Abstract
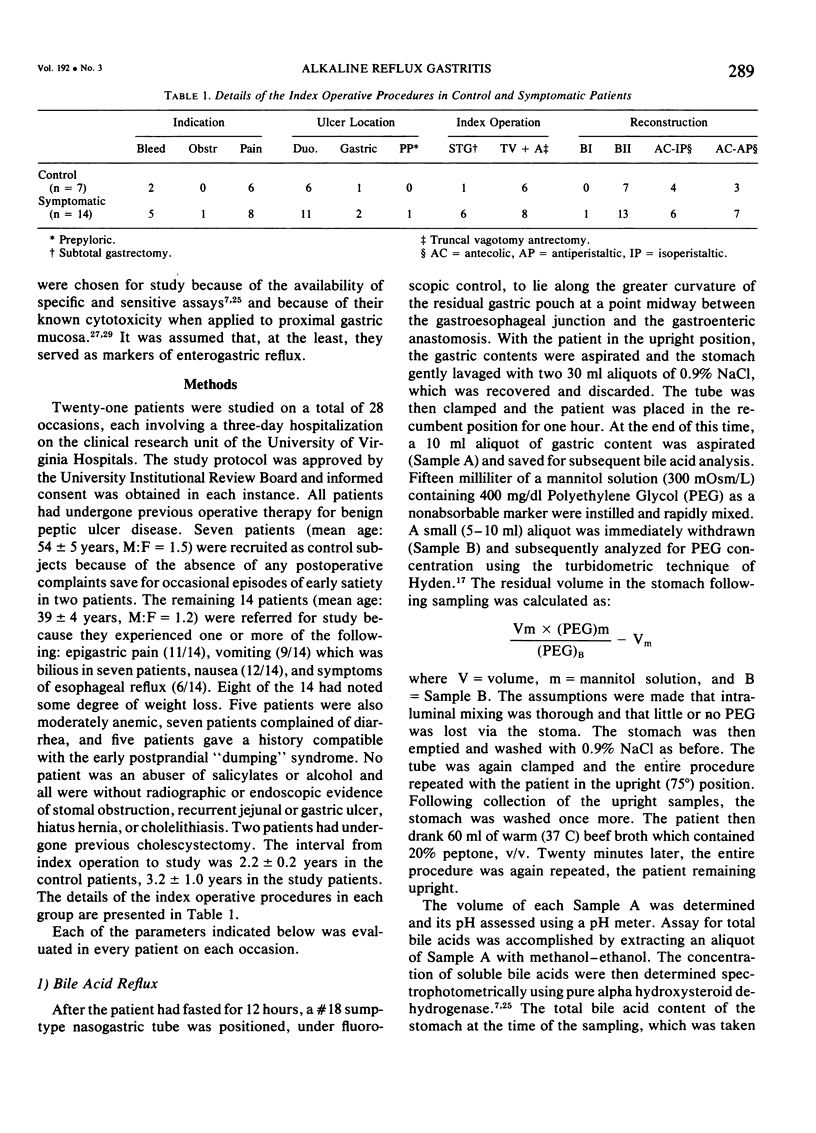
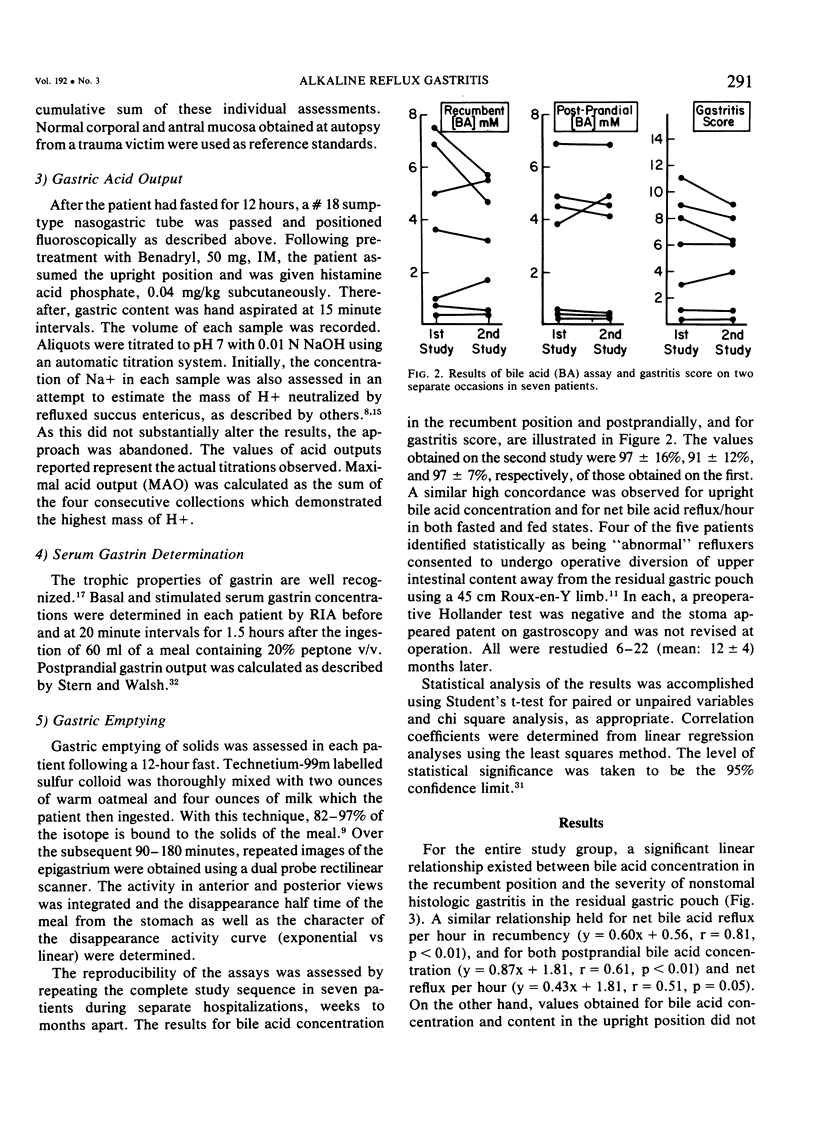
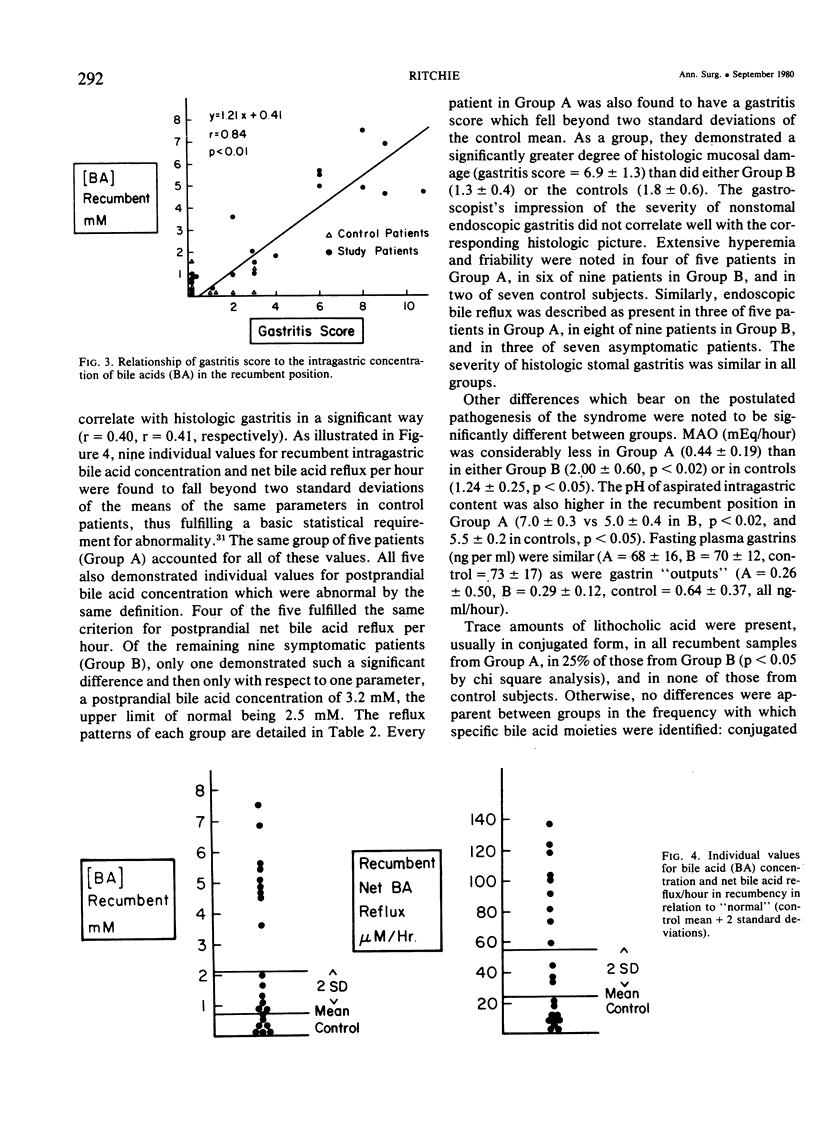
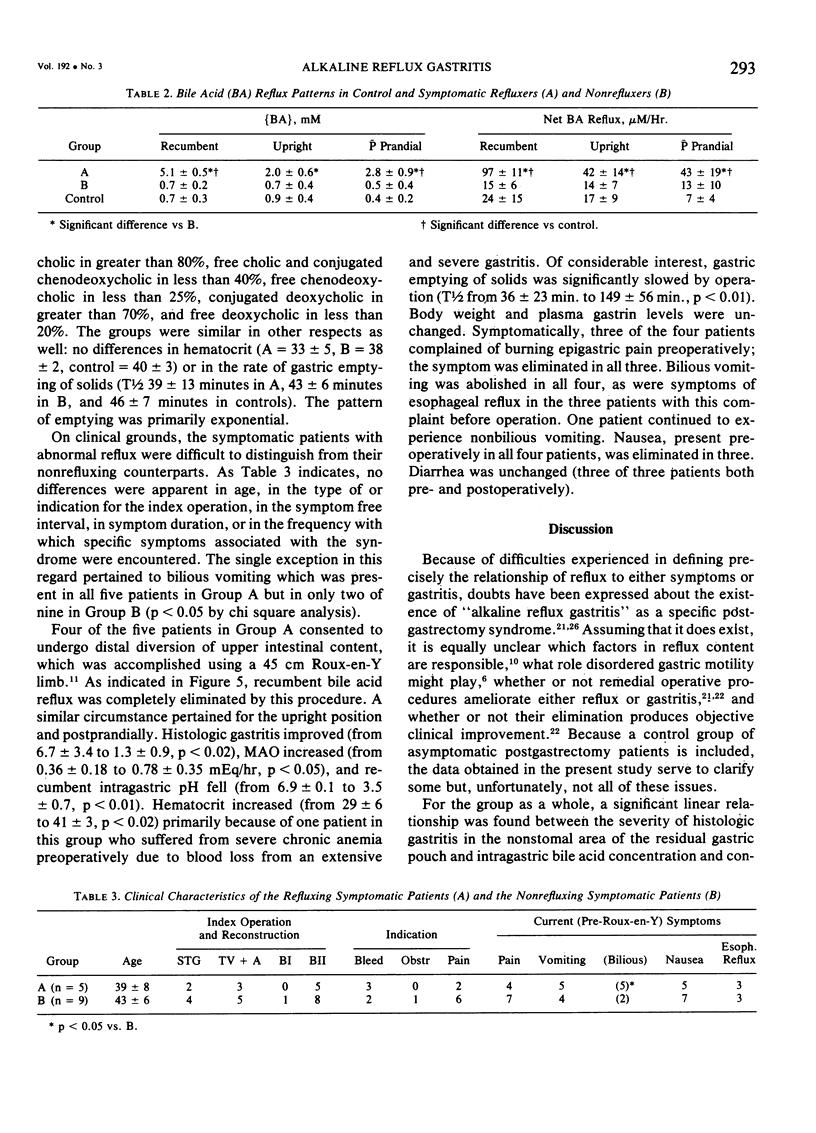
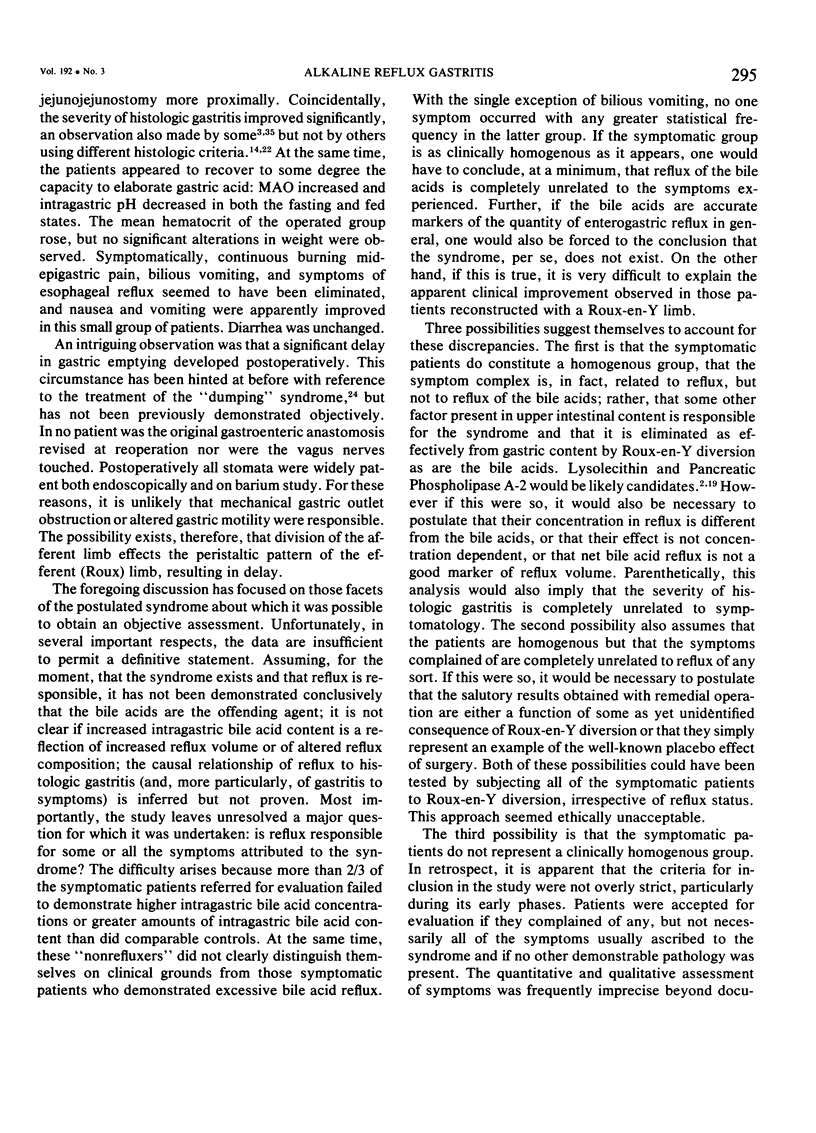
The hypothesis that reflux of upper intestinal content, particularly of bile acids (BA), is responsible for a unique postgastrectomy syndrome, alkaline reflux gastritis, was tested on 28 occasions in 21 postoperative patients (14 symptomatic patients, 7 controls). Parameters evaluated: recumbent (rec.), upright, p.c. intragastric pH, {BA}, net BA reflux per hour, specific BA fractions, fasting and p.c. gastrin, maximal acid output (MAO), gastric emptying of solids by δ-scintigraphy), and the severity of nonstomal histologic gastritis, the “gastritis score,” graded 0-15 by an independent senior pathologist. For the entire group, gastritis severity correlated positively with intragastric {BA} and net BA reflux per hour, both in recumbency and p.c. Five symptomatic patients demonstrated rec. and p.c. {BA} and net BA reflux per hour greater than two standard deviations from comparable mean values in control patients. They differed significantly from the remaining symptomatic patients as follows: increased intragastric {BA} and net BA reflux per hour, increased intragastric pH and decreased MAO. They also demonstrated a more severe grade of gastritis. Lithocholic acid was present in their reflux content significantly more often. Bilious vomiting was also more frequent. No other differences could be identified, either objectively or clinically, between the symptomatic groups. Four patients with excessive reflux underwent Roux-en-Y revision and restudy 6-22 months later. BA reflux was completely abolished, histologic gastritis improved, hematocrit rose, MAO increased, and gastric emptying slowed. Burning pain, bilious vomiting, and symptoms of esophageal reflux were eliminated. Vomiting and nausea were improved. Diarrhea was unchanged. The objective criteria outlined can identify symptomatic postgastrectomy patients with a greater than normal reflux and gastritis. Clinical criteria alone cannot. Revisional surgery in these patients eliminates reflux, improves gastritis, and produces symptomatic improvement. The hypothesis under consideration is strengthened but not proven.
Full text
PDF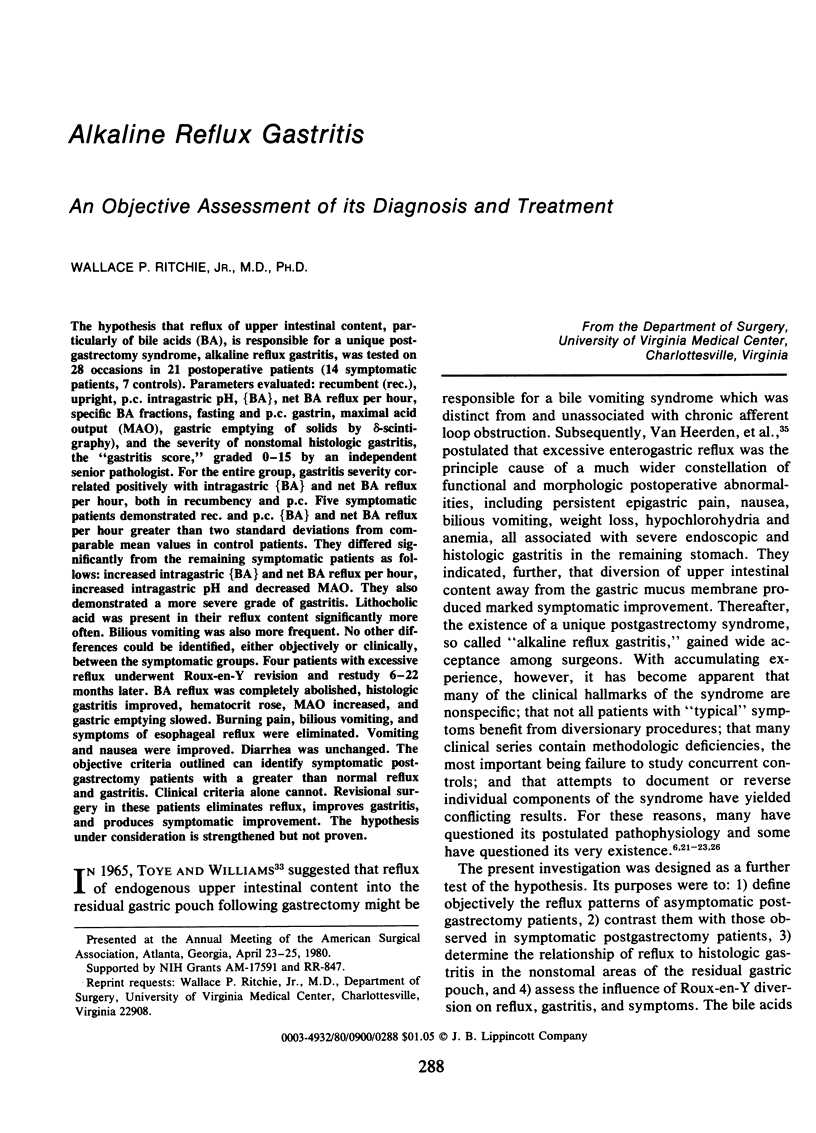

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berardi R. S., Siroospour D., Ruiz R., Carnes W., Devaiah K. A., Peterson C., Becknell W. E., Jr, Olivencia J. Alkaline reflux gastritis. A study in forty postoperative duodenal ulcer patients. Am J Surg. 1976 Nov;132(5):552–557. doi: 10.1016/0002-9610(76)90339-1. [DOI] [PubMed] [Google Scholar]
- Bushkin F. L., Wickbom G., DeFord J. W., Woodward E. R. Postoperative alkaline reflux gastritis. Surg Gynecol Obstet. 1974 Jun;138(6):933–939. [PubMed] [Google Scholar]
- Davidson E. D., Hersh T. Bile reflux gastritis. Contribution of inadequate gastric emptying. Am J Surg. 1975 Nov;130(5):514–518. doi: 10.1016/0002-9610(75)90502-4. [DOI] [PubMed] [Google Scholar]
- Delaney J. P., Broadie T. A., Robbins P. L. Pyloric reflux gastritis: the offending agent. Surgery. 1975 Jun;77(6):764–772. [PubMed] [Google Scholar]
- Fausa O., Skålhegg B. A. Quantitative determination of bile acids and their conjugates using thin-layer chromatography and a purified 3alpha-hydroxysteroid dehydrogenase. Scand J Gastroenterol. 1974;9(3):249–254. [PubMed] [Google Scholar]
- Fiddian-Green R., Hobsley M. Proceedings: Defective bicarbonate secretion in response to duodenal acid loads. Br J Surg. 1974 Apr;61(4):330–331. [PubMed] [Google Scholar]
- Fitzpatrick M. L., Alderson A. M. Solid food label for measurement of gastric emptying. Br J Radiol. 1979 Nov;52(623):920–920. doi: 10.1259/0007-1285-52-623-920-a. [DOI] [PubMed] [Google Scholar]
- Gadacz T. R., Zuidema G. D. Bile acid composition in patients with and without symptoms of postoperative refulx gastritis. Am J Surg. 1978 Jan;135(1):48–52. doi: 10.1016/0002-9610(78)90008-9. [DOI] [PubMed] [Google Scholar]
- Herrington J. L., Jr, Sawyers J. L., Whitehead W. A. Surgical management of reflux gastritis. Ann Surg. 1974 Oct;180(4):526–537. doi: 10.1097/00000658-197410000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoare A. M., Jones E. L., Alexander-Williams J., Hawkins C. F. Symptomatic significance of gastric mucosal changes after surgery for peptic ulcer. Gut. 1977 Apr;18(4):295–300. doi: 10.1136/gut.18.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoare A. M., Keighley M. R., Starkey B., Alexander-Williams J. Measurement of bile acids in fasting gastric aspirates: an objective test for bile reflux after gastric surgery. Gut. 1978 Mar;19(3):166–169. doi: 10.1136/gut.19.3.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoare A. M., McLeish A., Thompson H., Alexander-Williams J. Selection of patients for bile diversion surgery: use of bile acid measurement in fasting gastric aspirates. Gut. 1978 Mar;19(3):163–165. doi: 10.1136/gut.19.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobsley M. Pyloric reflux: a modification of the two-component hypothesis of gastric secretion. Clin Sci Mol Med. 1974 Aug;47(2):131–141. doi: 10.1042/cs0470131. [DOI] [PubMed] [Google Scholar]
- Hofmann A. F., Small D. M. Detergent properties of bile salts: correlation with physiological function. Annu Rev Med. 1967;18:333–376. doi: 10.1146/annurev.me.18.020167.002001. [DOI] [PubMed] [Google Scholar]
- Johnson L. R. The trophic action of gastrointestinal hormones. Gastroenterology. 1976 Feb;70(2):278–288. [PubMed] [Google Scholar]
- Keighley M. R., Asquith P., Alexander-Williams J. Duodenogastric reflux: a cause of gastric mucosal hyperaemia and symptoms after operations for peptic ulceration. Gut. 1975 Jan;16(1):28–32. doi: 10.1136/gut.16.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivilaakso E., Fromm D., Silen W. Effects of lysolecithin on isolated gastric mucosa. Surgery. 1978 Nov;84(5):616–621. [PubMed] [Google Scholar]
- Meshkinpour H., Elashoff J., Stewart H., 3rd, Sturdevant R. A. Effect of cholestyramine on the symptoms of reflux gastritis. A randomized, double blind, crossover study. Gastroenterology. 1977 Sep;73(3):441–443. [PubMed] [Google Scholar]
- Meyer J. H. Reflections on reflux gastritis. Gastroenterology. 1979 Nov;77(5):1143–1145. [PubMed] [Google Scholar]
- Miranda R., Steffes B., O'Leary J. P., Woodward E. R. Surgical treatment of the postgastrectomy dumping syndrome. Am J Surg. 1980 Jan;139(1):40–43. doi: 10.1016/0002-9610(80)90227-5. [DOI] [PubMed] [Google Scholar]
- Murphy G. M., Billing B. H., Baron D. N. A fluorimetric and enzymatic method for the estimation of serum total bile acids. J Clin Pathol. 1970 Oct;23(7):594–598. doi: 10.1136/jcp.23.7.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie W. P., Jr Acute gastric mucosal damage induced by bile salts, acid, and ischemia. Gastroenterology. 1975 Apr;68(4 Pt 1):699–707. [PubMed] [Google Scholar]
- Ritchie W. P., Jr, Delaney J. P. Parietal cell changes in the stomach after ulcer operations. J Surg Res. 1972 Jan;12(1):17–23. doi: 10.1016/0022-4804(72)90138-2. [DOI] [PubMed] [Google Scholar]
- Ritchie W. P., Jr, Shearburn E. W., 3rd Acute gastric mucosal ulcerogenesis is dependent on the concentration of bile salt. Surgery. 1976 Jul;80(1):98–105. [PubMed] [Google Scholar]
- Stern D. H., Walsh J. H. Gastrin release in postoperative ulcer patients: evidence for release of duodenal gastrin. Gastroenterology. 1973 Mar;64(3):363–369. [PubMed] [Google Scholar]
- Toye D. K., Williams J. A. Post-gastrectomy bile vomiting. Lancet. 1965 Sep 11;2(7411):524–526. doi: 10.1016/s0140-6736(65)91475-3. [DOI] [PubMed] [Google Scholar]
- Tympner F., Domschke W., Demling L. Duodeno-gastric reflux in gastric ulcer patients in relation to intestinal metaplasia of the gastric mucosa. Acta Hepatogastroenterol (Stuttg) 1976 Sep-Oct;23(5):360–364. [PubMed] [Google Scholar]
- van Heerden J. A., Phillips S. F., Adson M. A., McIlrath D. C. Postoperative reflux gastritis. Am J Surg. 1975 Jan;129(1):82–88. doi: 10.1016/0002-9610(75)90172-5. [DOI] [PubMed] [Google Scholar]