Abstract
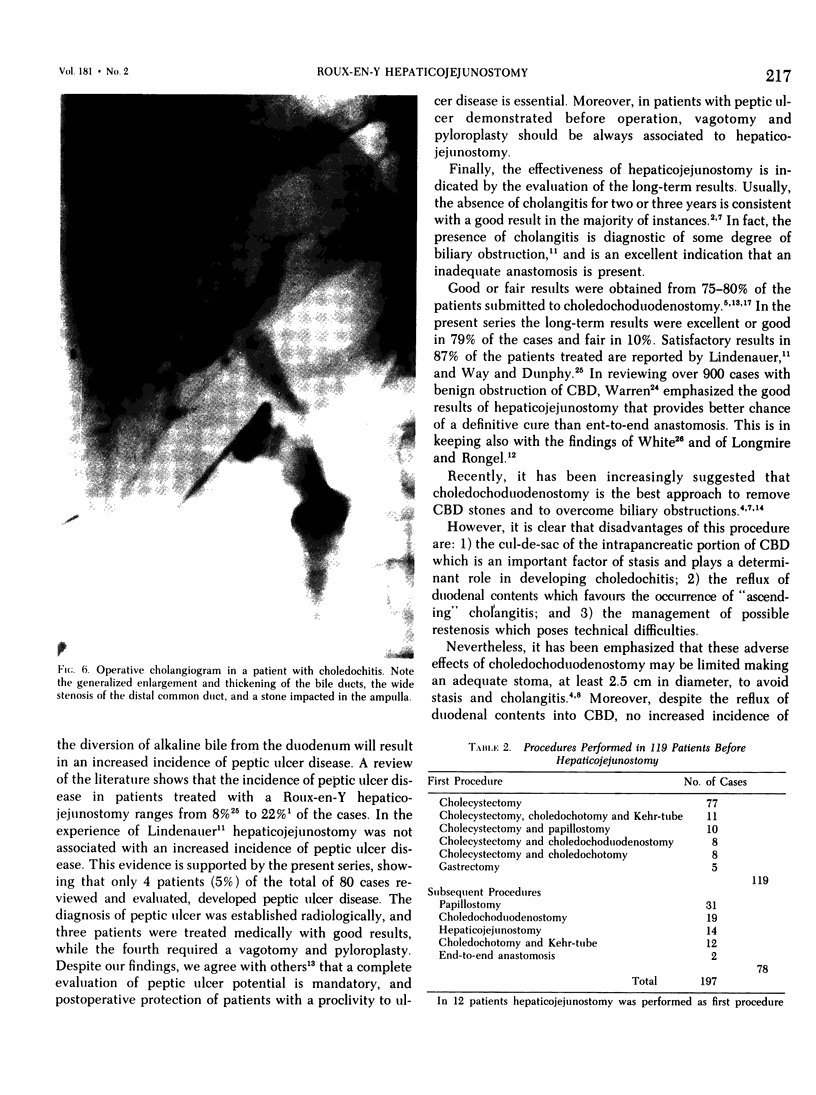
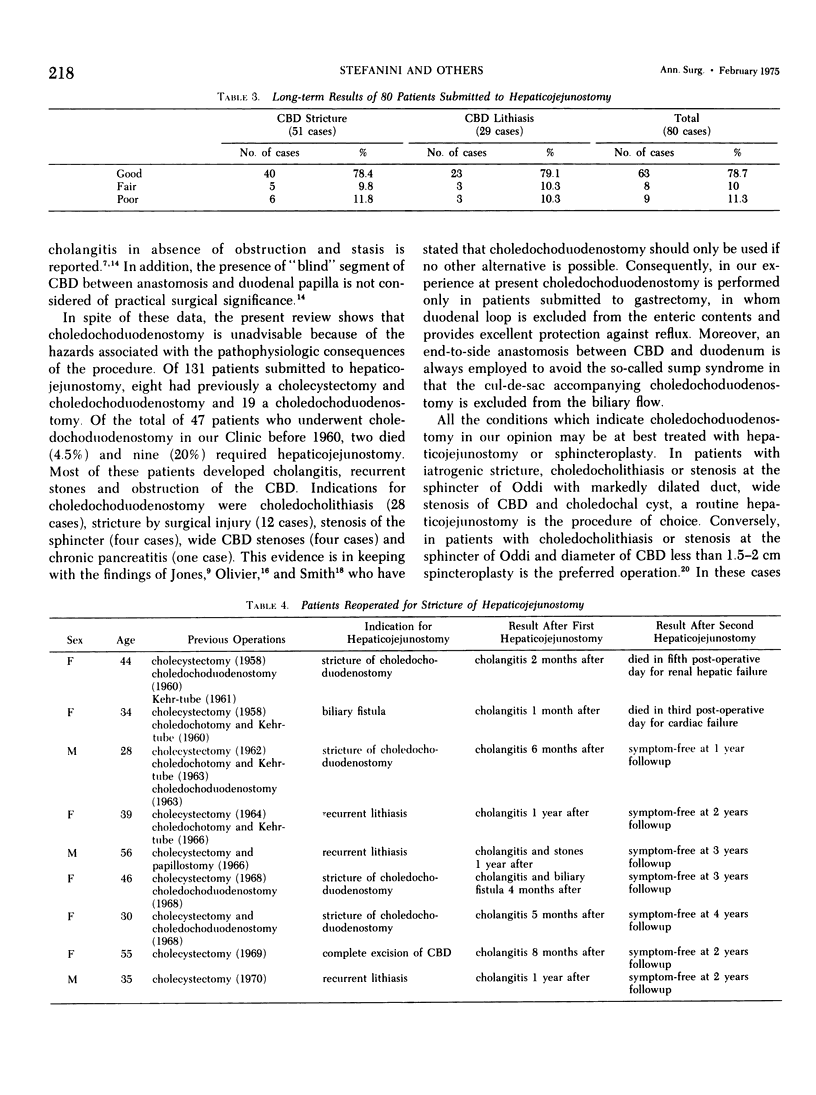
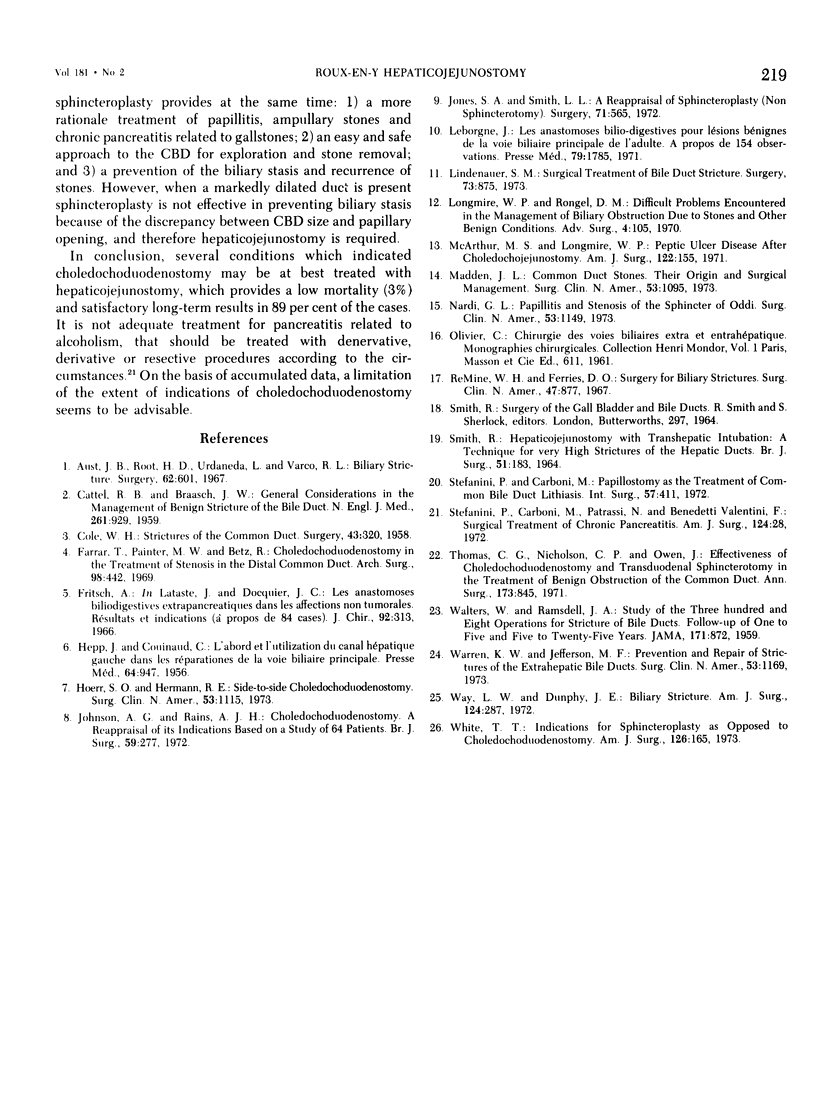
A critical evaluation is made of 131 patients submitted to choledocho or hepaticojejunostomy. The main indications for hepaticojejunostomy were iatrogenic strictures of CBD (60 patients), and choledocholithiasis with markedly dilated duct (41 patients). The overall mortality rate was 4% representing principally renal hepatic failure, bile peritonitis and bleeding. The complications following hepaticojejunostomy included only in one case biliary fistula which required reoperation. The long-term results of 80 patients available for a followup study were as follows: 63 patients (78.7%) were symptom-free at 2-13 years followup; 8 patients had brief episodes of cholangitis which responded to antibiotic and corticosteroid treatment; 9 patients required reoperation for stricture of anastomosis. These overall results are a strong argument for hepaticojejunostomy which, compared with choledochoduodenostomy, avoids the hazards of the so-called sump syndrome and of the reflux of enteric contents in the CBD. An increased incidence of peptic ulcer disease in the patients submitted to hepaticojejunostomy was not observed. In very high strictures and in reinterventions anastomosis between left hepatic duct and Roux-en-Y jejunal limb was carried out. The results achieved with this technique, which was performed in 26 patients, were about the same following hepaticojejunostomy.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aust J. B., Root H. D., Urdaneta L., Varco R. L. Biliary stricture. Surgery. 1967 Oct;62(4):601–608. [PubMed] [Google Scholar]
- COLE W. H. Stricutres of the common duct. Surgery. 1958 Feb;43(2):320–324. [PubMed] [Google Scholar]
- Farrar T., Painter M. W., Betz R. Choledochoduodenostomy. In the treatment of stenosis in the distal common duct. Arch Surg. 1969 Apr;98(4):442–446. doi: 10.1001/archsurg.1969.01340100074008. [DOI] [PubMed] [Google Scholar]
- HEPP J., COUINAUD C. L'abord et l'utilisation du canal hépatique gauche dans les réparations de la voie biliaire principale. Presse Med. 1956 May 23;64(41):947–948. [PubMed] [Google Scholar]
- Hoerr S. O., Hermann R. E. Side-to-side choledochoduodenostomy. Surg Clin North Am. 1973 Oct;53(5):1115–1122. doi: 10.1016/s0039-6109(16)40140-4. [DOI] [PubMed] [Google Scholar]
- Johnson A. G., Rains A. J. Choledochoduodenostomy. A reappraisal of its indications based on a study of 64 patients. Br J Surg. 1972 Apr;59(4):277–280. [PubMed] [Google Scholar]
- Jones S. A., Smith L. L. A reappraisal of sphincteroplasty (not sphincterotomy). Surgery. 1972 Apr;71(4):565–575. [PubMed] [Google Scholar]
- Leborgne J. Les anastomoses bilio-digestives pour lésions bénignes de la voie biliaire principale de l'adulte. A propos de 154 observations. Presse Med. 1971 Oct 2;79(41):1785–1788. [PubMed] [Google Scholar]
- Lindenauer S. M. Surgical treatment of bile duct strictures. Surgery. 1973 Jun;73(6):875–880. [PubMed] [Google Scholar]
- Longmire W. P., Jr, Rangel D. M. Difficult problems encountered in the management of biliary obstruction due to stones and other benign conditions. Adv Surg. 1970;4:105–161. [PubMed] [Google Scholar]
- Madden J. L. Common duct stones. Their origin and surgical management. Surg Clin North Am. 1973 Oct;53(5):1095–1113. doi: 10.1016/s0039-6109(16)40139-8. [DOI] [PubMed] [Google Scholar]
- Nardi G. L. Papillitis and stenosis of the sphincter of Oddi. Surg Clin North Am. 1973 Oct;53(5):1149–1160. doi: 10.1016/s0039-6109(16)40143-x. [DOI] [PubMed] [Google Scholar]
- SMITH R. HEPATICOJEJUNOSTOMY: CHOLEDOCHOJEJUNOSTOMY: A METHOD OF INTRAJEJUNAL ANASTOMOSIS. Br J Surg. 1964 Mar;51:183–186. doi: 10.1002/bjs.1800510306. [DOI] [PubMed] [Google Scholar]
- Stefanini P., Carboni M., Patrassi N., Benedetti-Valentini F J. Surgical treatment of chronic pancreatitis. Am J Surg. 1972 Jul;124(1):28–30. doi: 10.1016/0002-9610(72)90159-6. [DOI] [PubMed] [Google Scholar]
- Stefanini P. Papillostomy as the treatment of common bile duct lithiasis. Int Surg. 1972 May;57(5):411–412. [PubMed] [Google Scholar]
- Thomas C. G., Jr, Nicholson C. P., Owen J. Effectiveness of choledochoduodenostomy and transduodenal sphincterotomy in the treatment of benign obstruction of the common duct. Ann Surg. 1971 Jun;173(6):845–856. doi: 10.1097/00000658-197106010-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren K. W., Jefferson M. F. Prevention and repair of strictures of the extrahepatic bile ducts. Surg Clin North Am. 1973 Oct;53(5):1169–1190. doi: 10.1016/s0039-6109(16)40145-3. [DOI] [PubMed] [Google Scholar]
- Way L. W., Dunphy J. E. Biliary stricture. Am J Surg. 1972 Aug;124(2):287–295. doi: 10.1016/0002-9610(72)90026-8. [DOI] [PubMed] [Google Scholar]
- White T. T. Indications for sphincteroplasty as opposed to choledochoduodenostomy. Am J Surg. 1973 Aug;126(2):165–170. doi: 10.1016/s0002-9610(73)80148-5. [DOI] [PubMed] [Google Scholar]