Abstract
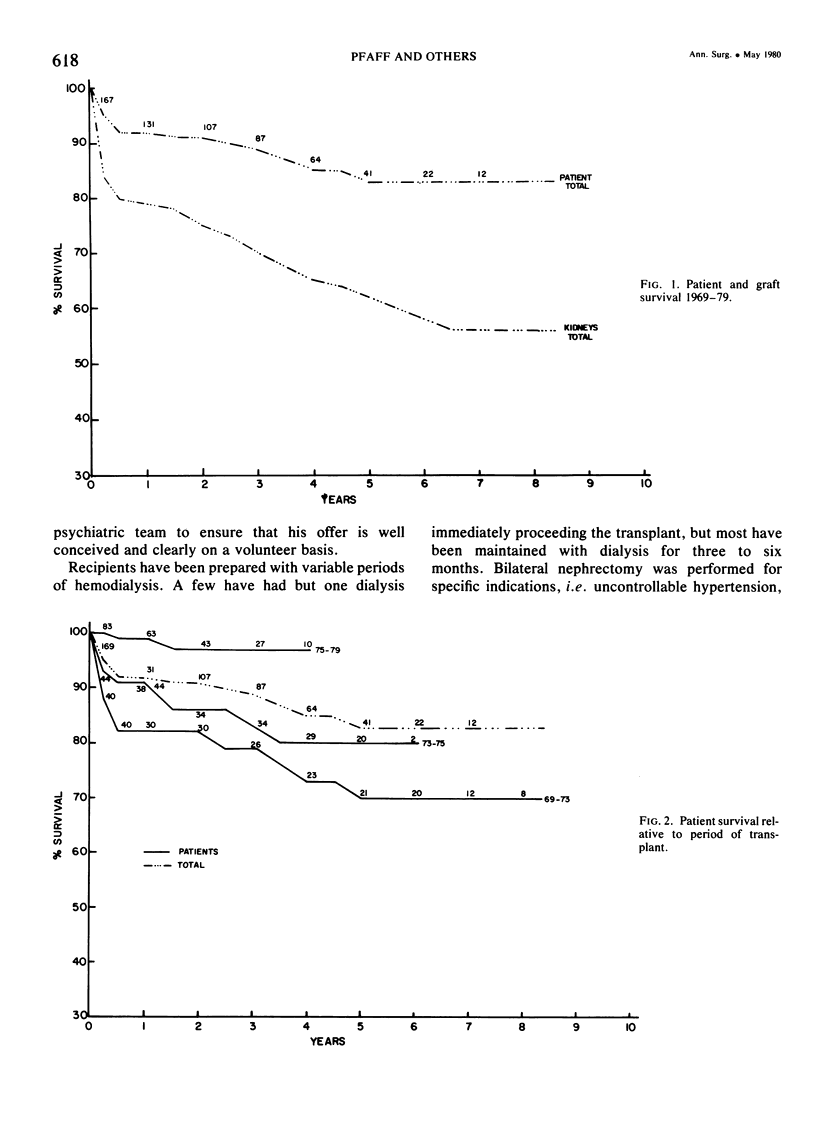
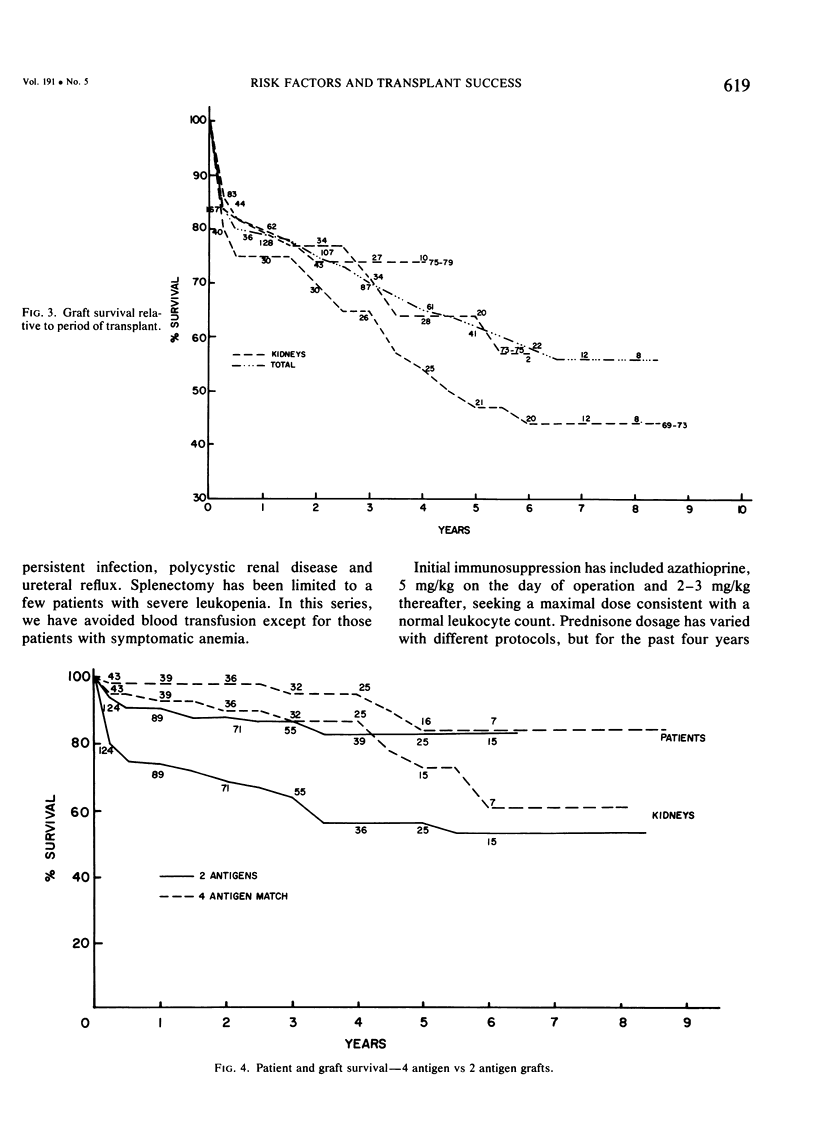
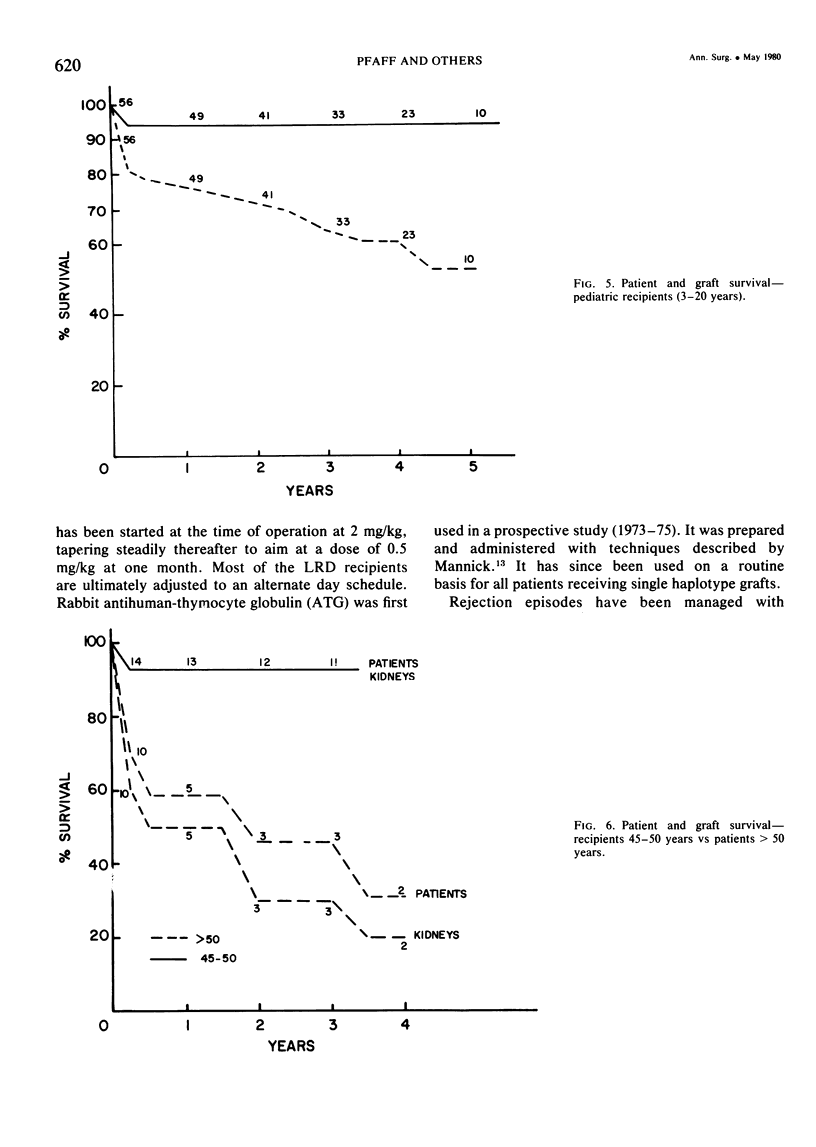
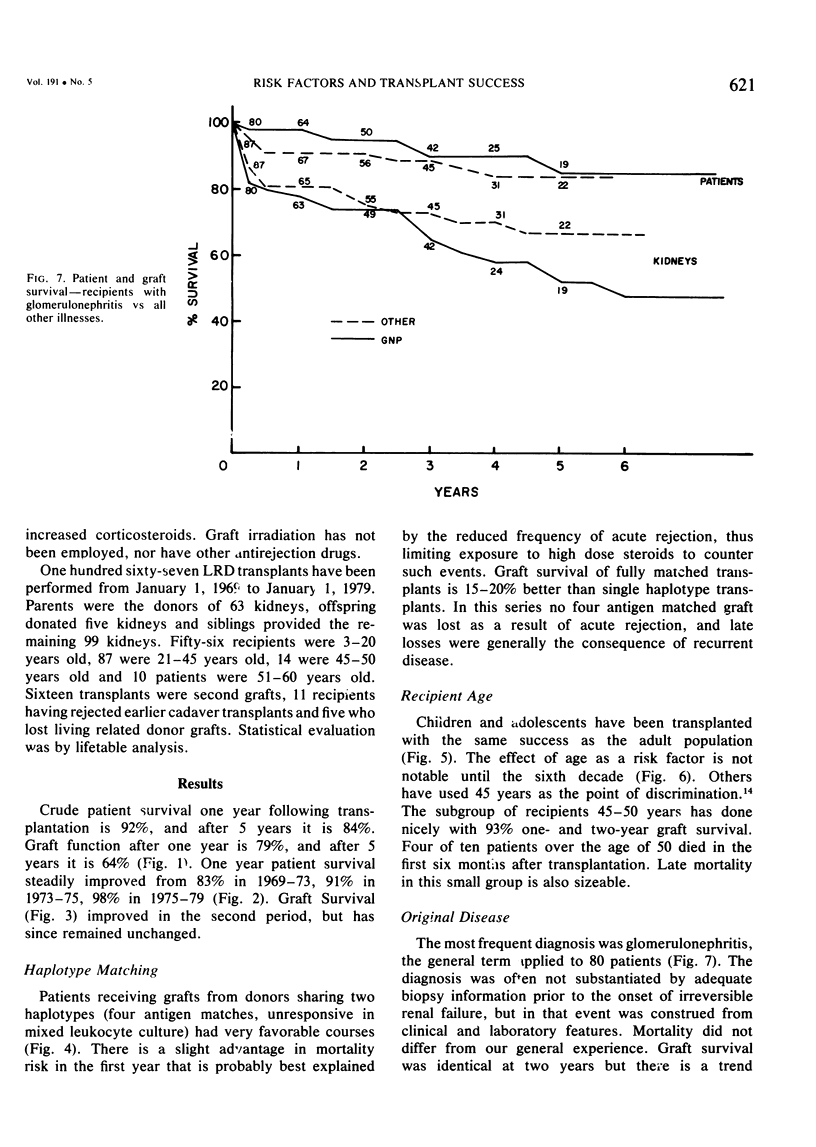
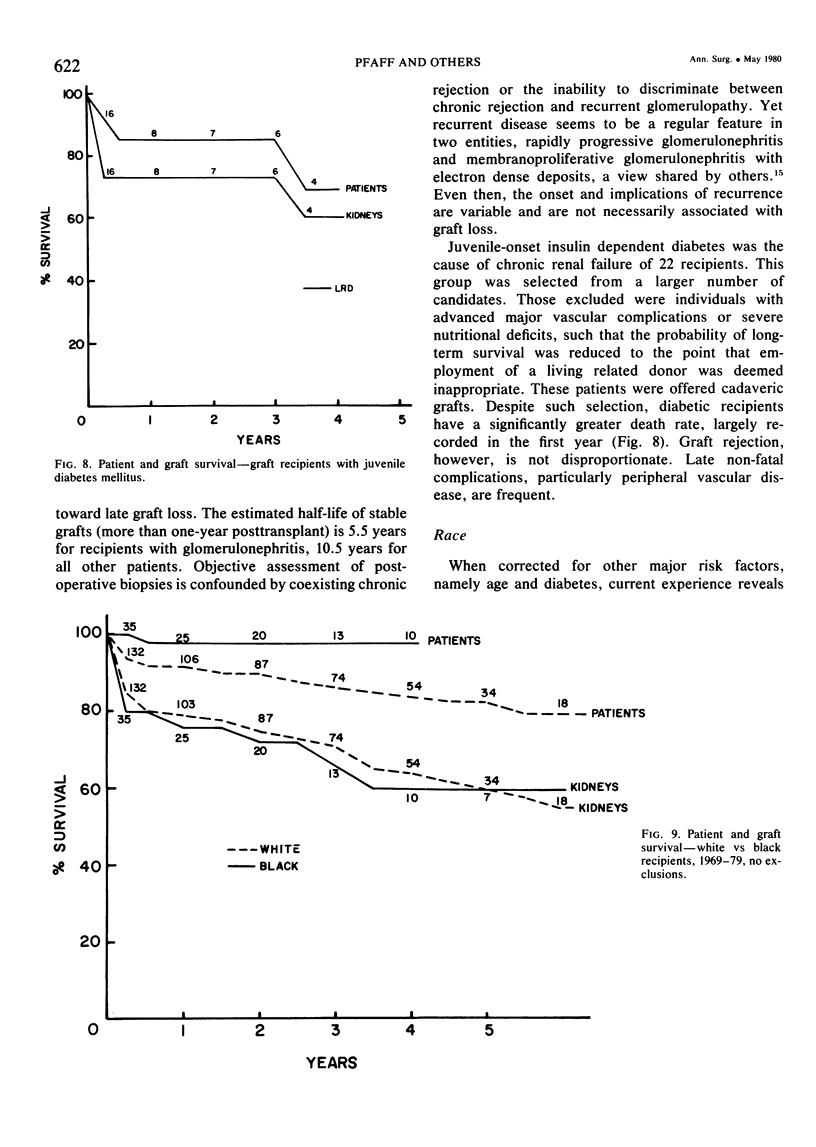
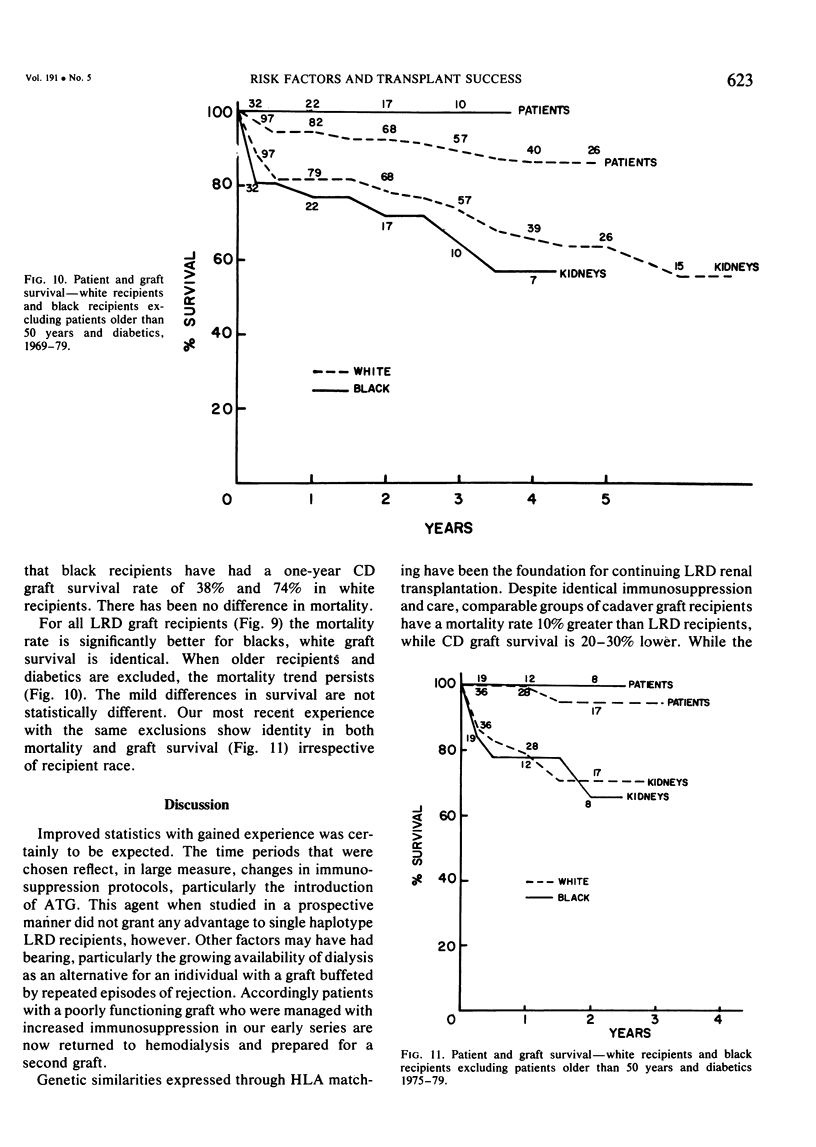
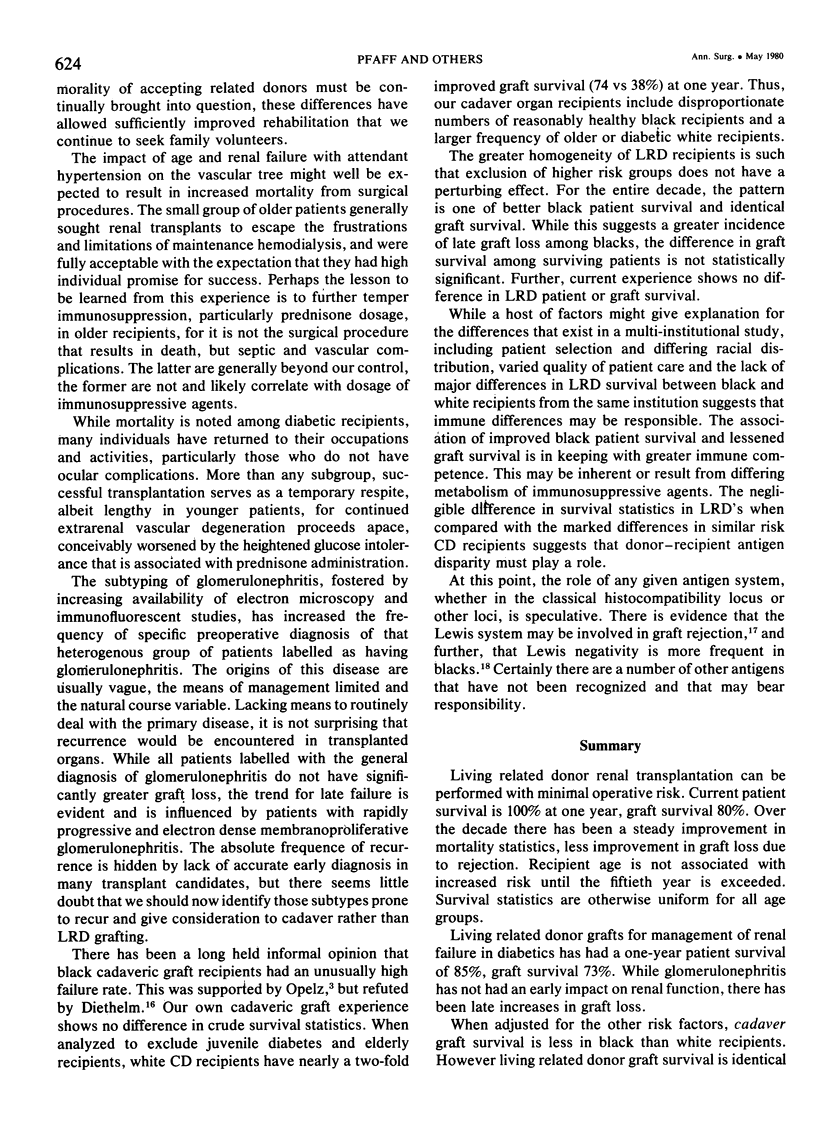
Assessment of living related donor (LRD) survival statistics offers the opportunity to gauge the effects of recipient characteristics without the perturbations of viability, function, and antigen sharing that are inherent in cadaveric organ grafting. From January 1, 1969 to January 1, 1979, 167 LRD grafts were performed. Crude patient survival at one year is 92% and 84% at five years. Graft function at one year is 79%, and at five years it is 64%. One year patient survival has steadily improved: 1969-73: 83%, 1973-75: 91%, 1975-79: 98%. Graft survival improved during the first two periods and has since remained unchanged. HLA identical grafts showed the expected advantage compared with single haplotype grafts (93 vs 74%). Recipient age was without effect until 50 years, all younger subgroups having one-year patient survival of 92-95%, while those older than 50 had a one-year survival of 60%. Juvenile diabetes was associated with a one-year patient survival of 85% and graft survival of 74%. Glomerulonephritis did not affect early graft survival statistics, but there was a greater frequency of graft loss after 2.5 years, with function at five years of 51 versus 68% for recipients with all other diagnoses. Cadaveric graft statistics vary with recipient race when adjusted to exclude older patients and diabetics, white recipient one-year graft survival 74%, black 38%. No meaningful difference exists among LRD recipients as to graft function, but there is a trend toward improved black patient survival. This suggests that there is not an inherent difference in immune response to genetically similar grafts, but that the disparate results with racially mixed donor-recipient combinations rests with other factors.
Full text
PDF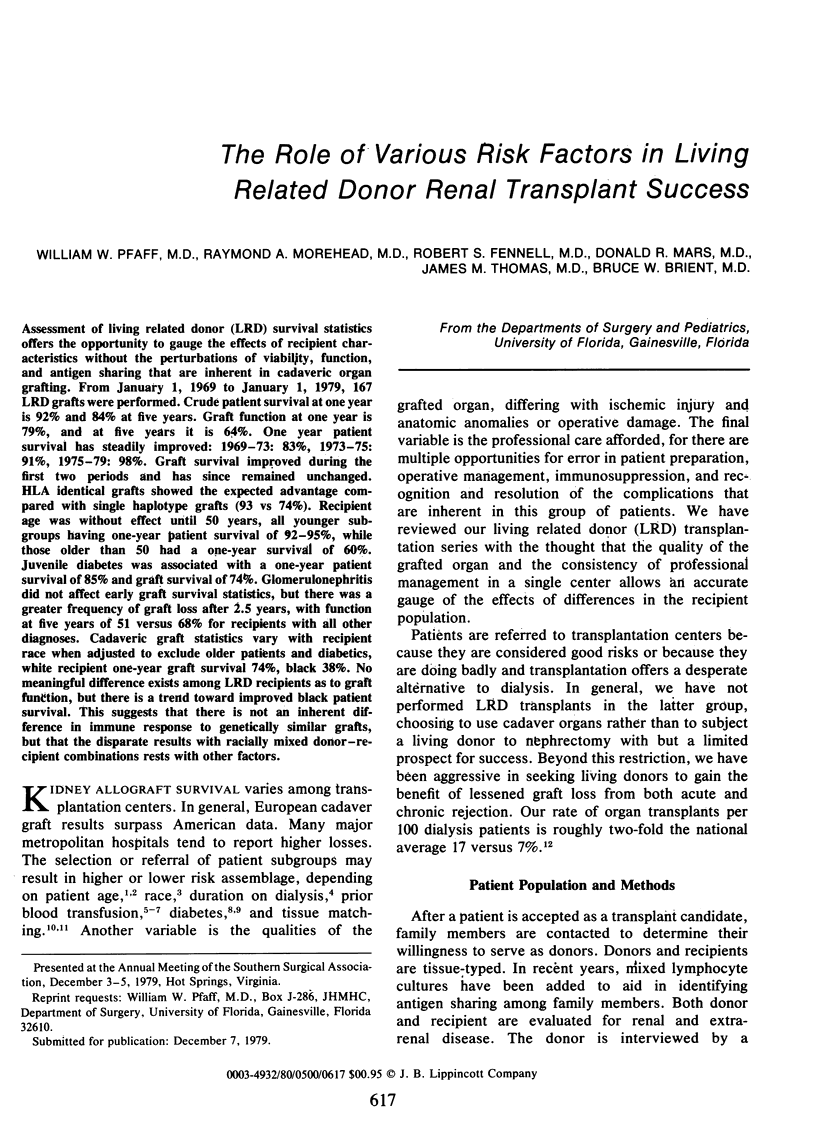
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Belzer F. O., Perkins H. A., Fortmann J. L., Kountz S. L., Salvatierra O., Cochrum K. C., Payne R. Is HL-A typing of clinical significance in cadaver renal transplantation? Lancet. 1974 Apr 27;1(7861):774–777. doi: 10.1016/s0140-6736(74)92842-6. [DOI] [PubMed] [Google Scholar]
- Byrnger H., Sandberg L., Ahlmén J., Bitter-Suermann H., Blohmé I., Lindholm A., Gelin L. E. Effect of HLA compatibility on primary kidney grafts from living related and cadaveric donors. Transplant Proc. 1977 Mar;9(1):479–482. [PubMed] [Google Scholar]
- Cameron J. S., Turner D. R. Recurrent glomerulonephritis in allografted kidneys. Clin Nephrol. 1977 Feb;7(2):47–54. [PubMed] [Google Scholar]
- Delmonico F. L., Cosimi A. B., Russell P. S. Renal transplantation in the older age group. Arch Surg. 1975 Sep;110(9):1107–1109. doi: 10.1001/archsurg.1975.01360150051009. [DOI] [PubMed] [Google Scholar]
- Fehrman I., Groth C. G., Lundgren G., Magnusson G., Möller E. Pretransplant dialysis and blood transfusion--correlation with cadaveric kidney graft survival. Transplant Proc. 1979 Mar;11(1):152–155. [PubMed] [Google Scholar]
- Festenstein H., Sachs J. A., Pegrum G. D., Moorhead J. F., Paris A. M. Influence of HLA matching and blood-transfusion on outcome of 502 London Transplant Group renal-graft recipients. Lancet. 1976 Jan 24;1(7952):157–161. doi: 10.1016/s0140-6736(76)91270-8. [DOI] [PubMed] [Google Scholar]
- Kjellstrand C. M., Simmons R. L., Goetz F. C., Buselmeier T. J., Shideman J. R., Von Hartitzsch B., Najarian J. S. Renal transplantation in patients with insulin-dependent diabetes. Lancet. 1973 Jul 7;2(7819):4–8. doi: 10.1016/s0140-6736(73)91944-2. [DOI] [PubMed] [Google Scholar]
- Opelz G., Mickey M. R., Terasaki P. I. Influence of race on kidney transplant survival. Transplant Proc. 1977 Mar;9(1):137–142. [PubMed] [Google Scholar]
- Opelz G., Sengar D. P., Mickey M. R., Terasaki P. I. Effect of blood transfusions on subsequent kidney transplants. Transplant Proc. 1973 Mar;5(1):253–259. [PubMed] [Google Scholar]
- Oriol R., Cartron J., Yvart J., Bedrossian J., Duboust A., Bariety J., Gluckman J. C., Gagnadoux M. F. The Lewis system: New histocompatibility antigens in renal transplantation. Lancet. 1978 Mar 18;1(8064):574–575. doi: 10.1016/s0140-6736(78)91024-3. [DOI] [PubMed] [Google Scholar]
- Persijn G. G., Cohen B., Lansbergen Q., van Rood J. J. Retrospective and prospective studies on the effect of blood transfusions in renal transplantation in The Netherlands. Transplantation. 1979 Nov;28(5):396–401. doi: 10.1097/00007890-197911000-00010. [DOI] [PubMed] [Google Scholar]
- Renal transplantation in insulin-dependent diabetics. A joint Scandinavian report. Lancet. 1978 Oct 28;2(8096):915–917. [PubMed] [Google Scholar]
- Simmons R. L., Kjellstrand C. M., Buselmeier T. J., Najarian J. S. Renal transplantation in high-risk patients. Arch Surg. 1971 Aug;103(2):290–298. doi: 10.1001/archsurg.1971.01350080206032. [DOI] [PubMed] [Google Scholar]


