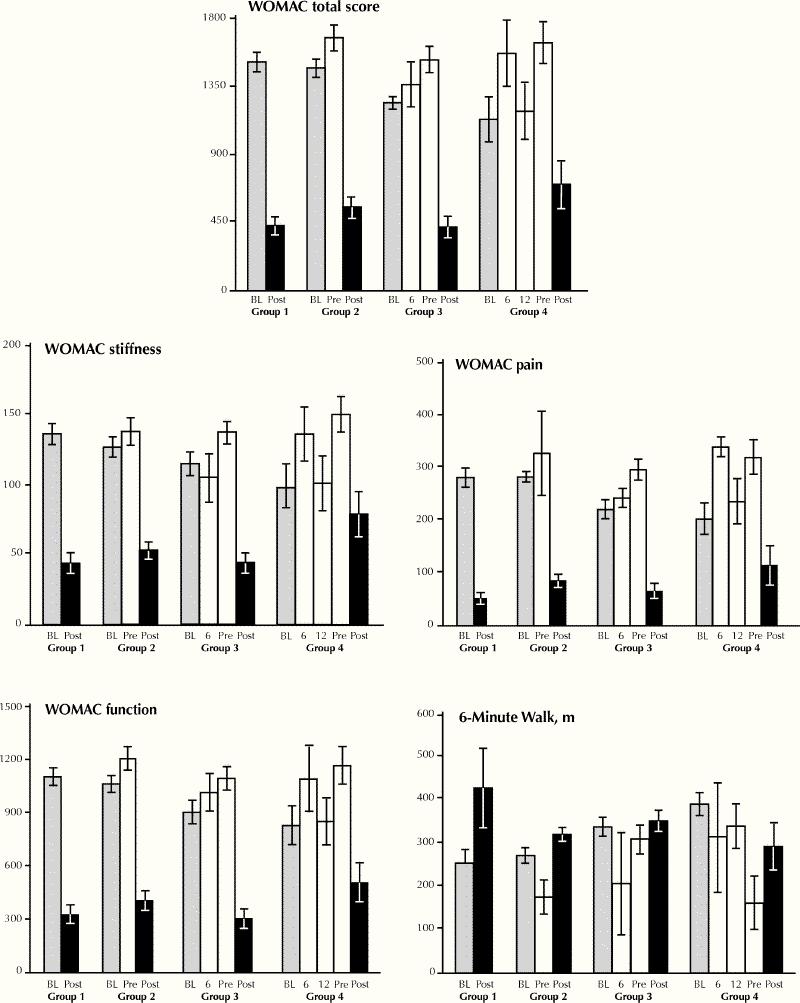
Fig. 2: Health-related quality of life (HRQOL) and mobility in subgroups of patients defined by time from referral to surgery. Group 1 (n = 24) waited less than 3 months to surgery, group 2 (n = 39) 3–6 months, group 3 (n = 23) 6–12 months, and group 4 (n = 13) over 12 months. Higher values for all WOMAC (Western Ontario McMaster) Osteoarthritis Index scales indicate poorer HRQOL. Means and standard errors are shown. Bar labels: BL = baseline value, 6 = 6-month value, 12 = 12-month value, Pre = value just before surgery, Post = value after surgery.
We observed significant associations between waiting time by subgroup and changes from baseline to after surgery in HRQOL (p < 0.001 for all WOMAC Osteoarthritis Index components) and mobility (p = 0.04 for the 6-Minute Walk results). We also noted significant associations between waiting time by subgroup and changes over time in the SF-36 bodily pain and physical function subscales (p = 0.002 and 0.04 respectively, data not shown) and the state anxiety level (p = 0.015, data not shown). In each case patients waiting less time experienced larger gains in HRQOL and distance walked and greater reductions in anxiety after surgery.
Interpretation
In this observational study involving patients awaiting elective total hip arthroplasty for osteoarthitis in a publicly funded health care system, we prospectively followed patients from the time of referral rather than from the first visit with the surgeon. We found that (a) there was no association between the time patients waited for surgery and postoperative HRQOL and mobility; (b) the more disabled patients had surgery sooner and experienced larger gains in HRQOL and mobility than did patients who waited longer; and (c) patients who waited more than 6 months experienced clinically important losses in HRQOL and mobility during the wait. The study's other strengths were the simultaneous use of validated measures of HRQOL and mobility that respond to osteoarthritis and total hip arthroplasty, and the masking of surgeons regarding results of these measures.
We did not confirm our hypothesis that a longer wait is associated with poorer postoperative results. We doubt that this negative result could be explained by inadequate power as it concerns the WOMAC Osteoarthritis Index, because the sample size was sufficient to detect a clinically important difference of 10% between the short- and long-wait groups, should it have existed. We did find that patients with a short wait had significantly larger gains in HRQOL and mobility from referral to after surgery than did patients with a long wait. However, because we used an observational design and did not randomly assign patients to waiting times irrespective of their disability at referral, we cannot be sure that the gains in HRQOL and mobility seen in the short-wait group can be explained solely by the fact that surgery was done sooner. Thus, these observational data support but cannot prove a causal relation between shorter waits for elective total hip arthroplasty and greater improvement in HRQOL and mobility after surgery relative to longer waits.
In the absence of randomized trials, Fig. 2 provides some indication of the disability attending the wait for total hip arthroplasty. One-third of the patients waited at least 6 months (groups 3 and 4), during which they experienced progressive increases in pain and reduced mobility. Surgery reversed those effects in amounts that exceeded the accepted clinically important changes of 10% in the WOMAC Osteoarthritis Index29 and 30 m in the 6-Minute Walk.30 These findings, and the fact that osteoarthritis of the hip is common, imply a large burden from prolonged waits for surgery and support a case for limiting waits to less than 6 months. The wait's impact is borne by individual patients and society through the effects of pain, reduced function, lost productivity and the need for medical therapies (e.g., analgesics) and community resources for patients with severe osteoarthritis of the hip.
A limitation of our study was that the mean length of follow-up after surgery was 4 months. Thus, we cannot rule out longer term changes in HRQOL between patients with short and long waits for surgery. However, at least 1 prospective study has shown that most improvement in HRQOL occurs within 3 months after surgery,13 and we are extending our follow-up to determine whether long-term differences arise. Another limitation relates to our study's generalizability. We achieved 80% (99/123) follow-up within the waiting list cohort, but we did not track patients who could not be contacted or who met initial entry criteria but who declined to participate. We do not know whether these patients differed from those in the waiting list cohort, especially in ways that affected the wait for or response to surgery. Similarly, although our study was done in hospitals that are generally like those performing the majority of elective total hip arthroplasty procedures in Ontario,1 we do not know if our results apply to non-tertiary care settings.
Our finding that more disabled patients had surgery sooner contradicts the view that publicly funded health care systems cannot allocate services relative to need in the absence of integrated management systems.21 Although the p values were not adjusted for multiple comparisons, they were generally low and the associations were consistent across HRQOL measures. Bias on behalf of the surgeons was also unlikely to explain this result, because the date for surgery was set without knowledge of the patients' specific HRQOL scores and 6-Minute Walk results. That other studies did not observe a relation between baseline HRQOL or mobility and the time until surgery may have been because they enrolled patients only after placement on the surgeons' waiting lists.4,10,11,12,13,14,15,16,17,18,19,20 Thus, they did not consider the level of disability when the referring physician judged that total hip arthroplasty might be indicated or the changes in HRQOL between referral and placement on the waiting list.
In summary, we identified both positive and negative aspects about the wait imposed by a publicly funded health care system on patients needing total hip arthroplasty for osteoarthritis. The waiting time appears to reflect patient impairment because more disabled patients had surgery sooner. Longer waits were not associated with differences in HRQOL and mobility after surgery relative to shorter waits, but patients who waited more than 6 months experienced clinically important declines in these measures. As well, a shorter wait was associated with larger gains in HRQOL and mobility compared with a longer wait. We do not know whether this result reflects a causal relation in the absence of trials that randomly assign patients to specific waiting times, but our study provides a rationale for such trials and, pending their completion, reason to limit waits for total hip arthroplasty to 6 months.
Acknowledgments
We gratefully acknowledge the help of the patients who participated in the study, the London orthopedic surgeons (Drs. Harvey Bailey, David Chess, Stuart Grainger, Paul Kim and Robert McAlden) and Dr. Michael Farnsworth. The study was funded by Physicians Services Incorporated (PSI) of Ontario (grant no. 94-30). The PSI played no role in the design, interpretation or analysis of the project and did not review or approve the manuscript.
Footnotes
This article has been peer reviewed.
Contributors: Dr. Mahon was involved in the study conception and design, including grant preparation, and the data analysis and interpretation; he drafted and revised the article. Drs. Bourne, Rorabeck and Feeny were also involved in the study conception and design, grant preparation, data interpretation and critical revision of the article for important intellectual content. Mr. Stitt performed the data analysis, contributed to the data interpretation and revised the article for important intellectual content. Ms. Webster-Bogaert was involved in the data acquisition and interpretation, and critical revision of the article for important intellectual content. All of the authors gave final approval of the version accepted for publication.
Competing interests: None declared for Drs. Mahon, Bourne and Rorabeck, Mr. Stitt and Ms. Webster-Bogaert. Dr. Feeny is employed by Health Utilities Inc., which provides copyrighted health-related quality-of-life questionnaires, including the Health Utilities Index Mark 3 (HUI 3) used in this study.
Correspondence to: Dr. Jeffrey L. Mahon, Rm. 6OF-11, London Health Sciences Centre — University Hospital Campus, 339 Windermere Rd., London ON N6A 5A5; fax 519 663-3211; Jl.Mahon@lhsc.on.ca
References
- 1.Cohen MM, de Boer D, Young W. Total hip replacement. In: Naylor CD, Anderson GM, Goel V, editors. Patterns of health care in Ontario. Ottawa: Canadian Medical Association; 1994. p. 72-6.
- 2.Lavernia CJ, Drakeford MK, Tsao AK, Gittelsohn A, Krackow KA, Hungerford DS. Revision and primary hip and knee arthroplasty — a cost analysis. Clin Orthop 1995;311:136-41. [PubMed]
- 3.Laupacis A, Bourne R, Rorabeck C, Feeny D, Wong C, Tugwell P, et al. Costs of elective total hip arthroplasty. J Arthroplasty 1994;9:481-7. [DOI] [PubMed]
- 4.Williams JI, Llewellyn-Thomas H, Arshinoff R, Young N, Naylor CD. The burden of waiting for hip and knee replacements in Ontario. J Eval Clin Pract 1997;3:59-68. [DOI] [PubMed]
- 5.Hadorn DC, Holmes AC. The New Zealand priority criteria project. Part 1: Overview. BMJ 1997;314:131-4. [DOI] [PMC free article] [PubMed]
- 6.Smith T. Waiting times: monitoring the total postreferral wait. BMJ 1994;309:593-6. [PMC free article] [PubMed]
- 7.Niinimaki T. Increasing demands on orthopedic services. Acta Orthop Scand Suppl 1991;241:42-3. [DOI] [PubMed]
- 8.Beverland DE, McKee WS, Murphy JS, Mollan RA, Barron DW. Development of the Belfast orthopedic information system. Health Serv Manage 1989; 85:270-2. [PubMed]
- 9.Abyholm G, Riise G, Melsom MN, Piene H, Gulbrandsen I. The waiting list guarantee and its violation. Characteristics of patients who have been waiting more than five months. Tidsskr Nor Laegeforen 1997;117:366-8. [PubMed]
- 10.Groothoff JW, Kruijer SW, Post D. What determines waiting time for cataract surgery, knee arthroscopy and total hip arthroplasty and how satisfied are the patients? Ned Tijdschr Geneeskd 1995;139:1489-93. [PubMed]
- 11.Derrett S, Paul C, Morris JM. Waiting for elective surgery: effects on health-related quality of life. Int J Qual Health Care 1999;11:47-57. [DOI] [PubMed]
- 12.March LM, Cross MJ, Lapsley H, Brnabic AJ, Tribe KL, Bachmeier CJ, et al. Outcomes after hip or knee replacement surgery for osteoarthritis. A prospective cohort study comparing patients' quality of life before and after surgery with age-related population norms. Med J Aust 1999;171:235-8. [PubMed]
- 13.Shields RK, Enloe LJ, Leo KC. Health related quality of life in patients with total hip or knee replacement. Arch Phys Med Rehabil 1999;572-9. [DOI] [PubMed]
- 14.Clover KA, Dobbins TA, Smyth TJ, Sanson-Fisher RW. Factors associated with waiting time for surgery. Med J Aust 1998;169:464-8. [DOI] [PubMed]
- 15.Knutsen S, Engberg IB. An evaulation of patients' quality of life before, 6 weeks and 6 months after total hip replacement surgery. J Adv Nurs 1999; 30: 1349-59. [DOI] [PubMed]
- 16.Rissanen P, Aro S, Sintonen H, Slatis P, Paavolainen P. Quality of life and functional ability in hip and knee replacements: a prospective study. Qual Life Res 1996;5:56-64. [DOI] [PubMed]
- 17.Kelly KD, Voaklander D, Kramer G, Johnston DWC, Redfern L, Suarez-Almazor ME. The impact of health status on waiting time for major joint arthroplasty. J Arthroplasty 2000;15:877-83. [DOI] [PubMed]
- 18.Kelly KD, Voaklander DC, Johnston DWC, Newman SC, Suarez-Almazor ME. Change in pain and function while waiting for major joint arthroplasty. J Arthroplasty 2001;16:351-9. [DOI] [PubMed]
- 19.Kelly KD, Voaklander DC, Johnston WC, Suarez-Almazor ME. Equity in waiting times for major joint arthroplasty. Can J Surg 2002;45(4):269-76. [PMC free article] [PubMed]
- 20.Mangione CM, Goldman L, Orav EJ, Marcantonio ER, Pedan A, Ludwig LE, et al. Health-related quality of life after elective surgery: measurement of longitudinal changes. J Gen Intern Med 1997;12:686-97. [DOI] [PMC free article] [PubMed]
- 21.Lewis S, Barer ML, Sanmartin C, Sheps S, Shortt SE, McDonald PW. Ending waiting-list mismanagement: principles and practice. CMAJ 2000;162(9): 1297-300. [PMC free article] [PubMed]
- 22.Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. CMAJ 1985;132(8):919-23. [PMC free article] [PubMed]
- 23.Ware JE, Sherbourne CD. The MOS-36-item short-form health survey (SF-36): conceptual framework and item selection. Med Care 1992;30:473-83. [PubMed]
- 24.Feeny DH, Torrance GW, Furlong WJ. Health Utilities Index. In: Spilker B, editor. Quality of life and pharmacoeconomics in clinical trials. 2nd ed. Philadelphia: Lippincott-Raven Press; 1996. p. 239-52.
- 25.Furlong W, Feeny D, Torrance GW, Goldsmith C, DePauw Z, Zhu Z, et al. Multiplicative multi-attribute utility function for the Health Utilities Index Mark 3 (HUI 3) system: a technical report. Hamilton (ON): McMaster University Centre for Health Economics and Policy; 1998. Working paper no. 98-11.
- 26.Bellamy N, Burhanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833-40. [PubMed]
- 27.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg [Am] 1969;51:737-55. [PubMed]
- 28.Spielberger CD. Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto: Consulting Psychologist's Press; 1983.
- 29.Ehrich E, Davies G, Watson D, Bolognese J, Seidenberg B, Bellamy N. Minimal perceptible clinical improvement (MPCI) in osteoarthritis: WOMAC and global assessments, influence of age, gender, and geographic region. Arthritis Rheum 1999;42(Suppl):S143.
- 30.Guyatt GH, Townsend M, Pugsley SO, Keller JL, Short HD, Taylor DW, et al. Bronchodilators in chronic airflow limitation. Am Rev Respir Dis 1987; 135: 1069-74. [DOI] [PubMed]
- 31.Hopman WM, Towheed T, Anastassiades T, Tenenhouse A, Poliquin S, Berger C, et al. Canadian normative data for the SF-36 health survey. Canadian Multicentre Osteoporosis Study Research Group. CMAJ 2000;163(3):265-71. [PMC free article] [PubMed]


