Abstract
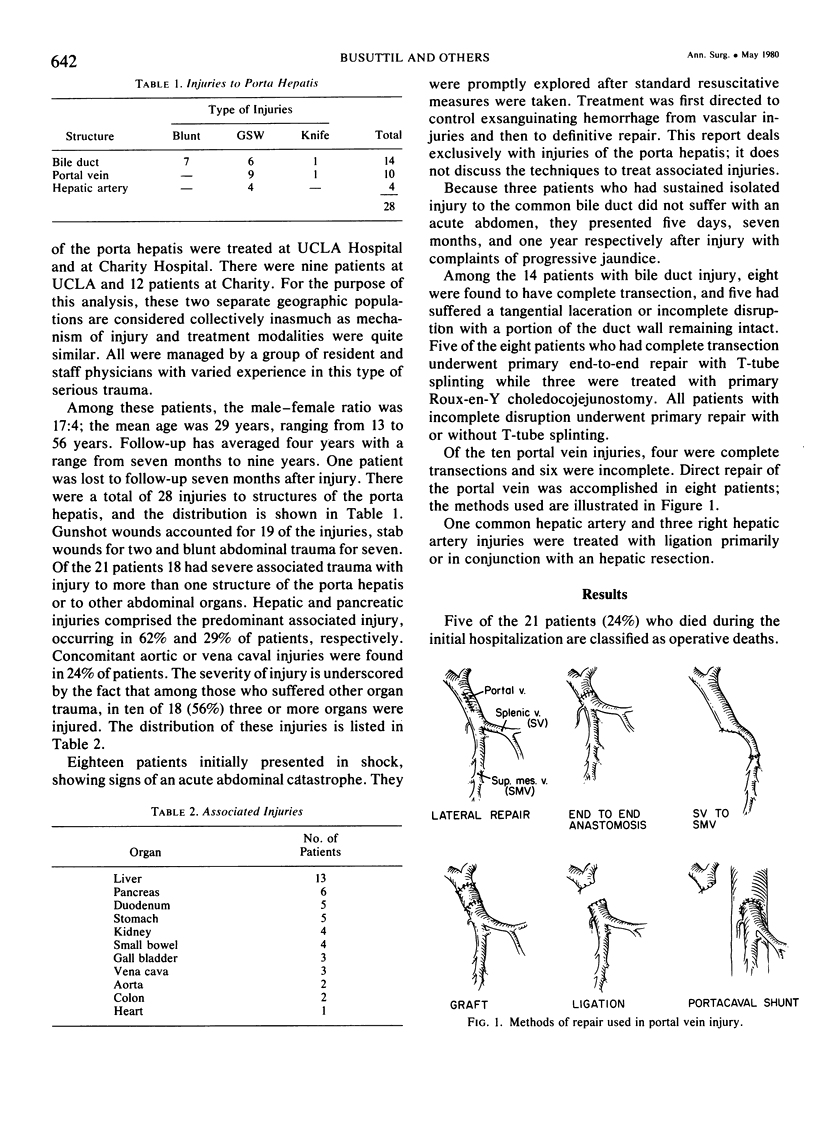
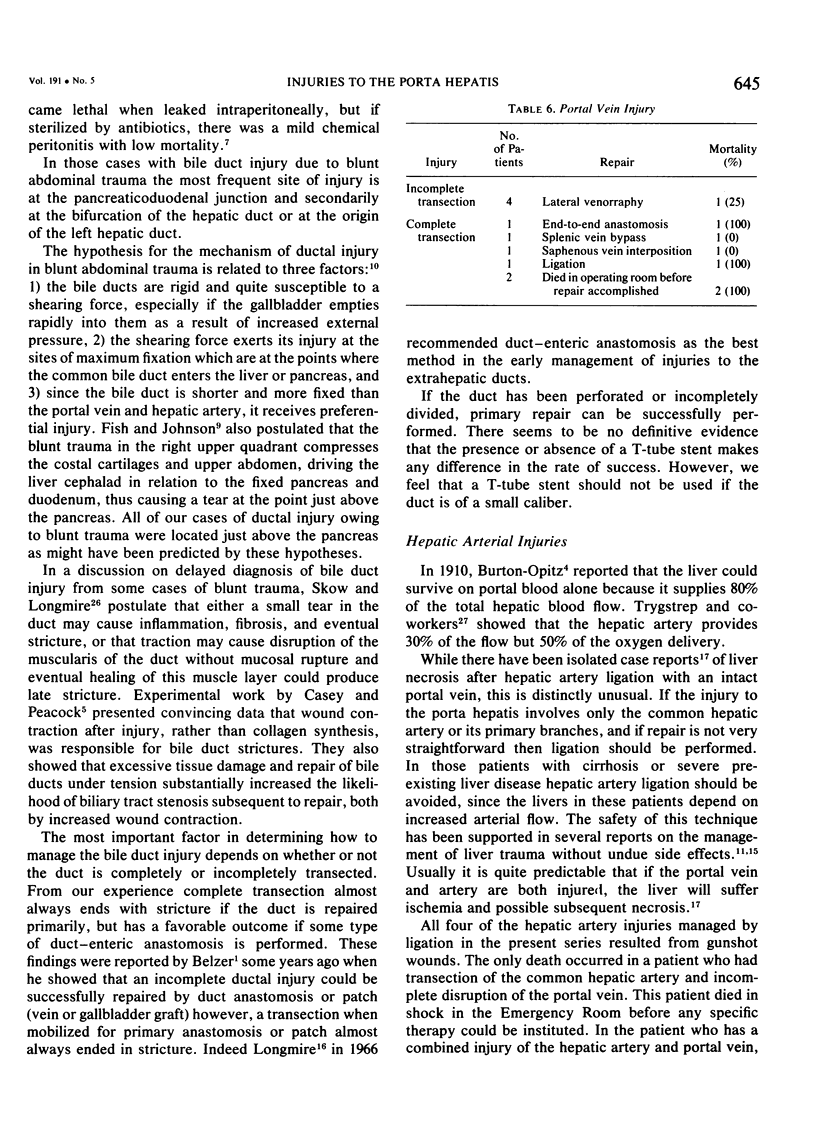
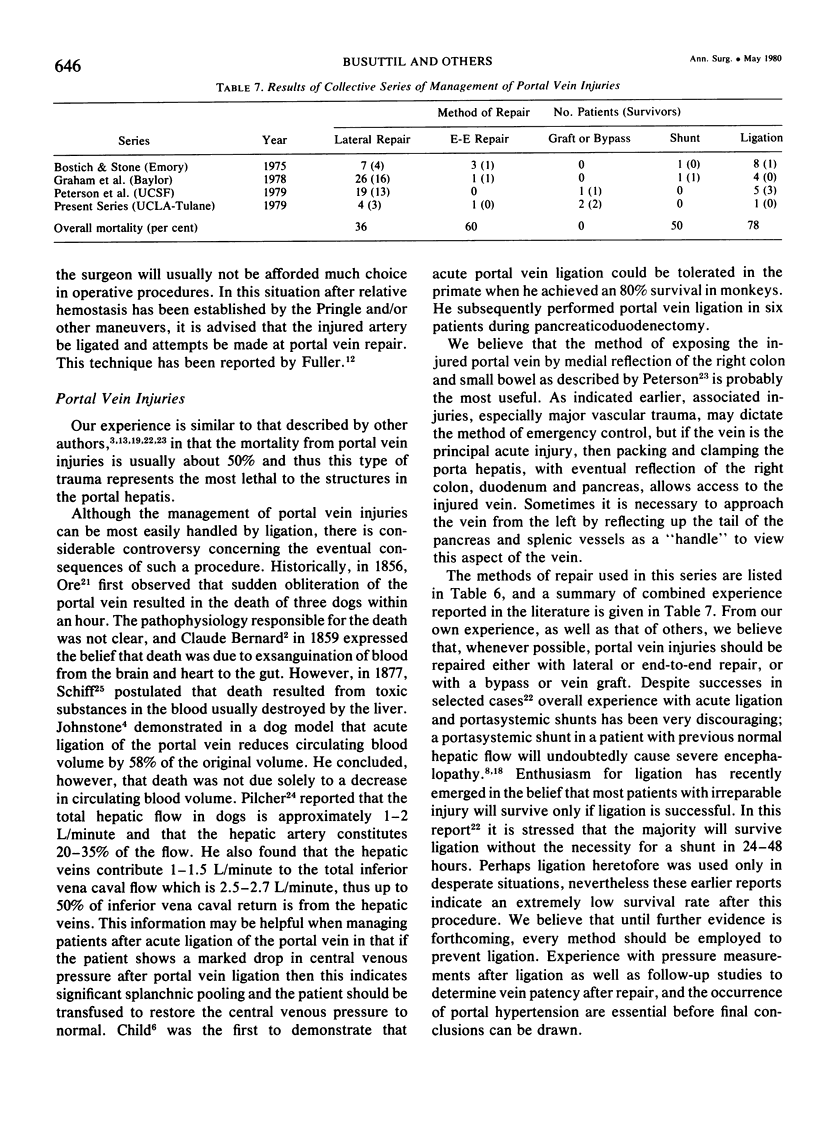
Injuries to the porta hepatis pose difficult problems in management, and transection of the bile ducts, portal vein and hepatic artery is among the most challenging. Twenty-one patients with severe injuries to the porta hepatis were treated over a ten-year period. Ages ranged from 13 to 56 years, and follow-up was up to nine years. Among the 14 patients with bile duct injury, eight were found to have complete transection, and five suffered a tangential laceration or incomplete disruption with a portion of a duct wall remaining intact. Five of the eight patients who had complete transection underwent primary end-to-end repair with T-tube splinting, while three were treated with primary Roux-en-Y choledocojejunostomy. All patients with incomplete disruption underwent primary repair with or without T-tube splinting. Of the five patients with complete disruption who were treated with primary end-to-end anastomosis of the bile duct in conjunction with T-tube splinting, all required secondary biliary tract reconstruction of some type. No patient with complete transection that was treated with primary Roux-en-Y biliary enteric anastomosis required reoperation. Partial transections were successfully treated with primary repair. Portal vein injury was encountered in ten patients. Injury was successfully managed by primary closure, interposition of a vein, or splenicmesenteric vein bypass. Associated injuries to liver, pancreas, kidney and duodenum were common. In four patients there was injury to the main or left or right hepatic artery which was managed successfully by repair or ligation, with or without hepatic lobectomy. By adhering to the principles of management to be outlined, many patients with injury to the porta hepatis will survive, and the long term outcome can be gratifying.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Belzer F. O., Watts J. M., Ross H. B., Dunphy J. E. Auto-reconstruction of the common bile duct after venous patch graft. Ann Surg. 1965 Sep;162(3):346–355. doi: 10.1097/00000658-196509000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick J., 3rd, Stone H. H. Trauma to the portal venous system. South Med J. 1975 Nov;68(11):1369–1372. doi: 10.1097/00007611-197511000-00011. [DOI] [PubMed] [Google Scholar]
- COHN I., Jr, COTLAR A. M., ATIK M., LUMPKIN W. M., HUDSON T. L., WERNETTE G. J. Bile peritonitis. Ann Surg. 1960 Nov;152:827–835. doi: 10.1097/00000658-196011000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey W. J., Peacock E. E., Jr Some factors affecting pathophysiology of bile duct stenosis. Surg Forum. 1977;28:414–416. [PubMed] [Google Scholar]
- Fish J. C., Johnson G. L. Rupture of Duodenum following Blunt Trauma: Report of a Case with Avulsion of Papilla of Vater. Ann Surg. 1965 Nov;162(5):917–919. doi: 10.1097/00000658-196511000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish J. C. Reconstruction of the portal vein. Case reports and literature review. Am Surg. 1966 Jul;32(7):472–478. [PubMed] [Google Scholar]
- Fletcher W. S. Nonpenetrating trauma to the gallbladder and extrahepatic bile ducts. Surg Clin North Am. 1972 Jun;52(3):711–717. doi: 10.1016/s0039-6109(16)39743-2. [DOI] [PubMed] [Google Scholar]
- Flint L. M., Mays E. T., Aaron W. S., Fulton R. L., Polk H. C. Selectivity in the management of hepatic trauma. Ann Surg. 1977 Jun;185(6):613–618. doi: 10.1097/00000658-197706000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller J. W., Anderson P. H. Operative management of combined injuries to the portal vein and hepatic artery. South Med J. 1978 Apr;71(4):423–424. doi: 10.1097/00007611-197804000-00023. [DOI] [PubMed] [Google Scholar]
- Graham J. M., Mattox K. L., Beall A. C., Jr Portal venous system injuries. J Trauma. 1978 Jun;18(6):419–422. doi: 10.1097/00005373-197806000-00006. [DOI] [PubMed] [Google Scholar]
- Graham J. M., Mattox K. L., Beall A. C., Jr Portal venous system injuries. J Trauma. 1978 Jun;18(6):419–422. doi: 10.1097/00005373-197806000-00006. [DOI] [PubMed] [Google Scholar]
- JOHNSTONE F. R. Acute ligation of the portal vein. Surgery. 1957 Jun;41(6):958–971. [PubMed] [Google Scholar]
- Lewis F. R., Lim R. C., Jr, Blaisdell F. W. Hepatic artery ligation: adjunct in the management of massive hemorrhage from the liver. J Trauma. 1974 Sep;14(9):743–755. [PubMed] [Google Scholar]
- Longmire W. P., Jr Early management of injury to the extrahepatic biliary tract. JAMA. 1966 Feb 21;195(8):623–625. [PubMed] [Google Scholar]
- Lucas C. E., Ledgerwood A. M. Liver necrosis following hepatic artery transection due to trauma. Arch Surg. 1978 Sep;113(9):1107–1107. doi: 10.1001/archsurg.1978.01370210089014. [DOI] [PubMed] [Google Scholar]
- Mattox K. L., Espada R., Beall A. R., Jr Traumatic injury to the portal vein. Ann Surg. 1975 May;181(5):519–522. doi: 10.1097/00000658-197505000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachter H. L., Drager S., Godfrey N., LeFleur R. Traumatic injuries of the portal vein. The role of acute ligation. Ann Surg. 1979 Apr;189(4):383–385. [PMC free article] [PubMed] [Google Scholar]
- Petersen S. R., Sheldon G. F., Lim R. C., Jr Management of portal vein injuries. J Trauma. 1979 Aug;19(8):616–620. doi: 10.1097/00005373-197908000-00009. [DOI] [PubMed] [Google Scholar]
- Skow J. R., Longmire W. P., Jr Common duct stricture secondary to blunt abdominal trauma. Am Surg. 1974 Oct;40(10):576–578. [PubMed] [Google Scholar]
- TYGSTRUP N., WINKLER K., MELLEMGAARD K., ANDREASSEN M. Determination of the hepatic arterial blood flow and oxygen supply in man by clamping the hepatic artery during surgery. J Clin Invest. 1962 Mar;41:447–454. doi: 10.1172/JCI104497. [DOI] [PMC free article] [PubMed] [Google Scholar]