Abstract
Human cytomegalovirus (HCMV) replication in epithelial and endothelial cells appears to be important in virus spread, disease, and persistence. It has been difficult to study infection of these cell types because HCMV laboratory strains (e.g., AD169 and Towne) have lost their ability to infect cultured epithelial and endothelial cells during extensive propagation in fibroblasts. Clinical strains of HCMV (e.g., TR and FIX) possess a cluster of genes (UL128 to UL150) that are largely mutated in laboratory strains, and recent studies have indicated that these genes facilitate replication in epithelial and endothelial cells. The mechanisms by which these genes promote infection of these two cell types are unclear. We derived an HCMV UL128-to-UL150 deletion mutant from strain TR, TRΔ4, and studied early events in HCMV infection of epithelial and endothelial cells, and the role of genes UL128 to UL150. Analysis of wild-type TR indicated that HCMV enters epithelial and endothelial cells by endocytosis followed by low-pH-dependent fusion, which is different from the pH-independent fusion with the plasma membrane observed with human fibroblasts. TRΔ4 displayed a number of defects in early infection processes. Adsorption and entry of TRΔ4 on epithelial cells were poor compared with those of TR, but these defects could be overcome with higher doses of virus and the use of polyethylene glycol (PEG) to promote fusion between virion and cellular membranes. High multiplicity and PEG treatment did not promote infection of endothelial cells by TRΔ4, yet virus particles were internalized. Together, these data indicate that genes UL128 to UL150 are required for HCMV adsorption and penetration of epithelial cells and to promote some early stage of virus replication, subsequent to virus entry, in endothelial cells.
Human cytomegalovirus (HCMV) is a ubiquitous herpesvirus that seldom causes clinical symptoms in healthy, immunocompetent adults. However, primary infection of neonates is a significant cause of life-threatening diseases and is associated with several neurological birth defects (2, 6). Persistent or recurrent infections in immunocompromised AIDS patients and transplant recipients result in significant morbidity and mortality with the retina, the lungs, and the gastrointestinal tract representing major sites of pathogenesis (6, 28). HCMV displays an extremely broad host cell range in immunocompromised hosts, infecting many different cell types, including epithelial cells, endothelial cells, smooth muscle cells, fibroblasts, neurons, monocytes, and macrophages (6, 28, 42). HCMV replication in retinal pigment epithelial cells appears to be largely responsible for the retinal damage that leads to blindness in HCMV retinitis, and infection of endothelial and smooth muscle cells may contribute to transplant vascular sclerosis, restenosis following angioplasty, and atherosclerosis (16, 28, 49, 58, 66). Epithelial and endothelial cells may also play important roles in viral persistence and dissemination of virus within the body and between hosts (16, 28, 55).
Given the significance of epithelial and endothelial cells to the pathology and epidemiology of HCMV disease, it is vital to understand how the virus replicates in these cells. Unfortunately, commonly studied laboratory strains, including AD169 and Towne, do not replicate well in cultured epithelial or endothelial cells. It has become generally accepted that the loss of broad host cell range exhibited by laboratory strains is the result of a number of genetic mutations and rearrangements that can be correlated with extensive serial propagation on fibroblasts. Strains that have not been extensively propagated on fibroblasts (referred to as “clinical” or “wild-type” strains) generally harbor fewer mutations and retain the ability to infect a wider variety of cultured cell types (10, 13, 20, 35, 43).
Most of the genes located between UL128 and UL150 are either missing or mutated in laboratory strains AD169 and Towne, while HCMV Toledo and other so-called “clinical strains” such as TR, FIX, and Merlin retain these genes (10, 13, 20, 35). Several recent reports have implicated individual genes in the left end of this gene cluster (i.e., UL128, UL130, and UL131) in infection of epithelial and endothelial cells (20, 40, 60). Hahn et al. found that independent deletion of UL128, UL130, or UL131 from an endothelial tropic strain (FIX) resulted in a virus that could no longer infect endothelial cells (20). Additionally, they described a multicistronic mRNA encoding UL128, UL130, and UL131 and an additional transcript encoding just UL128 (20). Transcomplementation experiments suggested that UL130 and UL131 facilitate endothelial cell infection and replication, while the effect of deleting UL128 was probably due to reduced stability of the entire UL128-to-UL131 mRNA (20). Patrone et al. showed that the UL130 gene product is a virion envelope component and that the UL130 protein encoded by Towne is less stable, and therefore less efficiently incorporated, than the UL130 protein of the wild-type FIX. When Towne was propagated on a cell line expressing the more stable FIX UL130 protein, progeny virions were able to infect endothelial cells for one replication cycle (40). Wang et al. reported that a recombinant AD169 containing a repaired UL131 gene (derived from TR) displayed enhanced infection of epithelial and endothelial cells (60). The mechanism or mechanisms by which UL131 enhances infection of epithelial cells remain to be determined. The AD169 UL131 repair virus was syncytial, suggesting that there are other mutations in AD169, which complicates interpretation of these results. Recently, the UL132 protein was shown to be a virion component of strain AD169 and deletion mutants were impaired for growth on fibroblasts, likely during late stages of maturation or egress (56). The UL132 gene is present in all HCMV strains; however, the amino acid sequence is highly variable (10, 13, 35). Genes to the right (i.e., UL133 to UL150) may also participate in infection of epithelial and endothelial cells, but their contribution has not been well characterized. Moreover, little is known about the mechanisms by which any of the UL128-to-UL150 gene products function to promote infection in epithelial and endothelial cells. Infection of epithelial or endothelial cells by laboratory strains of HCMV might potentially be blocked at any stage of virus replication, from entry and uncoating through assembly and egress of virions. However, in many cases early or immediate-early (IE) genes are not expressed in epithelial or endothelial cells, suggesting defects in entry, uncoating, or early gene expression.
We were interested in the earliest events in HCMV infection of epithelial and endothelial cells, including entry. For other herpesviruses, entry into the cytoplasm of host cells frequently involves two stages that can be separated biochemically or genetically. The first step, adsorption or binding of herpesviruses onto cell surfaces, frequently involves very numerous, charged cell surface molecules such as heparan or chondroitin sulfate glycosyaminoglycans (GAGs) (50, 57). For example, adsorption of herpes simplex virus (HSV) is difficult to saturate and does not require viral glycoproteins that are necessary for virus penetration (25). The second step, entry or penetration of herpesvirus into the cytoplasm, requires fusion between viral and cellular membranes. Adsorption onto GAGs may simply increase cell surface concentrations of virus, thus enhancing entry, or, alternatively, GAG binding may be required to trigger fusion (57).
Entry of herpesviruses appears be a complex process involving several sequential stages in the activation of the viral fusion machinery and is best understood for HSV, which requires at least three glycoproteins: gD, which binds several different receptors, gB, and gH/gL (8, 15, 31, 47, 57). Moreover, it is now well established that some herpesviruses can enter different cell types through different mechanisms. For example, Epstein-Barr virus (EBV) can enter epithelial cells and transformed B cells by fusion at the plasma membrane, but enters normal B cells by endocytosis and pH-independent fusion with endosomes (33). Similarly, HSV enters some cells by fusion with the plasma membrane and others by endocytosis followed by low-pH-dependent fusion with endosomal membranes, and still others by pH-independent fusion with endosomes (34, 36-38, 63).
The early stages of HCMV replication, adsorption, and entry have largely been characterized using laboratory strains and human fibroblast cells. HCMV AD169 adsorbs or attaches onto cell surface heparan sulfate GAGs, as shown by competition experiments and digestion with heparan sulfate-specific enzymes (12). Entry of HCMV into fibroblasts involves fusion between the viral envelope and the plasma membrane and is not sensitive to compounds that raise endosomal pH (11). There is evidence that HCMV enters fibroblasts by utilizing cellular receptors, including epidermal growth factor receptor and certain integrins (14, 61, 62). Nucleocapsids are then transported to nuclear pores where the viral genome is released (39). Adsorption of AD169 onto endothelial cells was shown to be comparable to that of endotheliotropic HCMV, but there were apparently other defects in early virus replication preceding release of the genome into the nucleus (52). Given the diversity of entry mechanisms of other herpesviruses, it seems probable that HCMV, with its comparatively large coding capacity, can also utilize different entry pathways to infect different cell types.
In order to characterize early stages of HCMV replication in epithelial and endothelial cells, we utilized a clinical HCMV strain, TR, which infected these cells well, and derived a UL128-to-UL150 deletion mutant, denoted TRΔ4. The data presented suggest that one or more of the genes UL128 to UL150 facilitate adsorption and entry of wild-type HCMV on epithelial cells and that on both epithelial and endothelial cells, wild-type HCMV TR entry is through endocytosis followed by fusion with endosomal membranes in a pH-dependent fashion. In these experiments, both TRΔ4 and AD169 were internalized but failed to enter epithelial cells and were unable to induce IE gene expression. However, defects with both viruses could be overcome by chemically enhancing fusion of virus with cells using polyethylene glycol (PEG). In contrast, endothelial cells infected with TRΔ4 and AD169 did not express IE, even after PEG treatment, indicating that there is another block, subsequent to entry. These results describe aspects of HCMV entry into epithelial and endothelial cells and demonstrate that the HCMV UL128-to-UL150 gene cluster encodes proteins important in virus entry and other early stages of infection of these cells.
MATERIALS AND METHODS
Cells and viruses.
Neonatal, normal human dermal fibroblasts (NHDF) were obtained from Cascade Biologics (Portland, OR) and grown in Dulbecco's modified Eagle's medium (DMEM) (Invitrogen) supplemented with 12% fetal bovine serum (FBS) (HyClone). The retinal pigment epithelial cell line ARPE-19 was obtained from the American Type Culture Collection (ATCC-CRL-2302) and was grown in a 1:1 mix of DMEM and Ham's F-12 medium (Invitrogen) supplemented with 10% FBS. Transformed human umbilical vein endothelial cells (t-HUVECs) were provided by Ashlee Moses (Oregon Health and Sciences University, Portland, OR) and were grown in EBM-2 plus the supplied EGM-2 supplement kit (Cambrex). HCMV strain AD169 was obtained from ATCC. The wild-type strain TR was derived from the vitreous fluid of a patient with AIDS-related HCMV retinitis and was cloned into a bacterial artificial chromosome (BAC), and infectious virus was produced by transfecting NHDF cells (35, 54). All strains of HCMV were propagated on NHDF cells by infection at a multiplicity of less than 0.1 in DMEM plus 5% FBS for 10 to 16 days, cell-associated virus was harvested by sonicating cell pellets, and the cellular debris was removed by centrifugation at 8,000 × g for 20 min. Virus particles were concentrated by centrifugation at 50,000 × g for 1 h through a 20% sorbitol cushion. Virus titers were determined by plaque assay on NHDF cells. HSV-1 gD-null mutant vRR1097 (44) was provided by Richard Roller (University of Iowa, Iowa City) and was propagated on complementing VD60 cells as described previously (31).
Construction of recombinant HCMV TRΔ4.
Recombinant HCMV TRΔ4 was constructed by using the lambda phage linear recombination technique as previously described (7, 29, 65). Briefly, a 1.7-kb PCR product containing the β-galactosidase and ampicillin resistance genes flanked by 60 bp of sequence identical to sequences flanking the UL128-to-UL150 region of the TR genome was generated using primers 5′-AATTTAGTCGGCGACAGAAATCTCAAAACGCGTATTTCGGACAAACACACATTTTATTATGCTGGCACGACAGGTTTCCCGACT-3′ and 5′-GCTATTCTTTATTAACGTCGTTCTCCCCCCGCTTCTACACGCGGACCGCTGCAGACGGCTGAGTTGGTAGCTCTTGAT CCGGCA-3 using a PCR template modified from a pBluescript plasmid (7). The 60-bp regions of flanking sequence identity correspond to nucleotides 211814 to 211874 and 229978 to 230038 of the published TR sequence (accession no. AC146906). Following transformation of TR-BAC host bacteria (EL250; a kind gift from D. L. Court; National Cancer Institute, Frederick, MD) with the LacZ/Ampr PCR product, transformants were selected for growth on ampicillin. Ampicillin-resistant clones were analyzed by EcoRI restriction digest for the loss of an EcoRI site within the replaced TR sequences. Correct genome structure was verified by Southern blotting using a probe directed against sequences within the ampicillin resistance gene. Infectious HCMV was produced by electroporation of BAC DNA into NHDF cells, and the resulting virus, denoted TRΔ4, was propagated on NHDF cells as described above. DNA from the TRΔ4 virus was prepared, and PCR fragments of the junction regions of the insert were generated and sequenced to ensure the fidelity of the mutation.
Antibodies and immunofluorescence.
All antibodies were diluted in immunofluorescence (IF) buffer (0.5% Triton X-100, 0.5% deoxycholate, 2% goat serum, 0.05% sodium azide in phosphate-buffered saline [PBS]). Rabbit polyclonal anti-IE86 antibody (R683) has been described previously (23). Mouse monoclonal anti-gB antibody 27-156 was from William Britt (University of Alabama, Birmingham).Alexa-488-conjugated goat anti-mouse and Alexa-594-conjugated goat anti-rabbit secondary antibodies were obtained from Molecular Probes (Eugene, OR). Cells were grown on glass coverslips in multiwell culture dishes and infected with HCMV and then fixed with 2% formaldehyde in PBS for 15 min followed by three postfixation washes in PBS. Fixed cells were permeabilized and blocked for at least 1 h in IF buffer and then stained with primary antibodies for 1 h, washed with IF buffer, and stained with secondary antibodies for 1 h. For experiments quantifying the percentage of cells infected, cells were subsequently stained with 1.4 μM 4′,6′-diamidino-2-phenylindole dihydrochloride (DAPI) in PBS for 10 min. Coverslips were mounted with Fluoromount-G (Southern Biotech, Birmingham, AL) and analyzed on a Nikon Microphoto-FX immunofluorescence microscope.
Lysosomotropic agents.
A 1.5 M stock of NH4Cl, pH 7.3, in PBS was made fresh for each experiment. Chloroquine was prepared as a 25 mM stock in PBS, and bafilomycin A1 (Sigma) was prepared as a 10 μM stock in dimethyl sulfoxide. Cells were preincubated for 1 h in either normal medium or medium containing drug and then infected with 5 PFU per cell of HCMV strain TR using centrifugal enhancement. Drugs were either present throughout the experiment or added 4 h after inoculation. Cells were fixed at 20 h (fibroblasts and epithelial) or 8 h (endothelial) and analyzed by immunofluorescence for IE86.
Centrifugal and PEG enhancement of infection.
Cells growing on glass coverslips were inoculated with 10 PFU per cell of HCMV. Culture dishes were centrifuged at 800 × g for 2 h at room temperature and then moved to 37°C for 1 h. The cells were washed twice with PBS and were subsequently treated with polyethylene glycol or returned to 37°C until immunofluorescence analysis was performed. PEG 6000 (Fluka) was prepared as a 60% (wt/wt) solution in PBS and diluted with warm PBS to 40% or 44%. Cells were treated with diluted PEG for 30 s and washed immediately five times with warm PBS. To control for effects of PEG on endothelial cells, t-HUVECs were incubated with HSV-1 vRR1097 derived from Vero cells that had been treated with anti-gD monoclonal antibody LP2 and DL11 to neutralize any gD-containing virions. Cultures were then centrifuged and treated with 40% PEG as before. After 12 to 24 h, the number of green fluorescent protein (GFP)-expressing cells was quantified.
Purification of radiolabled virus particles and internalization assays.
NHDF cells were infected with HCMV (3 PFU/cell), and after 24 h, [3H]thymidine (25 μCi/ml; Amersham) was added. Radiolabeled virus particles were collected from culture supernatants after approximately 6 to 9 days. Cells and debris were removed by sequential centrifugation at 800 × g for 25 min and 8,000 × g for 30 min. Radiolabeled virus particles were concentrated and partially purified by centrifugation at 50,000 × g for 1 h through a 20% sorbitol cushion. Virus pellets were resuspended in DMEM plus 10% FBS. Radioactivity was determined by liquid scintillation, and relative pp65 abundance was determined by Western blotting. Internalization of radiolabeled HCMV particles was measured as described previously (38). Briefly, cells were grown to near confluence in 2-cm2 multiwell culture dishes and cooled to 4°C on ice and radiolabeled particles were added in a total volume of 150 μl. Cultures were centrifuged at 800 × g for 2 h at 4°C, and then unbound virus was removed by washing with cold PBS. Cultures were then shifted to 37°C for various times and then cooled back to 4°C on ice. To remove cell surface virions, cells were then treated for 2 h at 4°C with proteinase K (PK; 2 mg/ml; Fisher Scientific) in PBS or with 2% bovine serum albumin in PBS. The cells were then scraped from wells, pelleted at 1,000 × g for 5 min, and washed with cold PBS, and radioactivity was quantified by liquid scintillation.
HCMV cell-to-cell spread assay.
NHDF and ARPE-19 cells were grown to near confluence on glass coverslips and infected with 20 PFU per well of HCMV. Infected ARPE-19 cells were centrifuged and treated with PEG. Cells were maintained in appropriate media containing 0.3% pooled human immunoglobulin for 21 days and then fixed and analyzed by immunofluorescence for IE86 and HCMV gB.
RESULTS
Construction of a recombinant HCMV lacking epithelial and endothelial cell tropism.
HCMV strain TR was derived from an ocular specimen (54) and, after a very limited number of passages on human fibroblasts, was cloned into a BAC (35). HCMV TR derived from both the original clinical specimen and virus derived from the BAC clone can infect epithelial and endothelial cells much more efficiently than HCMV AD169 or Towne (60; I. Smith, unpublished results; M. Jarvis, unpublished results). TR contains all of the genes UL128 to UL150 (35); however, little is known about the mechanisms by which these genes promote HCMV infection of epithelial or endothelial cells. The goal of our experiments was to determine which stages of HCMV replication were affected in epithelial and endothelial cells when the UL128-to-UL150 genes were deleted. AD169 contains mutations and deletions in this region but also likely harbors mutations elsewhere in the virus genome that may complicate analyses. Therefore, to specifically address the role of the UL128-to-UL150 genes in infection of epithelial and endothelial cells, we produced an HCMV TR UL128-to-UL150 mutant.
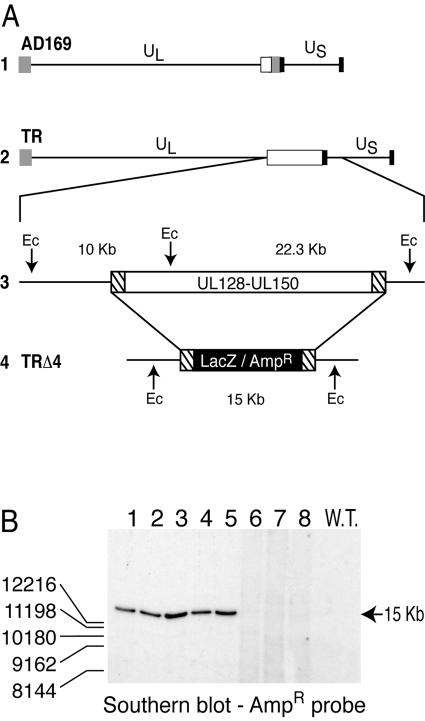
The UL128-to-UL150 genes of TR-BAC were replaced with a β-galactosidase/ampicillin resistance (LacZ/Ampr) gene cassette (refer to Fig. 1). The mutagenesis strategy involved the lambda phage linear recombination machinery (RED locus) of the bacterial host strain EL250 and has been described previously (7, 29, 65). Briefly, the lambda recombination gene products can mediate recombination between the ends of a linear DNA species and homologous sequences within the BAC-cloned HCMV genome. An expression cassette containing the LacZ and Ampr genes flanked by 60 nucleotides of sequences upstream of the UL128 start codon and downstream of the UL150 stop codon was generated by PCR and used to transform recombination-competent bacteria that harbor the HCMV TR-BAC. Transformants were selected for growth on ampicillin, and the resulting clones were screened by restriction digest and Southern blot analysis for correct recombination. The UL128-to-UL150 region of HCMV strain TR spans two EcoRI fragments of 22.3 kb and 10 kb (Fig. 1A, line 3). Replacement of UL128 to UL150 was predicted to remove one EcoRI site and thereby collapse the two fragments into a single 15-kb fragment (Fig. 1A, line 4). Southern blot analysis using a probe specific for the Ampr sequences confirmed the presence of a single insertion of the LacZ/Ampr cassette in the intended location within the genome (on a 15-kb EcoRI fragment) in five of eight clones (Fig. 1B, lanes 1 to 5). Other analyses indicated the absence of the 22- and 10-kb fragments in recombinants 1 to 5 (not shown). Clone 3 was confirmed by sequence analysis, and infectious virus was produced by transfecting human fibroblasts. The resulting UL128-to-UL150 mutant was designated TRΔ4. TR and TRΔ4 produced similar amounts of infectious virus in fibroblasts (not shown); however, less infectious virus was found in culture supernatants with TRΔ4, consistent with a recent report that UL132 functions in virus egress (56).
FIG. 1.
HCMV genome and structure of UL128-to-UL150 mutant TRΔ4. (A, lines 1 and 2) Schematic diagrams of the HCMV AD169 and TR genomes. Indicated are the unique long (UL) and unique short (US) segments and inverted terminal and internal repeats (gray and black rectangles). The open rectangle represents the UL128-to-UL150 genes. AD169 lacks most of the UL128-to-UL150 genes and has mutations in others (35). (Line 3) The UL128-to-UL150 region of the TR genome. Hatched rectangles represent 60-bp sequences used to mediate homologous recombination with TR-BAC sequences. The positions of EcoRI restriction sites (Ec) and the predicted fragment sizes (10 kb and 22.3 kb) are indicated. (Line 4) Schematic diagram of UL128-to-UL150 genes in TRΔ4 replaced with LacZ/Ampr sequences (wide horizontal black rectangle). (B) Southern blot analysis of viral DNA. Eight ampicillin-resistant BAC clones were screened for the replacement of UL128-to-UL150 genes with LacZ/Ampr sequences. DNA was digested with EcoRI and subjected to electrophoresis and Southern blot analysis with a probe directed against Ampr gene sequences. W.T., parental (wild type) TR. A 15-kb fragment was expected for recombinants in which UL128 to UL150 were replaced with LacZ/Ampr sequences.
HCMV lacking the UL128-to-UL150 genes adsorbs or binds poorly onto epithelial cells.
To study the earliest phase of HCMV replication, we characterized adsorption of HCMV onto epithelial cells. Centrifugation of HCMV onto cells enhances infectivity, potentially by increasing adsorption (22). To determine whether centrifugation could increase adsorption of HCMV TR onto epithelial cells, virus radiolabeled with [3H]thymidine was purified from fibroblast cell culture supernatants and then incubated with ARPE-19 epithelial cells in conjunction with centrifugation at 800 × g for 2 h (at 4°C to prevent entry and other processes). Centrifugation consistently increased adsorption or binding of radiolabeled HCMV onto epithelial cells by 5- to 10-fold compared with that onto cells that were not centrifuged (data not shown). For this reason, most other studies utilized centrifugal enhancement.
To compare the adsorption of TR, TRΔ4, and AD169 onto ARPE-19 cells, [3H]thymidine-labeled HCMV virions were partially purified and characterized by immunoblotting for levels of pp65. The specific radioactivities of TRΔ4 and TR were very similar, and AD169 was approximately half that of TR. Radiolabeled particles were centrifuged onto cells at 4°C, the cells were washed extensively, and radioactivity associated with cells was determined. TRΔ4 reproducibly bound at approximately 10% the levels observed for TR, suggesting that at least one of the UL128-to-UL150 genes promotes adsorption to epithelial cells (Table 1, experiment 1). In this experiment, AD169 bound well to epithelial cells (Table 1). In a second experiment, cells were incubated with TRΔ4 that was three times more concentrated (compared with TR) and adsorption was increased to approximately 50% the level observed for TR (Table 1, experiment 2). This indicates that at higher virus doses, or when TRΔ4 particles are more concentrated, adsorption can be enhanced. The observation that AD169 bound better than TR may reflect the fact that AD169 has been extensively passaged in culture and may have acquired compensatory mutations that enhance virus adsorption onto cultured cells. A similar defect in TRΔ4 binding was observed on fibroblasts (not shown). These results suggest that the UL128-to-UL150 gene cluster encodes one or more proteins that increase adsorption of wild-type HCMV onto epithelial cells and fibroblasts.
TABLE 1.
Binding of radiolabeled HCMV strains onto ARPE-19 epithelial cells
Relative specific radioactivity (cpm/units of pp65): TR = 1, TRΔ4 = 1.1, and AD169 = 0.4.
The amount of radiolabeled TR that bound onto cells was arbitrarily set at 100.
Similar quantities of virus, as judged by pp65 content, were incubated with cells.
Three times more TRΔ4 (as judged by pp65) was incubated with cells compared with TR.
ND, not done.
HCMV TRΔ4 and AD169 are defective for entry into epithelial cells.
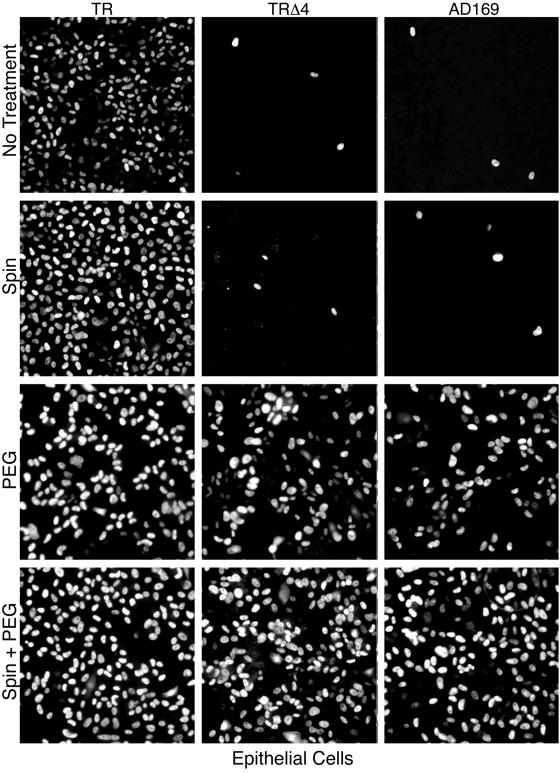
To study entry of HCMV into epithelial cells, 10 PFU/cell of TR, TRΔ4, or AD169 was applied to cells and cultures were either centrifuged or not centrifuged. The percentage of cells infected was then determined by indirect immunofluorescence detection of the HCMV IE86 protein. Without centrifugation, strain TR caused IE expression in 76% of ARPE-19 cells, while TRΔ4 and AD169 infected only 0.5% and 0.8% (Fig. 2 and Table 2). Centrifugation increased infection by TR to 90% and resulted in a 3.6-fold enhancement of infection by TRΔ4 and AD169 so that 1.8 and 2.6% of cells were infected. Therefore, while adsorption was enhanced by centrifugation, the number of cells that were infected by AD169 or TRΔ4, as judged by IE expression, was still dramatically lower than that observed with TR. Given that relatively high input doses of virus were applied to the cells in these experiments, the failure of TRΔ4 and AD169 to induce IE expression was probably not due solely to defects in virus binding or adsorption.
FIG. 2.
Effects of polyethylene glycol and centrifugation on infection of ARPE-19 epithelial cells by HCMV. Replicate cultures of ARPE-19 cells were inoculated with 10 PFU/cell of HCMV strain TR, TRΔ4, or AD169 and were either incubated at room temperature for 2 h or centrifuged at 800 × g at room temperature for 2 h. All cultures were then shifted to 37°C for 2 h and subsequently treated with either PBS or 44% PEG for 30 s. After 48 h, cells were fixed and analyzed by immunofluorescence to detect HCMV IE86. Representative fields are shown.
TABLE 2.
Effects of polyethylene glycol and centrifugation on HCMV infection of ARPE-19 epithelial cells
| Virusa | % IE86 positive (fold increase)b
|
|||
|---|---|---|---|---|
| No treatment | Spin | PEG | Spin + PEG | |
| TR | 76 | 90 (1.18) | 93 (1.22) | 98 (1.28) |
| TRΔ4 | 0.5 | 1.8 (3.6) | 44 (88) | 62 (124) |
| AD169 | 0.8 | 2.6 (3.6) | 38 (47.5) | 70 (87.5) |
Viruses were incubated with cells at 10 PFU/cell.
Ratio of IE86-positive nuclei to DAPI-stained nuclei (n > 650 cells). Values in parentheses represent the fold increase compared to no treatment. “Spin” represents centrifugation of cells and virus at 800 × g for 2 h at room temperature. “PEG” represents treated with 44% PEG for 30 s.
PEG can chemically induce fusion by dehydrating the surfaces of juxtaposed membranes (30). In this way, PEG can force the entry of otherwise entry-defective herpesviruses when adsorbed onto the cell surface (31, 46, 48). To test the hypothesis that AD169 and TRΔ4 are defective for entry on epithelial cells, cells were inoculated with TR, AD169, or TRΔ4, with or without centrifugation, and then subjected to a brief treatment with 44% PEG. As shown in Fig. 2 and Table 2, PEG treatment dramatically increased the number of cells infected with TRΔ4 and AD169 (88- and 47.5-fold, respectively). Centrifugation followed by PEG treatment increased infection by TRΔ4 and AD169 so that 62% and 70% of cells were infected, respectively. These results indicate that there was sufficient TRΔ4 and AD169 absorbed onto the cells to initiate infection when entry was forced with PEG. Furthermore, the dramatic increase in infection by TRΔ4 and AD169 with PEG treatment suggests that these UL128-to-UL150 mutants are defective for entry into epithelial cells.
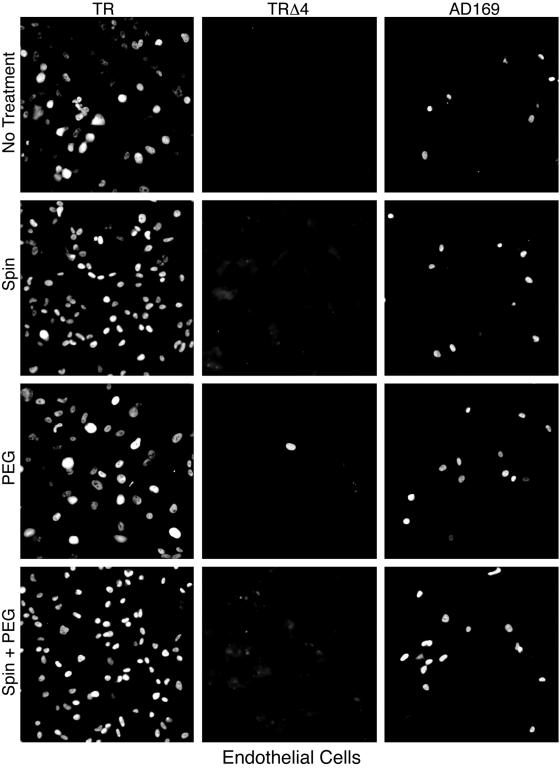
Infection of endothelial cells by HCMV lacking UL128 to UL150 is blocked at postentry stages.
As with epithelial cells, AD169 also poorly infects endothelial cells (17, 20, 60). To characterize entry into endothelial cells and the requirement for the UL128-to-UL150 genes, t-HUVECs were infected with TR, TRΔ4, or AD169 and treated with PEG. Without centrifugal enhancement or PEG treatment, HCMV strain TR infected 85% of endothelial cells while TRΔ4 and AD169 infected less than 1% and 6%, respectively (Fig. 3 and Table 3). Centrifugation alone had no effect on the number of cells infected by either TRΔ4 or AD169 (Fig. 3 and Table 3). PEG treatment, with or without prior centrifugation, had no effect on TRΔ4 infection and only marginally enhanced infection by AD169 (Fig. 3 and Table 3).
FIG. 3.
Effects of polyethylene glycol and centrifugation on infection of t-HUVECs by HCMV. Replicate cultures of t-HUVECs were inoculated with 10 PFU/cell of HCMV strain TR, TRΔ4, or AD169 and subsequently centrifuged as in Fig. 2 and treated with 40% PEG. After 48 h, IE86 was detected by immunofluorescence. Representative fields are shown.
TABLE 3.
Effects of polyethylene glycol and centrifugation on HCMV infection of t-HUVECs
| Virusa | % IE86 positive (fold increase)b
|
|||
|---|---|---|---|---|
| No treatment | Spin | PEG | Spin + PEG | |
| TR | 85.8 | 94.5 (1.1) | 89.5 (1.04) | 95.2 (1.11) |
| TRΔ4 | <1 | <1 (1) | <1 (1) | <1 (1) |
| AD169 | 5.9 | 5.8 (1) | 7.9 (1.34) | 12.7 (2.15) |
Viruses were incubated with cells at 10 PFU/cell.
Ratio of IE86-positive nuclei to DAPI-stained nuclei (n > 450 cells). Values in parentheses represent fold increase compared to no treatment. “Spin” represents centrifugation of cells and virus at 800 × g for 2 h at room temperature. “PEG” represents treated with 40% PEG for 30 s.
Despite the effectiveness of PEG on epithelial cells, it was possible that the PEG treatment failed to cause fusion between HCMV and endothelial cells. To determine if endothelial cells are somehow less sensitive to PEG, an entry-defective HSV mutant was used. The gD gene of HSV vRR1097 was replaced by a gene coding for GFP (44). Glycoprotein D is essential for entry of HSV into all cells characterized to date (57), and PEG has been shown to enhance the infectivity of HSV virions that lack gD (31). Therefore, HUVECs were incubated with vRR1097 (grown on noncomplementing Vero cells) and then centrifuged and treated with 40% PEG. No infected cells (i.e., GFP-expressing cells) were detected in cultures that were not treated with PEG, whereas levels of over 50 infected cells per culture were observed after PEG treatment (data not shown). This indicated that PEG treatment is capable of promoting entry of another herpesvirus into these endothelial cells and, therefore, likely had a similar effect on TRΔ4 entry. From these experiments, the failure of TRΔ4 to enter endothelial cells cannot be excluded. However, since PEG promotes entry and yet did not result in additional IE86 expression by TRΔ4, it appears that the UL128-to-UL150 genes are required for a stage of infection subsequent to entry that could include disassembly of capsids, transport to nuclear pores, release of viral DNA into the nucleus, or IE gene expression.
Internalization of HCMV into epithelial and endothelial cells.
Enveloped viruses reach the cytoplasm by numerous mechanisms, including fusion with the plasma membrane and endocytosis followed by fusion with endosomal membranes (33, 37). PEG essentially bypasses normal entry processes by inducing fusion with the plasma membrane. To more directly follow the internalization of HCMV, [3H]thymidine-labeled virions were purified from fibroblast culture supernatants and adsorbed onto fibroblast, epithelial, or endothelial cells at 4°C to synchronize uptake. Cells were then shifted to 37°C, and after various times, uptake of virus into cells was measured by treating cells with PK to release any cell surface virus. The internalization at any time point was quantified by subtracting the fraction of HCMV that was PK resistant at 0 min (5 to 15%) from the fraction that was PK-resistant virus at that time point. This assay measures only internalization: either fusion with the plasma membrane, endocytosis, or other uptake processes that remove the virus from the cell surface. First, the internalization kinetics of radiolabeled TR particles was compared between fibroblasts and epithelial cells. Fibroblasts internalized more TR than epithelial cells, and in both cases, the internalization began to plateau by 120 min (Fig. 4A). Subsequent experiments compared the fraction of each strain that was internalized after 180 min at 37°C. Approximately 25 to 45% of the cell-bound TR, TRΔ4, and AD169 were internalized into fibroblasts in the 3-h period (Fig. 4B). AD169 was more efficiently internalized into fibroblasts than other viruses. This was not surprising given that AD169 has been propagated extensively on fibroblasts. On epithelial cells, TRΔ4 and AD169 were internalized at least as efficiently as TR, although, for all three viruses, internalization was lower than on fibroblasts (Fig. 4B). This indicates that the UL128-to-UL150 gene products are not required for internalization into epithelial cells. Since IE gene expression was not seen in epithelial cells inoculated with AD169 and TRΔ4 unless PEG was used (Fig. 2 and Table 2), the internalization detected by this assay is not sufficient to initiate infection. If internalization was primarily via fusion at the plasma membrane, both TRΔ4 and AD169 capsids would be expected to enter the cytoplasm and IE gene expression would be expected. More likely, internalization of TRΔ4 and AD169 involves endocytosis that leads to nonproductive infection. This would be similar to the accumulation of HSV virions within endosomes of cells that express gD (expression of gD blocks HSV entry) that was previously described as a dead end pathway (9).
FIG. 4.
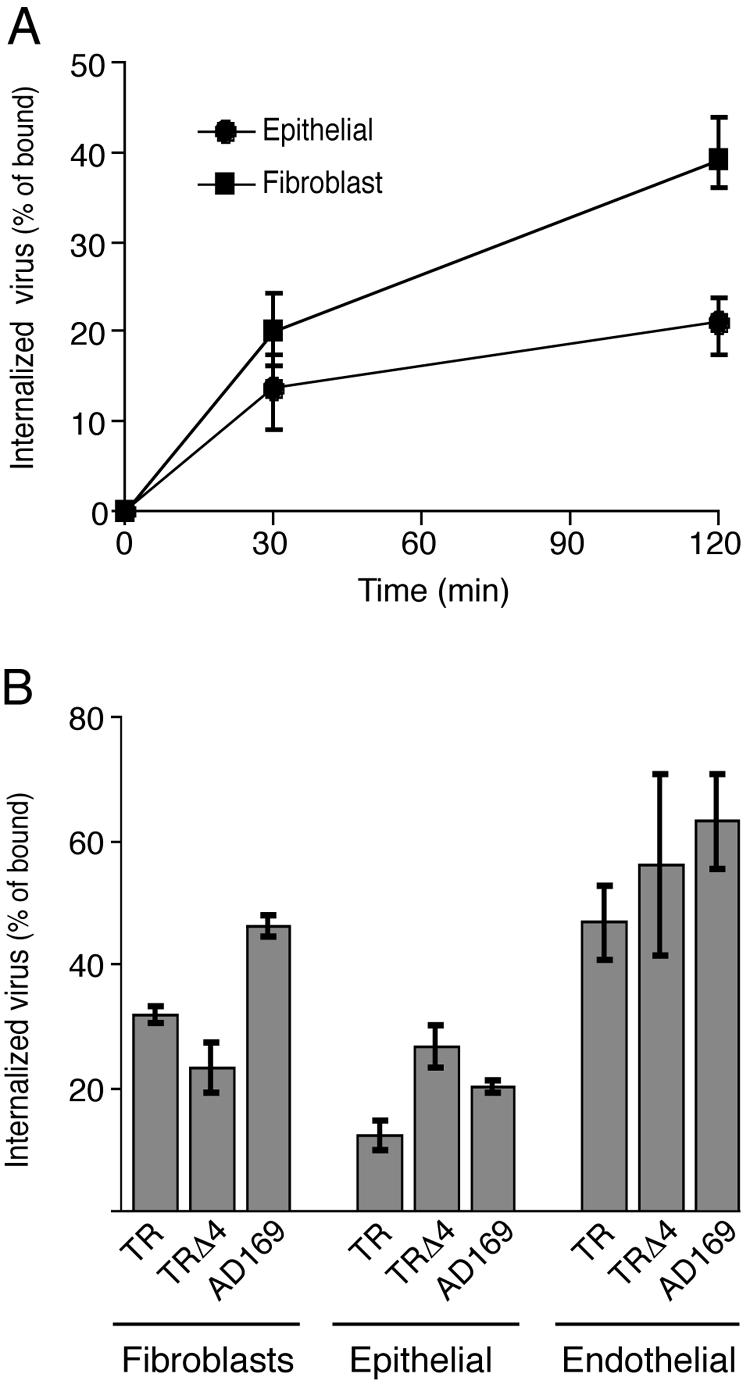
Internalization of radiolabeled HCMV particles. (A) Purified [3H]thymidine-labeled HCMV TR particles were centrifuged onto fibroblasts or epithelial cells at 4°C for 2 h. Cells were washed extensively with PBS and shifted to 37°C for 0, 30, or 120 min. Radiolabeled particles that remained on the cell surface were removed by placing the cells on ice and treating them with PK at 4°C. The internalization of virus was calculated as follows: % of PK-resistant virus after 30 or 120 min (virus remaining with cells after PK treatment/virus remaining with cells not PK treated) − % PK-resistant virus at 0 min (virus remaining with cells after PK treatment at 0 min/virus remaining with cells not PK treated at 0 min). (B) Radiolabeled TR, AD169, or TRΔ4 particles were centrifuged onto fibroblasts, epithelial cells, or endothelial cells at 4°C, and the cells were washed extensively with PBS. Cells were treated with proteinase K immediately or after 3 h at 37°C. Shown is the internalization of virus as described for panel A. Values are the mean of three experiments, and error bars represent standard deviations.
Internalization on endothelial cells was generally more efficient than that on either fibroblasts or epithelial cells, and the levels of internalization were comparable for TR, TRΔ4, and AD169 (Fig. 4B). This indicates that genes in the region of UL128 to UL150 are not required for internalization on endothelial cells. Whether internalization into endothelial cells represents fusion at the plasma membrane or endocytosis, these results are consistent with the previous observation that TRΔ4 and AD169 were blocked at one or more postentry stages of infection that could not be overcome with PEG (Fig. 3and Table 3).
Infection of epithelial and endothelial cells by HCMV requires acidification of endosomes.
Many viruses that are internalized by endocytosis subsequently require the low-pH environment of endosomes to trigger the viral membrane glycoproteins that promote fusion (27, 37). Lysosomotropic agents such as NH4Cl and chloroquine interfere with endosome acidification by buffering endosomal pH, and the drug bafilomycin prevents endosome acidification by poisoning the endosomal ATPase proton pump (5, 18). These agents have been shown to inhibit infection by viruses that require low endosomal pH (21, 32, 33, 37, 64).
To test whether HCMV requires low endosomal pH, fibroblasts, epithelial cells, and endothelial cells were treated with NH4Cl, chloroquine, or bafilomycin during the early stages of infection with HCMV strain TR. To control for toxicity to processes subsequent to virus entry, each agent was added to replicate cultures 4 h after infection. After 20 h (fibroblasts and epithelial cells) or 8 h (endothelial cells), the number of cells expressing IE86 was determined by immunofluorescence. None of the lysosomotropic agents had any detectable inhibitory effect on IE86 expression in fibroblasts (Fig. 5A to C). This is consistent with the previous report that HCMV infects fibroblast cells by pH-independent fusion at the plasma membrane (11). Furthermore, these results indicate that NH4Cl, chloroquine, and bafilomycin do not directly damage HCMV virions and that effects observed on other cell types are likely to result from modification of cellular processes. When added 1 h before and during virus infection, NH4Cl and bafilomycin dramatically reduced the number of IE86-expressing epithelial and endothelial cells (Fig. 5A and B). These drugs had no effect when added 4 h after virus. Treatment with chloroquine produced a similar but less dramatic effect on both epithelial and endothelial cells (Fig. 5C). These results indicate that efficient HCMV infection of epithelial and endothelial cells requires acidification of endosomes.
FIG. 5.
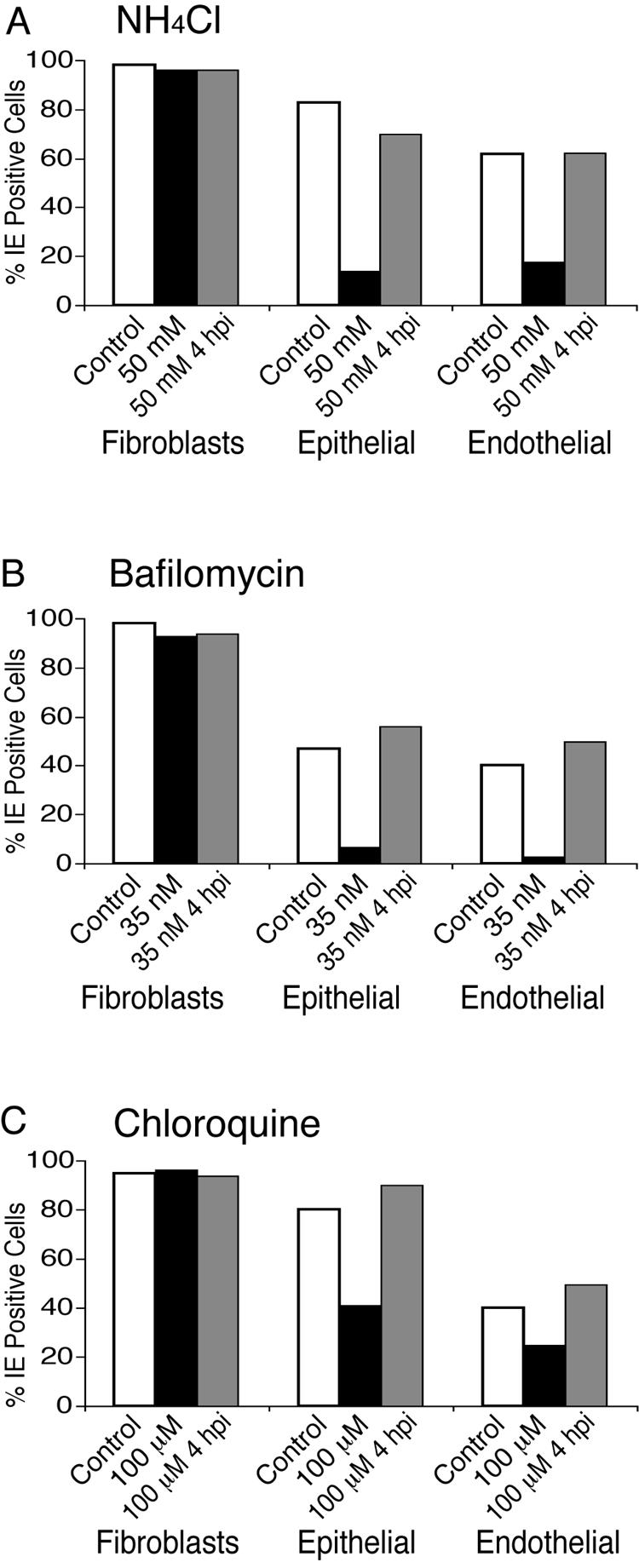
Effects of lysosomotropic agents on HCMV infection of fibroblasts, epithelial cells, and endothelial cells. NHDF, ARPE-19 or t-HUVEC cultures were either not treated (open bars) or treated (black bars) for 1 h with (A) 50 mM NH4Cl, (B) 35 nM bafilomycin, or (C) 100 μM chloroquine and then infected with HCMV TR (5 PFU/cell). hpi, hours postinfection. Alternatively, drugs were added 4 h after the addition of virus (gray bars). After 20 h (fibroblasts and epithelial) or 8 h (endothelial), cells were fixed and analyzed by immunofluorescence for the HCMV IE86 protein and DAPI-stained nuclei. For each condition, at least 350 cells were counted in random fields and the ratio of IE86-positive nuclei to DAPI-positive nuclei was determined. Each experiment was performed at least three times, and representative results are shown.
Mutant HCMVs lacking UL128 to UL150 fail to spread on epithelial cells.
Many herpesviruses are capable of spreading from cell to cell without being released to the extracellular space. Often, these viruses remain attached to one cell while spreading across narrow cell junctions to an adjacent cell (reviewed in reference 24). Spread across cell junctions in epithelial tissues, as well as in cultured epithelial cells, involves processes that mimic entry of extracellular virus, but there can be important differences between these processes. For example, HSV gE/gI functions selectively in cell-to-cell spread and not in entry of extracellular virus (24, 26). In contrast, pseudorabies virus gD is essential for entry of extracellular virus but is not required for cell-to-cell spread, either in cultured cells or in tissues (41, 45).
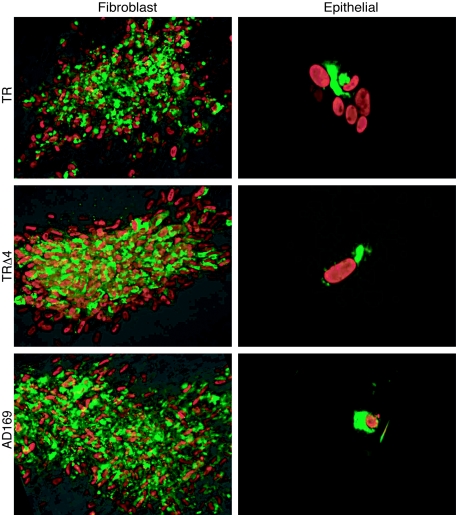
To characterize the role of the UL128-to-UL150 genes in epithelial cell-to-cell spread, ARPE-19 cells were infected with TR, TRΔ4, or AD169 by using centrifugal enhancement and PEG to promote entry. Cultures were then incubated at 37°C for 21 days in the presence of neutralizing antibodies and subsequently analyzed by immunofluorescence for the HCMV proteins IE86 and gB. Expression of gB would suggest that viruses are expressing late-gene products and presumably producing infectious progeny. HCMV TR, TRΔ4, and AD169 spread similarly on fibroblasts, producing robust plaques consisting of more than 300 cells (Fig. 6). Cells at the periphery of each plaque contained only IE86 protein, indicating that they represented an earlier stage of infection than cells nearer the center of the plaques that also expressed gB. When approximately 20 PFU/dish of TR, TRΔ4, and AD169 was applied to ARPE-19 cell monolayers and cells were treated with PEG, there were approximately 60 to 80% the numbers of plaques produced by TRΔ4 and AD169 compared with wild-type TR, similar to the entry observed in high-multiplicity-of-infection experiments. However, spread of TRΔ4 to adjacent epithelial cells was never observed; only single infected cells that expressed both IE86 and gB were detected (Fig. 6). By comparison, TR spread to approximately 5 to 10 cells during 21 days. As on fibroblasts, gB was detected primarily in ARPE-19 cells toward the center of the plaques, indicating outward virus spread. AD169 also largely failed to spread to adjacent epithelial cells in these experiments. This was somewhat different from earlier results in which single infected cells and small foci were observed with AD169 on ARPE-19 cells (22). In these previous experiments, the cells were pretreated with neuraminidase, which may have promoted plaque formation and spread. Alternatively, AD169 may be intermediate between TR and TRΔ4. However, comparison of TR and TRΔ4 suggests that wild-type HCMV relies on one or more of the UL128-to-UL50 genes for cell-to-cell spread between cultured epithelial cells.
FIG. 6.
Plaque formation by HCMV on fibroblasts and epithelial cells. Fibroblasts or ARPE-19 epithelial cells were infected with HCMV strain TR, AD169, or TRΔ4 at approximately 20 PFU/well, and the cells and virus were centrifuged at 800 × g for 2 h at room temperature. The epithelial cells were then treated briefly with 44% PEG. All cultures were incubated at 37°C in the presence of neutralizing antibody for 21 days, fixed, and analyzed by immunofluorescence for HCMV IE86 protein (red) and gB (green). Representative fields are shown. The magnification of the panels showing epithelial cells was three times greater than that for fibroblasts.
DISCUSSION
The ability of HCMV to replicate and spread in diverse cell types and tissues is important in the pathology and epidemiology of HCMV diseases. However, knowledge of the mechanisms by which HCMV infects and replicates in several relevant cell types is lacking. This is largely due to the fact that commonly studied laboratory strains of HCMV (e.g., AD169 and Towne) do not efficiently infect epithelial cells, endothelial cells, or monocytes/macrophages. Furthermore, many of the HCMV mutants available were derived from laboratory strains, adding to the difficulty of studying infection of these relevant cell types. The limited host cell range of AD169 and other laboratory strains is apparently due to a subset of the genetic mutations that have accumulated during extensive propagation on fibroblasts. Recently, certain clinical strains (including TR and FIX) have been frozen as BAC clones, and these viruses retain the capacity to infect endothelial and epithelial cells, as well as monocytes/macrophages (19, 35; D. Streblow and J. Nelson, unpublished results). There is obviously considerable interest in identifying the gene or genes that differ between laboratory and clinical strains and which mediate infection of these cell types. The genes in the UL128-to-UL150 region have been the focus of several studies of HCMV infection of endothelial and epithelial cells, but molecular mechanisms of how these viral genes function have, by and large, not yet been reported.
Here we focused on early stages in HCMV replication in epithelial and endothelial cells and investigated the role of the UL128-to-UL150 genes in adsorption and entry into these cells. Our experiments showed that the UL128-to-UL150 mutant, TRΔ4, adsorbed onto epithelial cells poorly compared to wild-type TR. Furthermore, at relatively high multiplicities of infection, TRΔ4 infected less than 2% of epithelial cells (as determined by IE protein expression), whereas wild-type TR infected over 90% of these cells. This is consistent with our previous observations that AD169 infected epithelial cells poorly and that infection was somewhat enhanced by centrifugation and neuraminidase treatment (22). Here we showed that when virus entry into epithelial cells was “forced” with the chemical fusogen PEG, TRΔ4 and AD169 infected up to 70% of cells, leading to IE and gB expression. These observations demonstrated that there was sufficient TRΔ4 adsorbed onto cells that most cells expressed the IE gene after PEG treatment. Moreover, the results showed that the UL128-to-UL150 genes are required for entry of HCMV into epithelial cells at a stage subsequent to adsorption. Once entry occurred through PEG-induced fusion, the HCMV UL128-to-UL150 mutant had the capacity to undergo postentry processes: i.e., capsid disassembly, translocation to the nucleus, and gene expression. However, in what could be misinterpreted as confounding observations, radiolabeled TRΔ4 and AD169 were internalized into epithelial cells as efficiently as TR. The simplest explanation for this is that HCMV is taken up by endocytosis and that productive entry occurs by fusion of the virion envelope with endosomal membranes. Thus, in the case of TRΔ4 and AD169, substantial amounts of virus were taken up by cells, as measured by the internalization assay, yet there was a failure of virus to enter cells presumably by fusion with endosomes. Data shown in Fig. 4 indicate that endocytosis is not complete since substantial amounts of radiolabeled virus remain on the cell surface even after 3 h. Therefore, treatment with PEG would be expected to overcome defects in endocytosis or fusion with endosomal membranes by forcing entry of those HCMV particles that remain on the cell surface.
We also observed that drugs that raise endosomal pH (NH4Cl, chloroquine, or bafilomycin) inhibited infection of epithelial cells by wild-type HCMV. Together, these results strongly support the hypothesis that HCMV enters epithelial cells by endocytosis and low-pH-dependent fusion with endosomal membranes. It is possible, although unlikely, that HCMV entry into epithelial cells can also involve fusion with the plasma membrane. In this case, the internalization assay might follow uptake of a subpopulation of virus particles into a nonproductive pathway. However, this is unlikely given the dependence of HCMV entry on low pH. These results argue that one or more UL128-to-UL150 genes promote entry at endosomes. One likely candidate is UL131, which was recently shown to increase infectivity of AD169 in ARPE-19 epithelial cells (60).
It is possible that AD169 and TRΔ4 possess mutations that reduce virus replication in epithelial cells at stages subsequent to IE and gB expression. It might be possible to address this by measuring infectious virus yield after forcing HCMV into epithelial cells with PEG. However, this approach has a significant drawback. The percentage of cells infected by TRΔ4 after PEG treatment was 60% to 70%, compared with 98% for TR. Therefore, cells would not be synchronously infected and comparison of virus yield would be difficult. It is also possible that the construction of TRΔ4 produced secondary mutations outside of the UL128-to-UL150 region, and one could imagine that these secondary mutations could affect entry. However, AD169 (which also lacks the UL128-to-UL150 genes) behaved similarly or identically in entering epithelial cells; PEG increased IE expression by a similar amount. It is difficult to imagine that TRΔ4, which was constructed by using the high-fidelity BAC system, could have acquired identical secondary mutations (outside the UL128-to-UL150 region) as are present in AD169. Our principal conclusion involving TRΔ4 was restricted to the notion that the UL128-to-UL150 genes play a role in entry. There may be other differences between AD169 and TRΔ4, but this conclusion is well substantiated without a rescued version of the UL128-to-UL150 mutant by the similar phenotype of AD169 and reversal by PEG experiments.
Endothelial cells were also efficiently infected by HCMV TR but not by AD169 or TRΔ4. In contrast to the results with epithelial cells, PEG treatment did not substantially increase the number of endothelial cells infected by AD169 or TRΔ4. Here again, radiolabeled particles of all three strains were internalized with similar efficiencies. These results, coupled with the observations that infection of endothelial cells by TR was inhibited by NH4Cl, bafilomycin, and chloroquine, support the hypothesis that HCMV enters endothelial cells through endocytosis followed by fusion with endosomal membranes. Furthermore, since PEG did not substantially increase infection by TRΔ4 or AD169, it is likely that HCMV UL128-to-UL150 genes are necessary for some stage of endothelial cell infection subsequent to entry but before gene expression. These postentry steps may include translocation of the nucleocapsid to the nucleus, capsid disassembly, release of the genome across the nuclear pore, or immediate-early transcription and translation. Our results are consistent with previous reports that AD169 and other nonendotheliotropic HCMV strains accumulate in the cytoplasm of endothelial cells and that viral DNA is poorly translocated into the nucleus (52, 53). The observed accumulation of virion components in the cytoplasm (52) could relate to a lack of fusion with endosomal membranes, so that enveloped virions build up in endosomal compartments, rather than in the cytoplasm. Our observations that PEG did not promote infection of endothelial cells by TRΔ4 or AD169 suggest that some step subsequent to entry is also blocked, although it is likely that there are also defects in entry into these cells. UL128-to-UL150 mutants may have multiple defects in initiating infection in endothelial cells. The UL130 and UL132 proteins are virion components (40, 56, 59) and, along with UL131, are good candidates for proteins that might promote entry or an early replication step in endothelial cells. Experiments are in progress to identify the specific UL128-to-UL150 proteins that facilitate infection of endothelial cells.
Endocytosis of HCMV particles by endothelial and epithelial cells was previously observed by electron microscopy (3). However, as with many electron microscopy experiments, the biologic relevance of these observations was not clear, especially since the particle/PFU ratio of AD169 has been estimated to be as high as 490 (1). Moreover, these authors reported that treating the cells with NH4Cl or chloroquine had only marginal effects on the number of cells infected (3). However, since they also observed inefficient infection of endothelial and epithelial cells by AD169, even in the absence of drug, the observed entry may not reflect the major pathway of HCMV entry.
Our conclusions that HCMV enters epithelial and endothelial cells by endocytosis followed by low-pH-dependent fusion, combined with earlier observations that HCMV enters fibroblasts by plasma membrane fusion (11), fit well with observations involving gamma- and alphaherpesviruses. Miller and Hutt-Fletcher showed that EBV enters normal B cells by endocytosis and pH-independent fusion, but infects Raji-transformed B cells and epithelial cells by direct fusion with the plasma membrane (33). Similarly, HSV can enter different cells by (i) direct fusion with the plasma membrane, (ii) endocytosis and low-pH-dependent fusion, or (iii) endocytosis and pH-independent fusion (34, 36, 37, 63). Thus, herpesviruses have adapted to different cells through a variety of different entry pathways. For EBV, there is good evidence that different envelope glycoproteins can function in entry into different cell types (4). This may also be the case for HCMV, a virus that infects many different cell types and that has more coding capacity to dedicate to different host cells. However, our knowledge of HCMV entry is still relatively rudimentary when compared with that of alpha- or gammaherpesviruses because there are few viral mutants.
Efficient cell-to-cell transmission of HCMV is likely important to allow virus spread in solid tissues, dissemination to other tissues, and avoidance of the host immune system. Herpesvirus cell-to-cell spread is a process that frequently involves proteins necessary for entry of extracellular virions, but there are also differences between these processes. The best examples are HSV gE/gI, which functions in spread, but not in entry, and PRV gD, which is essential for entry but is not needed for spread (reviewed in reference 24). HCMV replicates in several tissues that contain polarized cells that form extensive intercellular junctions. Thus, it is likely that progeny HCMVs are directed to cell junctions and are capable of crossing junctions efficiently. Recently, HCMV cell-to-cell spread was found to occur with a mutant unable to produce detectable extracellular virions (51). We found here that HCMVs lacking the UL128-to-UL150 genes could not spread between epithelial cells. The initial defect of entry of TRΔ4 and AD169 into these epithelial cells could be overcome by using PEG, and yet only single infected cells expressing both IE86 and gB were detected and there was no spread of TRΔ4 to adjacent cells. Wild-type TR replicated slowly in these cells and spread to 5 to 10 cells over 21 days. The inability of TRΔ4 and AD169 to spread in epithelial cells probably reflects the defect in entry, as most often herpesviruses that fail to enter also fail to spread. This is consistent with the notion that enveloped particles (which are capable of entry) are necessary in order for virus to spread between cells and that nucleocapsids are insufficient. However, it is also possible that TRΔ4 has other defects that affect replication in epithelial cells, including slower viral gene expression (although gB was produced) or defects in DNA replication, assembly, or egress.
In summary, we have shown that HCMV enters epithelial and endothelial cells by endocytosis followed by low-pH-dependent fusion with endosomes. HCMV UL128-to-UL150 mutants infected epithelial cells poorly, although virions were internalized, suggesting that one or more of the UL128-to-UL150 genes are required for fusion with endosomal membranes. With endothelial cells, PEG did not overcome the deletion of UL128-to-UL150 genes, supporting the hypothesis of other defects at postentry stages of early replication.
Acknowledgments
This work was supported by grants from the National Institutes of Health (NEI-EY11245 and NIAID-AI73996 to D.C.J. and AI21640 to J.A.N. and M.A.J.). B.J.R. was supported by a Ruth L. Kirschstein National Research Service Award from the NEI (F32-EY015965-02).
We are most grateful to Irene Smith for her discovery of HCMV TR, early observations that TR infected epithelial and endothelial cells well, and advice on our experiments. We also thank Richard Roller for advice on the use of polyethylene glycol, Don Court for the EL250 BAC host strain, Tiffani Howard for computer graphics, Barb Rainish for technical assistance in the latter stages of the experiments, and Jeff Vandehey for help with online manuscript submission. Finally, we appreciate the support and advice of all the members of the Johnson and Nelson laboratories.
REFERENCES
- 1.Benyesh-Melnick, M., F. Probstmeyer, R. McCombs, J. P. Brunschwig, and V. Vonka. 1966. Correlation between infectivity and physical virus particles in human cytomegalovirus. J. Bacteriol. 92:1555-1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bissinger, A. L., C. Sinzger, E. Kaiserling, and G. Jahn. 2002. Human cytomegalovirus as a direct pathogen: correlation of multiorgan involvement and cell distribution with clinical and pathological findings in a case of congenital inclusion disease. J. Med. Virol. 67:200-206. [DOI] [PubMed] [Google Scholar]
- 3.Bodaghi, B., M. E. P. Slobbe-Vandrunen, A. Topilko, E. Perret, R. C. R. M. Vossen, M. C. E. Van Dam-Mieras, D. Zipeto, J.-L. Virelizier, P. Lehoang, C. A. Bruggeman, and S. Michelson. 1999. Entry of human cytomegalovirus into retinal pigment epithelial and endothelial cells by endocytosis. Investig. Ophthalmol. Vis. Sci. 40:2598-2607. [PubMed] [Google Scholar]
- 4.Borza, C. M., and L. M. Hutt-Fletcher. 2002. Alternate replication in B cells and epithelial cells switches tropism of Epstein-Barr virus. Nat. Med. 8:594-599. [DOI] [PubMed] [Google Scholar]
- 5.Bowman, E. J., A. Siebers, and K. Altendorf. 1988. Bafilomycins: a class of inhibitors of membrane ATPases from microorganisms, animal cells, and plant cells. Proc. Natl. Acad. Sci. USA 85:7972-7976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Britt, W. J., and C. A. Alford. 1996. Cytomegaloviruses, p. 2493-2523. In B. N. Fields, D. M. Knipe, and P. M. Howley (ed.), Fields virology, 3rd ed. Lippincott-Raven Press, Philadelphia, Pa.
- 7.Britt, W. J., M. Jarvis, J.-Y. Seo, D. Drummond, and J. Nelson. 2004. Rapid genetic engineering of human cytomegalovirus by using a lambda phage linear recombination system: demonstration that pp28 (UL99) is essential for production of infectious virus. J. Virol. 78:539-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cai, W. H., B. Gu, and S. Person. 1988. Role of glycoprotein B of herpes simplex virus type 1 in viral entry and cell fusion. J. Virol. 62:2596-2604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campadelli-Fiume, G., M. Arsenakis, F. Farabegoli, and B. Roizman. 1988. Entry of herpes simplex virus 1 in BJ cells that constitutively express viral glycoprotein D is by endocytosis and results in degradation of the virus. J. Virol. 62:159-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cha, T.-A., E. Tom, G. W. Kemble, G. M. Duke, E. S. Mocarski, and R. R. Spaete. 1996. Human cytomegalovirus clinical isolates carry at least 19 genes not found in laboratory strains. J. Virol. 70:78-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Compton, T., R. R. Nepomuceno, and D. M. Nowlin. 1992. Human cytomegalovirus penetrates host cells by pH-independent fusion at the cell surface. Virology 191:387-395. [DOI] [PubMed] [Google Scholar]
- 12.Compton, T., D. M. Nowlin, and N. R. Cooper. 1993. Initiation of human cytomegalovirus infection requires initial interaction with cell surface heparan sulfate. Virology 193:834-841. [DOI] [PubMed] [Google Scholar]
- 13.Dolan, A., C. Cunningham, R. D. Hector, A. F. Hassan-Walker, L. Lee, C. Addison, D. J. Dargan, D. J. McGeoch, D. Gatherer, V. C. Emery, P. D. Griffiths, C. Sinzger, B. P. McSharry, G. W. G. Wilkinson, and A. J. Davison. 2004. Genetic content of wild-type human cytomegalovirus. J. Gen. Virol. 85:1301-1312. [DOI] [PubMed] [Google Scholar]
- 14.Feire, A. L., H. Koss, and T. Compton. 2004. Cellular integrins function as entry receptors for human cytomegalovirus via a highly conserved disintegrin-like domain. Proc. Natl. Acad. Sci. USA 101:15470-15475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forrester, A., H. Farrell, G. Wilkinson, J. Kaye, N. Davis-Poynter, and T. Minson. 1992. Construction and properties of a mutant of herpes simplex virus type 1 with glycoprotein H coding sequences deleted. J. Virol. 66:341-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gerna, G., F. Baldanti, and M. G. Revello. 2004. Pathogenesis of human cytomegalovirus infection and cellular targets. Hum. Immunol. 65:381-386. [DOI] [PubMed] [Google Scholar]
- 17.Gerna, G., E. Percivalle, A. Sarasini, F. Baldanti, G. Campanini, and M. G. Revello. 2003. Rescue of human cytomegalovirus strain AD169 tropism for both leukocytes and human endothelial cells. J. Gen. Virol. 84:1431-1436. [DOI] [PubMed] [Google Scholar]
- 18.Guinea, R., and L. Carrasco. 1995. Requirement for vacuolar proton-ATPase activity during entry of influenza virus into cells. J. Virol. 69:2306-2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hahn, G., H. Khan, F. Baldanti, U. H. Koszinowski, M. G. Revello, and G. Gerna. 2002. The human cytomegalovirus ribonucleotide reductase homolog UL45 is dispensable for growth in endothelial cells, as determined by a BAC-cloned clinical isolate of human cytomegalovirus with preserved wild-type characteristics. J. Virol. 76:9551-9555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hahn, G., M. G. Revello, M. Patrone, E. Percivalle, G. Campanini, A. Sarasini, M. Wagner, A. Gallina, G. Milanesi, U. Koszinowski, F. Baldanti, and G. Gerna. 2004. Human cytomegalovirus UL131-128 genes are indispensable for virus growth in endothelial cells and virus transfer to leukocytes. J. Virol. 78:10023-10033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helenius, A., J. Kartenbeck, K. Simons, and E. Fries. 1980. On the entry of Semliki forest virus into BHK-21 cells. J. Cell Biol. 84:404-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huber, M. T., R. Tomazin, T. Wisner, J. Boname, and D. C. Johnson. 2002. Human cytomegalovirus US7, US8, US9, and US10 are cytoplasmic glycoproteins, not found at cell surfaces, and US9 does not mediate cell-to-cell spread. J. Virol. 76:5748-5758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jarvis, M. A., C. E. Wang, H. L. Meyers, P. P. Smith, C. L. Corless, G. J. Henderson, J. Vieira, W. J. Britt, and J. A. Nelson. 1999. Human cytomegalovirus infection of Caco-2 cells occurs at the basolateral membrane and is differentiation state dependent. J. Virol. 73:4552-4560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson, D. C., and M. T. Huber. 2002. Directed egress of animal viruses promotes cell-to-cell spread. J. Virol. 76:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson, D. C., and M. W. Ligas. 1988. Herpes simplex viruses lacking glycoprotein D are unable to inhibit virus penetration: quantitative evidence for virus-specific cell surface receptors. J. Virol. 62:4605-4612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson, D. C., M. Webb, T. W. Wisner, and C. Brunetti. 2002. Herpes simplex virus gE/gI sorts nascent virions to epithelial cell junctions, promoting virus spread. J. Virol. 75:821-833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lakadamyali, M., M. J. Rust, and X. Zhuang. 2004. Endocytosis of influenza viruses. Microbes Infect. 6:929-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landolfo, S., M. Gariglio, G. Gribaudo, and D. Lembo. 2003. The human cytomegalovirus. Pharmacol. Ther. 98:269-297. [DOI] [PubMed] [Google Scholar]
- 29.Lee, E. C., D. Yu, J. Martinez De Velasco, L. Tessarollo, D. A. Swing, D. L. Court, N. A. Jenkins, and N. G. Copeland. 2001. A highly efficient Escherichia coli-based chromosome engineering system adapted for recombinogenic targeting and subcloning of BAC DNA. Genomics 73:56-65. [DOI] [PubMed] [Google Scholar]
- 30.Lentz, B. R., and J. K. Lee. 1999. Poly(ethylene glycol) (PEG)-mediated fusion between pure lipid bilayers: a mechanism in common with viral fusion and secretory vesicle release? Mol. Membr. Biol. 16:279-296. [DOI] [PubMed] [Google Scholar]
- 31.Ligas, M. W., and D. C. Johnson. 1988. A herpes simplex virus mutant in which glycoprotein D sequences are replaced by β-galactosidase sequences binds to but is unable to penetrate into cells. J. Virol. 62:1486-1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matlin, K. S., H. Reggio, A. Helenius, and K. Simons. 1982. Pathway of vesicular stomatitis virus entry leading to infection. J. Mol. Biol. 156:609-631. [DOI] [PubMed] [Google Scholar]
- 33.Miller, N., and L. M. Hutt-Fletcher. 1992. Epstein-Barr virus enters B cells and epithelial cells by different routes. J. Virol. 66:3409-3414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Milne, R. S. B., A. V. Nicola, J. C. Whitbeck, R. J. Eisenberg, and G. H. Cohen. 2005. Glycoprotein D receptor-dependent, low-pH-independent endocytic entry of herpes simplex virus type 1. J. Virol. 79:6655-6663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murphy, E., D. Yu, J. Grimwood, J. Schmutz, M. Dickson, M. A. Jarvis, G. Hahn, J. A. Nelson, R. M. Myers, and T. E. Shenk. 2003. Coding potential of laboratory and clinical strains of human cytomegalovirus. Proc. Natl. Acad. Sci. USA 100:14976-14981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nicola, A. V., J. Hou, E. O. Major, and S. E. Straus. 2005. Herpes simplex virus type 1 enters human epidermal keratinocytes, but not neurons, via a pH-dependent endocytic pathway. J. Virol. 79:7609-7616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nicola, A. V., A. M. McEvoy, and S. E. Straus. 2003. Roles for endocytosis and low pH in herpes simplex virus entry into HeLa and Chinese hamster ovary cells. J. Virol. 77:5324-5332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nicola, A. V., and S. E. Straus. 2004. Cellular and viral requirements for rapid endocytic entry of herpes simplex virus. J. Virol. 78:7508-7517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ogawa-Goto, K., K. Tanaka, W. Gibson, E. Moriishi, Y. Miura, T. Kurata, S. Irie, and T. Sata. 2003. Microtubule network facilitates nuclear targeting of human cytomegalovirus capsid. J. Virol. 77:8541-8547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patrone, M., M. Secchi, L. Fiorina, M. Ierardi, G. Milanesi, and A. Gallina. 2005. Human cytomegalovirus UL130 protein promotes endothelial cell infection through a producer cell modification of the virion. J. Virol. 79:8361-8373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peeters, B., J. Pol, A. Gielkens, and R. Moormann. 1993. Envelope glycoprotein gp50 of pseudorabies virus is essential for virus entry but is not required for viral spread in mice. J. Virol. 67:170-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Plachter, B., C. Sinzger, and G. Jahn. 1996. Cell types involved in replication and distribution of human cytomegalovirus. Adv. Virus Res. 46:195-261. [DOI] [PubMed] [Google Scholar]
- 43.Prichard, M. N., M. E. Penfold, G. M. Duke, R. R. Spaete, and G. W. Kemble. 2001. A review of genetic differences between limited and extensively passaged human cytomegalovirus strains. Rev. Med. Virol. 11:191-200. [DOI] [PubMed] [Google Scholar]
- 44.Rauch, D. A., N. Rodriguez, and R. J. Roller. 2000. Mutations in herpes simplex virus glycoprotein D distinguish entry of free virus from cell-cell spread. J. Virol. 74:11437-11446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rauh, I., and T. C. Mettenleiter. 1991. Pseudorabies virus glycoproteins gII and gp50 are essential for virus penetration. J. Virol. 65:5348-5356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roller, R. J., and B. Roizman. 1994. A herpes simplex virus 1 US11-expressing cell line is resistant to herpes simplex virus infection at a step in viral entry mediated by glycoprotein D. J. Virol. 68:2830-2839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roop, C., L. Hutchinson, and D. C. Johnson. 1993. A mutant herpes simplex virus type 1 unable to express glycoprotein L cannot enter cells, and its particles lack glycoprotein H. J. Virol. 67:2285-2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sarmiento, M., M. Haffey, and P. G. Spear. 1979. Membrane proteins specified by herpes simplex viruses. III. Role of glycoprotein VP7(B2) in virion infectivity. J. Virol. 29:1149-1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Scholz, M., H. W. Doerr, and J. Cinatl. 2003. Human cytomegalovirus retinitis: pathogenicity, immune evasion and persistence. Trends Microbiol. 11:171-178. [DOI] [PubMed] [Google Scholar]
- 50.Shukla, D., and P. G. Spear. 2001. Herpesviruses and heparan sulfate: an intimate relationship in aid of viral entry. J. Clin. Investig. 108:503-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Silva, M. C., J. Schroer, and T. Shenk. 2005. Human cytomegalovirus cell-to-cell spread in the absence of an essential assembly protein. Proc. Natl. Acad. Sci. USA 102:2081-2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sinzger, C., M. Kahl, K. Laib, K. Klingel, P. Rieger, B. Plachter, and G. Jahn. 2000. Tropism of human cytomegalovirus for endothelial cells is determined by a post-entry step dependent on efficient translocation to the nucleus. J. Gen. Virol. 81:3021-3035. [DOI] [PubMed] [Google Scholar]
- 53.Slobbe-Van Drunen, M. E., A. T. Hendrickx, R. C. Vossen, E. J. Speel, M. C. Van Dam-Mieras, and C. A. Bruggeman. 1998. Nuclear import as a barrier to infection of human umbilical vein endothelial cells by human cytomegalovirus strain AD169. Virus Res. 56:149-156. [DOI] [PubMed] [Google Scholar]
- 54.Smith, I. L., I. Taskintuna, F. M. Rahhal, H. C. Powell, E. Ai, A. J. Mueller, S. A. Spector, and W. R. Freeman. 1998. Clinical failure of CMV retinitis with intravitreal cidofovir is associated with antiviral resistance. Arch. Ophthalmol. 116:178-185. [DOI] [PubMed] [Google Scholar]
- 55.Smith, M. S., G. L. Bentz, J. S. Alexander, and A. D. Yurochko. 2004. Human cytomegalovirus induces monocyte differentiation and migration as a strategy for dissemination and persistence. J. Virol. 78:4444-4453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Spaderna, S., B. Kropff, Y. Ködel, S. Shen, S. Coley, S. Lu, W. Britt, and M. Mach. 2005. Deletion of gpUL132, a structural component of human cytomegalovirus, results in impaired virus replication in fibroblasts. J. Virol. 79:11837-11847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Spear, P. G., and R. Longnecker. 2003. Herpesvirus entry: an update. J. Virol. 77:10179-10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Streblow, D. N., S. L. Orloff, and J. A. Nelson. 2001. Do pathogens accelerate atherosclerosis? J. Nutr. 131:2798S-2804S. [DOI] [PubMed] [Google Scholar]
- 59.Varnum, S. M., D. N. Streblow, M. E. Monroe, P. Smith, K. J. Auberry, L. Paša-Tolić, D. Wang, D. G. Camp II, K. Rodland, S. Wiley, W. Britt, T. Shenk, R. D. Smith, and J. A. Nelson. 2004. Identification of proteins in human cytomegalovirus (HCMV) particles: the HCMV proteome. J. Virol. 78:10960-10966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang, D., and T. Shenk. 2005. Human cytomegalovirus UL131 open reading frame is required for epithelial cell tropism. J. Virol. 79:10330-10338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang, X., D. Y. Huang, S. M. Huong, and E. S. Huang. 2005. Integrin alphavbeta3 is a coreceptor for human cytomegalovirus. Nat. Med. 11:515-521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang, X., S. M. Huong, M. L. Chiu, N. Raab-Traub, and E. S. Huang. 2003. Epidermal growth factor receptor is a cellular receptor for human cytomegalovirus. Nature 424:456-461. [DOI] [PubMed] [Google Scholar]
- 63.Wittels, M., and P. G. Spear. 1991. Penetration of cells by herpes simplex virus does not require a low pH-dependent endocytic pathway. Virus Res. 18:271-290. [DOI] [PubMed] [Google Scholar]
- 64.Yoshimura, A., K. Kuroda, K. Kawasaki, S. Yamashina, T. Maeda, and S. Ohnishi. 1982. Infectious cell entry mechanism of influenza virus. J. Virol. 43:284-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yu, D., H. M. Ellis, E. C. Lee, N. A. Jenkins, N. G. Copeland, and D. L. Court. 2000. An efficient recombination system for chromosome engineering in Escherichia coli. Proc. Natl. Acad. Sci. USA 97:5978-5983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhou, Y. F., M. B. Leon, M. A. Waclawiw, J. J. Popma, Z. X. Yu, T. Finkel, and S. E. Epstein. 1996. Association between prior cytomegalovirus infection and the risk of restenosis after coronary atherectomy. N. Engl. J. Med. 335:624-630. [DOI] [PubMed] [Google Scholar]