Abstract
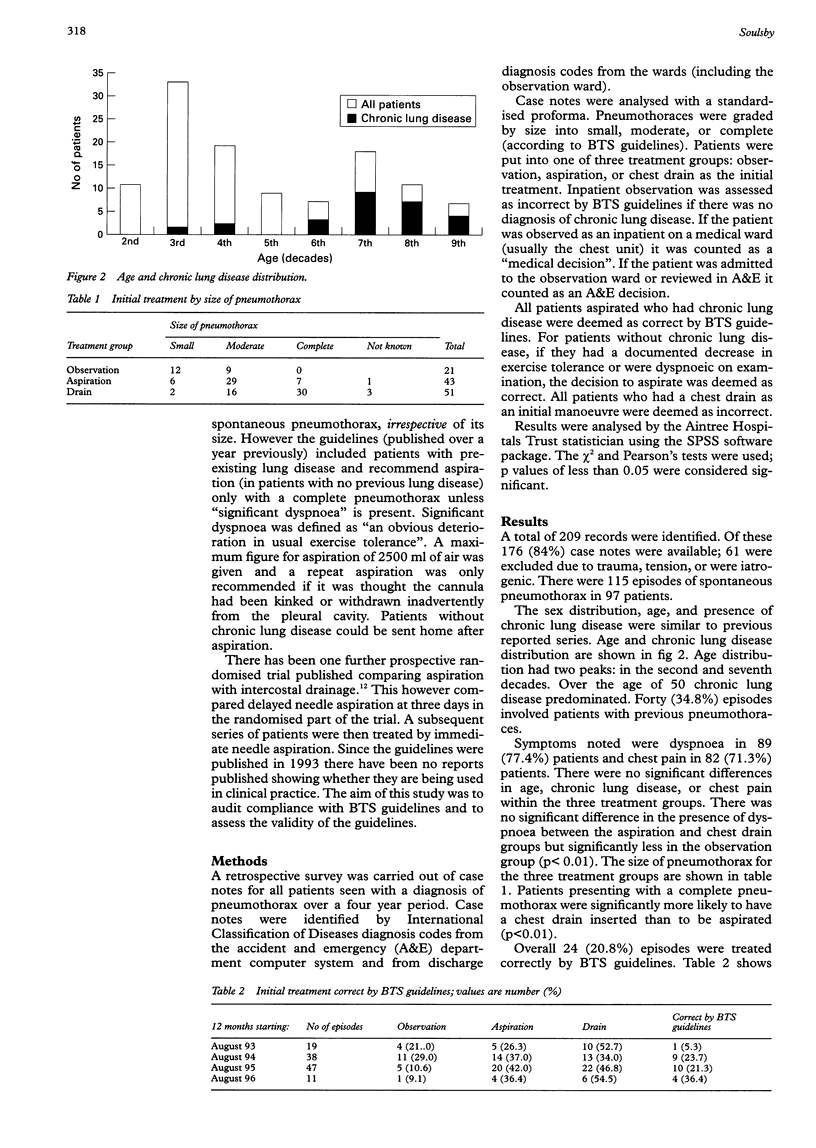
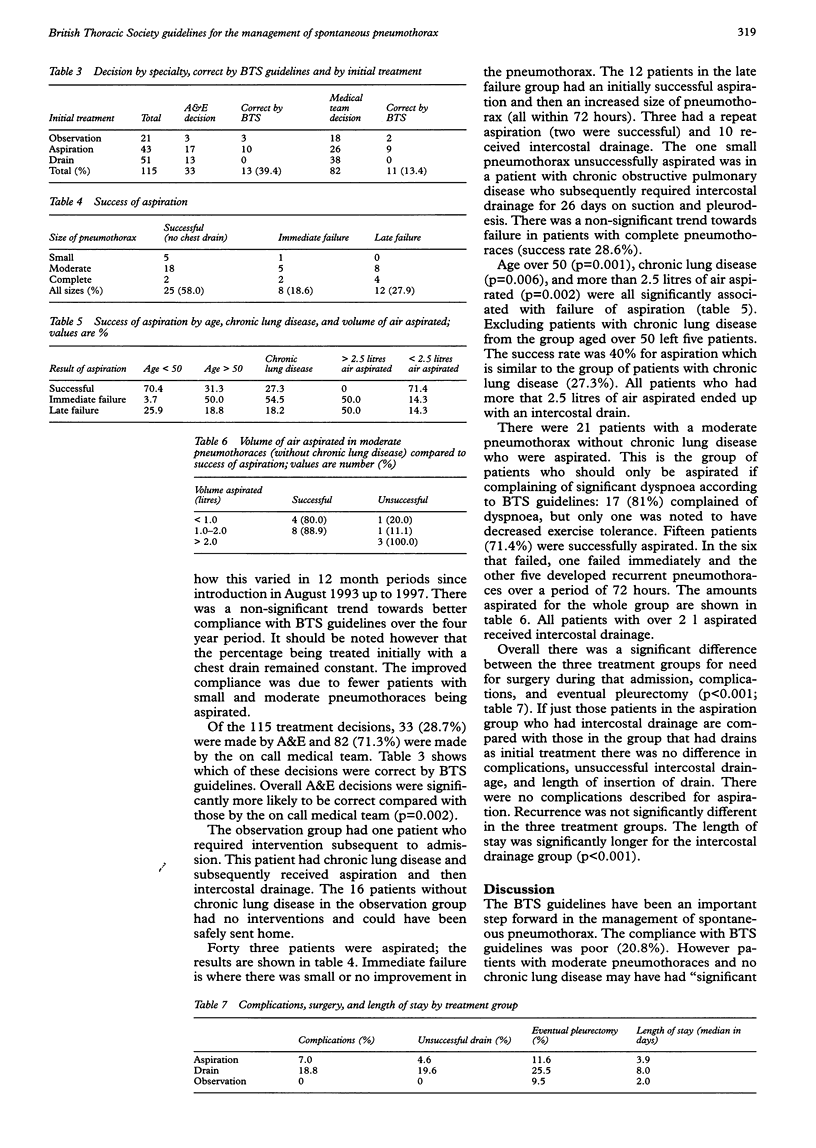
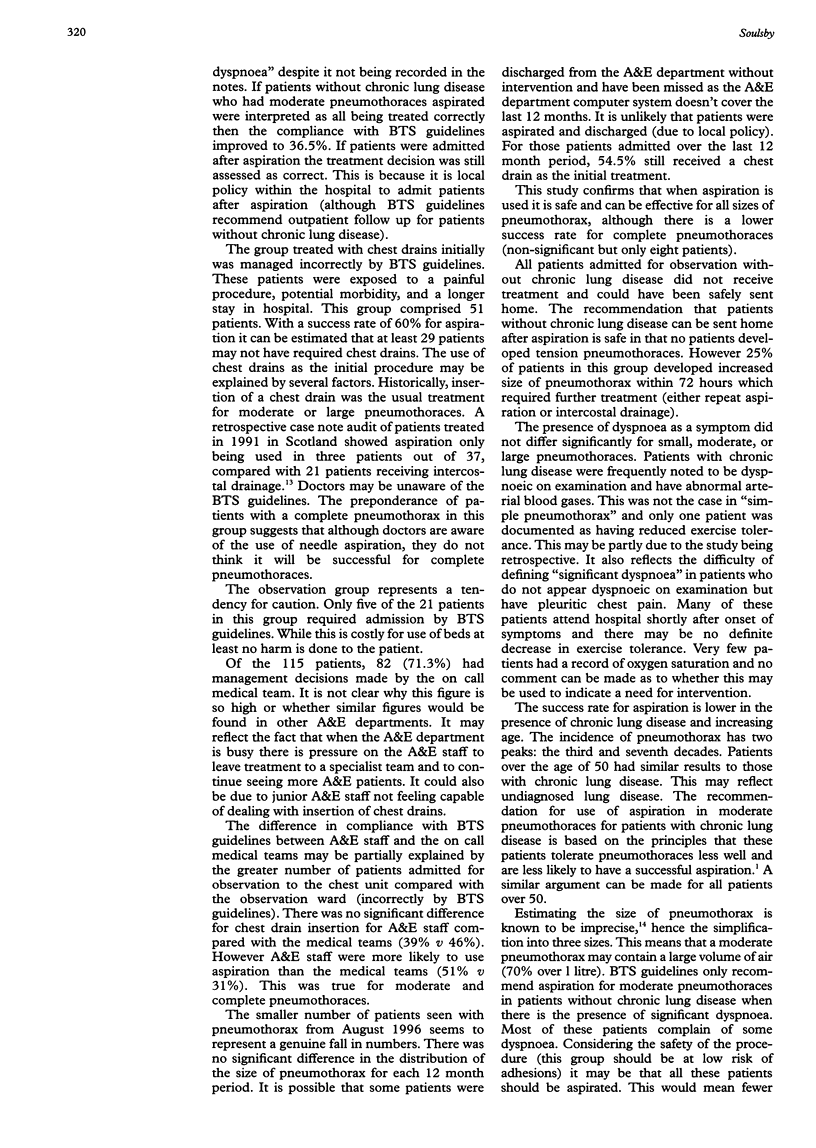
OBJECTIVES: To determine how British Thoracic Society (BTS) guidelines for the management of spontaneous pneumothorax have been implemented over a four year period in a large district general hospital with a specialised respiratory unit. To assess the validity of the guidelines in the management of spontaneous pneumothorax. METHODS: A retrospective case notes study over a four year period for all patients with spontaneous pneumothoraces attending the accident and emergency (A&E) department of a large district general hospital. RESULTS: 115 episodes of spontaneous pneumothorax were identified. Overall 20.8% of episodes were treated correctly by BTS guidelines. Decisions made by A&E staff were significantly more likely to be correct than decisions made by on call medical teams (39.4% v 13.4%, p = 0.002). There was a non-significant trend towards better compliance with BTS guidelines over the four year period. The management decision was made by A&E staff only in 28.7% of episodes. Patients without chronic lung disease could be safely observed as outpatients. Forty three pneumothoraces were aspirated: 23 (58%) successfully; eight (18.6%) with little or no improvement; and 12 (27.9%) initially successfully but developing increased size of pneumothorax within a period of 72 hours. Three patients had repeat aspirations, two successfully. Age over 50, chronic lung disease, and more than 2.5 litres of air aspirated were significantly associated with failure of aspiration (p < 0.01). There was a 28.6% failure rate of aspiration for patients with moderate pneumothoraces without chronic lung disease. CONCLUSIONS: Patients over the age of 50 should be treated the same as patients with chronic lung disease. A second aspiration should be attempted if the first aspiration is initially successful with subsequent recurrence of pneumothorax. Further research is required to clarify if patients with moderate pneumothoraces under the age of 50 and no chronic lung disease should be aspirated or observed.
Full text
PDF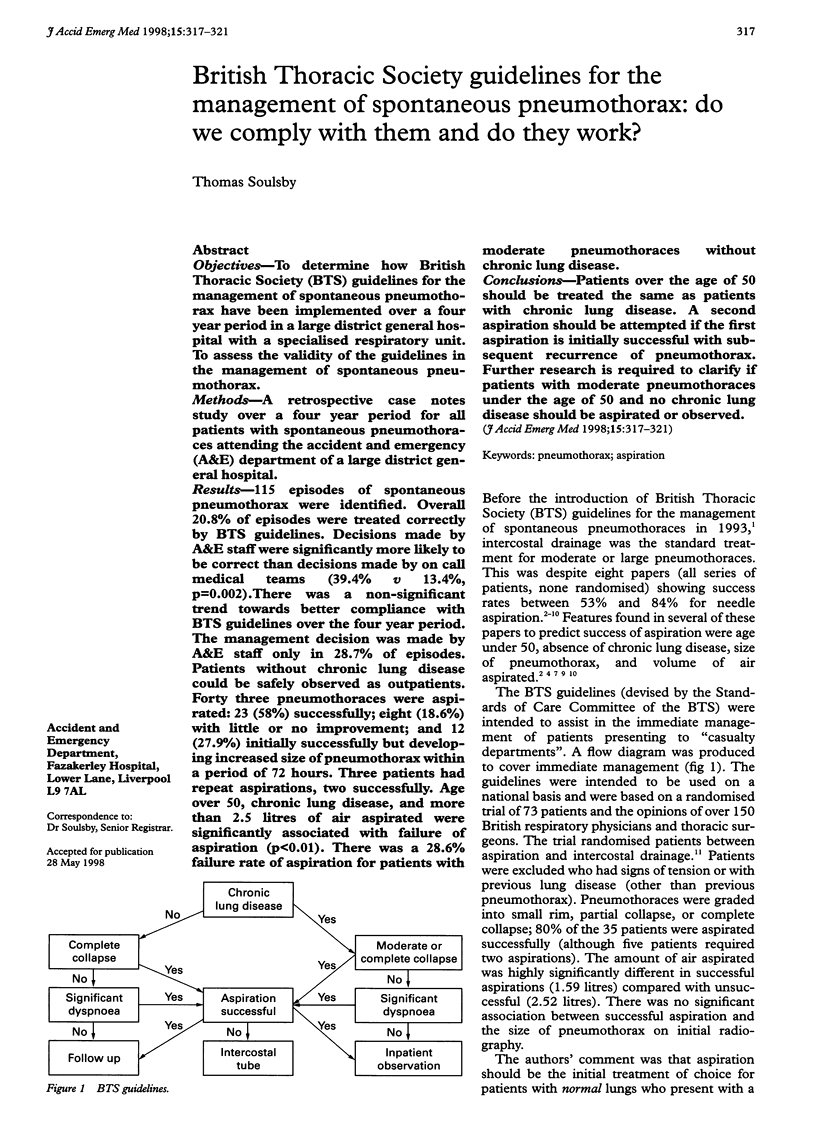

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andrivet P., Djedaini K., Teboul J. L., Brochard L., Dreyfuss D. Spontaneous pneumothorax. Comparison of thoracic drainage vs immediate or delayed needle aspiration. Chest. 1995 Aug;108(2):335–339. doi: 10.1378/chest.108.2.335. [DOI] [PubMed] [Google Scholar]
- Archer G. J., Hamilton A. A., Upadhyay R., Finlay M., Grace P. M. Results of simple aspiration of pneumothoraces. Br J Dis Chest. 1985 Apr;79(2):177–182. [PubMed] [Google Scholar]
- Delius R. E., Obeid F. N., Horst H. M., Sorensen V. J., Fath J. J., Bivins B. A. Catheter aspiration for simple pneumothorax. Experience with 114 patients. Arch Surg. 1989 Jul;124(7):833–836. doi: 10.1001/archsurg.1989.01410070091018. [DOI] [PubMed] [Google Scholar]
- Engdahl O., Toft T., Boe J. Chest radiograph--a poor method for determining the size of a pneumothorax. Chest. 1993 Jan;103(1):26–29. doi: 10.1378/chest.103.1.26. [DOI] [PubMed] [Google Scholar]
- Harvey J., Prescott R. J. Simple aspiration versus intercostal tube drainage for spontaneous pneumothorax in patients with normal lungs. British Thoracic Society Research Committee. BMJ. 1994 Nov 19;309(6965):1338–1339. doi: 10.1136/bmj.309.6965.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones J. S. A place for aspiration in the treatment of spontaneous pneumothorax. Thorax. 1985 Jan;40(1):66–67. doi: 10.1136/thx.40.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markos J., McGonigle P., Phillips M. J. Pneumothorax: treatment by small-lumen catheter aspiration. Aust N Z J Med. 1990 Dec;20(6):775–781. doi: 10.1111/j.1445-5994.1990.tb00422.x. [DOI] [PubMed] [Google Scholar]
- Miller A. C., Harvey J. E. Guidelines for the management of spontaneous pneumothorax. Standards of Care Committee, British Thoracic Society. BMJ. 1993 Jul 10;307(6896):114–116. doi: 10.1136/bmj.307.6896.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng A. W., Chan K. W., Lee S. K. Simple aspiration of pneumothorax. Singapore Med J. 1994 Feb;35(1):50–52. [PubMed] [Google Scholar]
- Selby C. D., Sudlow M. F. Deficiencies of management of spontaneous pneumothoraces. Scott Med J. 1994 Jun;39(3):75–77. doi: 10.1177/003693309403900306. [DOI] [PubMed] [Google Scholar]
- Stradling P., Poole G. Conservative management of spontaneous pneumothorax. Thorax. 1966 Mar;21(2):145–149. doi: 10.1136/thx.21.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallee P., Sullivan M., Richardson H., Bivins B., Tomlanovich M. Sequential treatment of a simple pneumothorax. Ann Emerg Med. 1988 Sep;17(9):936–942. doi: 10.1016/s0196-0644(88)80676-0. [DOI] [PubMed] [Google Scholar]


