Abstract
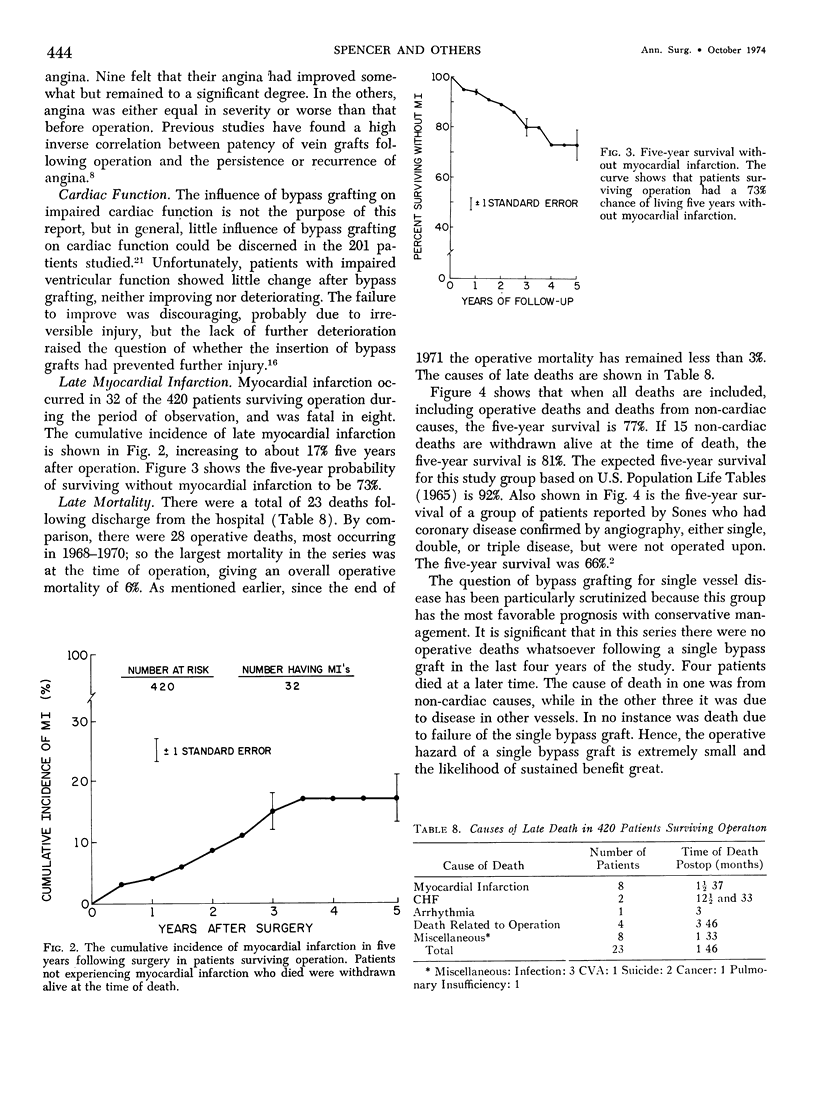
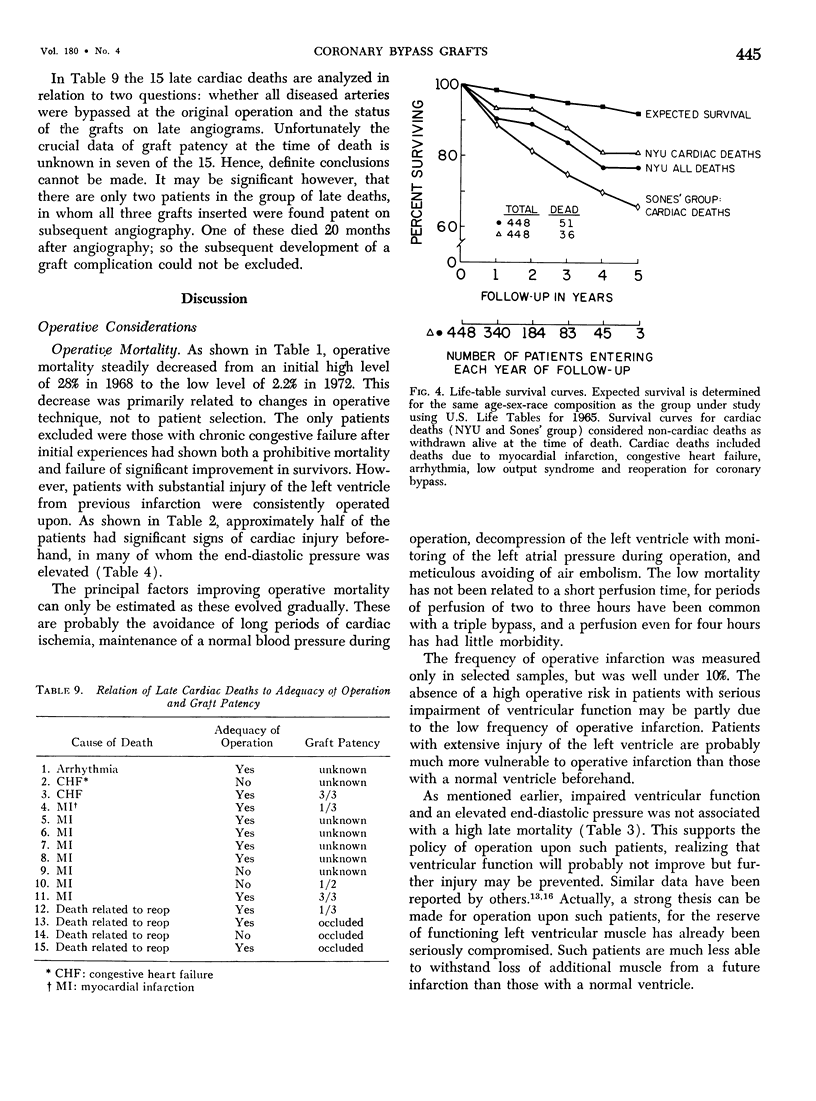
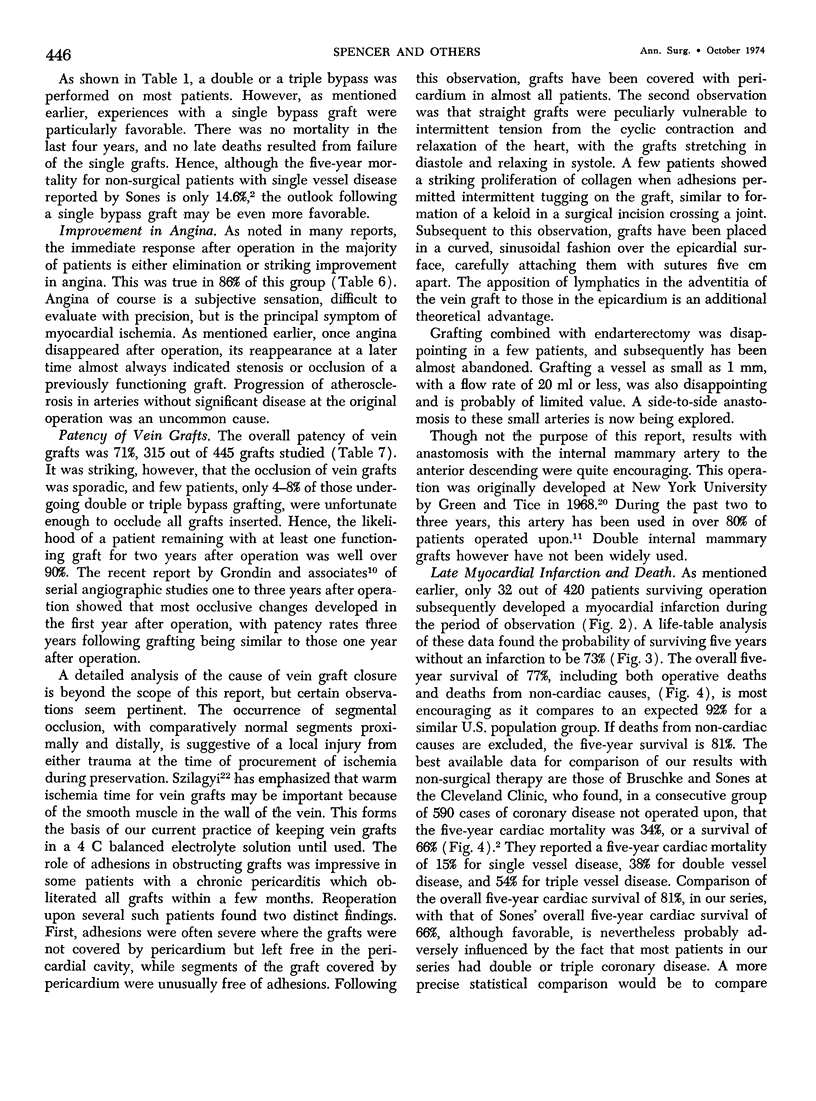
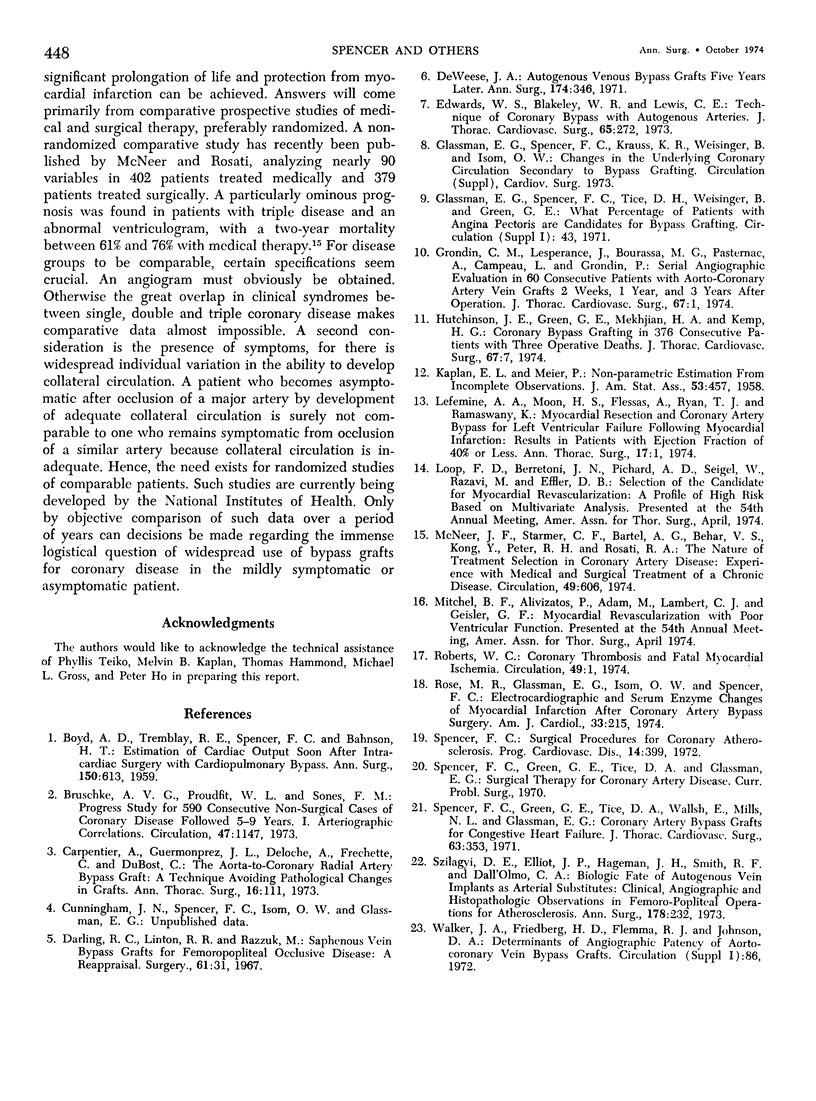
Approximately 1,000 coronary bypass procedures were performed at New York University between February 1968 and December 1973. This report reviews all elective operations performed for angina between 1968 and 1972, a total of 448 patients. In this five-year period the percentage of diseased arteries bypassed rose from 40% to 84%, and operative mortality decreased from 28% to less than 3%. There were a total of 28 operative deaths, mostly from myocardial infarction and low cardiac output. Operability was nearly 95%. The only fixed contraindication was chronic congestive failure. Over one-half of the patients had an abnormal ventriculogram, and there was some history of mild congestive failure in nearly 20%. Elevation of left ventricular end-diastolic pressure above 20 mm before operation was associated with a higher operative mortality, but the late mortality was similar to those with a normal preoperative end-diastolic pressure. In 383 surviving patients, angina was eliminated or greatly improved in 86%, unimproved in 12% and worse in 2%. Late angiograms were performed on 201 patients, studying a total of 445 venous grafts with an overall patency rate of 71%. Graft occlusion was sporadic and unpredictable, but over 90% of patients with multiple grafts remained with at least one patent graft. A late myocardial infarction occurred in 32 out of 420 patients surviving operation, and was fatal in eight. The cumulative incidence over a period of five years was 17%. Twenty-three deaths occurred following discharge from the hospital. Life-table analyses showed a five-year survival of 77% when all deaths were included, and a five-year cardiac survival of 81% when non-cardiac deaths were withdrawn alive at the time of death. The expected survival in a comparable population group without coronary disease was 92%, while data published by Sones of patients treated without operation showed a five-year cardiac survival of 66%. Current operative techniques have an operative mortality of 2-3% and a subclinical infarction rate of 5-10%. The ideal graft is yet evolving, but data with internal mammary artery grafts are most encouraging. A future goal should be a five-year graft patency of at least 80%. Because many infarcts probably develop from a relatively small decrease in coronary blood flow, either during rest or mild activity, the likelihood that future data will demonstrate a marked increase in longevity with bypass grafting is great.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BOYD A. D., TREMBLAY R. E., SPENCER F. C., BAHNSON H. T. Estimation of cardiac output soon after intracardiac surgery with cardiopulmonary bypass. Ann Surg. 1959 Oct;150:613–626. doi: 10.1097/00000658-195910000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruschke A. V., Proudfit W. L., Sones F. M., Jr Progress study of 590 consecutive nonsurgical cases of coronary disease followed 5-9 years. I. Arterographic correlations. Circulation. 1973 Jun;47(6):1147–1153. doi: 10.1161/01.cir.47.6.1147. [DOI] [PubMed] [Google Scholar]
- Carpentier A., Guermonprez J. L., Deloche A., Frechette C., DuBost C. The aorta-to-coronary radial artery bypass graft. A technique avoiding pathological changes in grafts. Ann Thorac Surg. 1973 Aug;16(2):111–121. doi: 10.1016/s0003-4975(10)65825-0. [DOI] [PubMed] [Google Scholar]
- Darling R. C., Linton R. R., Razzuk M. A. Saphenous vein bypass grafts for femoropopliteal occlusive disease: a reappraisal. Surgery. 1967 Jan;61(1):31–40. [PubMed] [Google Scholar]
- DeWeese J. A., Rob C. G. Autogenous venous bypass grafts five years later. Ann Surg. 1971 Sep;174(3):346–356. doi: 10.1097/00000658-197109000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards W. S., Blakeley W. R., Lewis C. E. Technique of coronary bypass with autogenous arteries. J Thorac Cardiovasc Surg. 1973 Feb;65(2):272–275. [PubMed] [Google Scholar]
- Grondin C. M., Lespérance J., Bourassa M. G., Pasternac A., Campneau L., Grondin P. Serial angiograpic evaluation in 60 consecutive patients with aorto-coronary artery vein grafts 2 weeks, 1 year, and 3 years after operation. J Thorac Cardiovasc Surg. 1974 Jan;67(1):1–6. [PubMed] [Google Scholar]
- Hutchinson J. E., 3rd, Green G. E., Mekhjian H. A., Kemp H. G. Coronary bypass grafting in 376 consecutive patients, with three operative deaths. J Thorac Cardiovasc Surg. 1974 Jan;67(1):7–16. [PubMed] [Google Scholar]
- Lefemine A. A., Moon H. S., Flessas A., Ryan T. J., Ramaswamy K. Myocardial resection and coronary artery bypass for left ventricular failure following myocardial infarction. Results in patients with ejection fraction of 40 per cent or less. Ann Thorac Surg. 1974 Jan;17(1):1–15. doi: 10.1016/s0003-4975(10)65052-7. [DOI] [PubMed] [Google Scholar]
- McNeer J. F., Starmer C. F., Bartel A. G., Behar V. S., Kong Y., Peter R. H., Rosati R. A. The nature of treatment selection in coronary artery disease. Experience with medical and surgical treatment of a chronic disease. Circulation. 1974 Apr;49(4):606–614. doi: 10.1161/01.cir.49.4.606. [DOI] [PubMed] [Google Scholar]
- Roberts W. Editorial: Coronary thrombosis and fatal myocardial ischemia. Circulation. 1974 Jan;49(1):1–3. doi: 10.1161/01.cir.49.1.1. [DOI] [PubMed] [Google Scholar]
- Rose M. R., Glassman E., Isom O. W., Spencer F. C. Electrocardiographic and serum enzyme changes of myocardial infarction after coronary artery bypass surgery. Am J Cardiol. 1974 Feb;33(2):215–220. doi: 10.1016/0002-9149(74)90277-x. [DOI] [PubMed] [Google Scholar]
- Spencer F. C. Surgical procedures for coronary atherosclerosis. Prog Cardiovasc Dis. 1972 Jan;14(4):399–419. doi: 10.1016/0033-0620(72)90033-3. [DOI] [PubMed] [Google Scholar]
- Szilagyi D. E., Elliott J. P., Hageman J. H., Smith R. F., Dall'olmo C. A. Biologic fate of autogenous vein implants as arterial substitutes: clinical, angiographic and histopathologic observations in femoro-popliteal operations for atherosclerosis. Ann Surg. 1973 Sep;178(3):232–246. doi: 10.1097/00000658-197309000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]


