Abstract
Background
Overweight older adults are often counseled to lose weight, even though there is little evidence of excess mortality in that age group. Overweight and underweight may be more associated with health status than with mortality, but few clinical trials of any kind have been based on maximizing years of healthy life (YHL), as opposed to years of life (YOL).
Objective
This paper examines the relationship of body mass index (BMI) to both YHL and YOL. Results were used to determine whether clinical trials of weight-modification based on improving YHL would be more powerful than studies based on survival.
Design
We used data from a cohort of 4,878 non-smoking men and women aged 65–100 at baseline (mean age 73) and followed 7 years. We estimated mean YHL and YOL in four categories of BMI: underweight, normal, overweight, and obese.
Results
Subjects averaged 6.3 YOL and 4.6 YHL of a possible 7 years. Both measures were higher for women and whites. For men, none of the BMI groups was significantly different from the normal group on either YOL or YHL. For women, the obese had significantly lower YHL (but not YOL) than the normals, and the underweight had significantly lower YOL and YHL. The overweight group was not significantly different from the normal group on either measure.
Conclusions
Clinical trials of weight loss interventions for obese older women would require fewer participants if YHL rather than YOL was the outcome measure. Interventions for obese men or for the merely overweight are not likely to achieve differences in either YOL or YHL. Evaluations of interventions for the underweight (which would presumably address the causes of their low weight) may be conducted efficiently using either outcome measure.
Keywords: Aged, Mortality, QALY, Self-rated health, Active life expectancy, Ideal weight, Body mass index, Elderly
Introduction
Older adults are frequently counseled to lose weight, even though there is little evidence that overweight is associated with increased mortality in those over age 65. Six large controlled population-based studies of non-smoking older adults have investigated the association between body mass index (BMI) and mortality, controlling for relevant covariates [1-6]. All studies found excess risk for persons with very low BMI, but that persons with moderately high BMI had little or no extra risk except in certain small subsets. A review of 13 studies of older adults drew similar conclusions [7].
Many healthy older adults report gradual weight gain throughout adult life. It may be that a small amount of gradual weight gain is normative and associated with the most robust health as we age. It has been suggested that weight standards be adjusted upwards for age [8]. Such recommendations remain controversial, however, because the number of studies of older persons is fairly small, and because few studies have examined the relation of BMI to quality of life or years of healthy life (YHL) in the elderly [9].
In older adults, risk factors may have a greater effect on health than on mortality. If so, then behavior change trials of weight modification might be more successful if they were evaluated on improved health, rather than on decreased mortality. Clinical trials powered to detect differences in YHL would often require fewer subjects than trials to detect survival differences or cardiovascular events [10]. In this paper we study whether BMI at baseline is associated with living longer, and/or with more years of being healthy, in a cohort of older adults for whom risk factors, subclinical disease, and morbidity are well characterized. The goal is to determine whether analyses based on years of life (YOL) or on YHL would provide substantively different results, and which measure would yield more powerful evaluations of weight modification interventions in older adults.
Materials and methods
Study design: The Cardiovascular Health Study
The Cardiovascular Health Study (CHS) is a population-based longitudinal study of 5,888 adults aged 65 and older at baseline [11]. Subjects were recruited from a random sample of the Medicare eligibility lists in four US counties. Extensive baseline data were collected for all subjects using a baseline home interview, an annual mail questionnaire, and annual clinic examinations. Additional information was collected in a brief telephone interview 6 months after each scheduled visit. Two cohorts were followed, one with 7 years of follow-up (n = 5,201) and the second (all African American, n = 687) with 4 years of follow-up to date. Data collection began in 1989, and follow-up is virtually complete for all surviving subjects [12].
Body mass index
BMI was calculated as measured weight in kilograms divided by the square of measured height in meters. A report from the National Heart Lung and Blood Institute classifies normal weight (without reference to age) as a BMI of 18.5 to 24.9; overweight as 25 to 29.9; and obesity as 30.0 and higher [13]. We consider separately the group with BMI between 18.5 and 20, which was associated with lower survival in studies cited above.
Years of life and years of healthy life
YOL is the number of years that a person lived in the 7 years after baseline. YHL is the number of years in which the person was 'healthy', and is similar in concept to quality-adjusted life-years, healthy year equivalents, or active life expectancy [14]. We based YHL on self-rated health (is your health excellent, very good, good, fair, or poor?) (EVGFP) which was collected every 6 months. EVGFP is a simple but well-known measure, which has been studied in detail [15,16], and is predictive of health events in many studies [17]. Because we are examining health status over time, we added a sixth health state, dead. Data were available about 93% of the time. We used linear interpolation to estimate missing data when there were known values before and after the missing value, bringing the percent complete to 95% [18].
For this analysis we defined YHL as the number of years (of 7) in which a person reported excellent, very good, or good health (were 'healthy'). YHL ranges from 0 (for persons who were never in excellent, very good, or good health) to 7 years (for persons who were healthy throughout). Since people reported their health every 6 months, YHL has a reasonably continuous distribution. A drawback of this simple definition of 'healthy' is that it does not distinguish between fair or poor health and death, since all are considered 'not healthy'. We also used an alternative approach, which assigns a different value to each level of EVGFP [19]. Preliminary results were similar for the two approaches, however, and we report results using only the simpler definition.
The calculations had to be modified to include the 438 persons in the second African American cohort, who have been followed only 4 years to date. For those persons, and for 70 persons in the first cohort who did not have complete data, we estimated the last 4 years of YOL and YHL from their age, sex, and health at the end of 3 years, using validated methods presented elsewhere [20]. That article showed that estimated 4-year YOL and YHL were unbiased for the African American cohort. In the primary analysis we used observed 7-year YOL and YHL when they were available, and observed 3-year YOL and YHL plus 4-year estimated YOL and YHL when they were not (about 10% of the sample). We performed all analyses with and without the persons who had partially estimated data, to ensure that the estimation had not distorted the findings.
Covariates
The goal is to examine the association of YOL and YHL with BMI. To adjust for possible confounding we chose baseline covariates that were prevalent in the elderly, related to mortality and morbidity in previous studies, and likely to be related to BMI. Self-reported covariates include age, gender, smoking (never or former), history of arthritis, cancer, diabetes, fair or poor self-rated health status, limitations in activities of daily living or in instrumental activities of daily living, and 10 pounds or more unintended weight loss in the year before baseline. Clinical covariates include hypertension, cardiovascular disease (prevalent heart disease, peripheral vascular disease, or cerebrovascular disease), maximum thickness of the internal carotid artery, depression (CESD score), serum albumin, serum cholesterol, and serum creatinine. These measures are explained in more detail elsewhere [21-24]. We excluded 697 current smokers and 313 others with incomplete covariate data, leaving 4,878 persons on whom this analysis is based.
Analysis
All analyses were performed separately for men and women. We calculated two sets of adjusted values, as follows. We regressed YOL and YHL first on age, age squared, race, and smoking history (former or never), and second on all of the covariates listed above. We calculated adjusted YOL as a person's observed YOL minus predicted YOL (from the regression) plus the mean YOL (6.52 years for women or 6.06 for men). That is, a person's adjusted YOL is his residual from the regression plus the grand mean. The mean of this new variable, for a group of subjects, is the adjusted mean YOL for that group. Adjusted YHL was calculated in a similar manner. We calculated two sets of adjusted variables because of the possibility of 'over-adjustment', controlling inappropriately for factors (such as diabetes) which may have been causally affected by the person's weight. We plotted mean adjusted YOL and YHL against BMI, and tested for difference among BMI groups using confidence intervals or analysis of variance. Finally we calculated the effect size for each measure, comparing each BMI subgroup to the 'normal' group. The effect size is the difference in mean YOL (or YHL) in two groups divided by their common standard deviation. Since the sample size required to detect an effect of this magnitude is proportional to the inverse of the squared effect size, large effect sizes are desirable.
Results
Table 1 shows the distribution of key variables by sex and race. Mean age at baseline was 73.1 and about two thirds of the men and a third of the women were former smokers. Black women had a higher mean BMI and higher percent obese (BMI ≥ 30) than the other three groups. Black men were most likely to have unintentionally lost more than 10 pounds in the past year; white women were least likely.
Table 1.
Distributions of key baseline variables by sex and race
| Black Women |
Black Men |
White Women |
White Men |
All | ||
| N | 449 | 240 | 2329 | 1860 | 4878 | |
| Age at baseline | Mean | 73.1 | 73.3 | 72.6 | 73.6 | 73.1 |
| Std deviation | 5.6 | 5.7 | 5.4 | 5.7 | 5.6 | |
| Former smoker | % | 32.7 | 60.8 | 35.5 | 64.7 | 47.6 |
| Body mass index | Mean | 30.0 | 27.0 | 26.4 | 26.4 | 26.8 |
| Std deviation | 5.8 | 4.1 | 4.9 | 3.6 | 4.6 | |
| BMI ≥ 30 | % | 43.2 | 17.9 | 19.7 | 15.7 | 20.3 |
| 10# unintended wt loss | % | 8.0 | 12.1 | 6.2 | 7.1 | 7.0 |
| YOL, adjusted for age | Mean | 6.3 | 5.7 | 6.6 | 6.1 | 6.3 |
| Std deviation | 1.3 | 1.7 | 1.2 | 1.6 | 1.4 | |
| YHL, adjusted for age | Mean | 4.2 | 3.9 | 4.9 | 4.6 | 4.6 |
| Std deviation | 1.4 | 1.6 | 1.5 | 1.7 | 1.6 | |
| Yrs of Unhealthy Life | Mean | 2.1 | 1.9 | 1.7 | 1.5 | 1.7 |
| (YOL-YHL) | Std deviation | 1.1 | 1.1 | 1.1 | 1.1 | 1.1 |
| Yrs lost to death | Mean | .7 | 1.3 | .4 | .9 | .7 |
| (7 minus YOL) | Std deviation | 1.3 | 1.7 | 1.2 | 1.6 | 1.4 |
About 78% of the subjects were healthy at baseline, declining to 57% at the end of 7 years; 20% had died (data not shown). Of the 22% who were unhealthy (fair or poor) at baseline, about 24% were healthy 7 years later. There was thus substantial change in EVGFP over time, in both directions. Table 1 shows the mean YOL and YHL (calculated from EVGFP) in the first seven years of the study, adjusted to age 73. For example, black women averaged 6.3 YOL, but only 4.2 YHL of a maximum possible 7. We calculated some additional descriptive statistics, shown in the final two lines: years of unhealthy life (YOL minus YHL) and years lost to death (7 minus YOL). White women had the most YHL and black men the fewest; black women had the most years of unhealthy life, and white men the fewest; black men lost the most years to death (1.3 out of 7) while white women lost only 0.4 years. For blacks, about 68% of their YOL were healthy (YHL/YOL, not shown); for whites, about 75% were healthy.
Among whites, the gender differences in Table 1 were statistically significant (p <.05) except for BMI and unintended weight loss. Among blacks, gender differences were significant except for 10 pounds unintended weight loss and weight loss since age 50. Among males, there were significant differences between black and white for BMI, unintended weight loss, YOL, YHL, years of unhealthy life, and years lost to death. Whites in the sample had higher income and education (data not shown). After adjusting for income and education, as well as age and former smoking, the difference in BMI was no longer statistically significant. Among females, blacks and whites differed significantly on BMI, BMI>30, weight loss since age 50, YOL, YHL, years of unhealthy life, and years lost to death. After adjustment for income and education, the difference in weight loss since age 50 was no longer significant. Blacks had significantly lower YOL and YHL than whites after adjustment for age, but the difference disappeared after adjustment for the entire set of health-related baseline covariates (analyses not shown).
We next examined the relationship of BMI to YOL and YHL. Table 2 presents the mean values of YOL and YHL, adjusted for age, race, and previous smoking (columns 1 and 3), and also adjusted for the entire set of covariates (columns 2 and 4). For example, YOL for women, adjusted for age, race, and smoking, averaged 6.0 years for women with a baseline BMI below 18.5, but averaged 6.6 years for women with a BMI from 25 to 29.9. The second column, which shows results adjusted for all covariates, is not very different (the only discrepancy is for men with BMI < 18.5, a category containing only 14 men). Adjustment for extensive covariates also made little difference for YHL (columns 3 and 4). Subsequent analyses are adjusted only for age, race, and former smoking. As mentioned above, the group with BMI from 18.5 to 20 would be considered 'normal' by the NHLBI guidelines, but had lower YOL and YHL than those with 20–24.9 in all comparisons. For this reason, and to increase sample size for those with low BMI, we combined the two lower categories, defining underweight as a BMI under 20.
Table 2.
YOL and YHL by BMI and sex. Adjusted for age/race/smoking, and for all covariates.
| BMI | YOL (7 Yrs), adj for age, race, past smoking | YOL (7 Yrs), adj for all variables* | YHL (7 Yrs), adj for age, race, past smoking | YHL (7 Yrs), adj for all variables* | N | |
| Women | <18.5 | 6.0 | 6.1 | 4.1 | 4.2 | 53 |
| 18.5–19.9 | 6.3 | 6.3 | 4.8 | 4.7 | 90 | |
| 20.0–24.9 | 6.5 | 6.5 | 4.9 | 4.8 | 938 | |
| 25.0–29.9 | 6.6 | 6.5 | 4.8 | 4.8 | 1,044 | |
| 30+ | 6.5 | 6.6 | 4.4 | 4.7 | 653 | |
| Men | <18.5 | 5.1 | 5.5 | 3.7 | 4.3 | 14 |
| 18.5–19.9 | 5.6 | 5.6 | 4.4 | 4.2 | 28 | |
| 20.0–24.9 | 6.0 | 6.0 | 4.5 | 4.4 | 701 | |
| 25.0–29.9 | 6.1 | 6.1 | 4.6 | 4.5 | 1,021 | |
| 30+ | 6.1 | 6.1 | 4.3 | 4.4 | 336 |
• The self-reported covariates were: age, gender, smoking (never or former), history of arthritis, cancer, diabetes, fair or poor self-rated health status, limitations in activities of daily living or in instrumental activities of daily living, and 10 pounds or more unintended weight loss in the year before baseline. Clinical covariates were: hypertension, cardiovascular disease (prevalent heart disease, peripheral vascular disease, or cerebrovascular disease), maximum thickness of the internal carotid artery, depression (CESD score), serum albumin, serum cholesterol, and serum creatinine.
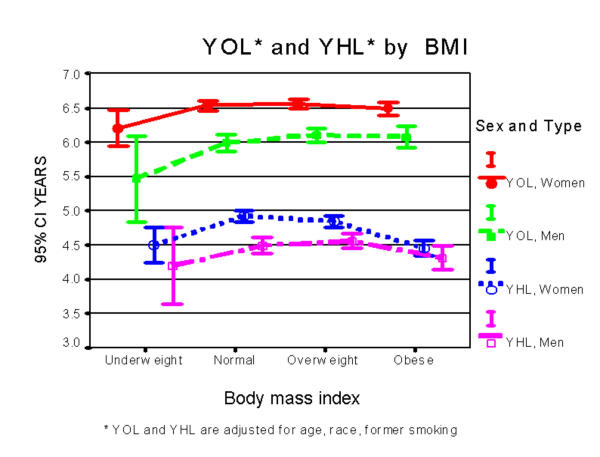
Figure 1 is a plot of adjusted YOL and YHL by sex and BMI. For each BMI category the mean and its 95% confidence interval are plotted. Categories whose confidence intervals do not overlap, or overlap only slightly, are significantly different. The bars are slightly offset to permit all error bars to be seen.
Figure 1.
*YOL and YHL are adjusted for age, race, former smoking.
YOL for women (the uppermost curve on Figure 1) averaged about 6.5 out of 7 years, and showed no evident association between BMI and YOL for BMI above 20. Underweight women averaged about .25 fewer YOL than other women (p < .05 compared with normal group). Underweight men also had lower YOL, but this group was not significantly different from the normal group, in part because of low sample size. Men classified as normal, overweight or obese all had about the same YOL.
The lowermost two lines in Figure 1 show mean YHL for women and men. Women who were normal or overweight averaged about 4.9 YHL. The YHL for underweight or obese women was about 4.5 years, which was significantly lower than the normal group. The relationship of BMI to YHL for men is similar, but differences among BMI groups were not statistically significant. YHL was significantly higher for women than for men in the normal and overweight groups, but the sexes had similar YHL in the underweight and obese groups.
We next present the effect size for comparing each group to the normal BMI group. The effect sizes are shown in Table 3, with the significance results of the associated t-tests for the differences in means of the two groups being compared. For example, underweight women averaged 4.50 YHL compared to 4.92 for normal women, and the common standard deviation was 1.44. The effect size is thus (4.92–4.50)/1.44 = .29. The two groups had significantly different YHL, implying that the effect size is also significantly greater than zero. A clinical trial of a treatment to help underweight women achieve normal weight (presumably by addressing the underlying cause) could be expected to have 80% power with N = (1.96+.84)2/.292 = about 93 women per treatment arm, if 7-year YHL were the outcome measure.
Table 3.
Estimated effect sizes, comparing normal to other BMI categories
| Women | Women | Men | Men | |
| YHL | YOL | YHL | YOL | |
| Underweight | .290* | .270* | .174 | .298' |
| Overweight | .054 | -.020 | -.035 | -.065 |
| Obese | .328* | .039 | .103 | -.057 |
* Effect size is significantly different from zero (p < .01). ' P = .06, because of small sample size (n = 42) in the underweight group
The biggest effect sizes are in the first row, comparing underweight to normal. YHL and YOL have similar effect sizes for women, and are significantly different from zero. The effect sizes are not significantly different from zero for men, in part because there were only 42 men in the underweight category. The effect size comparing overweight to normal yielded small, non-significant effect sizes, with inconsistent signs, suggesting extremely large sample sizes would be needed. For comparing obese to normal, only YHL for women showed a large and significant effect size. Thus, an intervention to improve the health of underweight women to that of their normal weight peers could be performed using either YHL or YOL as the outcome variable. Trials to make obese women comparable to normal women could be evaluated using YHL, but not YOL. Trials to improve the health of the other groups to that of the normals would probably be fruitless since there is no evidence that being overweight (for men or women) or obese (for men) affects YOL or YHL.
As mentioned above, we repeated these analyses excluding the persons with partially estimated data, and using two different ways of coding YHL. The only substantive change was that some of the differences between blacks and whites shown in Table 1 were no longer statistically significant, due to a smaller sample size.
Discussion
As expected, women averaged more YOL than men, even after adjustment for a variety of baseline covariates. The proportion of life spent in good health was similar for men and women. The differences between black and white subjects could be explained substantially by the complete set of baseline covariates, suggesting that differences in the burden of disease are responsible for racial differences in YOL and in YHL [25].
Our findings based on YOL are consistent with the literature on older adults, which consistently finds worse mortality for the underweight but little association with high weight. [5,9,26] Some studies have shown lower health-related quality of life in overweight persons, but these studies included few older adults [27,28]. Our analysis, based only on the elderly, detected diminished health for the obese and the underweight, but not for the overweight. YOL and YHL thus perform similarly to one another in trials that involve middle-aged persons, but yield somewhat different results in trials involving the elderly.
The association of obesity with YHL was stronger for women than for men (Figure 1). Since women spend more years in poor health than men do, it may not be surprising that results for men and women are different. Another possibility, however, is that obese women were more likely than men to down-rate their health because of society's pressure on women to be slender [29]. Measures of YHL that did not have such a bias would be preferable.
Optimal weight and overweight
Recent studies have defined obesity without reference to age [6,13,30]. Andres et al proposed a desirable BMI of 24–30 for persons aged 60 to 69 [8]. Allison et al[31] proposed 27–30 for older men and 30–35 for older women. In Figure 1, the overweight (as opposed to the obese) are no different from those of normal weight, suggesting that these two categories could be combined for older adults. Since future improvements in life expectancy may be limited [32], the greatest advances may be made by improving people's YHL. This suggests that the development of future guidelines should take YHL or other measures of quality of life into account.
Implications for clinical trials
Based on these findings, trials to address obesity in older women could be efficient if YHL (but not YOL) was the outcome measure. That is, women who changed from being obese to being normal would likely show changes in YHL, but not YOL. Clinical trials of weight modification interventions for older adults who were merely overweight would appear to be fruitless since the interventions would probably not have a direct effect on either YOL or YHL.
Weight or weight change are sometimes used as the outcome in evaluations of interventions such as diet or exercise programs. The fact that weight is not associated in a consistent way with health suggests that such evaluations should be considered critically when older adults are the subjects. This is particularly important in the light of recent findings, which found that interventions such as weight-loss drugs may be harmful [33,34]. For older adults, the risks associated with higher weight are especially unclear, and the optimal outcome for a trial of weight loss in older adults requires specific attention to improved health and mortality.
Interestingly, the strongest health relationships were found for underweight older adults. Clinical trials whose objective was to make the underweight as healthy as their normal-weight peers (presumably by addressing the underlying conditions that caused the low weight) could be performed efficiently using either YOL or YHL as the outcome measure. Both YOL and YHL would be clinically significant in this patient group.
Potential limitations
CHS participants were somewhat healthier than the average older adult; however, adjustment for detailed covariates made little difference in the findings. We estimated the last four years of health data for about 10% of the sample, but results with and without this group were similar. Analysis of mean YOL instead of the more traditional survival analysis survival analysis was appropriate here, since virtually no persons were lost to follow-up. Biases caused by over-adjustment are probably not large, since the findings were not sensitive to the number of variables adjusted for.
These results are for a 7-year follow-up. The relative superiority of YHL to YOL would probably hold in trials with shorter follow-up. The effect sizes in Table 3 might also be appropriate in shorter trials, since lengthy trials often add little information [10].
EVGFP, on which YHL was based, might have missed some effects of obesity on risk factors for future health. A person who is depressed because of a poor self-image related to obesity or who has osteo-arthritis related to obesity and limits to activities to successfully avoid pain would surely have worse EVGFP than others, based on results from many studies. However, health measures designed specifically to measure those conditions might be more sensitive to change in weight than EVGFP. If YHL were based on such measures, the superiority of YHL to YOL would likely be even greater than that shown here. These more sensitive measures might also have detected differences between the overweight and normal weight persons, but we think this is unlikely given the absence of any differences in EVGFP.
Conclusion
Recommendations for desirable weight have been criticized for emphasizing mortality rather than health. We found associations between YHL and obesity that were not present in the mortality analysis, suggesting that YHL may be a more sensitive measure of the burden of obesity in older adults, especially for women. Future efforts to determine desirable weight guidelines should include measures of YHL. Using either YOL or YHL, however, we found no excess risk for older adults who would be classified as 'overweight' by the NHLBI guidelines. This suggests using YHL as the outcome measure in clinical trials involving obese or underweight older adults, and discouraging trials that address older adults who are merely overweight.
Competing interests
None declared
Abbreviations
BMI Body mass index
CESD Center for Epidemiologic Studies Depression Scale
CHS Cardiovascular Health Study
EVGFP Is your health excellent, very good, good, fair or poor?
QALY Quality-adjusted life years
YHL Years of healthy life
YOL Years of life
Acknowledgments
Acknowledgements
Forsyth County, NC-Wake Forest University School of Medicine: Gregory L. Burke, Sharon Jackson, Alan Elster, Curt D. Furberg, Gerardo Heiss, Dalane Kitzman, Margie Lamb, David S. Lefkowitz, Mary F. Lyles, Cathy Nunn, Ward Riley, John Chen, Beverly Tucker. Forsyth County, NC-Wake Forest University-ECG Reading Center: Farida Rautaharju, Pentti Rautaharju. Sacramento County, CA-University of California, Davis: William Bonekat, Charles Bernick, Michael Buonocore, Mary Haan, Calvin Hirsch, Lawrence Laslett, Marshall Lee, John Robbins, William Seavey, Richard White. Washington County, MD-The Johns Hopkins University: M. Jan Busby-Whitehead, Joyce Chabot, George W. Comstock, Adrian Dobs, Linda P. Fried, Joel G. Hill, Steven J. Kittner, Shiriki Kumanyika, David Levine, Joao A. Lima, Neil R. Powe, Thomas R. Price, Jeff Williamson, Moyses Szklo, Melvyn Tockman. Washington County, MD-The Johns Hopkins University-MRI Reading Center: Norman Beauchamp, R. Nick Bryan, Douglas Fellows, Melanie Hawkins, Patrice Holtz, Naiyer Iman, Michael Kraut, Cynthia Quinn, Grace Lee, Carolyn C. Meltzer, Larry Schertz, Earl P. Steinberg, Scott Wells, Linda Wilkins, Nancy C. Yue; Allegheny County, PA-University of Pittsburgh: Diane G. Ives, Charles A. Jungreis, Laurie Knepper, Lewis H. Kuller, Elaine Meilahn, Peg Meyer, Roberta Moyer, Anne Newman, Richard Schulz, Vivienne E. Smith, Sidney K. Wolfson. University of California, Irvine-Echocardiography Reading Center (baseline): Hoda Anton-Culver, Julius M. Gardin, Margaret Knoll, Tom Kurosaki, Nathan Wong. Georgetown Medical Center-Echocardiography Reading Center (follow-up): John Gottdiener, Eva Hausner, Stephen Kraus, Judy Gay, Sue Livengood, Mary Ann Yohe, Retha Webb. New England Medical Center, Boston-Ultrasound Reading Center: Daniel H. O'Leary, Joseph F. Polak, Laurie Funk. University of Vermont-Central Blood Analysis Laboratory: Elaine Cornell, Mary Cushman, Russell P. Tracy. University of Arizona, Tucson-Pulmonary Reading Center: Paul Enright. University of Washington, Seattle-Coordinating Center: Alice Arnold, Annette L. Fitzpatrick, Richard A. Kronmal, Bruce M. Psaty, David S. Siscovick, Will Longstreth, Patricia W. Wahl, David Yanez, Paula Diehr, Corrine Dulberg, Bonnie Lind, Thomas Lumley, Ellen O'Meara, Jennifer Nelson, Charles Spiekerman. NHLBI Project Office: Robin Boineau, Teri A. Manolio, Peter J. Savage, Patricia Smith.
Contributor Information
Paula Diehr, Email: pdiehr@u.washington.edu.
Anne B Newman, Email: anewman+@pitt.edu.
Sharon A Jackson, Email: shjackso@wfubmc.edu.
Lewis Kuller, Email: kuller@vms.cis.pitt.edu.
Neil Powe, Email: npowe@jhmi.edu.
References
- Diehr P, Bild D, Harris T, Duxbury A, Siscovick D, Rossi M. Body mass index and mortality in nonsmoking older adults: the cardiovascular health study. American Journal of Public Health. 1998;88:623–629. doi: 10.2105/ajph.88.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornoni-Huntley JC, Harris TB, Everett DF, et al. An overview of body weight of older persons, including the impact on mortality. The National Health and Nutrition Examination Survey I–Epidemiologic Follow-up Study. J Clin Epidemiol. 1991;44:743–753. doi: 10.1016/0895-4356(91)90126-t. [DOI] [PubMed] [Google Scholar]
- Harris T, Cook EF, Garrison R, et al. Body mass index and mortality among nonsmoking older persons: the Framingham study. JAMA. 1988;259:1520–1524. doi: 10.1001/jama.259.10.1520. [DOI] [PubMed] [Google Scholar]
- Losonczy KG, Harris TB, Cornoni-Huntley J, Simonsick EM, Wallace RB, Cook NR, Ostfeld AM, Blazer DG. Does weight loss from middle age to old age explain the inverse weight mortality relation in old age? American Journal of Epidemiology. 1995;141:312–321. doi: 10.1093/aje/141.4.312. [DOI] [PubMed] [Google Scholar]
- Stevens J, Cai J, Pamuk E, Williamson D, Thun M, Wood J. The effect of age on the association between body-mass index and mortality. N Engl J Med. 1998;338:1–7. doi: 10.1056/NEJM199801013380101. [DOI] [PubMed] [Google Scholar]
- Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Health CW. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- Heiat A, Vaccarino V, Krumholz HM. An evidence-based assessment of federal guidelines for overweight and obesity as they apply to elderly persons. Arch Intern Med. 2001;161:1194–1203. doi: 10.1001/archinte.161.9.1194. [DOI] [PubMed] [Google Scholar]
- Andres R, Elahi D, Tobin JD, et al. Impact of age on weight goals. Ann Intern Med. 1985;103:1030–1033. doi: 10.7326/0003-4819-103-6-1030. [DOI] [PubMed] [Google Scholar]
- Van Itallie TB, Lew EA. Health implications of overweight in the elderly. Progress in clinical and biological research. 1990;326:89–108. [PubMed] [Google Scholar]
- Diehr P, Patrick DL, Burke GL, Williamson J. Survival versus years of healthy life: which is more powerful as a study outcome?. Control Clin Trials. 1997;20:267–279. doi: 10.1016/S0197-2456(98)00062-2. [DOI] [PubMed] [Google Scholar]
- Fried LP, Borhani NO, Enright PL, et al. The Cardiovascular Health Study: design and rationale. Annals of Epidemiology. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- Ives G, Fitzpatrick A, Bild D, et al. Surveillance and ascertainment of cardiovascular events: the cardiovascular health study. Annals of Epidemiology. 1995;5:278–285. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- Clinical Guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute. 1998.
- Kate S, Branch LG, Branson MH, Papsidero JA, Beck JC, Greer DS. Active life expectancy. N Engl J Med. 1983;309:1218–1224. doi: 10.1056/NEJM198311173092005. [DOI] [PubMed] [Google Scholar]
- Krause NM, Jay GM. What do global self-rated health items measure? Med Care. 1994;32:930–942. doi: 10.1097/00005650-199409000-00004. [DOI] [PubMed] [Google Scholar]
- Gold M, Siegel J, Weinstein M, Russell L, eds. Cost effectiveness in health and medicine. New York: Oxford University Press. 1996.
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- Mundahl JM. Imputation of missing longitudinal data: a comparison of methods. Master's thesis University of Washington, Department of Biostatistics. 1998.
- Diehr P, Patrick DL, Spertus J, Kiefe C, McDonell M, Fihn SD. Transforming self-rated health and the SF-36 scales to include death and improve interpretability. Medical Care. 2001;39:670–680. doi: 10.1097/00005650-200107000-00004. [DOI] [PubMed] [Google Scholar]
- Diehr P, Patrick D, Bild D, Burke G, Williamson J. Predicting future years of healthy life for older adults. J Clin Epidemiol. 1998;51:343–353. doi: 10.1016/S0895-4356(97)00298-9. [DOI] [PubMed] [Google Scholar]
- Psaty BM, Kuller LH, Bild D, et al. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–277. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- O'Leary DH, Polak JF, Wolfson Jr SK, et al. The use of sonography to evaluate carotid atherosclerosis in the elderly: The Cardiovascular Health Study. Stroke. 1991;22:1155–1163. doi: 10.1161/01.str.22.9.1155. [DOI] [PubMed] [Google Scholar]
- Radoff LL. The CESD Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Cushman M, Cornell ES, Howard PR, et al. Laboratory methods and quality assurance in the Cardiovascular Health Study. Clinical Chemistry. 1995;41:264–270. [PubMed] [Google Scholar]
- Guralnik JM, Land KC, Blazer D, Fillenbaum G, Branch LG. Educational status and active life expectancy among older blacks and whites. N Engl J Med. 1993;329:110–116. doi: 10.1056/NEJM199307083290208. [DOI] [PubMed] [Google Scholar]
- Folsom AR, Kaye SA, Sellers TA, et al. Body fat distribution and 5-year risk of death in older women. JAMA. 1993;269:483–487. doi: 10.1001/jama.269.4.483. [DOI] [PubMed] [Google Scholar]
- Katz DA, McHorney CA, Atkinson RL. Impact of obesity on health-related quality of life in patients with chronic illness. Journal of General Internal Medicine. 2000;15:789–796. doi: 10.1046/j.1525-1497.2000.90906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein MM. Body mass index and quality of life in a survey of primary care patients. Journal of Family Practice. 2000;49:734–737. [PubMed] [Google Scholar]
- Kolotkin RL, Head S, Hamilton M, Tse CK. Assessing Impact of weight on quality of life. Obes Res. 1995;3:49–56. doi: 10.1002/j.1550-8528.1995.tb00120.x. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalence of overweight among US adults: the National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 1994;272:205–211. doi: 10.1001/jama.272.3.205. [DOI] [PubMed] [Google Scholar]
- Allison DB, Gallagher D, Heo M, Pi-Sunyer FX, Heymsfield SB. Body mass index and all-cause mortality among people age 70 and over: the longitudinal study of aging. International Journal of Obesity. 1997;21:424–431. doi: 10.1038/sj/ijo/0800423. [DOI] [PubMed] [Google Scholar]
- Olshansky SJ, Carnes BA, Desesquelles A. Prospects for human longevity. Science. 2001;291:1491–1492. doi: 10.1126/science.291.5508.1491. [DOI] [PubMed] [Google Scholar]
- Mark EJ, Patalas ED, Chang HT, et al. Fatal pulmonary hypertension associated with short-term use of fenfluramine and phentermine. N Engl J Med. 1997;337:602–606. doi: 10.1056/NEJM199708283370904. [DOI] [PubMed] [Google Scholar]
- Connolly HM, Crary JL, McGoon MD, et al. Valvular heart disease associated with fenfluramine-phentermine. N Engl J Med. 1997;337:581–588. doi: 10.1056/NEJM199708283370901. [DOI] [PubMed] [Google Scholar]