Abstract
BAL8557 is the water-soluble prodrug of BAL4815, a new broad-spectrum antifungal. Healthy male subjects were randomly assigned to four treatment cohorts to receive multiple oral doses or multiple 1-h constant-rate intravenous infusions of BAL8557. Loading doses of BAL8557 were equivalent to 100 mg (followed by once-daily maintenance doses of 50 mg) or 200 mg (followed by once-daily maintenance doses of 100 mg) of BAL4815. In each cohort, six subjects received active drug and two subjects received the placebo. Study duration was 21 days (oral) and 14 days (intravenous). All adverse events reported were mild or moderate, except one severe rhinitis event which was not related to trial medication. After both routes of administration, maximum drug concentration observed in plasma (Cmax) and area under the concentration-time curve (AUC) values of BAL4815 increased proportionally to the administered dose. AUC values reflected a fourfold to fivefold accumulation of active drug in plasma during once-daily dosing, which is in line with the long elimination half-life of BAL4815 determined after the last administration (mean, 84.5 to 117 h). At steady state, the volume of distribution was large and amounted to 308 to 542 liters. Systemic clearance reached only 2.4 to 4.1 liter/h. At the levels obtained in the present study, Cmax values of 2.56 and 2.55 μg/ml after oral and intravenous administrations, respectively, there was no indication of CYP3A4 induction or inhibition (as revealed by the urinary 6-β-hydroxycortisol/cortisol test). Based on AUC values after oral and intravenous administration, an excellent oral bioavailability can be predicted for BAL4815. Once-daily oral dosing of 50- or 100-mg equivalents of BAL8557 were recently demonstrated to be efficacious in a phase 2 study conducted with patients with esophageal candidiasis. These doses (preceded by adequate loading dose[s]) will be further explored in the treatment of systemic mycoses.
The frequency of severe systemic mycoses has steadily increased during the last years, and resistance to currently prescribed antifungals is growing rapidly (8, 10, 17). Therefore, there is an urgent need for new potent and safe antifungals which can be administered orally as well as intravenously (6, 9, 18).
The water-soluble triazole prodrug BAL8557 (for chemical structure, see reference 15) is suitable for oral and intravenous administration. In plasma, it is rapidly and almost quantitatively (>99%) converted by esterases to BAL8728 (prodrug cleavage product) and to BAL4815 (active drug) (2). Area under the concentration-time curve (AUC) values of BAL8728 were low and amounted to approximately 1% of the corresponding AUCs of BAL4815 (15). BAL4815 is a potent inhibitor of ergosterol biosynthesis and shows in vitro broad-spectrum activity against all major opportunistic fungi and the true pathogenic fungi. In rat and murine models, BAL4815 was highly effective against systemic candidiasis and aspergillosis (2; Warn et al., Poster at Advances Against Aspergillus, San Francisco, CA, 2004; and D. Te Dorsthorst, P. E. Verwej, J. F. Meis, and J. W. Mouton, Abstr. 44th Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-1874, 2004).
First pharmacokinetic data of BAL4815 in human were obtained in a single-ascending-dose study after intravenous and oral administrations (15). As already expected from animal experiments (2), BAL4815 was characterized in healthy subjects by a long elimination half-life (56 to 104 h), a low plasma clearance (1.9 to 5.0 liter/h), and a large volume of distribution (155 to 494 liters). Urinary recovery of BAL4815 was less than 0.4% of the infused dose. The toxicity profile of BAL8557 in animals was consistent with that of other azoles (2).
To assess the safety and pharmacokinetics of BAL4815 in humans, healthy male subjects received multiple ascending oral and intravenous doses of prodrug BAL8557. Based on the pharmacokinetic data obtained in a single-ascending-dose study, a considerable drug accumulation in plasma was to be expected during once-daily dosing. Therefore, loading doses of BAL8557, which were equivalent to 100 mg (respectively, 200 mg) of BAL4815, followed by once-daily maintenance doses of 50 mg (respectively, 100 mg), were administered orally or as an intravenous infusion.
MATERIALS AND METHODS
Study design.
This was a double-blind, randomized, placebo-controlled, multiple-dose study investigating two sequential dose levels for each route of administration. The study was conducted in full compliance with the principles of the Declaration of Helsinki, part III, as amended at Somerset West (1996) and according to the International Conference on Harmonization Guideline for Good Clinical Practice. Prior to study start, written informed consent was obtained from all participating volunteers. This study was performed at Applied Analytical Industries GmbH & Co. in Neu-Ulm, Germany, and the protocol was approved prior to study start by the Ethics Committee of the Bavarian Chamber of Physicians, Munich, Germany.
Subjects and study procedure.
Thirty-two healthy male subjects were randomly assigned to four treatment cohorts to receive BAL8557 (six subjects per cohort) or placebo (two subjects per cohort). The mean age plus or minus standard deviation (SD) of the participating subjects was 37.5 ± 6.5 years (range, 21 to 45 years), and the mean body weight plus or minus SD was 80.1 ± 9.0 kg (range, 61.1 to 100 kg). Cohort 1 received an oral loading dose of 100-mg equivalents of BAL4815 in the form of prodrug BAL8557, followed by once-daily maintenance doses of 50 mg up to study day 21. Cohort 2 received an oral loading dose of 200-mg equivalents of BAL4815 followed by once-daily maintenance doses of 100 mg up to study day 21. Cohort 3 received a constant-rate 1-h intravenous infusion of 100 mg as the loading dose, followed by once-daily maintenance infusions of 50 mg up to study day 14. Cohort 4 received a constant-rate 1-h intravenous infusion of 200 mg as the loading dose, followed by once-daily maintenance infusions of 100 mg up to study day 14. Administration of starting dose level was supported by safety factors from the single-dose study with humans and toxicity experiments with animals. The second higher-dose regimen depended on the availability and acceptance of all relevant tolerability and safety data assessed at the previous lower-dose level.
Intravenous infusions or hard gelatin capsules, containing 50 or 100 mg of active drug, were administered in the morning after an overnight fast. All subjects remained in the clinical unit from the morning of study day −1 until the 24-h pharmacokinetic blood sample had been drawn on study day 14 (cohorts 3 and 4) or on study day 21 (cohorts 1 and 2).
Safety parameters assessed at screening included medical history, serology (hepatitis B, hepatitis C, and human immunodeficiency virus), and drug abuse testing, and physical examination, including determination of body weight and body mass index, was performed at screening and follow-up. Recording of vital signs and body temperature, 12-lead electrocardiograms (ECGs), and performance of laboratory safety tests (hematology, blood chemistry, creatinine clearance, and urinalysis) occurred at screening, during the study, and at follow-up. Adverse events were monitored daily from the first drug administration until follow-up.
Pharmacokinetic sampling.
Blood samples for pharmacokinetic assessment in cohorts 1 and 2 (oral administration) were collected from the cubital vein of the forearm on study day 1, study day 8, and study day 14 predose and at 15, 30, 45, 60, 75, and 90 min and 2, 3, 4, 6, 8, 10, 12, 14, 16, and 24 h after administration. In addition, trough-level samples were collected predose on study days 3, 4, 5, 6, 7, 10, 11, 12, 13, 16, 17, 18, 19, and 20. On study day 21, blood samples were collected predose and at 15, 30, 45, 60, 75, and 90 min and 2, 3, 4, 6, 8, 10, 12, 14, 16, 24, 36, 48, 60, 72, 96, 120, 240, 360, and 480 h after drug administration.
Blood samples for pharmacokinetic assessment in cohorts 3 and 4 (intravenous infusion) were collected on study day 1 and study day 8 predose and at appropriate time intervals (see previous paragraph) up to 24 h after start of the 1-h constant infusion. In addition, trough-level samples were collected predose on study days 3, 4, 5, 6, 7, 10, 11, 12, and 13. On study day 14, blood samples were collected predose and at appropriate time intervals up to 480 h after start of infusion (see previous paragraph).
At each time point, a 2.7-ml blood sample was collected into Monovetten tubes containing EDTA as anticoagulant. To avoid degradation of the analytes, 10 μl of 2 M citric acid and 10 μl of 0.1 M paraoxon (plasma esterase inhibitor) were added per ml blood to the collection tubes on the day before blood drawing. The plasma was separated from blood cells by centrifugation (15 min at 1,500 × g, temperature 4°C), transferred into polypropylene tubes, and stored at −70°C.
Urine was collected at 24-h intervals for the determination of the excretion ratio “6-β-hydroxycortisol/cortisol” prior to treatment on study day −1, on study days 1, 8, and 14, and at follow-up. Urine samples were weighted and stored at −20°C. 6-β-Hydroxycortisol and cortisol were measured using standard methods (enzyme-linked immunosorbent assay kit from Stabiligen S. A. [Nancy, France] and Biomérieux Vidas technology).
Analytical methods.
Quantification of BAL4815 and BAL8728 in plasma was performed by liquid chromatography coupled online with tandem mass spectrometry operating in the positive electrospray ionization and multiple reaction-monitoring modes. Calibration and quality control samples were prepared in pretested blank plasma. Day-to-day performance was controlled by analysis of quality control samples.
Sample analysis was carried out with 50 μl of plasma. Plasma used for the calibration samples and quality control samples was stabilized with citric acid at pH 5 (±0.1) and 1 mM paraoxon to prevent metabolic degradation. After precipitation of proteins with acetonitrile and subsequent centrifugation, a 100-μl aliquot of supernatant was diluted with 350 μl of mobile phase A (H2O plus 1% HCOOH and 0.05% NH3 [25%]). An aliquot of each solution (20 to 50 μl) was injected into the system of liquid chromatography coupled online with tandem mass spectrometry. All unknown, calibration, or quality control samples were subjected to the same procedure.
The interassay precision for human plasma was ≤6.6% for BAL4815, ≤6.8% for BAL8728, and ≤11.1% for BAL4815 in human urine, respectively. The validated lower limit of quantification in plasma was 5 ng/ml for both analytes. Approximately 10% of the plasma samples were randomly analyzed in duplicate. The means of both measured values were reported.
Analysis of pharmacokinetic data.
Pharmacokinetic parameters were derived by noncompartmental analysis (7) using the computer program WinNonlin version 4.0.1 (16). Actual sampling times and uniform weighting were used for the pharmacokinetic analysis. The following pharmacokinetic parameters were estimated from the plasma concentration-versus-time curves for active drug BAL4815 and for prodrug cleavage product BAL8728: AUC0-∞, AUC0-24 h or AUClast, Cmax, Tmax, and t1/2. In addition, clearance and volume of distribution were estimated for BAL4815 because conversion of prodrug to BAL4815 is virtually complete (15).
Cmax is the maximum drug concentration observed in plasma and Tmax is the time to reach maximum drug concentration in plasma (not assessed after intravenous infusion). AUC0-∞ is the area under the plasma concentration time curve from time point zero extrapolated to infinity. AUClast is the area under the plasma concentration time curve from time point zero to the last sampling time with a concentration above the limit of quantification. AUC0-24 h is the area under the plasma concentration-versus-time curve from time point zero up to 24 h after drug intake or start of infusion. AUC values were calculated using the linear trapezoidal rule. t1/2 is the apparent terminal elimination half-life. CLSS is the total systemic clearance at steady state after intravenous infusion, estimated by CLSS = dose/AUC0-24 h. VSS is the apparent volume of distribution at steady state after intravenous infusion, estimated by VSS = (dose × AUMC/AUC2) − (dose × T/2AUC), where AUMC is area under the first moment of the concentration-time curve. CLSS/F is the total systemic clearance after oral administration at steady state, estimated by CLSS/F = dose/AUC0-24 h, where F is the fraction of dose available to the systemic circulation (bioavailability). VSS/F is the apparent volume of distribution in the postdistributive phase, estimated by VSS/F = CLSS/k, where k is the elimination rate constant.
Drug accumulation “RACC” was estimated by “AUC0-24 h on the last study day divided by AUC0-24 h on study day 1” normalized for identical doses (assuming dose proportionality). The predicted drug accumulation “R” was calculated according to R = 1/1−e−kτ, where τ is the dosing interval (7).
Urinary excretion was calculated from urine concentrations of 6-β-hydroxycortisol or cortisol and from the urine volumes collected during the 24-h sampling intervals.
Statistical evaluation.
The primary parameters for the assessment of “dose proportionality” after oral or intravenous administration were the AUC0-24 h values after the first administration and AUC0-∞ values of BAL4815 after the last administration as well as the Cmax values on the first and last days of administration. A one-way analysis of variance (ANOVA) model with the factor “dose” was applied to the logarithmically transformed and dose-normalized values of AUC and Cmax (15).
The primary parameters for assessing the effect of time on AUC (observed accumulation) were the AUC0—24 h values on all study days for cohorts 1 and 2 and for cohorts 3 and 4. A linear mixed-effect model with within factor day and between factor cohort was applied separately to the logarithmically transformed AUC0-24 h values to cohorts 1 and 2 and cohorts 3 and 4. Assuming dose proportionality, AUC values of the loading doses were adjusted to those of the maintenance doses. There was no need to adjust for heteroscedasticity and temporal dependency.
To test the effect of dose on t1/2, VSS, and CLSS (estimated on the last study day), a one-way ANOVA model with the factor “dose” was applied separately to cohorts 1 and 2 and cohorts 3 and 4.
RESULTS
Subjects.
A total of 24 healthy male subjects received the study medication and were evaluable for pharmacokinetics and safety on all study days, except for subject no. 23 in cohort 3, who discontinued the study prematurely on study day 10 (see “Safety” below).
Pharmacokinetics.
On the study days where plasma samples were collected up to only 24 h postdosing, elimination half-lives could not be estimated reliably in many subjects. Plasma concentrations of BAL4815 seemed to decrease biphasically/multiphasically (15), and, therefore, much shorter half-lives were obtained during the 24-h intervals compared with the half-lives assessed on the last study days, where concentrations were available up to 480 h postdose. On the first study days, mean t1/2 amounted to 24 to 31 h, while t1/2 was 85 to 117 h on the last study days. The mean extrapolated AUC from the last sampling point to infinity was approximately 42 to 78% on the 24-h sampling days, but only 2.4 to 5.7% on the last study days (0- to 480-h sampling). Obviously, the “true” elimination half-lives of BAL4815 were reliably assessable on only the last study days. Clearance and volume of distribution at steady state were calculated using AUC0-24 h and are thus provided in the tables for study day 14 and study day 21 (if applicable).
Pharmacokinetics of BAL4815 after oral administration.
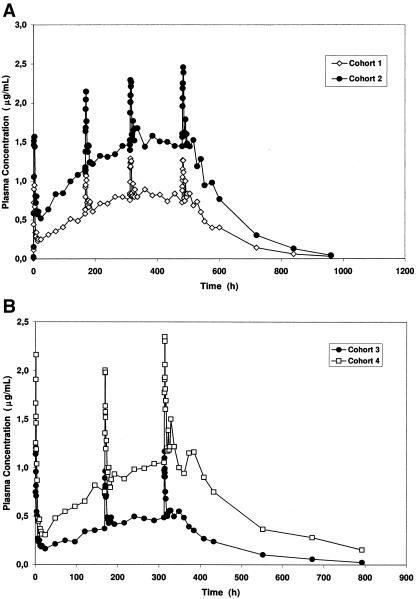
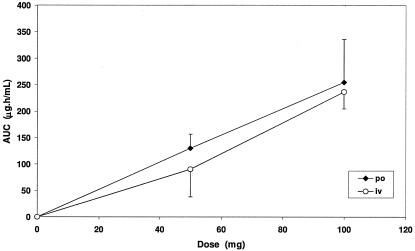
The mean (plus or minus SD) plasma concentration-time profiles of BAL4815 after oral administration of BAL8557 are presented in Fig. 1A. Plasma concentrations of BAL4815 increased rapidly after administration of BAL8557 and reached a maximum of 2.0 to 3.5 h after drug intake (Table 1). Thereafter, plasma levels declined slowly and remained detectable after the last dose up to the last sampling point at 480 h in all subjects except one. Figure 1A and the AUC0-24 h values in Table 1 reflect a considerable accumulation of BAL4815 in plasma during multiple dosing. On study day 1 and on study day 21, AUC and Cmax values increased proportionally to the dose. Figure 2 shows the AUC0-∞ values of BAL4815 versus dose on the last study day. At steady state, mean elimination half-lives estimated in the terminal elimination phase reached 85 to 98 h. Systemic clearance (CLSS/F) was low (2.4 to 2.5 liter/h), and the volume of distribution (VSS/F) was large (310 to 350 liters). There were no significant differences between dose groups regarding t1/2, CLSS/F, and VSS/F (see statistical assessment).
FIG. 1.
A, Mean plasma profiles of BAL4815 after oral administration of BAL8557 (cohort 1, loading dose of 100-mg equivalents of BAL4815 followed by once-daily maintenance doses of 50 mg; cohort 2, loading dose of 200-mg equivalents of BAL4815 followed by once-daily maintenance doses of 100 mg). B, Mean plasma profiles of BAL4815 after intravenous infusion of BAL8557 (cohort 3, loading dose of 100-mg equivalents of BAL4815 followed by once-daily maintenance doses of 50 mg; cohort 4, loading dose of 200-mg equivalents of BAL4815 followed by once-daily maintenance doses of 100 mg).
TABLE 1.
Pharmacokinetic parameters by cohort for BAL4815 estimated after once-daily oral administrations of BAL8557a
| Cohortb and study day | Tmax (h) | Cmax (μg/ml) | AUC0-24 h (μg · h/ml) | AUC0-∞ (μg · h/ml)c | t1/2 (h) | VSS/F (liters) | CLSS/F (liters/h) |
|---|---|---|---|---|---|---|---|
| Cohort 1 | |||||||
| Day 1 | 2.0 (2.0-3.0) | 1.10 (±0.173) | 8.75 (±1.26) | — | — | — | — |
| Day 8 | 2.0 (1.5-3.0) | 1.20 (±0.215) | 18.1 (±4.45) | — | — | — | — |
| Day 14 | 3.0 (1.25-4.0) | 1.40 (±0.178) | 22.1 (±4.92) | — | — | — | 2.36 (±0.479) |
| Day 21 | 2.25 (1.5-3.0) | 1.37 (±0.230) | 21.6 (±4.30) | 130 (±26.5) | 98.4 (±21.3) | 346 (±112) | 2.39 (±0.430) |
| Cohort 2 | |||||||
| Day 1 | 2.0 (1.25-3.07) | 1.85 (±0.326) | 18.5 (±3.11) | — | — | — | — |
| Day 8 | 3.0 (2.0-12.0) | 2.33 (±0.472) | 34.0 (±5.70) | — | — | — | — |
| Day 14 | 2.25 (1.5-4.0) | 2.61 (±0.365) | 41.5 (±6.02) | — | — | — | 2.45 (±0.356) |
| Day 21 | 3.5 (2.0-4.0) | 2.56 (±0.434) | 40.3 (±4.28) | 255 (±80.5) | 84.5 (±28.3) | 308 (±118) | 2.51 (±0.275) |
Values are presented as arithmetic means plus or minus SD for six subjects; median and range are presented for Tmax.
For cohort 1, loading doses of 100-mg equivalents of BAL4815 were followed by once-daily maintenance doses of 50-mg equivalents of BAL4815; for cohort 2, loading doses of 200-mg equivalents of BAL4815 were followed by once-daily maintenance doses of 100-mg equivalents of BAL4815.
—, values could not be reliably estimated as plasma samples could be collected during only a 24-h interval.
FIG. 2.
Mean (plus or minus SD) AUC0-∞ values of BAL4815 on the last study day versus dose after multiple oral administrations or intravenous infusion of prodrug BAL8557.
Pharmacokinetics of BAL4815 after intravenous infusion.
Mean (plus or minus SD) plasma concentration-time profiles of BAL4815 that were obtained after the 1-h constant-rate intravenous infusions of BAL8557 are presented in Fig. 1B. Plasma concentrations of BAL4815 were quantifiable after the last infusion up to the last sampling point at 480 h in all subjects except one. Cmax and AUC values on study days 1 and 14 increased proportionally to the dose. A graphical presentation of AUC0-∞ values versus dose on the last study day is shown in Fig. 2. As found after oral administration, the pharmacokinetic parameters of BAL4815 assessed after intravenous infusion were characterized by a long elimination half-life, a low clearance, and a large volume of distribution (Table 2). The AUC0-24 h values in Table 2 reflect very similar drug accumulations observed after repeated oral administrations.
TABLE 2.
Pharmacokinetic parameters by cohort for BAL4815 estimated after once-daily intravenous 1-h constant-rate infusion of BAL8557a
| Cohortb and study day | Cmax (μ/ml) | AUC0-24 h (μ · h/ml) | AUC0-∞ (μ · h/ml) | t1/2 (h) | VSS (liters) | CLSS (liters/h) |
|---|---|---|---|---|---|---|
| Cohort 3 | ||||||
| Day 1 | 1.28 (±0.122) | 7.32 (±1.09) | — | — | — | — |
| Day 8 | 0.987 (±0.180) | 12.4 (±3.77) | — | — | — | — |
| Day 14c | 1.17 (±0.237) | 14.3 (±5.33) | 90.2 (±52.2) | 93.0 (±40.1) | 470 (±162) | 4.06 (±1.97) |
| Cohort 4 | ||||||
| Day 1 | 2.32 (±0.445) | 12.9 (±1.93) | — | — | — | — |
| Day 8 | 2.52 (±1.05) | 24.3 (±5.79) | — | — | — | — |
| Day 14 | 2.55 (±0.883) | 33.6 (±9.67) | 236 (±31.5)d | 117 (±17.6)d | 542 (±229)d | 3.19 (±0.901) |
Values are presented as arithmetic means plus or minus SD of six subjects except where indicated. —, values could not be reliably estimated as plasma samples could be collected during only a 24-h interval.
For cohort 3, loading doses of 100-mg equivalents of BAL4815 were followed by once-daily maintenance doses of 50-mg equivalents of BAL4815; for cohort 4, loading doses of 200-mg equivalents of BAL4815 were followed by once-daily maintenance doses of 100-mg equivalents of BAL4815.
n = 5.
n = 4.
Intersubject variability after oral and intravenous administration was 10 to 43% for Cmax and 11 to 37% for AUC0-24 h of BAL4815.
Dose proportionality and effect of dose on t1/2, VSS, and CLSS of BAL4815.
The statistical assessments of dose proportionality of AUC0-24 h on the first study day, AUC0-∞ on the last study day, and Cmax on the first and last study days were based on the comparison of the dose-normalized and logarithmically transformed parameters between dose groups by using a one-way ANOVA.
After oral administration, there was no significant dose effect for AUC (P = 0.58 on study day 1 and P = 0.76 on study day 21) or Cmax (P = 0.09 on study day 1 and P = 0.51 on study day 21), and at the α = 5% level dose, proportionality can be assumed for both parameters. A similar result was obtained after intravenous infusion. A statistically significant dose effect was not found for AUC (P = 0.19 on study day 1 and P = 0.28 on study day 14) or Cmax (P = 0.24 on study day 1 and P = 0.73 on study day 14), and dose proportionality can be assumed for both parameters.
The dependency of variables VSS, VSS/F, CLSS, CLSS/F, and t1/2 (estimated on the last study day) on dose was tested by a one-way ANOVA. There was no significant effect of dose on t1/2 (P = 0.36 after oral [p.o.] dose and P = 0.31 after intravenous [i.v.] dose), VSS (P = 0.58 after p.o. and P = 0.59 after i.v.), and CLSS (P = 0.59 after p.o. and P = 0.36 after i.v.). Therefore, at the α = 5% level, the null hypothesis of equal parameter means, for the factor, “dose” cannot be rejected.
Accumulation of BAL4815 in plasma.
Drug accumulation “RACC” of BAL4815 in plasma was estimated by “AUC0-24 h on the last study day divided by AUC0-24 h on study day 1.” As shown in Table 3, drug accumulation in plasma was high (3.8- to 5.2-fold) and comparable after both routes of administration. This drug accumulation (effect of time) was highly statistically significant.
TABLE 3.
Drug accumulation of BAL4815 after once-daily oral or intravenous dosinga
| Cohort no. (dose type) | AUC0-24 hb on study day 1 (μg · h/ml) | AUC0-24 h on last study day (μg · h/ml) | Accumulation factor RACC |
|---|---|---|---|
| 1 (p.o.) | 8.75 (±1.26) | 21.6 (±4.30) | 4.93 (±0.66) |
| 2 (p.o.) | 18.5 (±3.11) | 40.3 (±4.28) | 4.54 (±0.65) |
| 3 (i.v.) | 7.32 (±1.09) | 14.3 (±5.33) | 3.82 (±1.01) |
| 4 (i.v.) | 12.9 (±1.93) | 33.6 (±9.67) | 5.20 (±1.14) |
Values are presented as arithmetic means plus or minus SD of six subjects.
Accumulation was calculated with AUC values adjusted to maintenance dose as dose proportionality can be assumed for BAL4815.
The starting dose in all cohorts was twice as high as the subsequent maintenance doses. Therefore, the AUC0-24 h on day 1 has been divided by 2. This division is justified because dose proportionality could be assumed in all cohorts.
Pharmacokinetics of prodrug cleavage product BAL8728.
After oral administration, plasma concentrations of BAL8728 were quantifiable in less than 5% of all samples and, therefore, pharmacokinetics were not evaluable. BAL8728 concentrations were detectable up to 90 min after dosing, and maximum concentrations reached 0.009 μg/ml in cohort 1 and 0.019 μg/ml in cohort 2. In contrast, after intravenous infusion, plasma concentrations of BAL8728 were quantifiable for up to 8 h after start of infusion and reliable pharmacokinetic parameters could be estimated by noncompartmental analysis (Table 4). Mean elimination half-lives were short and amounted to approximately 1 h in both cohorts. Cmax and AUClast values seemed to increase fairly proportionally to the dose. On the last day of administration, mean AUC0-∞ values of BAL8728 reached 0.4% and 0.2% of the corresponding AUC0-∞ values of BAL4815 in cohorts 3 and 4, respectively. Mean Cmax values of BAL8728 on study day 1 amounted to 24.4% and 21.6% of those determined for BAL4815. As expected with the short half-life of BAL8728, no accumulation of this compound occurred in plasma during once-daily dosing of BAL8557.
TABLE 4.
Pharmacokinetic parameters by cohort for BAL8728 estimated after once-daily intravenous 1-h constant-rate infusion of BAL8557a
| Cohortb and study day | Tmax (h) | Cmax (μg/ml) | AUClast (μg · h/ml) | AUC0-∞ (μg · h/ml) | t1/2 (h) |
|---|---|---|---|---|---|
| Cohort 3 | |||||
| Day 1 | 1.0 (0.5-1.0) | 0.311 (±0.027) | 0.476 (±46.8) | 0.491 (±0.039) | 1.05 (±0.153) |
| Day 8 | 1.0 (0.5-1.0) | 0.157 (±0.018) | 0.229 (±24.8) | 0.245 (±0.030) | 1.04 (±0.122) |
| Day 14c | 0.75 (0.5-1.0) | 0.167 (±0.019) | 0.238 (±52.2) | 0.253 (±0.048) | 1.10 (±0.213) |
| Cohort 4 | |||||
| Day 1 | 1.0 (0.25-1.0) | 0.492 (±0.072) | 0.872 (±49.1) | 0.881 (±0.052) | 1.07 (±0.215) |
| Day 8 | 1.0 (0.75-1.0) | 0.278 (±0.039) | 0.425 (±59.7) | 0.436 (±0.059) | 1.09 (±0.120) |
| Day 14 | 1.0 (1.0-1.02) | 0.282 (±0.042) | 0.428 (±64.3) | 0.440 (±0.062) | 1.06 (±0.188) |
Values are presented as arithmetic means plus or minus SD of six subjects except where indicated; median and range are presented for Tmax.
For cohort 3, loading doses of 100-mg equivalents of BAL4815 were followed by once-daily maintenance doses of 50-mg equivalents of BAL4815; for cohort 4, loading doses of 200-mg equivalents of BAL4815 were followed by once-daily maintenance doses of 100-mg equivalents of BAL4815.
n = 5.
Intersubject variability of the pharmacokinetic parameters of BAL8728 was low and reached 8.7 to 15% for Cmax and 5.2 to 22% for AUC0-∞.
Urinary excretion ratio of “6-β-hydroxycortisol/cortisol.”
In the present study, the 24-h urinary excretion ratio of 6-β-hydroxycortisol/cortisol was investigated on study day −1 (predose), study days 1, 8, and 14, and at follow-up. As shown in Table 5, there was no indication of relevant inducing or inhibiting properties of BAL4815 during once-daily oral administration over 3 weeks and intravenous infusions over 2 weeks.
TABLE 5.
Mean (plus or minus SD) ratios of 24-hour urinary excretion of 6-β-hydroxycortisol/cortisol after once-daily administration of BAL8557a
| Group (dose type) | Dose (loading dose/maintenance dose) | Ratio of 6-β-hydroxycortisol/cortisol
|
||||
|---|---|---|---|---|---|---|
| Day 1 | Day 1 | Day 8 | Day 14 | Follow-up | ||
| Cohort 1 (p.o.) | 100 mg/50 mg | 8.01 (4.39) | 8.80 (3.31) | 8.28 (2.52) | 7.77 (4.01) | 10.4 (5.94) |
| Cohort 2 (p.o.) | 200 mg/100 mg | 8.87 (3.29) | 8.44 (2.18) | 5.95 (2.59) | 6.73 (2.71) | 6.89 (1.68) |
| Cohort 3 (i.v.) | 100 mg/50 mg | 11.7 (6.16) | 12.9 (2.24) | 10.1 (2.57) | 14.4b (1.43) | 11.1b (7.23) |
| Cohort 4 (i.v.) | 200 mg/100 mg | 5.81 (2.70) | 6.85 (3.11) | 6.52 (2.31) | 6.39 (4.37) | 4.96 (2.40) |
| Placeboc | 8.87 (2.81) | 10.0 (3.22) | 10.7 (7.49) | 9.31 (3.51) | 10.8 (5.04) | |
Values present means plus or minus SD of six subjects except where indicated.
n = 5.
n = 8.
Safety.
Overall, out of 24 subjects dosed with BAL8557, 19 subjects reported 39 adverse events (Table 6). The most frequent adverse events reported were headache, nasopharyngitis, and rhinitis. All adverse events reported were mild or moderate, except one volunteer who suffered from severe rhinitis. However, the responsible physician judged this event to be not related to the trial medication. There were no serious adverse events. One subject on low-dose i.v. BAL8557 discontinued study medication on study day 10 for intercurrent illness, with symptoms of headache, nasopharyngitis, and diarrhea.
TABLE 6.
Summary of adverse events by dose and intensity level
| AE parameter | No. of mild, moderate, and severe AEsa for dose equivalents of BAL4815
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 100 mg/50 mg p.o., i.v. (n = 12)
|
200 mg/100 mg p.o, i.v. (n = 12)
|
Placebo (n = 8)
|
|||||||
| Mild | Moderate | Severe | Mild | Moderate | Severe | Mild | Moderate | Severe | |
| All body systems | |||||||||
| Subjects with at least one AE | 7 | 1 | 0 | 7 | 3 | 1 | 4 | 4 | 0 |
| Total no. of AEs | 15 | 3 | 0 | 15 | 5 | 1 | 9 | 5 | 0 |
| Investigations | |||||||||
| Liver function test abnormal | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Musculoskeletal | |||||||||
| Back pain | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Pain in extremity | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| CNSb | |||||||||
| Dizziness | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Headache | 1 | 1 | 0 | 3 | 2 | 0 | 3 | 3 | 0 |
| Migraine | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Respiratory | |||||||||
| Cough | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Pharyngolaryngeal pain | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Rhinitis | 2 | 0 | 0 | 3 | 0 | 1 | 1 | 0 | 0 |
| Gastrointestinal | |||||||||
| Abdominal pain | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Diarrhea | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Gingivitis | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| General diseases | |||||||||
| Fatigue | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Soft tissue inflammation | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Venipuncture site pain | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 |
| Venipuncture site reaction | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Vessel puncture site haem | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Infections | |||||||||
| Nasopharyngitis | 3 | 1 | 0 | 1 | 2 | 0 | 4 | 1 | 0 |
AE, adverse event.
CNS, central nervous system.
An abnormal liver function test, with elevated γ-glutamyl transpeptidase (161 U/liter), aspartate amino transferase (66 U/liter), and (90 U/liter) alanine aminotransferase, was reported on study day 14 for one subject on oral high-dose BAL8557. The study medication was continued, and aspartate amino transferase and alanine aminotransferase values returned to normal on study day 17 and the γ-glutamyl transpeptidase value returned to normal at follow-up.
For all other laboratory values, abnormal values were infrequent and sporadic, and no dose-dependent trend in abnormal values was apparent for any parameter. No ECG abnormalities were reported, and there were no clinically relevant changes of vital signs.
DISCUSSION
The primary objectives of this study with two dose regimens for oral and intravenous administration were the assessment of the pharmacokinetics of active drug BAL4815 and the investigation of its safety and tolerability. As a secondary objective, the pharmacokinetics of prodrug cleavage product BAL8728 were investigated.
The “true” elimination half-lives of BAL4815 (and elimination rate constants) were reliably assessable only when steady-state conditions had been reached. Therefore, the pharmacokinetic parameters (except for Cmax and Tmax) that were obtained on the first study days in the present study are not directly comparable with those estimated after single-ascending doses, where plasma concentrations were analyzed up to more than 16 days after dosing (14). Nevertheless, this multiple-dose study confirms BAL4815 as a drug with a low clearance and a large volume of distribution (pointing to a good tissue penetration). Intersubject variability of Cmax and AUC0-24 h of BAL4815 was low to moderate (10 to 42%).
After once-daily oral or intravenous dosing, concentrations of BAL4815 reflect considerable accumulation in plasma (fourfold to fivefold) in line with its long elimination half-life. However, the observed accumulation was somewhat lower than the predicted drug accumulation of 5.6- to 7.5-fold, which was calculated according to R = 1/1−e−kτ, where τ is the 24-h dosing interval and k is the mean elimination rate constant (derived from mean elimination half-lives of 85 and 117 h on the last study days [cf. Tables 1 and 2]). Obviously, steady-state conditions were not completely reached before 2 weeks of daily intravenous dosing or oral dosing. Assuming a half-life of 100 h, 90% of the steady state will be theoretically reached after 332 h (2 weeks) and 99% of the steady state after 664 h (4 weeks) (7).
Clearance values at steady state were calculated by dose/AUC0-24 h and are thus provided after oral administration on study days 14 and 21 (Table 1). However, as discussed above, steady-state conditions may have not been reached before study day 14 in all subjects and, therefore, CLSS values assessed on the last study days present the most reliable values.
As confirmed by a one-way ANOVA, AUC and Cmax of BAL4815 increased proportionally to the dose after both routes of administration (P ≥ 0.09). There was no significant effect of dose on CLSS (P ≥ 0.36), VSS (P ≥ 0.58), or t1/2 (P ≥ 0.31) (estimated on the last study day).
Based on a tentative comparison of the AUC values of BAL4815, the absolute bioavailability of the oral formulation of BAL8557 appeared to be excellent. The somewhat higher plasma concentrations of BAL4815 obtained after oral administration compared with those after intravenous infusion might be explained by presystemic metabolism of prodrug and prodrug cleavage product. The excellent absorption after oral administration should enable an easy switch from intravenous to oral administration during therapeutic treatment. As found after single-dose administration (15), only very few and low plasma concentrations of prodrug cleavage product BAL8728 were detectable after oral administration and a pharmacokinetic assessment was not possible. However, after intravenous infusion, plasma concentrations of BAL8728 were quantifiable up to 8 h after start of infusion. Pharmacokinetics were characterized by short elimination half-lives, and systemic exposure to BAL8728 was very low. On the last day of administration, mean AUC0-∞ values of BAL8728 were less than 1% of the corresponding AUC0-∞ values of active drug BAL4815. As expected by its short half-life, no accumulation of BAL8728 was observed in plasma upon daily dosing of BAL8557. The pharmacokinetic parameters of BAL8728 were comparable to those obtained previously in a single dose study after intravenous infusions (15).
Voriconazole, another broad-spectrum antifungal azole, exhibits, similarly to BAL4815, an excellent oral bioavailability and a large volume of distribution (4). Due to saturation of its metabolism, its terminal elimination half-life is dose dependent and not predictive of accumulation or elimination. Saturable elimination was also found for the antifungal azole itraconazole which reached steady-state conditions after 48 h of twice-daily intravenous dosing (3). Both voriconazole and itraconazole are given twice daily as loading regimens, followed by once daily. Shorter elimination half-lives than those found for BAL4815 were also determined for fluconazole (30 h) (14). Like BAL4815, the antifungal triazole ravuconazole is characterized by a long elimination half-life (76 to 202 h) and high protein binding (98%) (M. Marino, V. Mummaneni, J. Norton, O Hadjilambris, and P. Pierce, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstr. J-1622, 2001). Due to its pharmacokinetic and efficacy profiles, BAL4815 is an attractive drug for both treatment and prophylaxis of fungal infections.
The 24-h urinary excretion ratio of 6-β-hydroxycortisol/cortisol is considered to be a useful noninvasive test to evaluate inducing or inhibiting properties of drugs when subjects are their own control. While this test is totally validated for induction, it is still under debate for some inhibition and it seems not reliable enough to measure actual CYP3A4 activity (5). Rifampin, for example, which has been shown to be a very strong inducer, caused a sixfold increase of 6-β-hydroxycortisol urinary excretion (11) and ketoconazole was the most potent inhibitor of cortisol metabolism (1). In the present study, the above-mentioned ratio was investigated predose, on 3 days during the study, and at follow-up. A comparison of these ratios provided no indication of relevant inducing and inhibiting CYP3A4 properties of BAL4815 during the applied dose regimens.
BAL8557 was well tolerated. All adverse events were classified as mild or moderate except one severe event which was not related to the trial medication. No clinically relevant changes in vital signs or ECG were observed. Abnormal laboratory values were infrequent and revealed no trend for dose dependency.
Conclusion.
BAL8557 was rapidly converted in plasma to its active form, BAL4815, which revealed predictable pharmacokinetics. After repeated oral and intravenous administrations, dose proportionality could be assumed for AUC and Cmax values and there was no indication of a relevant inhibition or induction of CYP3A4-metabolizing enzymes at the levels investigated. Based on a tentative comparison of the AUC values of BAL4815, the absolute bioavailability of the oral formulation of BAL8557 appeared to be excellent.
Once-daily oral dosing of 50- or 100-mg equivalents of BAL8557 was recently demonstrated to be efficacious in a phase 2 study conducted with patients with esophageal candidiasis. These doses (preceded by adequate loading dose[s]) will be further explored in the treatment of systemic mycoses.
REFERENCES
- 1.Back, D. J., J. F. Tjia, and S. M. Abel. 1992. Azoles, allylamines and drug metabolism. Br. J. Dermatol. 126:14-18. [DOI] [PubMed] [Google Scholar]
- 2.Basilea Pharmaceutica, Ltd. Data on file.
- 3.Boogaerts, M. A., J. Maertens, R. Van der Geest, A. Bosly, J. M. Michaux, A. Van Hoof, M. Cleeren, R. Wostenborghs, and K. De Beule. 2001. Pharmacokinetics and safety of a 7-day administration of intravenous itraconazole followed by a 14-day administration of itraconazole oral solution in patients with hematologic malignancy. Antimicrob. Agents Chemother. 45:981-985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.FDA Antiviral Drugs Advisory Committee. 2002. Voriconazole. Briefing document. [Online.] http://www.fda.gov/cder/foi/nda/2002/21-266_VFEND_biopharmr.pdf.
- 5.Galteau, M. M., and F. Shamsa. 2003. Urinary 6β-hydroxycortisol: a validated test for evaluating drug induction or drug inhibition mediated through CYP3A in humans and in animals. Eur. J. Clin. Pharmacol. 59:713-733. [DOI] [PubMed] [Google Scholar]
- 6.Garber, G. 2001. An overview of fungal infections. Drugs 61(Suppl. 1):1-12. [DOI] [PubMed] [Google Scholar]
- 7.Gibaldi, M., and D. Perrier. 1982. Pharmacokinetics, p. 445-449, 2nd ed. Marcel Dekker, Inc., New York, N.Y.
- 8.Granier, F. 2000. Invasive fungal infections. Epidemiology and therapeuties. Presse Med. 29:2051-2056. [PubMed] [Google Scholar]
- 9.Hossain, M. A., and M. A. Ghannoum. 2000. New investigational antifungal agents for treating fungal infections. Expert Opin. Investig. Drugs 9:1797-1813. [DOI] [PubMed] [Google Scholar]
- 10.Karthaus, M., and O. A. Cornely. 2005. Recent developments in the management of invasive fungal infections in patients with hematological malignancies. Ann. Hematol. 84:207-216. [DOI] [PubMed] [Google Scholar]
- 11.McColl, K. E., G. G. Thompson, E. El Omar, M. R. Moore, B. K. Park, and M. J. Brodie. 1978. Effect of rifampicin on haem and bilirubin metabolism in man. Br. J. Pharmacol. 23:553-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meis, J. F., and P. E. Verweij. 2001. Current management of fungal infections. Drugs 61(Suppl. 1):13-25. [DOI] [PubMed] [Google Scholar]
- 13.Richardson, M., and D. Warnock. 1997. Fungal infection: diagnosis and management, 2nd ed. Blackwell Science, Ltd., Oxford, England.
- 14.Ripa, S., L. Ferrante, and M. Prenna. 1993. Pharmacokinetics of fluconazole in normal volunteers. Chemotherapy 39:6-12. [DOI] [PubMed] [Google Scholar]
- 15.Schmitt-Hoffmann, A. , B. Roos, M. Heep, M. Schleimer, E. Weidekamm, T. Brown, M. Roehrle, and C. Beglinger. 2006. Single-ascending-dose pharmacokinetics and safety of the novel broad-spectrum antifungal triazole BAL4815 after intravenous infusions (50, 100, and 200 milligrams) and oral administrations (100, 200, and 400 milligrams) of its prodrug, BAL8557, in healthy volunteers. Antimicrob. Agents Chemother. 50:279-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scientific Consulting, Inc. 2002. Professional WinNonlin, version 4.0.1. Scientific Consulting, Inc., Mountain View, Calif.
- 17.USPHS/IDSA Prevention of Opportunistic Infections Working Group. 1999. USPHS/IDSA guidelines for the prevention of opportunistic infections in persons infected with human immunodeficiency virus. Clin. Infect. Dis. 30:29-65. [PubMed] [Google Scholar]
- 18.Wong-Beringer, A., R. A. Jacobs, and B. J. Guglielmo. 1998. Lipids formulations of amphotericin B: clinical efficacy and toxicities. Clin. Infect. Dis. 27:603-618. [DOI] [PubMed] [Google Scholar]