Abstract
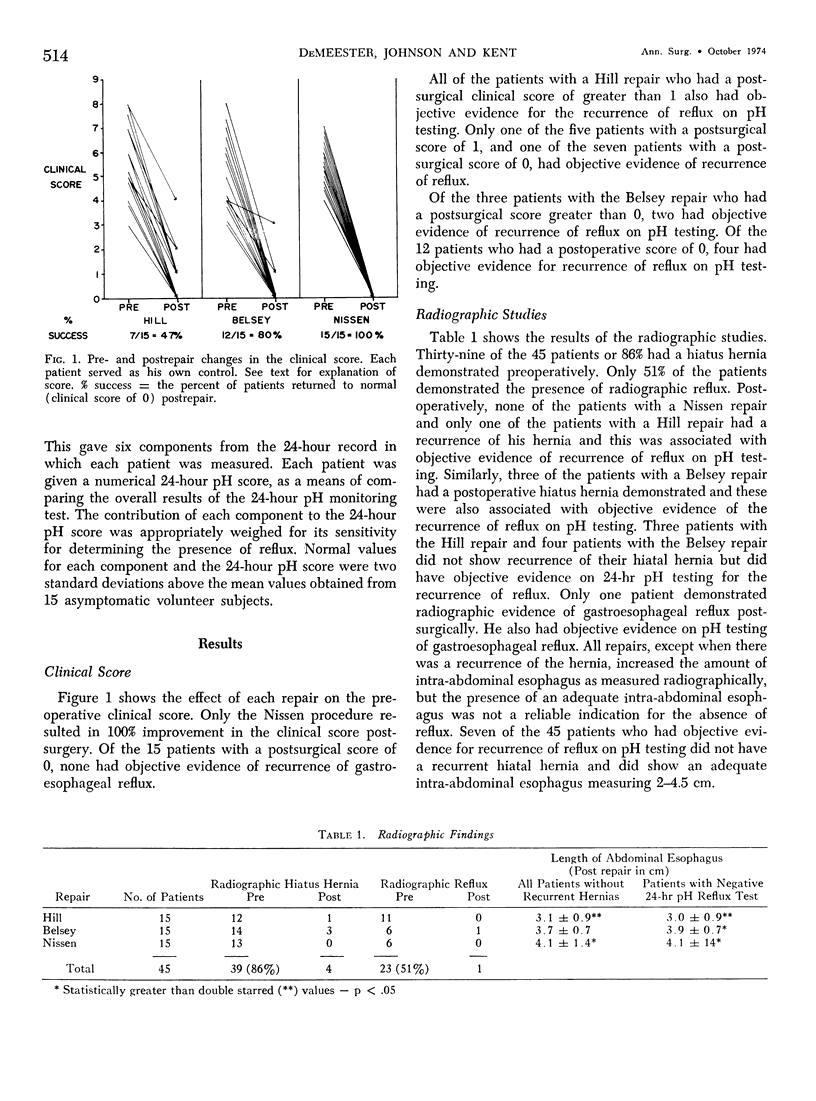
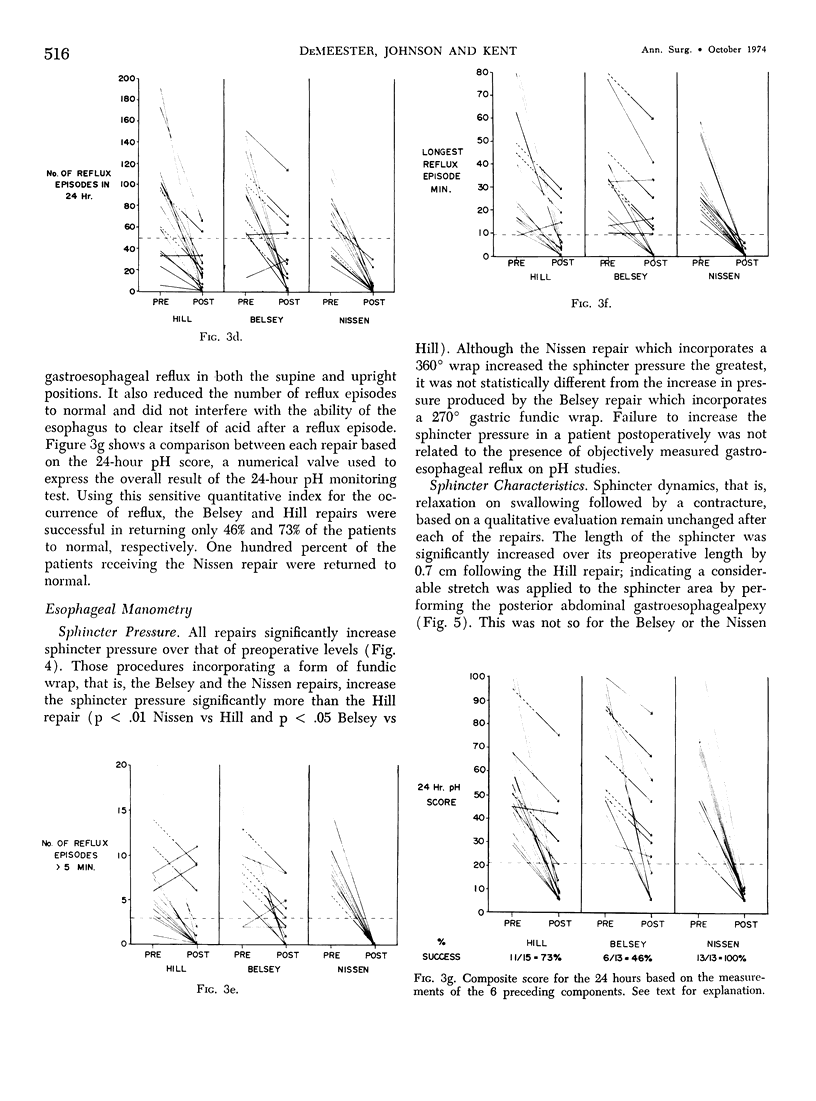
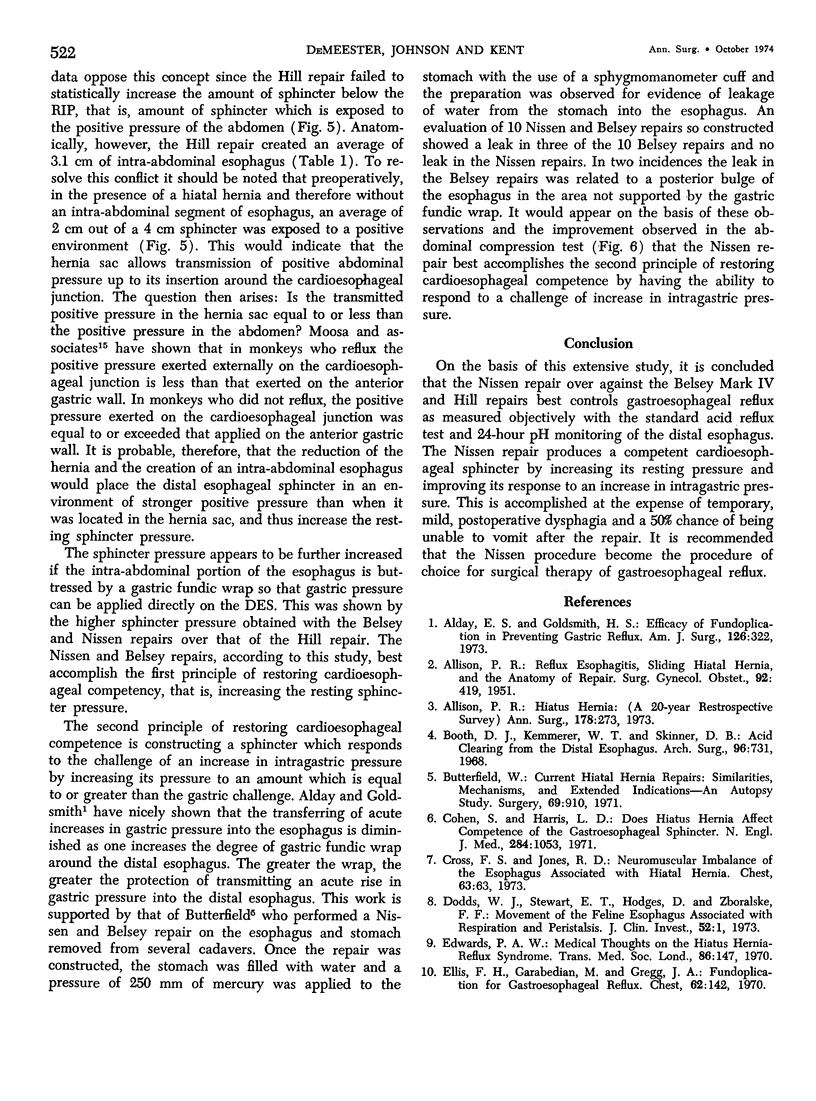
A prospective randomized study was done on 45 patients to evaluate the effectiveness of the Hill, Nissen or Belsey anti-reflux procedure. All patients had symptoms of GE reflux unresponsive to medical therapy, a + standard acid reflux test (SART), and esophagitis (38/45) or + Burnstein test (7/45). Esophageal symptomatic, radiographic, manometric and pH (SART and 24-hr monitoring) evaluation was done pre- and 154 days (ave.) postsurgery. All procedures improved the symptoms of pyrosis. The best improvement was seen after the Nissen repair. All procedures increased the distal esophageal sphincter (DES) pressures over preoperative levels. The Nissen and Belsey increased it more than the Hill. Sphincter length and dynamics remained unchanged. The Nissen procedure placed more of the manometric sphincter below the respiratory inversion point in the positive pressure environment of the abdomen. The esophageal length was increased by the Nissen and Hill repairs. This was thought to account for the high incidence of temporary postsurgery dysphagia following the Nissen and Hill repairs and the lower incidence following the Belsey repair. Reflux was most effectively prevented by the Nissen repair, as shown by the SART and the 24-hr esophageal pH monitoring, a sensitive measurement of frequency and duration of reflux. The average length of hospital stay was 20 days for Belsey and 12 days for both Nissen and Hill procedure. Postsurgery complications were more common following the thoracic than the abdominal approach. Ability to vomit postrepair was greatest with the Hill and least with the Belsey and Nissen repair. All procedures temporarily increased amount of flatus. It is concluded that the Nissen repair best controls reflux and its symptoms by providing the greatest increase in DES pressure and placing more of the sphincter in the positive abdominal environment. This is accomplished with the lowest morbidity but at the expense of temporary postoperative dysphagia and a 50% chance of being unable to vomit after the repair.
Full text
PDF









Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ALLISON P. R. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg Gynecol Obstet. 1951 Apr;92(4):419–431. [PubMed] [Google Scholar]
- Alday E. S., Goldsmith H. S. Efficacy of fundoplication in preventing gastric reflux. Am J Surg. 1973 Sep;126(3):322–324. doi: 10.1016/s0002-9610(73)80117-5. [DOI] [PubMed] [Google Scholar]
- Allison P. R. Hiatus hernia: (a 20-year retrospective survey). Ann Surg. 1973 Sep;178(3):273–276. doi: 10.1097/00000658-197309000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth D. J., Kemmerer W. T., Skinner D. B. Acid clearing from the distal esophagus. Arch Surg. 1968 May;96(5):731–734. doi: 10.1001/archsurg.1968.01330230039006. [DOI] [PubMed] [Google Scholar]
- Butterfield W. C. Current hiatal hernia repairs: similarities, mechanisms, and extended indications--an autopsy study. Surgery. 1971 Jun;69(6):910–916. [PubMed] [Google Scholar]
- Cohen S., Harris L. D. Does hiatus hernia affect competence of the gastroesophageal sphincter? N Engl J Med. 1971 May 13;284(19):1053–1056. doi: 10.1056/NEJM197105132841902. [DOI] [PubMed] [Google Scholar]
- Cross F. S., Jones R. D. Neuromuscular imbalance of the esophagus associated with hiatal hernia. Chest. 1973 Jan;63(1):63–68. doi: 10.1378/chest.63.1.63. [DOI] [PubMed] [Google Scholar]
- Dodds W. J., Stewart E. T., Hodges D., Zboralske F. F. Movement of the feline esophagus associated with respiration and peristalsis. An evaluation using tantalum markers. J Clin Invest. 1973 Jan;52(1):1–13. doi: 10.1172/JCI107152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards D. A. Medical thoughts on the "hiatus hernia-reflux" syndrome. Trans Med Soc Lond. 1970;86:147–153. [PubMed] [Google Scholar]
- Ellis F. H., Jr, Garabedian M., Gregg J. A. Fundoplication for gastroesophageal reflux. A comparison of preoperative and early postoperative manometric findings. Chest. 1972 Aug;62(2):142–145. doi: 10.1378/chest.62.2.142. [DOI] [PubMed] [Google Scholar]
- Hill L. D. An effective operation for hiatal hernia: an eight year appraisal. Ann Surg. 1967 Oct;166(4):681–692. doi: 10.1097/00000658-196710000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moossa A. R., Cooley G. R., Skinner D. B. Intraluminal and intraperitoneal pressures at the cardia: effect of hormones and surgical intervention. Surg Forum. 1973;24:370–372. [PubMed] [Google Scholar]
- NISSEN R. Gastropexy and "fundoplication" in surgical treatment of hiatal hernia. Am J Dig Dis. 1961 Oct;6:954–961. doi: 10.1007/BF02231426. [DOI] [PubMed] [Google Scholar]
- Polk H. C., Jr, Zeppa R. Hiatal hernia and esophagitis: a survey of indications for operation and technic and results of fundoplication. Ann Surg. 1971 May;173(5):775–781. doi: 10.1097/00000658-197105000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner D. B., Belsey R. H. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J Thorac Cardiovasc Surg. 1967 Jan;53(1):33–54. [PubMed] [Google Scholar]
- Skinner D. B., Booth D. J. Assessment of distal esophageal function in patients with hiatal hernia and-or gastroesophageal reflux. Ann Surg. 1970 Oct;172(4):627–637. doi: 10.1097/00000658-197010000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]


