Abstract
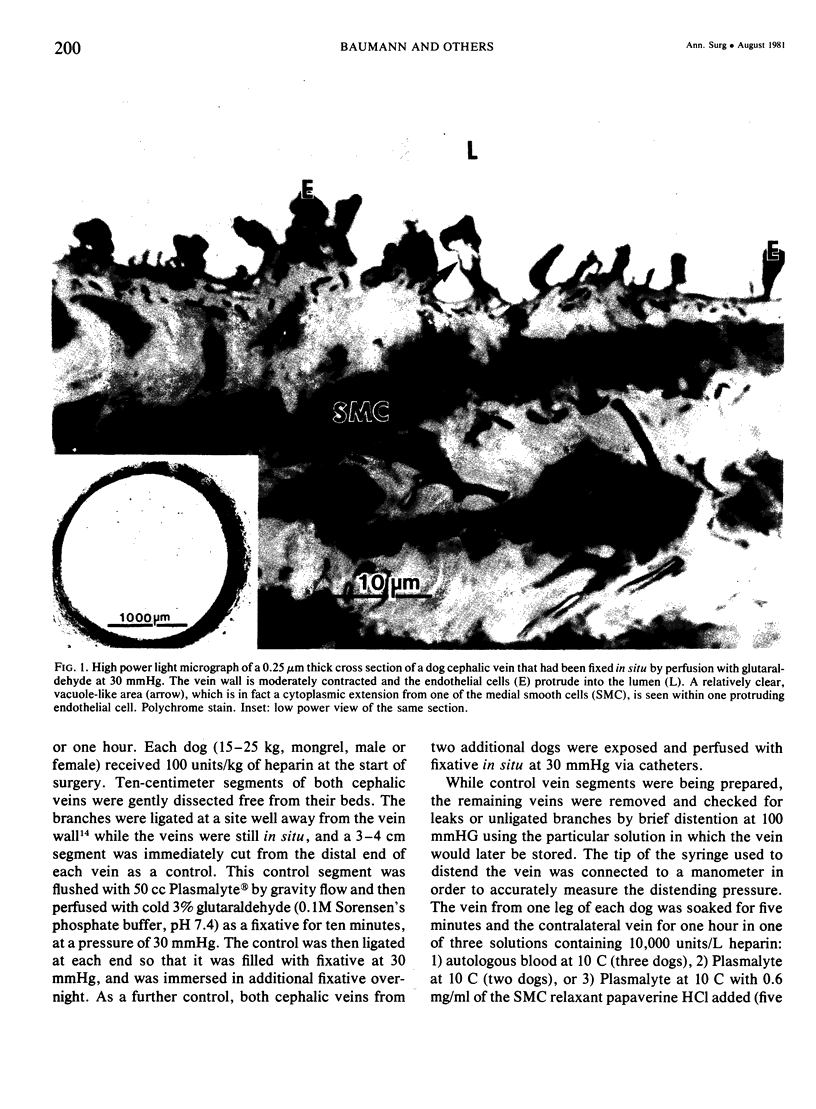
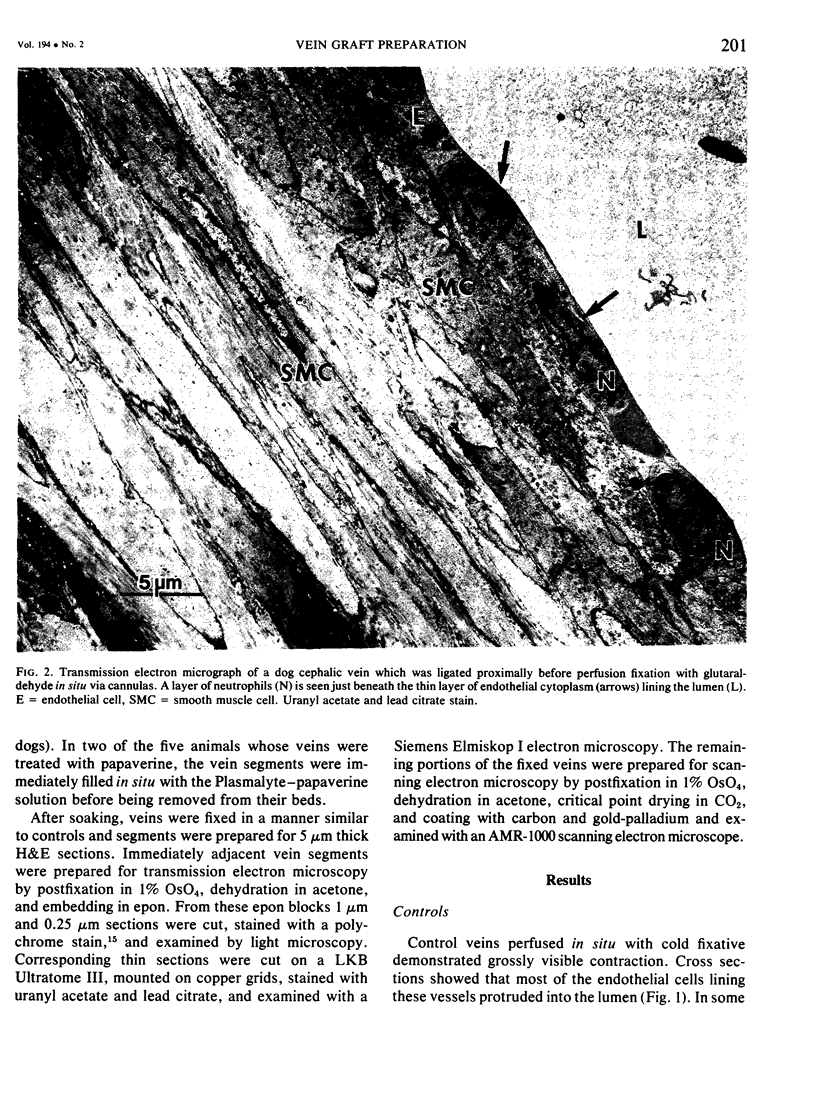
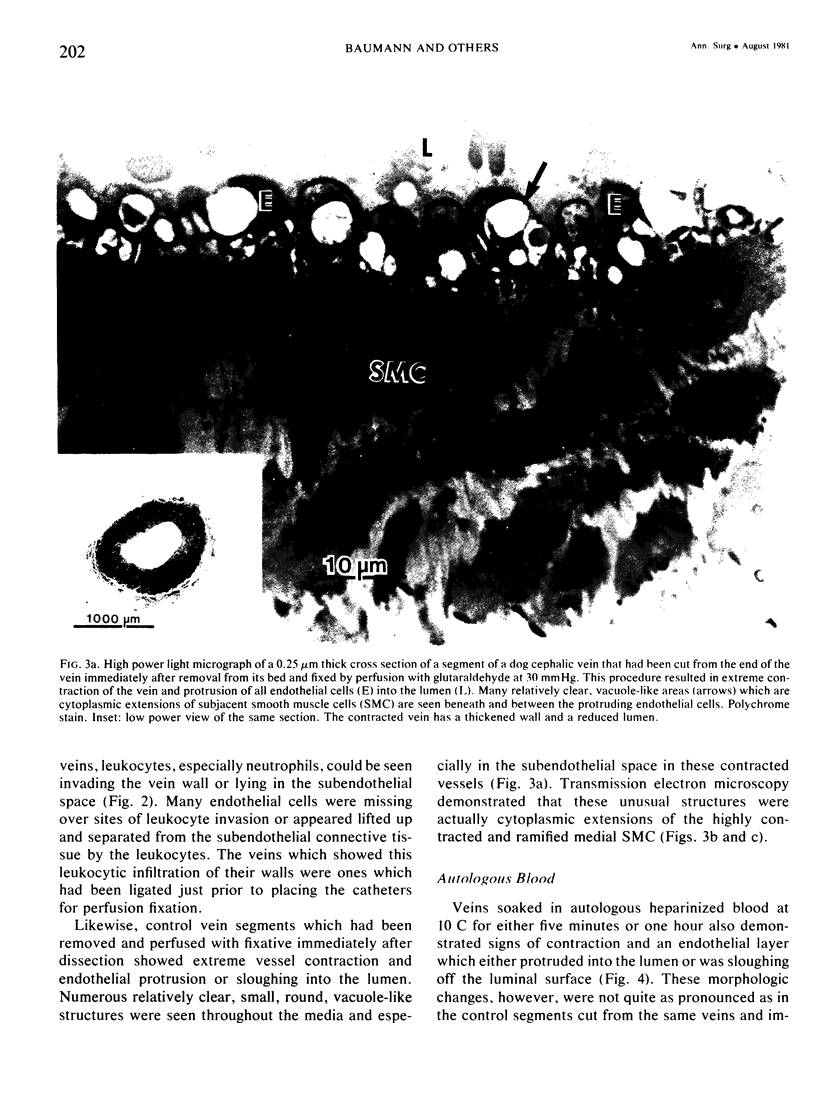
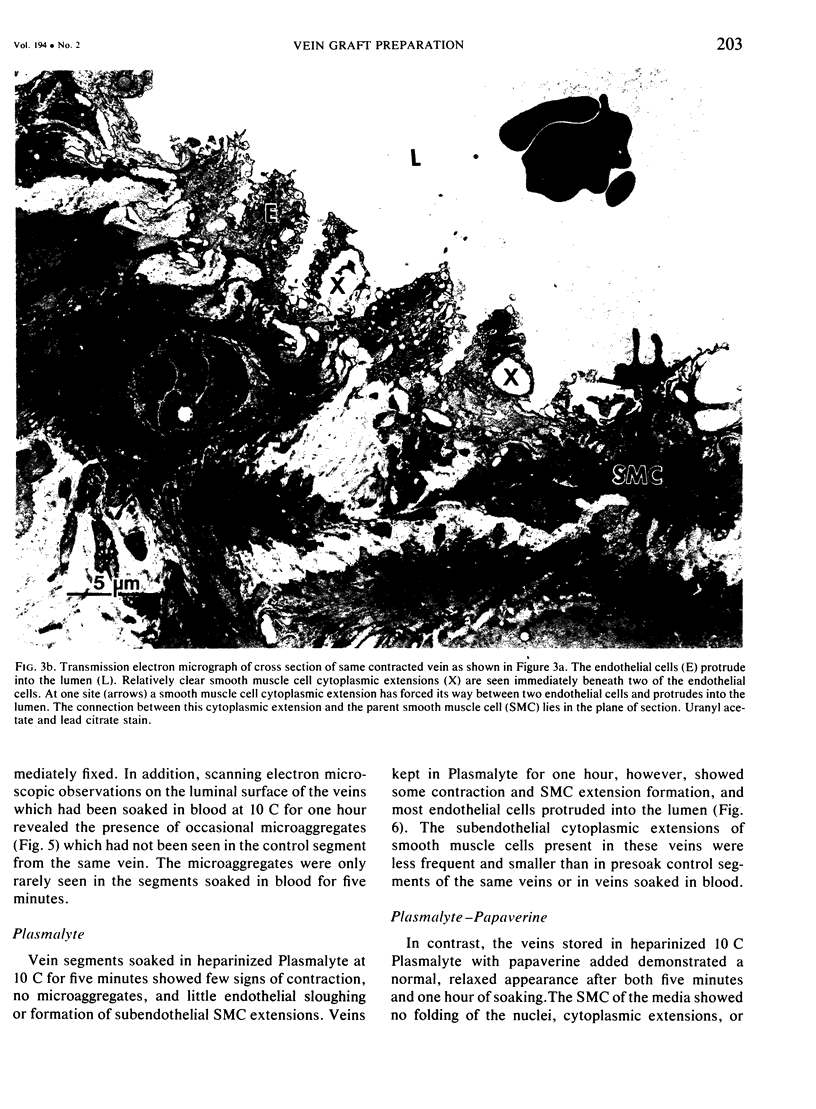
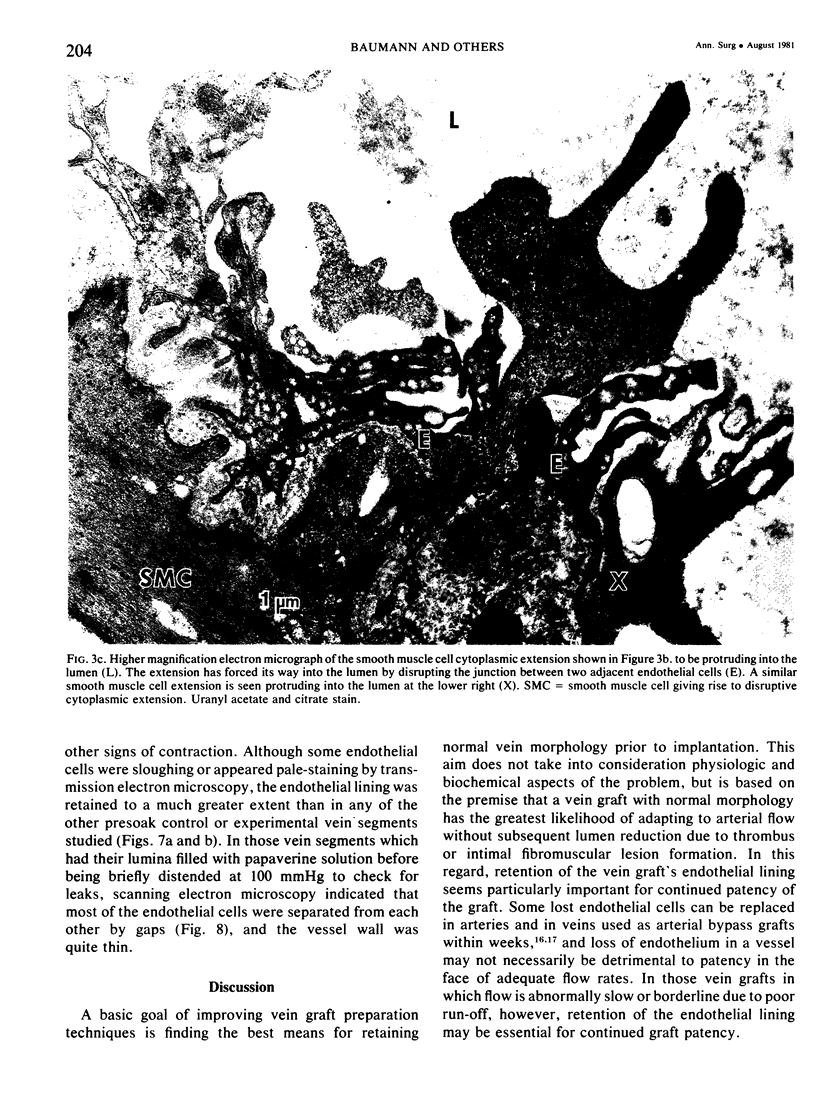
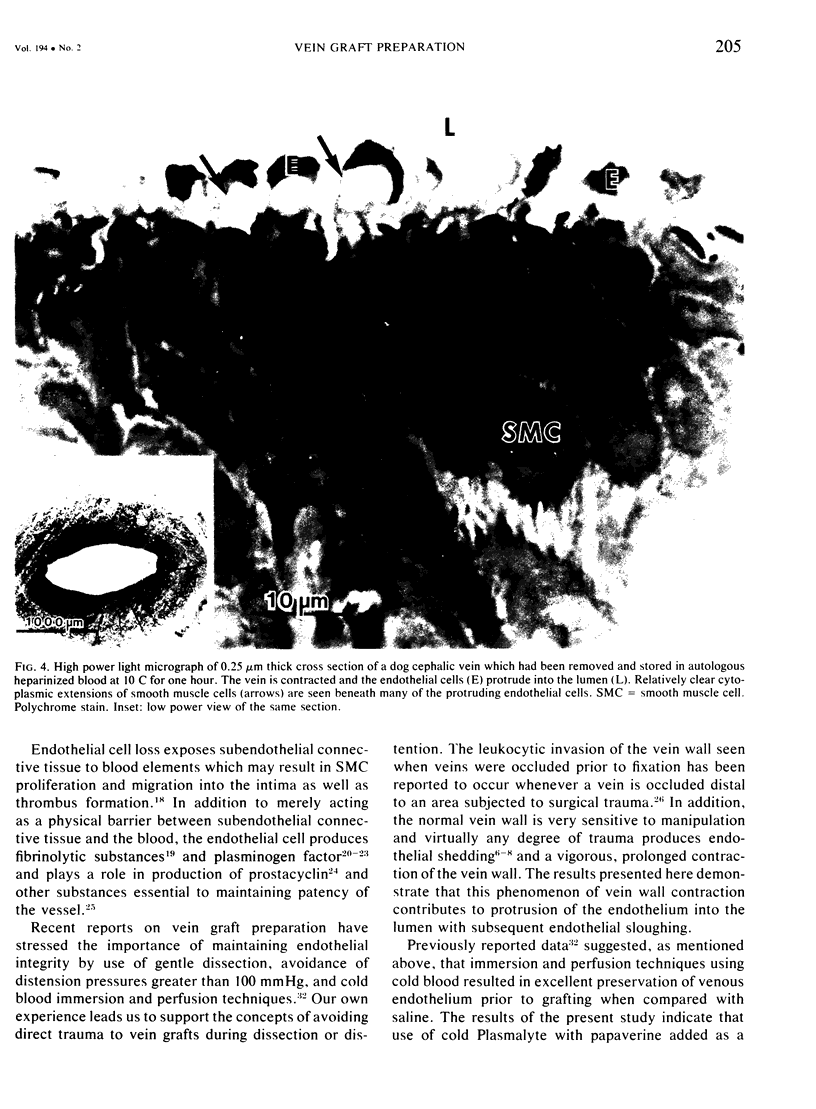
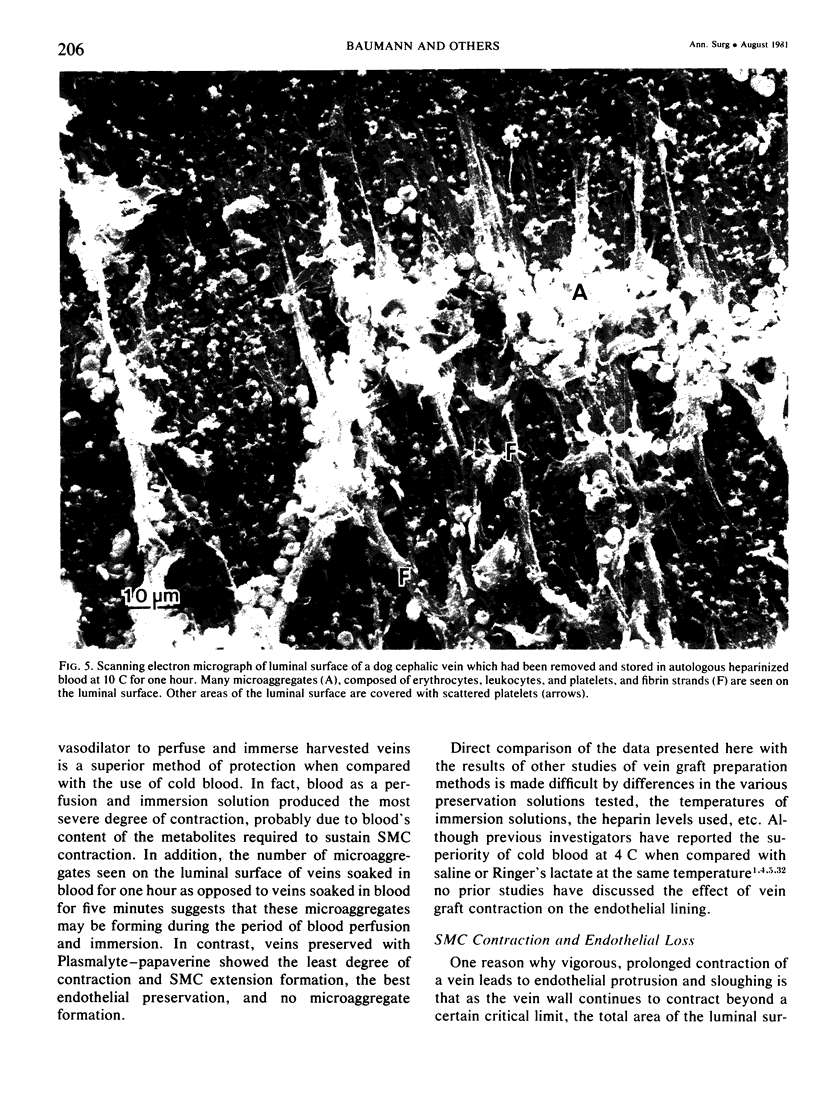
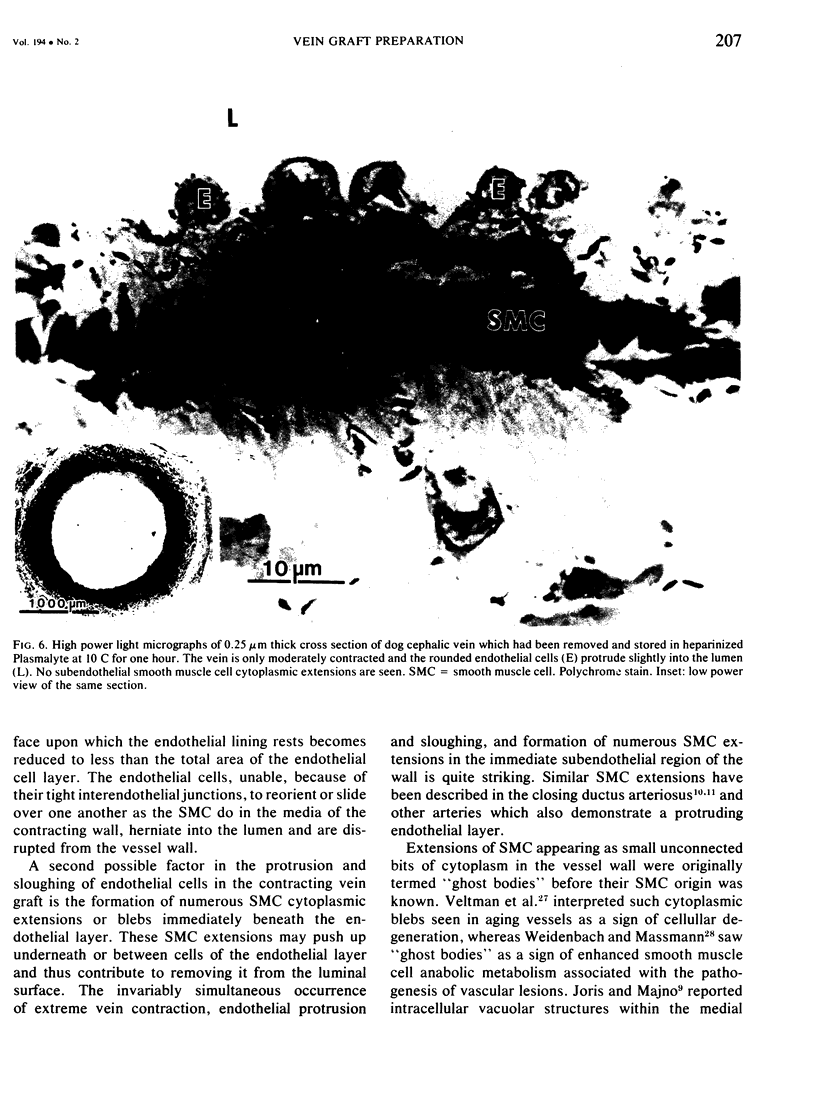
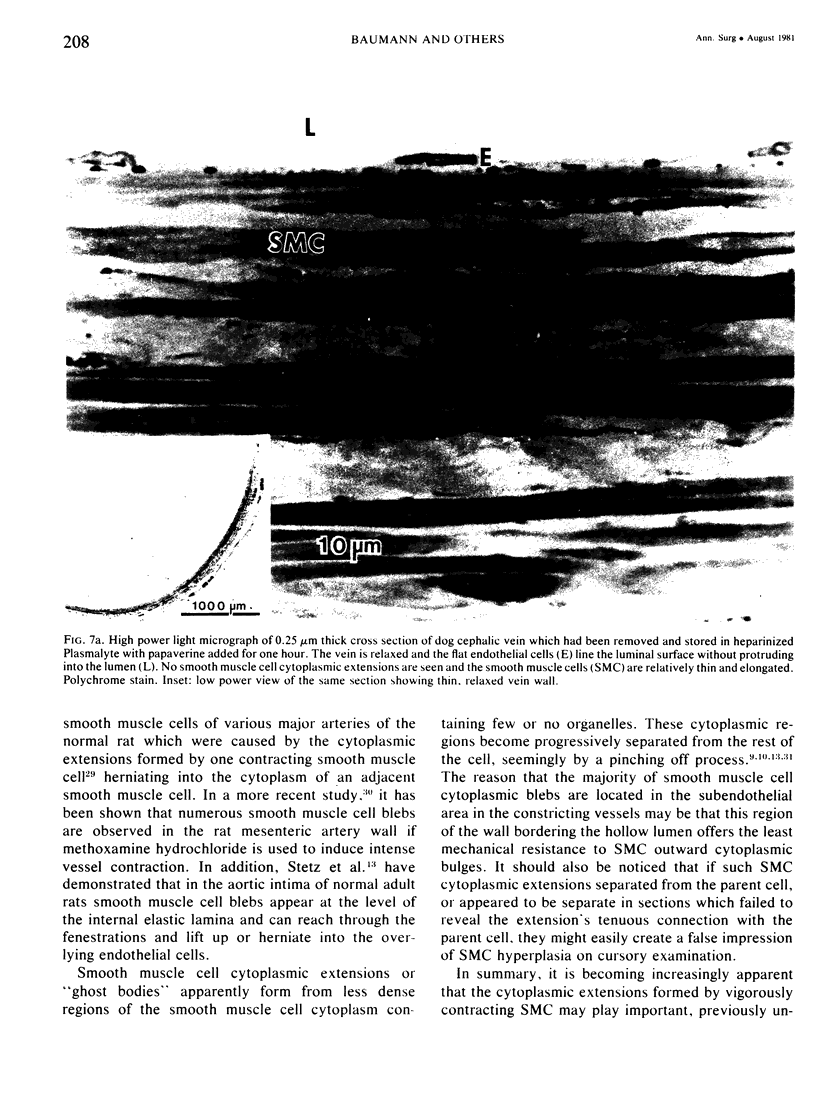
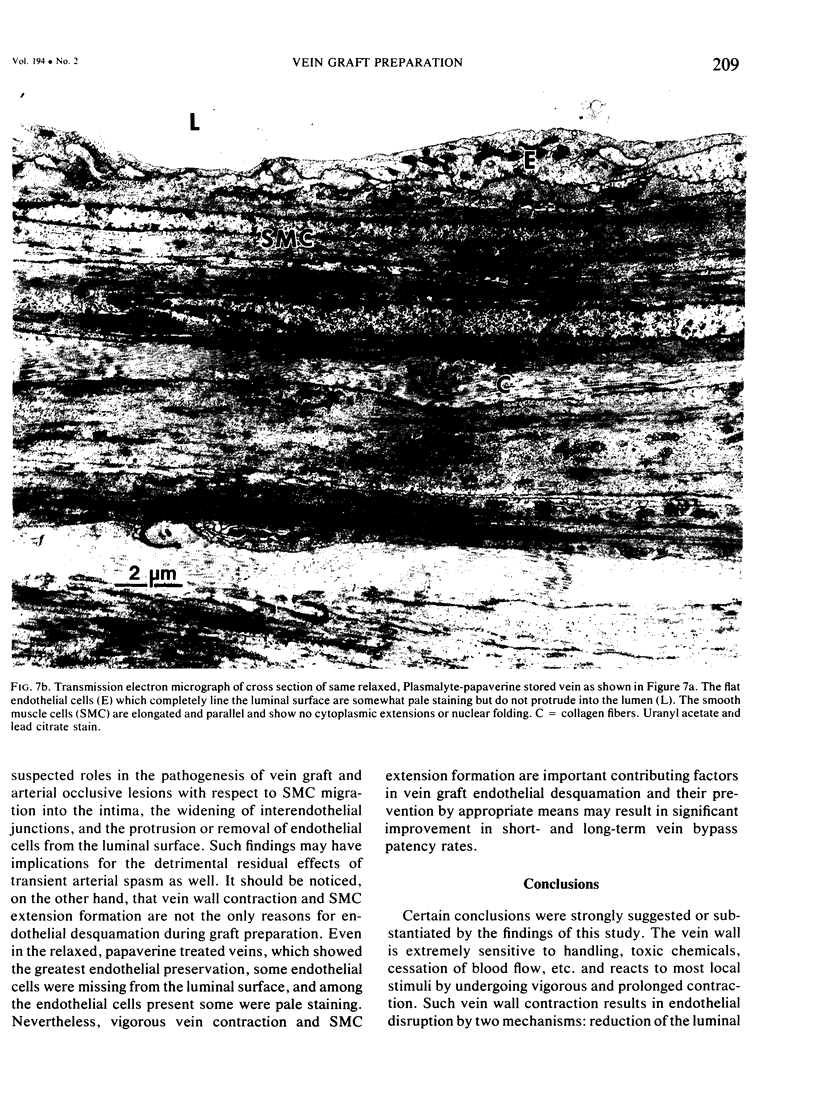
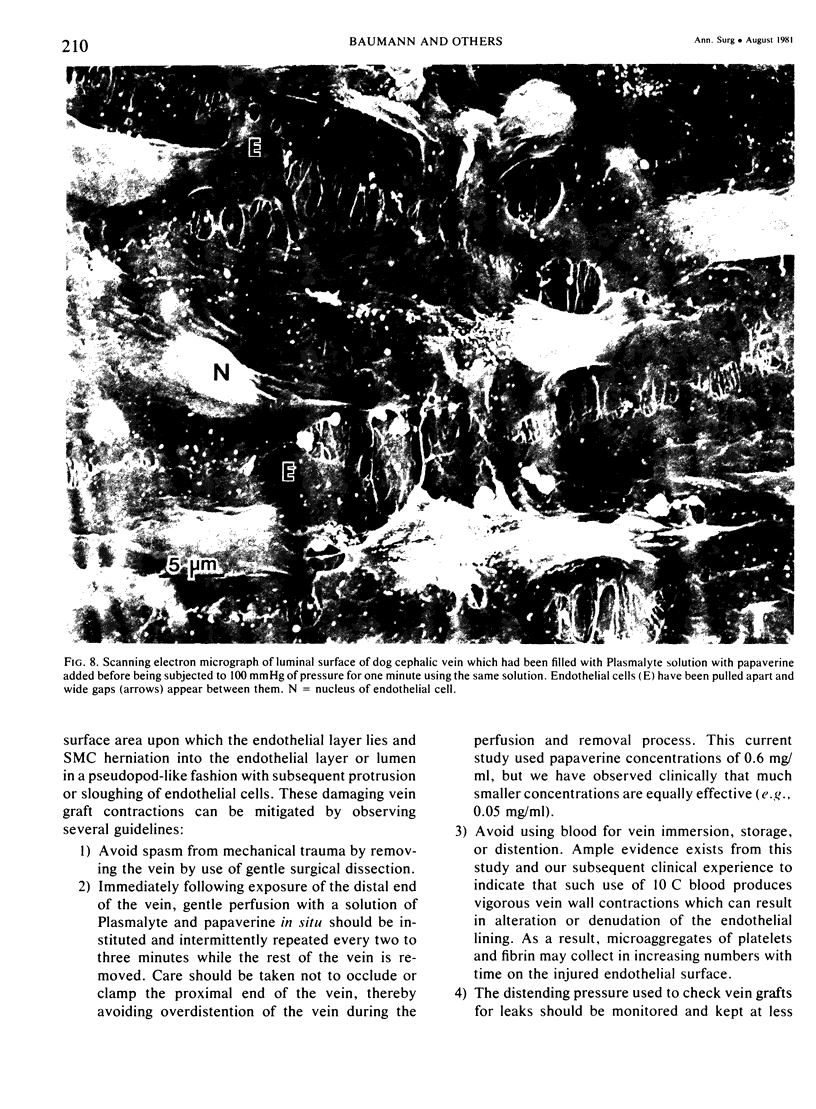
Meticulous preservation of the endothelial lining of vein grafts harvested during vascular operations is undoubtedly an important factor in determining patency rates following bypass procedures. Destruction of the vein graft's endothelial lining prior to graft implantation results in a more thrombogenic graft which is essentially a collagen-lined tube. This study used light, transmission, and scanning electron microscopy to investigate effects of various methods of vein graft preparation on endothelial and smooth muscle cells of the dog cephalic vein. Veins were removed and stored in one of three heparinized solutions at 10 C for either five minutes or one hour: autologous blood, Plasmalyte® or Plasmalyte® with 0.6 mg/ml papaverine HCI added. The vein wall was extremely sensitive to dissection, manipulation, or introduction of fixative solutions and reacted to such stimuli with severe contraction which not only diminished the luminal diameter but also resulted in protrusion of endothelial cells into the lumen and formation of cytoplasmic extensions of medial smooth muscle cells. Such cytoplasmic extensions were particularly frequent in the immediate subendothelial area and appeared to be instrumental in elevating, separating, or desquamating the endothelial cell lining. Veins stored in blood alone demonstrated the greatest vessel wall contraction and endothelial cell loss. Veins soaked in Plasmalyte®-papaverine solution had the most relaxed and normal appearance with minimal endothelial cell loss. Papaverine-treated veins which were subjected to brief periods of distension at pressures of 100 mmHg or greater demonstrated large gaps between the endothelial lining cells. The results suggest pretreatment with papaverine greatly reduces vein graft endothelial cell loss due to contraction, although such relaxation may be detrimental if vein grafts are subjected to excessive pressure prior to reversal of relaxation.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ASTRUP T., BULUK K. THROMBOPLASTIC AND FIBRINOLYTIC ACTIVITIES IN VESSELS OF ANIMALS. Circ Res. 1963 Sep;13:253–260. doi: 10.1161/01.res.13.3.253. [DOI] [PubMed] [Google Scholar]
- COCCHERI S., ASTRUP T. Thromboplastic and fibrinolytic activities of large human vessels. Proc Soc Exp Biol Med. 1961 Nov;108:369–372. doi: 10.3181/00379727-108-26941. [DOI] [PubMed] [Google Scholar]
- Fay F. S., Delise C. M. Contraction of isolated smooth-muscle cells--structural changes. Proc Natl Acad Sci U S A. 1973 Mar;70(3):641–645. doi: 10.1073/pnas.70.3.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonkalsrud E. W., Sanchez M., Zerubavel R. Morphological evaluation of canine autogeneous vein grafts in the arterial circulation. Surgery. 1978 Aug;84(2):253–264. [PubMed] [Google Scholar]
- Gottlob R. The preservation of the venous endothelium by "dissection without touchin" and by an atraumatic technique of vascular anastomosis. The importance for arterial and venous surgery. Minerva Chir. 1977 Jun 15;32(11):693–700. [PubMed] [Google Scholar]
- Gundry S. R., Jones M., Ishihara T., Ferrans V. J. Intraoperative trauma to human saphenous veins: scanning electron microscopic comparison of preparation techniques. Ann Thorac Surg. 1980 Jul;30(1):40–47. doi: 10.1016/s0003-4975(10)61200-3. [DOI] [PubMed] [Google Scholar]
- Gundry S. R., Jones M., Ishihara T., Ferrans V. J. Optimal preparation techniques for human saphenous vein grafts. Surgery. 1980 Dec;88(6):785–794. [PubMed] [Google Scholar]
- Holle G., Massmann J., Weidenbach H. Experimentally induced early changes in arteries. Pathol Eur. 1974;9(2):125–132. [PubMed] [Google Scholar]
- Joris I., Majno G. Cell-to-cell herniae in the arterial wall. I. The pathogenesis of vacuoles in the normal media. Am J Pathol. 1977 May;87(2):375–398. [PMC free article] [PubMed] [Google Scholar]
- Kobori K., Suzuki K., Yoshida Y., Ooneda G. Light and electron microscopic studies on rat arterial lesions induced by experimental arterial contraction. Virchows Arch A Pathol Anat Histol. 1979 Dec;385(1):29–39. doi: 10.1007/BF00433538. [DOI] [PubMed] [Google Scholar]
- Kobori K., Suzuki K., Yoshida Y., Ooneda G. Light and electron microscopic studies on rat arterial lesions induced by experimental arterial contraction. Virchows Arch A Pathol Anat Histol. 1979 Dec;385(1):29–39. doi: 10.1007/BF00433538. [DOI] [PubMed] [Google Scholar]
- Krupski W., Thal E. R., Gewertz B. L., Buja L. M., Murphy M. E., Hagler H. K., Fry W. J. Endothelial response to venous injury. Arch Surg. 1979 Nov;114(11):1240–1248. doi: 10.1001/archsurg.1979.01370350042004. [DOI] [PubMed] [Google Scholar]
- Loskutoff D. J., Edgington T. E. Synthesis of a fibrinolytic activator and inhibitor by endothelial cells. Proc Natl Acad Sci U S A. 1977 Sep;74(9):3903–3907. doi: 10.1073/pnas.74.9.3903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malczak H. T., Buck R. C. Regeneration of endothelium in rat aorta after local freezing. A scanning electron microscopic study. Am J Pathol. 1977 Jan;86(1):133–148. [PMC free article] [PubMed] [Google Scholar]
- Ross R., Glomset J. A. The pathogenesis of atherosclerosis (first of two parts). N Engl J Med. 1976 Aug 12;295(7):369–377. doi: 10.1056/NEJM197608122950707. [DOI] [PubMed] [Google Scholar]
- Sato T., Shamoto M. A simple rapid polychrome stain for epoxy-embedded tissue. Stain Technol. 1973 Sep;48(5):223–227. doi: 10.3109/10520297309116628. [DOI] [PubMed] [Google Scholar]
- Smokovitis A. Regions of constantly increased plasminogen activator activity along the intima of the normal aorta. Haemostasis. 1978;7(5):303–319. doi: 10.1159/000214273. [DOI] [PubMed] [Google Scholar]
- Stanley J. C., Sottiurai V., Fry R. E., Fry W. J. Comparative evaluation of vein graft preparation media: electron and light microscopic studies. J Surg Res. 1975 Mar;18(3):235–246. doi: 10.1016/0022-4804(75)90147-x. [DOI] [PubMed] [Google Scholar]
- Stewart G. J., Ritchie W. G., Lynch P. R. Venous endothelial damage produced by massive sticking and emigration of leukocytes. Am J Pathol. 1974 Mar;74(3):507–532. [PMC free article] [PubMed] [Google Scholar]
- Szilagyi D. E., Elliott J. P., Hageman J. H., Smith R. F., Dall'olmo C. A. Biologic fate of autogenous vein implants as arterial substitutes: clinical, angiographic and histopathologic observations in femoro-popliteal operations for atherosclerosis. Ann Surg. 1973 Sep;178(3):232–246. doi: 10.1097/00000658-197309000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TODD A. S. The histological localisation of fibrinolysin activator. J Pathol Bacteriol. 1959 Jul;78:281–283. doi: 10.1002/path.1700780131. [DOI] [PubMed] [Google Scholar]
- Veltmann E., Backwinkel K. P., Themann H., Hauss W. H. Elektronenmikroskopische Untersuchungen zur Entstehung von 'ghost bodies' in Aorten. Virchows Arch A Pathol Anat Histol. 1975 Sep 18;367(4):281–288. doi: 10.1007/BF01239336. [DOI] [PubMed] [Google Scholar]
- Weidenbach H., Massmann J. Zur Frage der "ghost bodies" bei experimenteller Gefässwandschädigung. Exp Pathol (Jena) 1975;10(5-6):251–257. [PubMed] [Google Scholar]
- Weksler B. B., Marcus A. J., Jaffe E. A. Synthesis of prostaglandin I2 (prostacyclin) by cultured human and bovine endothelial cells. Proc Natl Acad Sci U S A. 1977 Sep;74(9):3922–3926. doi: 10.1073/pnas.74.9.3922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt A. P., Taylor G. W. Vein grafts: changes in the endothelium of autogenous free vein grafts used as arterial replacements. Br J Surg. 1966 Nov;53(11):943–947. doi: 10.1002/bjs.1800531107. [DOI] [PubMed] [Google Scholar]
- Yoder M. J., Baumann F. G., Goodyear J. I., Imparato A. M. Endothelial alterations in the constricting rabbit ductus arteriosus: relationship to smooth muscle cell bleb formation. Scan Electron Microsc. 1980;(3):271–276. [PubMed] [Google Scholar]
- Yoder M. J., Baumann F. G., Grover-Johnson N. M., Brick I., Imparato A. M. A morphological study of early cellular changes in the closure of the rabbit ductus arteriosus. Anat Rec. 1978 Sep;192(1):19–39. doi: 10.1002/ar.1091920103. [DOI] [PubMed] [Google Scholar]