Abstract
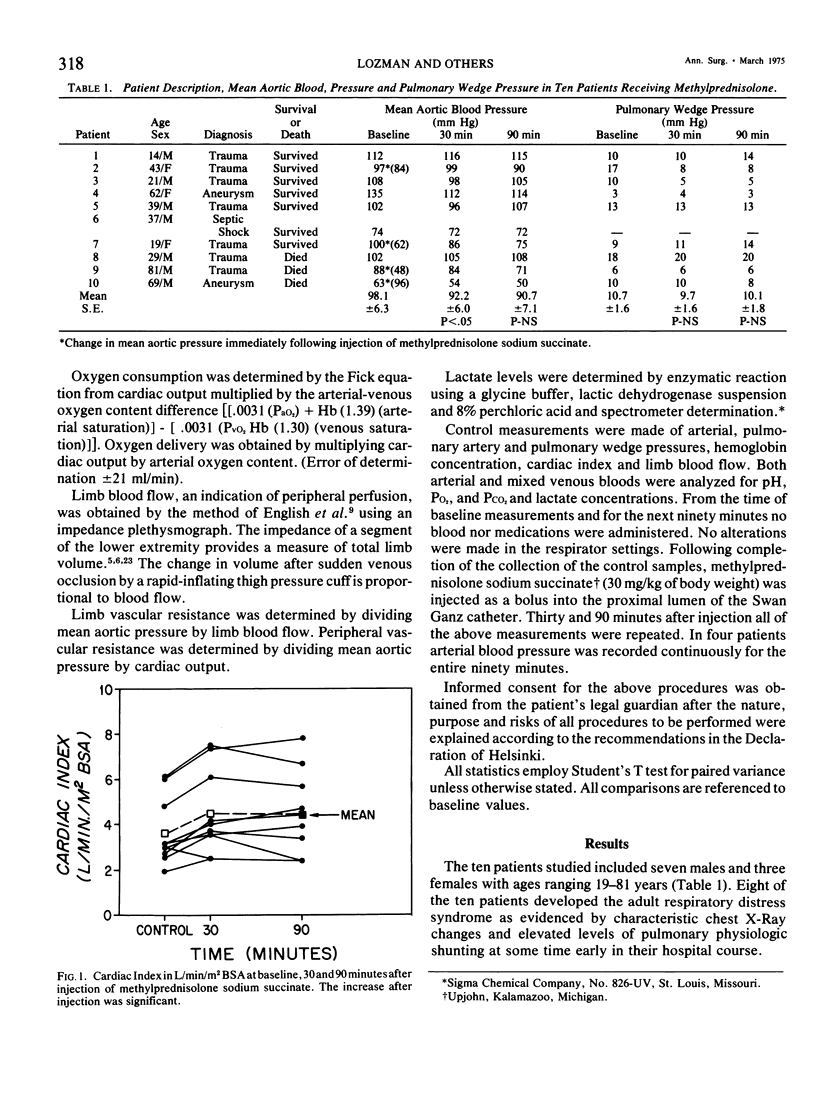
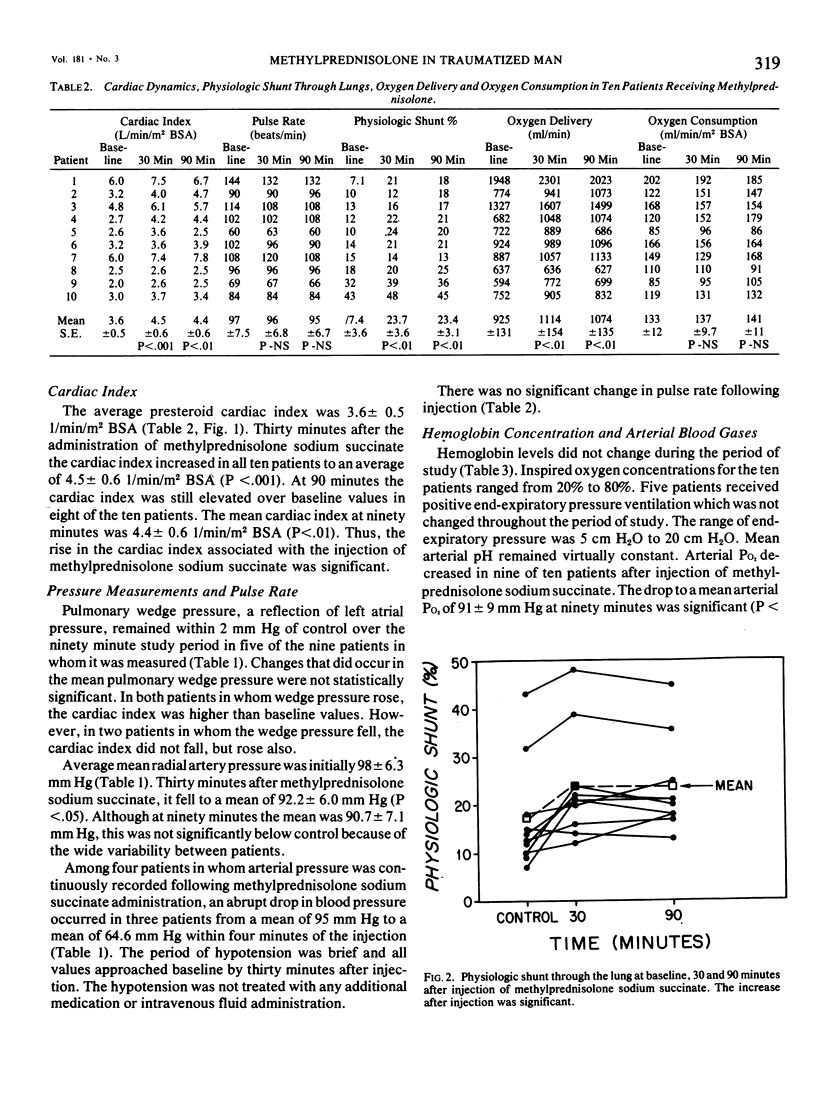
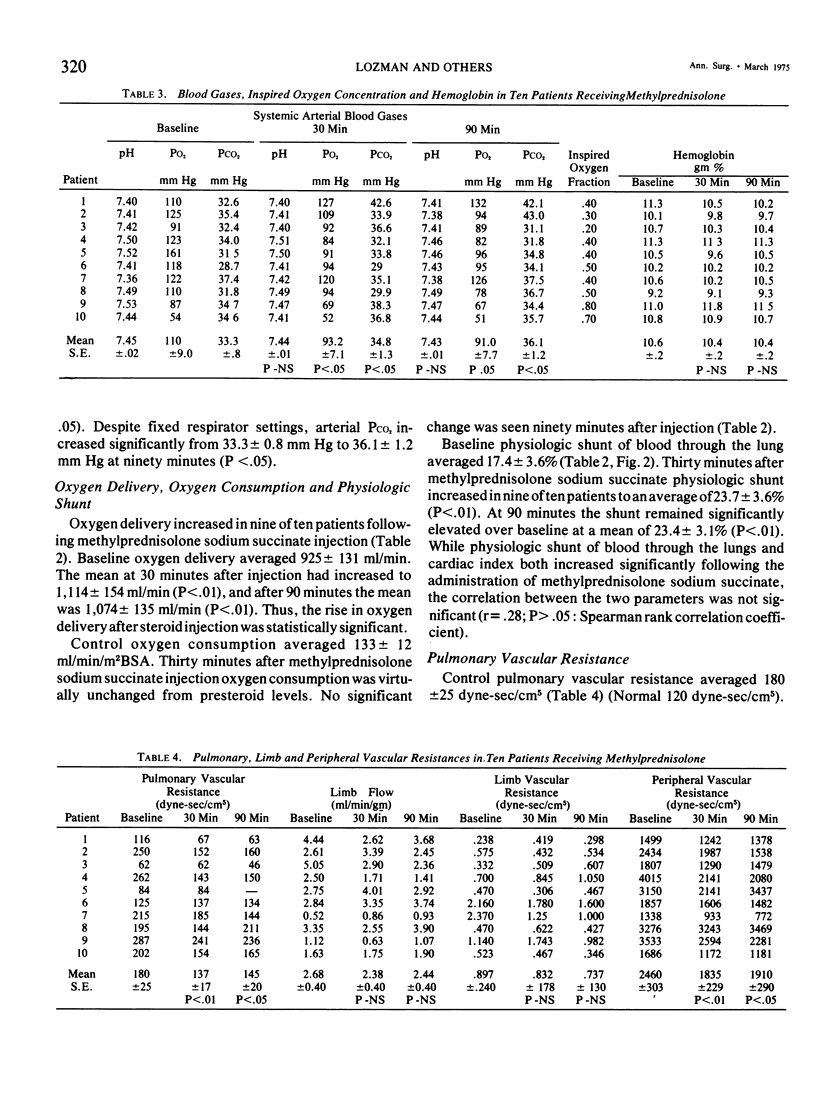
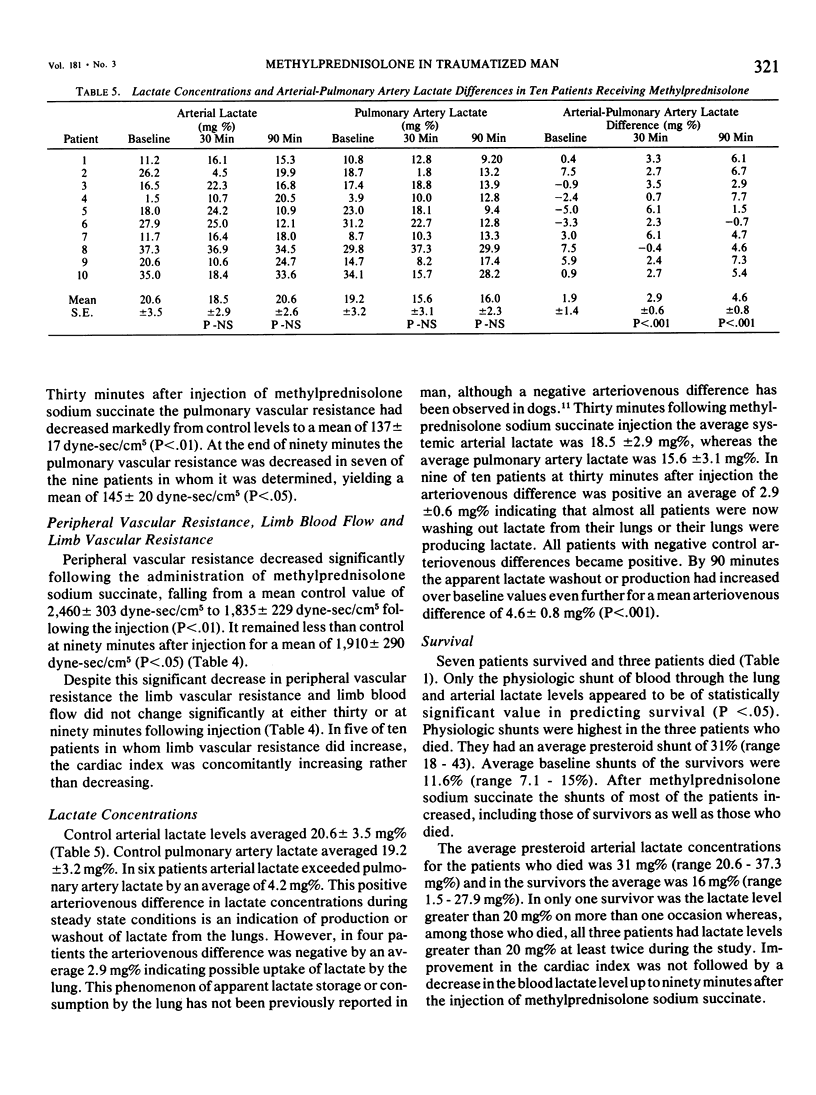
Pharmacologic doses of methylprednisolone sodium succinate were administered to 10 critically ill patients when the steroid was the only variable. Measurements of respiratory and circulatory physiologic parameters were obtained in all patients prior to injection and at 30 and 90 minutes following injection of methylprednisolone sodium succinate. A significant increase in Cardiac Index was seen (P less than .01) which appeared to be in association with a decrease in pulmonary vascular resistance (P less than .01) at a time when physiologic shunting of blood through the lungs increased (P less than .01). These changes imply improved perfusion of non- or poorly ventilated portions of the lungs. Four of ten patients demonstrated removal of lactate by the lung during the control period. Following methylprednisolone sodium succinate injection, 9 of 10 patients demonstrated production or a washout of lactate from the lungs.
Full text
PDF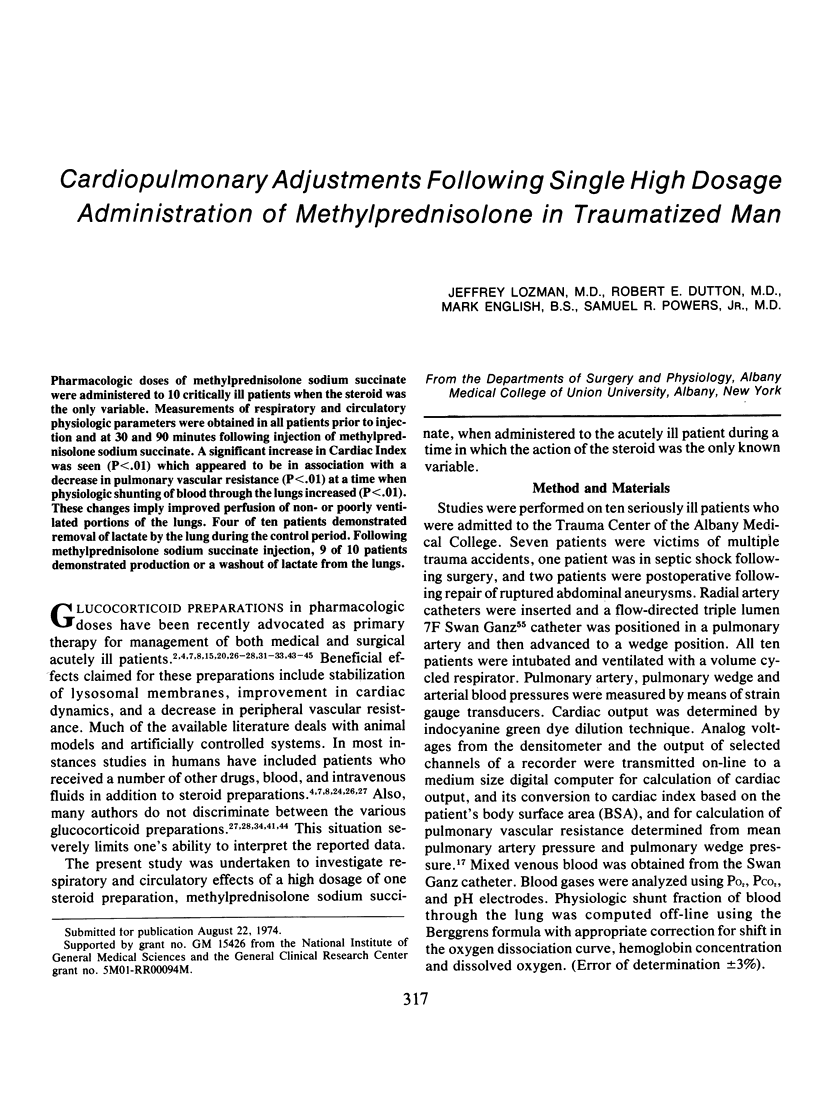
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BRODER G., WEIL M. H. EXCESS LACTATE: AN INDEX OF REVERSIBILITY OF SHOCK IN HUMAN PATIENTS. Science. 1964 Mar 27;143(3613):1457–1459. doi: 10.1126/science.143.3613.1457. [DOI] [PubMed] [Google Scholar]
- Blockwood J. M., Hsieh J., Fewel J., Rush B. F., Jr Tissue metabolites in endotoxin and hemorrhagic shock; a comparison. Arch Surg. 1973 Aug;107(2):181–185. doi: 10.1001/archsurg.1973.01350200055014. [DOI] [PubMed] [Google Scholar]
- Canizaro P. C., Prager M. D., Shires G. T. The infusion of Ringer's lactate solution during shock. Changes in lactate, excess lactate, and pH. Am J Surg. 1971 Oct;122(4):494–501. doi: 10.1016/0002-9610(71)90474-0. [DOI] [PubMed] [Google Scholar]
- Christy J. H. Treatment of gram-negative shock. Am J Med. 1971 Jan;50(1):77–88. doi: 10.1016/0002-9343(71)90207-5. [DOI] [PubMed] [Google Scholar]
- Couch N. P., Van de Water J. M., Dmochowski J. R. Noninvasive measurement of peripheral arterial flow. Impedance cardiograph and ultrasonic Doppler flowmeter. Arch Surg. 1971 May;102(5):435–439. doi: 10.1001/archsurg.1971.01350050001001. [DOI] [PubMed] [Google Scholar]
- Cranley J. J., Gay A. Y., Grass A. M., Simeone F. A. A plethysmographic technique for the diagnosis of deep venous thrombosis of the lower extremities. Surg Gynecol Obstet. 1973 Mar;136(3):385–394. [PubMed] [Google Scholar]
- Dietzman R. H., Casteda A. R., Lillehei C. W., Ersera, Motsay G. J., Lillehei R. C. Corticosteroids as effective vasodilators in the treatment of low output syndrome. Chest. 1970 May;57(5):440–453. doi: 10.1378/chest.57.5.440. [DOI] [PubMed] [Google Scholar]
- Dietzman R. H., Ersek R. A., Lillehei C. W., Castaneda A. R., Lillehei R. C. Low output syndrome. Recognition and treatment. J Thorac Cardiovasc Surg. 1969 Jan;57(1):138–150. [PubMed] [Google Scholar]
- Evans C. L., Hsu F. Y., Kosaka T. Utilization of blood sugar and formation of lactic acid by the lungs. J Physiol. 1934 Aug 24;82(1):41–61. doi: 10.1113/jphysiol.1934.sp003158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaviano V. V., Yo S., Masters T. Levels of lactate in lung tissue during sympathetic stimulation. Am J Physiol. 1967 Aug;213(2):437–440. doi: 10.1152/ajplegacy.1967.213.2.437. [DOI] [PubMed] [Google Scholar]
- HARRIS P., BAILEY T., BATEMAN M., FITZGERALD M. G., GLOSTER J., HARRIS E. A., DONALD K. W. LACTATE, PYRUVATE, GLUCOSE, AND FREE FATTY ACID IN MIXED VENOUS AND ARTERIAL BLOOD. J Appl Physiol. 1963 Sep;18:933–936. doi: 10.1152/jappl.1963.18.5.933. [DOI] [PubMed] [Google Scholar]
- HUCKABEE W. E. Relationships of pyruvate and lactate during anaerobic metabolism. III. Effect of breathing low-oxygen gases. J Clin Invest. 1958 Feb;37(2):264–271. doi: 10.1172/JCI103605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawarada Y., Wolferth C. C., Jr, Matsumoto T. Phenoxybenzamine and steroid in renal microcirculation in endotoxin shock. 1. Int Surg. 1972 Jan;57(1):17–22. [PubMed] [Google Scholar]
- Lozman J., Powers S. R., Jr, Older T., Dutton R. E., Roy R. J., English M., Marco D., Eckert C. Correlation of pulmonary wedge and left atrial pressures. A study in the patient receiving positive end expiratory pressure ventilation. Arch Surg. 1974 Aug;109(2):270–277. doi: 10.1001/archsurg.1974.01360020130025. [DOI] [PubMed] [Google Scholar]
- MITCHELL A. M., COURNAND A. The fate of circulating lactic acid in the human lung. J Clin Invest. 1955 Mar;34(3):471–476. doi: 10.1172/JCI103096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak E., Stubbs S. S., Seckman C. E., Hearron M. S. Effects of a single large intravenous dose of methylprednisolone sodium succinate. Clin Pharmacol Ther. 1970 Sep-Oct;11(5):711–717. doi: 10.1002/cpt1970115711. [DOI] [PubMed] [Google Scholar]
- Ongley P. A. Pediatric cardiology in Thailand. Circulation. 1966 Jul;34(1):1–3. doi: 10.1161/01.cir.34.1.1. [DOI] [PubMed] [Google Scholar]
- POWERS S. R., Jr, SCHAFFER C., BOBA A., NAKAMURA Y. Physical and biologic factors in impedance plethysmography. Surgery. 1958 Jul;44(1):53–62. [PubMed] [Google Scholar]
- Powers S. R., Jr, Mannal R., Neclerio M., English M., Marr C., Leather R., Ueda H., Williams G., Custead W., Dutton R. Physiologic consequences of positive end-expiratory pressure (PEEP) ventilation. Ann Surg. 1973 Sep;178(3):265–272. doi: 10.1097/00000658-197309000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochester D. F., Wichern W. A., Jr, Fritts H. W., Jr, Caldwell P. R., Lewis M. L., Giuntini C., Garfield J. W. Arteriovenous differences of lactate and pyruvate across healthy and diseased human lung. Am Rev Respir Dis. 1973 Mar;107(3):442–448. doi: 10.1164/arrd.1973.107.3.442. [DOI] [PubMed] [Google Scholar]
- Rokkanen P., Alho A., Avikainen V., Karaharju E., Kataja J., Lahdensuu M., Lepistö P., Tervo T. The efficacy of corticosteroids in severe trauma. Surg Gynecol Obstet. 1974 Jan;138(1):69–73. [PubMed] [Google Scholar]
- Rosenbaum R. W., Hayes M. F., Jr, Matsumoto T. Efficacy of steroids in the treatment of septic and cardiogenic shock. Surg Gynecol Obstet. 1973 Jun;136(6):914–918. [PubMed] [Google Scholar]
- SAMBHI M. P., WEIL M. H., UDHOJI V. N. ACUTE PHARMACODYNAMIC EFFECTS OF GLUCOCORTICOIDS; CARDIAC OUTPUT AND RELATED HEMODYNAMIC CHANGES IN NORMAL SUBJECTS AND PATIENTS IN SHOCK. Circulation. 1965 Apr;31:523–530. doi: 10.1161/01.cir.31.4.523. [DOI] [PubMed] [Google Scholar]
- Schumer W. Dexamethasone in oligemic shock. Physiochemical effects in monkeys. Arch Surg. 1969 Mar;98(3):259–261. doi: 10.1001/archsurg.1969.01340090035001. [DOI] [PubMed] [Google Scholar]
- Spath J. A., Jr, Gorczynski R. J., Lefer A. M. Possible mechanisms of the beneficial action of glucocorticoids in circulatory shock. Surg Gynecol Obstet. 1973 Oct;137(4):597–607. [PubMed] [Google Scholar]
- Strauss B., Caldwell P. R., Fritts H. W., Jr Observations on a model of prolifer- ative lung disease. I. Transpulmonary arteriovenous differences of lactate, pyruvate, and glucose. J Clin Invest. 1970 Jul;49(7):1305–1310. doi: 10.1172/JCI106345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan T. J., 3rd, Cavanagh D. Corticosteroids in endotoxin shock. Effect on renal vasomotion. Arch Surg. 1966 May;92(5):732–739. doi: 10.1001/archsurg.1966.01320230080015. [DOI] [PubMed] [Google Scholar]
- Swan H. J., Ganz W., Forrester J., Marcus H., Diamond G., Chonette D. Catheterization of the heart in man with use of a flow-directed balloon-tipped catheter. N Engl J Med. 1970 Aug 27;283(9):447–451. doi: 10.1056/NEJM197008272830902. [DOI] [PubMed] [Google Scholar]
- Thomas C. S., Jr, Brockman S. K. The role of adrenal corticosteroid therapy in Escherichia coli endotoxin shock. Surg Gynecol Obstet. 1968 Jan;126(1):61–69. [PubMed] [Google Scholar]
- Tierney D. F. Lactate metabolism in rat lung tissue. Arch Intern Med. 1971 May;127(5):858–860. [PubMed] [Google Scholar]
- WEIL M. H. Adrenocortical steroid for therapy of acute hypotension. Special reference to experiments on shock produced by endotoxin. Am Pract Dig Treat. 1961 Mar;12:162–168. [PubMed] [Google Scholar]
- WEIL M. H. The cardiovascular effects of corticosteroids. Circulation. 1962 Apr;25:718–725. doi: 10.1161/01.cir.25.4.718. [DOI] [PubMed] [Google Scholar]
- Weber K. C., Visscher M. B. Metabolism of the isolated canine lung. Am J Physiol. 1969 Oct;217(4):1044–1052. doi: 10.1152/ajplegacy.1969.217.4.1044. [DOI] [PubMed] [Google Scholar]
- Wilson J. W. Treatment or prevention of pulmonary cellular damage with pharmacologic doses of corticosteroid. Surg Gynecol Obstet. 1972 Apr;134(4):675–681. [PubMed] [Google Scholar]
- Wilson R. F., Fisher R. R. The hemodynamic effects of massive steroids in clinical shock. Surg Gynecol Obstet. 1968 Oct;127(4):769–776. [PubMed] [Google Scholar]
- Woodruff P., Caridis D., Cuevas P., Koizumi S., Fine J. Corticosteroid treatment of major trauma. Mechanisms involved in their therapeutic effect. Arch Surg. 1973 Oct;107(4):613–616. doi: 10.1001/archsurg.1973.01350220089019. [DOI] [PubMed] [Google Scholar]
- Yeager H., Jr, Massaro D. Glucose metabolism and glycoprotein synthesis by lung slices. J Appl Physiol. 1972 Apr;32(4):477–482. doi: 10.1152/jappl.1972.32.4.477. [DOI] [PubMed] [Google Scholar]


