Abstract
A nonexperimental study with a sample of 95 preterm infants was used to develop a model of feeding performance outcomes (proficiency, percent of prescribed volume consumed, and efficiency) using feeding readiness indicators (morbidity, maturity, behavior state at feeding start, and feeding experience). All readiness indicators were related to each other. In particular, there was a strong relationship between maturity and feeding experience. Morbidity only had an effect on efficiency; the most ill infants were less efficient feeders. Behavior state affects all feeding outcomes in a linear fashion; more awake and alert infants had better feeding performance outcomes. The effect of experience and maturity on the outcomes is more complex because of the relationship between the two. Experience has a greater effect as the infant matures, and as the infant matures, the amount of experience increases. Successful feeding requires maturity as well as experience.
Once physiological stability has been attained, a major challenge for preterm infants is achievement of oral feeding competence. Although breast-feeding may present fewer physiological challenges to the growing preterm infant,1,2 many preterm infants are bottle-fed either formula or expressed breast milk.3 For the bottle-fed infant, feeding competence is the achievement of total or complete oral feedings. The American Academy of Pediatrics has included competency at nipple-feeding, either breast or bottle, as a criterion for preterm infant readiness for hospital discharge.4 Achieving competence at this important task takes time, with the transition from gavage to full bottle-feedings reported to last 10 to 14 days.5 Longer transition to full bottle-feedings has been associated with increased length of hospital stay.6
Assisting the preterm infant achieve bottle-feeding competence is a primary responsibility of the nursing staff.7 Despite this responsibility, there continues to be a paucity of information available to support nurses in their decision making regarding preterm infant feeding. In particular, although the mechanics of bottle-feeding have been studied extensively,8,9 there is very little research on the predictors of feeding performance.10 Conventional wisdom in many nurseries follows numerous reports that safe bottle-feeding is dependent on suck-swallow-breathe coordination, which is reported to occur approximately 34 weeks postconceptional age (PCA).8,11,12 However, suck-swallow-breathe coordination has not been correlated with actual feeding performance.13 Moreover, few nurseries have specific policies governing the initiation or progression of bottle-feedings.7,14 Rather, the decision to offer a bottle-feeding is often made subjectively by the bedside nurse based on clinical judgement of certain parameters, including behavior state, PCA, and presence of complicating disorders. Although these parameters have been associated with decisions about feeding modality, the relationships among these parameters and actual feeding performance remain largely unexplored. Furthermore, little is known about the effect that feeding experience, in the form of feeding opportunities, may have on feeding performance. In fact, the contribution of feeding experience to the transition to full oral feeding has rarely been examined.6,15-18
Oral feeding practices, that is, when bottle-feedings are started and on what schedule they are provided, are highly variable. A national survey of neonatal intensive care unit feeding practices revealed no consistent criteria for the initiation of oral feeding and no organized protocol for oral feeding progression.19 Once oral feedings are initiated, a common but untested practice is to start with one oral feeding attempt per day and gradually, but arbitrarily, increase oral offerings over time. In practice, oral feeding attempts are often limited because of concerns that excessive energy will be expended at the cost of weight gain, although this is not documented in the literature. In fact, although research is limited, there is some evidence that preterm infants who have more bottle opportunities attain full oral feeding earlier than infants who receive fewer opportunities.15,17,18
The purpose of this study was to develop an exploratory model of feeding readiness that predicted feeding performance. Feeding readiness indicators in this study were morbidity, maturity, behavior state at the start of feeding (hereafter, behavior state), and feeding experience. Feeding performance outcomes were proficiency, percent of prescribed volume consumed (hereafter, consumed), and efficiency.13
Design
The longitudinal data for this analysis were collected from all infants who participated in a nonexperimental study designed to examine the relationship of feeding readiness to feeding outcomes in preterm infants. All data were collected between August 2001 and August 2004. The purpose of the study was to develop a model of feeding performance. The study was approved by the university's institutional review board, and parents of the infants gave informed consent.
Setting
Data collection occurred in a level 3 nursery located in a university medical center. The unit admits approximately 250 preterm infants per year who stay an average of 47 days.
Sample
The sample was recruited over 3 years. Infants were eligible for the study if they were born less than 32 weeks PCA and had no known gastrointestinal, craniofacial, cardiovascular, neurological, or muscular defects. The sample consisted of 95 preterm infants whose PCA at birth ranged from 24 to 32 weeks (mean, 29.3; SD, 2.0). Infants weighed from 550 to 2390 grams at birth (mean, 1290.6; SD, 397). There were 48 male and 47 female infants. Seventy-one percent (71%) of the sample were African American, and 24% were white. Only 3 (3%) were Hispanic.
Measures
There were four components of feeding readiness: morbidity, maturity, behavior state, and feeding experience. There were 3 components of feeding performance: proficiency, consumed, and efficiency. The methods and instruments used to measure the components of feeding readiness and feeding outcomes are described below.
Morbidity or illness complications are a variable that may influence a preterm infant's ability to successfully bottle-feed. Morbidity was measured using the Neonatal Medical Index (NMI).20 The NMI was designed to measure how ill the infants were during the hospital stay rather than representing a complete inventory of all the different complications and symptoms that infants experience. Neonatal Medical Index scores at 32 weeks have been found to be predictive of PCA at full bottle-feeding and discharge.6 Neonatal Medical Index classifications range from 1 to 5, with 1 describing preterm infants free of significant medical problems and 5 characterizing infants with the most serious complications. Data to calculate the NMI are readily available from medical records. In this study, the NMI classification was determined at 32 weeks PCA.
Maturity was measured using both PCA and a separate measure of neurological maturity, the Neurobehavioral Maturity Assessment (NMA).21 Neurological maturation is often measured by researchers using PCA, a calculation of gestational age plus postnatal age. Although the relationship between PCA and neurological function has been established,22 age alone may not reliably capture the construct of neurological maturation. Items on the NMA used in this study (posture, scarf sign, and popliteal angle) have high test-retest reliability, are nonredundant, and are minimally invasive.23 In addition, a neurologically maturing infant shows predictably increasing scores on these items. Postconceptional age was first determined on enrollment in the study using the gestational age at birth as estimated by first trimester ultrasound if available or mother's dates if not, plus postnatal age (day of life); PCA increases by 1 with each successive day. The NMA was measured before each feeding observation by the data collectors; scores range from 0 to 13. Interrater reliability on the NMA was evaluated every 6 months and maintained at 95% or greater throughout the study.
Behavior state at the start of feeding has been found to be related to feeding outcomes in several studies.24-26 Behavior state was measured in this study using the Anderson Behavior State Scale (ABSS).27 The ABSS, which has been used in many infant-feeding studies, measures sleep and wakefulness on a scale of 1 to 12, where 1 is deep sleep and 12 is hard crying. To score behavior using the ABSS, the data collector observed the infant for 30 seconds, just before starting the feeding. The highest behavior state category observed during that period was recorded. Interrater reliability of all data collectors on the ABSS was evaluated every 6 months and maintained at 95% or greater throughout the study.
Feeding experience was defined as the number of cumulative nipple-feedings (either bottle or breast). The study protocol did not prescribe the number of nipple-feedings that were offered. Rather, infants enrolled in the study were offered nipple-feedings at the discretion of the nursing staff, consistent with unit practice. Measurements for the study were taken at the infants' first nipple (bottle)–feeding, between 32 and 33 weeks PCA. After that, the daily number of feedings offered by nipple, as well as the number of potential opportunities to nipple-feed, was recorded by data collectors at each observed feeding. Infants received formula or breast milk in a volume prescribed by their primary care provider; this amount varied across infants but increased for all over the course of the study, consistent with infants' growth.
Feeding performance measures were proficiency, consumed, and efficiency.13 Proficiency refers to the percent of prescribed formula taken during the first 5 minutes of the feeding. Proficiency has been described as an index of oral-motor skill since its measurement occurs at a time when fatigue is expected to be minimal.13 To determine proficiency, the feeding was stopped briefly at 5 minutes, and the amount of formula remaining in the bottle was recorded. Consumed refers to the percent of prescribed formula consumed orally over the feeding time (not counting breaks for burps or rest). As a measure of feeding performance, consumed incorporates both oral-motor skill and level of endurance.13 The time it took for an infant to feed was highly variable and depended in part on the amount of prescribed formula and maturity. No feedings lasted longer than 20 minutes at nipple. The amount consumed was recorded at the end of the feeding. Efficiency refers to the total volume taken over feeding time and is a reflection of oral-motor skill as well as fatigue.13 The amount taken was recorded by the data collector at the end of the feeding. Fluid lost and not actually consumed was negligible. Feeding time was calculated by a computerized data acquisition system that eliminated nonfeeding times (ie, burp or rest breaks). Interrater reliability of data collectors on procedures related to recording volumes for calculation of proficiency, consumed, and efficiency was evaluated every 6 months and maintained at 95% or greater throughout the study.
Procedures
Infants were enrolled in the study when they were 30 to 32 weeks PCA. Infants were observed at bottle-feeding once every day or every other day depending on their NMI classification, with the most ill infants being observed every other day. This schedule of observation feedings was designed to ensure that these most ill infants were not subjected to undue stress related to feeding more frequently than was typical in the unit. The study period thus lasted 2 to 3 weeks, depending on NMI classification; observations did not continue until infants were fully nipple-feeding. In between observed feedings, infants' feeding modality was left to the discretion of the bedside nurse (gavage, breast, or bottle). Feeding performance data were collected at feeding observations by trained research nurses (data collectors). Feeding experience data were collected on standardized forms from the bedside record. These data included the number of possible nipple-feeding opportunities and the number of actual nipple-feeding attempts that occurred. The volume and the percent of prescribed volume taken at each attempt were also recorded.
Analysis
The unit of analysis for the study was the feeding observation. Participating infants were observed 4 to 14 times depending on their severity of illness classification and on other factors, such as early discharge. A total of 920 feedings were observed. The relationships between feeding readiness predictors and feeding performance outcomes were analyzed using repeated-measures analyses to account for the dependence of observations within infants across time. This was done using general estimating equations and generalized linear models (Proc Genmod in SAS v8, SAS Institute, Cary, NC). An exchangeable correlation structure was used, with subjects nested within NMI. The analyses took all readiness indicators and their interactions into account.
Results
Three of the readiness indicators changed over time—maturity, behavior state, and feeding experience. However, because a one-time measure of illness complications was used as the measure of morbidity, this indicator did not change over time. The average value for each feeding readiness indicator and each feeding performance outcome by morbidity (NMI) classification is shown in Table 1. Numbers of infants in each morbidity classification were not equal. However, equality of groups was not required because of the statistical methods used. Values for the first observed and last observed feedings are shown. At the first observed feeding, infants had no feeding experience, and by study design, all started at approximately the same time, between 32 and 33 weeks PCA. However, NMA, an independent measure of neurological maturity varied at the first feeding as did behavior state. At the final observed feeding, infants were still, by study design, at approximately the same PCA, 34 to 35 weeks. However, feeding experience was quite variable across NMI groups, whereas NMA was not. This variability is because no attempt was made to control the amount of feeding experience in this nonexperimental study. In addition, all components of feeding performance improved between the first observed feeding and the last observed feeding.
Table 1.
Average Indicator and Outcome Variables by Morbidity Classification* at First and Last Observed Feeding
| Median (range) |
|||||
|---|---|---|---|---|---|
| Measurement | NMI 1 (n = 16) | NMI 2 (n = 7) | NMI 3 (n = 47) | NMI 4 (n = 12) | NMI 5 (n = 13) |
| First observed feeding | |||||
| Maturity (PCA) | 33 (32.0–33.9) | 32.7 (32.1–34.0) | 32.4 (32.034.3) | 32.6 (32.0–33.0) | 32.9 (32.1–33.3) |
| Maturity (NMA) | 7 (3–10) | 6 (4–9) | 7.5 (5–10) | 6.5 (5–10) | 7 (5–9) |
| Behavior | 4 (2–10) | 2 (2–6) | 5 (2–10) | 2 (2–6) | 5 (2–10) |
| Experience | 0 (0–23) | 0 (0–9) | 0 (0–47) | 0 (0–14) | 0 (0–1) |
| Proficiency | 0.24 (0.09–1.00) | 0.40 (0.09–1.00) | 0.21 (0.00–1.00) | 0.22 (0.00–0.86) | 0.24 (0.00–0.56) |
| Consumed | 0.35 (0.12–1.00) | 0.50 (0.29–1.00) | 0.32 (0.00–1.00) | 0.26 (0.06–1.00) | 0.23 (0.00–1.00) |
| Efficiency | 1.50 (0.63–10.50) | 1.71 (0.70–5.45) | 1.20 (0.00–4.31) | 1.23 (0.47–4.04) | 1.04 (0.00–2.39) |
| Last observed feeding | |||||
| Maturity (PCA) | 34.5 (32.9–35.4) | 34.6 (33.4–35.9) | 34.6 (32.3–36.1) | 34.8 (33.6–35.4) | 35.3 (34.0–35.9) |
| Maturity (NMA) | 9.5 (7–12) | 9 (7–10) | 9 (7–12) | 9 (7–10) | 9 (7–11) |
| Behavior | 5 (2–10) | 3 (2– 6) | 4 (2–10) | 4 (2–7) | 5 (2–11) |
| Experience | 53.5 (18–92) | 37 (20–119) | 66 (0–117) | 71.5 (3– 108) | 41 (4–118) |
| Proficiency | 0.51 (0.07–1.00) | 0.52 (0.40–0.95) | 0.52 (0.07–1.00) | 0.54 (0.09–1.00) | 0.42 (0.10–0.86) |
| Consumed | 0.88 (0.13–1.00) | 1.00 (0.51–1.00) | 0.91 (0.07–1.00) | 1.00 (0.29–1.00) | 0.71 (0.20–1.00) |
| Efficiency | 3.24 (0.83–9.24) | 4.11 (1.60–9.09) | 3.63 (0.45–9.05) | 4.43 (1.12–10.59) | 2.75 (0.76–6.54) |
NMI 1, most well; NMI 5, most ill.
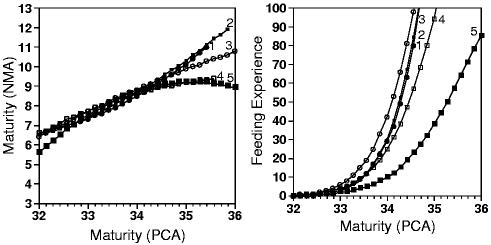
Readiness indicator values from each infant were related to each other over time. In particular, PCA and feeding experience were correlated at r = 0.87. To insure that the relationships among feeding readiness indicators were accounted for in model building, a repeated-measures mixed-models analysis was used. This analysis resulted in a description of the trends in these readiness indicators across time and allowed differences in trends according to morbidity to be examined. The trends in readiness indicators are seen in Fig 1. As PCA increased, infants evidenced greater neurological maturity on the NMA (left panel) and had increasing feeding experience (right panel). Thus, changes in maturity and experience were predictable across time. However, the most ill infants (NMI 4 and 5) had a leveling off of neurological maturity, whereas the most well infants continued to gain in neurological maturity as measured by the NMA. Moreover, the most ill infants (NMI 5) had a much slower rate of increase in feeding experience. That is, they were offered nipple-feedings much less frequently than more well infants. Behavior state did not have a predictable pattern and thus is not illustrated in these trends. Rather, infants were fed in almost all behavior states; these states affected feeding outcomes independent of experience or maturity.
Fig 1.
Trends in readiness indicators by morbidity classification. Classification 1–5 (1 = most well, 5 = most ill). Morbidity: indicates 1 (most well); ■, 2; ○, 3; ■, 4; ■, 5 (most ill).
Feeding readiness indicators were related to feeding performance outcomes. Table 2 summarizes the model of these associations. Feeding performance, the primary outcome, has 3 components—proficiency, consumed, and efficiency. The effects tested were morbidity, maturity (both PCA and NMA), behavior state, and feeding experience. Because the purpose of this study was to build a descriptive model rather than to test hypotheses, the significance level was set at .1. As seen, morbidity did not have a significant effect on proficiency or consumed. However, it was included in the model because morbidity did affect feeding experience and maturity. Maturity, behavior state, and feeding experience were all significantly related to feeding performance outcomes.
Table 2.
Relationships of Indicators to Outcomes*
| Outcomes |
|||||||
|---|---|---|---|---|---|---|---|
| Proficiency |
Consumed |
Efficiency |
|||||
| Feeding Readiness Indicators | df | χ2 | P value | χ2 | P value | χ2 | P value |
| Morbidity (NMI) | 3 | 5.06 | .167 | 3.01 | .391 | 8.18 | .043 |
| Maturity | 4 | 11.25 | .024 | 15.67 | ≤.00 | 11.30 | .023 |
| PCA (linear) | 1 | 0.88 | .349 | 0.95 | .331 | 1.45 | .229 |
| PCA (quadratic) | 1 | 3.40 | .065 | 6.03 | .014 | 2.97 | .085 |
| NMA | 1 | 4.58 | .032 | 10.38 | .001 | 3.23 | .072 |
| Behavior state | 1 | 8.09 | .005 | 11.82 | .001 | 9.95 | .002 |
| Experience | 2 | 11.48 | .003 | 12.00 | .007 | 6.07 | .048 |
| Cumulative attempts | 1 | 10.53 | .001 | 6.19 | .013 | 4.41 | .036 |
| Interaction (PCA × experience) | 1 | 7.55 | .006 | 9.54 | .002 | 2.8 | .094 |
P ≤ .1.
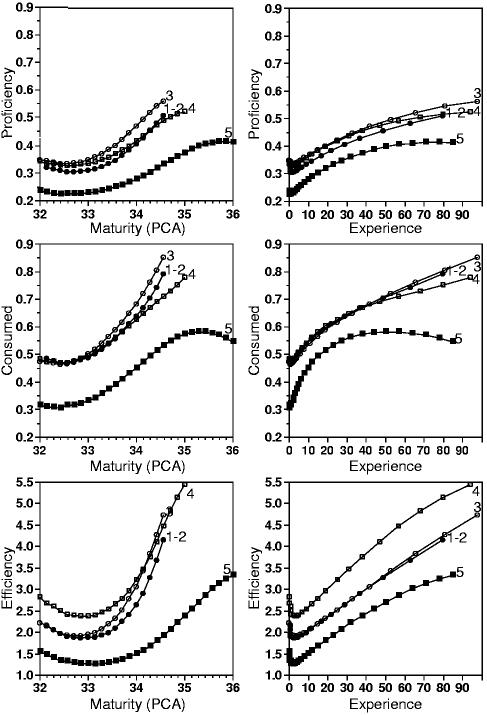
Fig 2 illustrates the predicted effect of feeding readiness indicators on feeding performance outcomes. Proficiency is the proportion of prescribed formula consumed during the first 5 minutes of the feeding. The predicted effect of PCA and neurological maturity on proficiency is shown in the upper left panel of Fig 2. Infants at 32 weeks PCA and NMA 6 consumed approximately 35% of the prescribed formula in the first 5 minutes of the feeding.
Fig 2.
Relationships between outcomes and maturity and experience. Classification 1–5 (1–2 = most well, 5 = most ill). Morbidity: indicates 1,2 (most well); ○, 3; ■, 4; ■, 5 (most ill).
With increasing PCA and neurological maturity, proficiency increased; this is a quadratic effect. However, this increase in proficiency did not emerge until after 33 weeks PCA when it increased to approximately 50% in all but the most ill infants (NMI 5). Neurological maturity (NMA) is thus an independent predictor of proficiency. That is, proficiency increased by only 1.4% for each unit increase in NMA even after the effect of PCA was taken into account. The effect of experience on proficiency is illustrated in the upper right hand panel of Fig 2. As the number of bottle-feedings increased, proficiency also increased.
Consumed is the proportion of the prescribed formula consumed over the feeding. The relationship of this outcome to the feeding readiness predictors was similar to that for proficiency, as illustrated in the middle panels in Fig 2. That is, after maturity, behavior state, and feeding experience were covaried out, there was no significant relationship due to morbidity. However, maturity was significantly related to the outcome consumed as was feeding experience. In addition, maturity and experience had a significant interaction here as well; the effect of maturity depended on experience, and the effect of experience depended on maturity. In addition, proficiency, the percent consumed at 5 minutes, is the lower bound on the final outcome, consumed. If infants completed a feeding in the first 5 minutes, then consumed would equal proficiency—this occurred in 34% of all the feedings. In all other feedings, however, what was consumed by 5 minutes was related to what was consumed over the entire feeding. These relationships are illustrated in Fig 3. For example, after the first 5 minutes of feeding, the most well infants (NMI 1-2) consumed an additional 15% at the first observed feeding and an additional 25% at the last observed feeding. On the other hand, the most ill infants (NMI 5) consumed an additional 8% at the first observed feeding and only 20% more at the last observed feeding. Maturity and experience did not affect the proportion of prescribed formula consumed by the end of the feeding for these sicker infants.
Fig 3.
Relationships between proficiency and consumed. Classification 1–5 (1–2 = most well, 5 = most ill). Morbidity: indicates 1,2 (most well); ○, 3; ■, 4; ■, 5 (most ill).
Efficiency is the volume (milliliters) taken per minute of feeding. The relationships between this outcome and the feeding readiness indicators were similar to those seen with proficiency and consumed. Here, however, morbidity was significant, as seen the lower panels in Fig 2. The most ill infants (NMI 5) had the least efficient feeding, beginning at approximately 1.5 mL/min and increasing slowly over 2 weeks to 3 mL/min. Most infants began with a feeding efficiency of 2 mL/min and increased to 4 mL/min by 34 weeks.
As seen in Table 2, there was a significant interaction between PCA and experience, indicating that the effect of PCA on proficiency, consumed, and efficiency depended on the infant's feeding experience and that the infant's feeding experience depended on the infant's PCA. This interaction of maturity and experience is seen in the trends in Fig 2. The panels on the left show a “sagging” in the feeding performance outcome curves before they increase with PCA. In the top left panel, the trend for infants with NMI 3 remained the most flat with a slight decrease between 32 and 33 weeks PCA. After 33 weeks PCA, the increase in proficiency becomes evident. The sagging of predicted trends is seen in the middle and lower left panels as well, revealing the consistency in the interaction between PCA and experience. Of note, the most ill infants (NMI 5) showed the longest “sag” in their predicted trends, indicating that these infants require more maturity before feeding performance improves with experience.
Similar sagging is seen in the right hand panels of Fig 2, although because of scaling, the sagging is not quite as evident. Thus, there was consistency in the interaction between maturity and experience. In other words, it took a certain amount of experience before maturity had an effect on feeding performance outcomes, and it took a certain maturity before experience had an effect on feeding performance outcomes.
Not illustrated in Fig 2 is the effect of behavior state on feeding performance outcomes. The model in Table 2 showed that there were differences in outcomes by behavior state categorization. Although behavior state did not have a predictable trend across time, infants fed in more active behavior states, including active and very active awake states, had increased proficiency, consumed, and efficiency.
Discussion
There are clear relationships between feeding readiness indicators and feeding performance outcomes. The feeding indicators (maturity, behavior state, and feeding experience) were all related to each of the outcomes (proficiency, consumed, and efficiency). However, except for the most ill infants, morbidity was not related to these feeding performance outcomes. The form of the relationship between behavior state and feeding outcomes was a simple linear trend. In the case of maturity and experience, however, the relationship was more complex because of the significant interaction between these 2 indicators. That is, the effect of maturity depended on experience, and the effect of experience depended on maturity. These findings are similar to those of other studies.13,28 Certainly, recent research increasingly supports the hypothesis that feeding experience, that is, increased opportunities to nipple-feed, results in improved feeding performance.15,29 In addition, although not studied here, there is growing evidence that increased opportunities to nipple-feed may shorten the transition from gavage to competent nipple-feeding.6,18 However, a challenge to providing increased opportunities for nipple-feeding is that nurses, whose responsibility is often to make decisions about oral vs gavage feeding, have few empirically tested criteria upon which to make those decisions. Thus, there is a trial-and-error approach to providing nipple-feeding opportunities that may not be in the infant's best interest.
Several studies have reported that a quiet alert state is optimal for feeding success.18,29 However, in this study where no attempt was made to alter behavior state before feeding, infants who were more active had greater proficiency and efficiency and consumed a greater percentage of prescribed volume than did infants in quiet awake or quiet alert states. This particular finding may challenge the belief that alert quiet behavior is optimal for successful nipple-feeding. The differences in findings may be due to different definitions of optimal feeding performance. The measures of feeding performance used in this study have been used extensively in other research.13,15 Although universally accepted measures of optimal feeding performance have not been established, most clinicians would agree that consumption of prescribed volume is probably an important outcome.
The findings of this study are limited by its design. In this study, feeding onset was controlled, occurring between 32 and 34 weeks PCA. In addition, data were only collected for the first 2 to 3 weeks of nipple-feeding. As a result, the measures of maturity have limited variability. In addition, because feeding experience was not controlled, it was not possible to directly test the effect of experience on the outcomes. Although the feeding observations were the unit of analysis in this study, the dependence of these data points was taken into account by the statistical analysis used. That is, the repeated-measures analyses treated each infant as independent and also allowed the observations within an infant to be correlated. Thus, the data presented here are predicted trends for average infants in each classification of morbidity and neurological maturity.
The purpose of this study was to develop a model of feeding readiness and feeding outcomes that could be tested in further research. Thus, a liberal significance level of .1 was used. As a result, some readiness indicators may have been retained that would have been excluded had a more stringent level of significance been used. The model presented in this paper posits relationships between morbidity, maturity, behavior state, and feeding experience and feeding performance outcomes that can be tested in future research. These findings, although clarifying some questions about the development of infant-feeding competence, also raise questions how to manage feedings for some infants, particularly the most ill.
Conclusion
Achieving competence at nipple-feeding requires maturity and experience. Readiness to feed is thus dependent on these indicators. In addition, a more wakeful behavior state contributes to improved feeding outcomes. The most well infants in this study achieved competence at consumption within 1 week of their first nipple-feeding; the most ill infants required at least 2 weeks. More research is needed about how frequently to offer feedings to infants at various stages of maturity and levels of morbidity.
Footnotes
Supported by a grant from the National Institute of Nursing Research, National Institutes of Health, R01 NR005182.
Contributor Information
Rita H. Pickler, From the Department of Maternal Child Nursing, Virginia Commonwealth University, Richmond, VA.
Al M. Best, From the Department of Biostatistics, Virginia Commonwealth University, Richmond, VA.
Barbara A. Reyna, From the Division of Nursing, Virginia Commonwealth University, Richmond, VA.
Paul A. Wetzel, From the Department of Biomedical Engineering, Virginia Commonwealth University, Richmond, VA.
Gary R. Gutcher, From the Department of Pediatrics, Virginia Commonwealth University, Richmond, VA..
References
- 1.Aguayo J. Maternal lactation for preterm newborn infants. Early Hum Dev. 2001;65:19–29. doi: 10.1016/s0378-3782(01)00203-1. [DOI] [PubMed] [Google Scholar]
- 2.Dowling DA. Physiological responses of preterm infants to breast-feeding and bottle-feeding with the orthodontic nipple. Nurs Res. 1999;48:78–85. doi: 10.1097/00006199-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Pinelli J, Atkinson SA, Saigal S. Randomized trial of breastfeeding support in very low-birth-weight infants. Arch Pediatr Adolesc Med. 2001;155:548–553. doi: 10.1001/archpedi.155.5.548. [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Pediatrics Proposed guidelines Committee on the Fetus and Newborn: hospital discharge of the high-risk neonate. Pediatrics. 1998;102:411–417. [PubMed] [Google Scholar]
- 5.Lemons PK. From gavage to oral feedings: just a matter of time. Neonatal Netw. 2001;20:7–14. doi: 10.1891/0730-0832.20.3.7. [DOI] [PubMed] [Google Scholar]
- 6.Pickler RH, Mauck AG, Geldmaker B. Bottle-feeding histories of preterm infants. J Obstet Gynecol Neonatal Nurs. 1997;26:414–420. doi: 10.1111/j.1552-6909.1997.tb02723.x. [DOI] [PubMed] [Google Scholar]
- 7.Kinneer MD, Beachy P. Nipple feeding premature infants in the neonatal intensive-care unit: factors and decisions. J Obstet Gynecol Neonatal Nurs. 1994;23:105–112. doi: 10.1111/j.1552-6909.1994.tb01859.x. [DOI] [PubMed] [Google Scholar]
- 8.Gewolb IH, Vice FL, Schwietzer-Kenney EL, et al. Developmental patterns of rhythmic suck and swallow in preterm infants. Dev Med Child Neurol. 2001;43:22–27. doi: 10.1017/s0012162201000044. [DOI] [PubMed] [Google Scholar]
- 9.Mathew OP. Science of bottle feeding. J Pediatr. 1991;119:511–519. doi: 10.1016/s0022-3476(05)82397-2. [DOI] [PubMed] [Google Scholar]
- 10.McCain GC, Gartside PS, Greenberg JM, et al. Introduction of oral feeding in preterm infants: a clinical trial. Cent Lines. 2002;16:12. [Google Scholar]
- 11.Bu'Lock F, Woolridge MW, Baum JD. Development of coordination of sucking, swallowing and breathing: ultrasound study of term and preterm infants. Dev Med Child Neurol. 1990;32:669–678. doi: 10.1111/j.1469-8749.1990.tb08427.x. [DOI] [PubMed] [Google Scholar]
- 12.Medoff-Cooper B. Changes in nutritive sucking patterns with increasing gestational age. Nurs Res. 1991;40:245–247. [PubMed] [Google Scholar]
- 13.Lau C, Sheena HR, Shulman RJ, et al. Oral feeding in low birth weight infants. J Pediatr. 1997;130:561–569. doi: 10.1016/s0022-3476(97)70240-3. [DOI] [PubMed] [Google Scholar]
- 14.Lau C, Alagugurusamy R, Schanler RJ, et al. Characterization of the developmental stages of sucking in preterm infants during bottle feeding. Acta Paediatr. 2000;89:846–852. [PubMed] [Google Scholar]
- 15.Simpson C, Schanler RJ, Lau C. Early introduction of oral feeding in preterm infants. Pediatrics. 2002;110:517–522. doi: 10.1542/peds.110.3.517. [DOI] [PubMed] [Google Scholar]
- 16.Pridham K, Brown R, Sondel S, et al. Transition time to full nipple feeding for premature infants with a history of lung disease. J Obstet Gynecol Neonatal Nurs. 1998;27:533–545. doi: 10.1111/j.1552-6909.1998.tb02620.x. [DOI] [PubMed] [Google Scholar]
- 17.Pickler RH, Reyna BA. A descriptive study of bottle feeding opportunities in preterm infants. Adv Neonatol Care. 2003;3:139–146. doi: 10.1016/s1536-0903(03)00074-2. [DOI] [PubMed] [Google Scholar]
- 18.McCain GC, Gartside P, Greenberg JM, et al. A feeding protocol for healthy preterm infants that shortens time to oral feeding. J Pediatr. 2001;139:374–379. doi: 10.1067/mpd.2001.117077. [DOI] [PubMed] [Google Scholar]
- 19.Romero R, Kleinman RE. Feeding the very low-birth-weight infant. Pediatr Rev. 1993;14:123–132. doi: 10.1542/pir.14-4-123. [DOI] [PubMed] [Google Scholar]
- 20.Korner AF, Stevenson DK, Kraemer HC, et al. Prediction of the development of low birth weight preterm infants by a new neonatal medical index. J Dev Behav Pediatr. 1993;14:106–111. [PubMed] [Google Scholar]
- 21.Korner AF, Kraemer HC, Reade EP, et al. A methodological approach to developing an assessment procedure for testing the neuro-behavioral maturity of preterm infants. Child Dev. 1987;58:1478–1487. [PubMed] [Google Scholar]
- 22.Amiel-Tison C. Neurological evaluation of the maturity of newborn infants. Arch Dis Child. 1968;43:89–93. doi: 10.1136/adc.43.227.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Myers BJ, Jarvis PA, Creasey GL, et al. Prematurity and respiratory illness: Brazelton scale (NBAS) performance of preterm infants with bronchopulmonary dysplasia (BPD), respiratory distress syndrome (RDS), or no respiratory illness. Inf Behav Dev. 1992;15:27–41. [Google Scholar]
- 24.McCain GC. Behavioral state activity during nipple feedings for preterm infants. Neonatal Netw. 1997;16:43–47. [PubMed] [Google Scholar]
- 25.McGrath JM, Medoff-Cooper B. Alertness and feeding competence in extremely early born preterm infants. Newborn Infant Nurs Rev. 2002;2:174–186. [Google Scholar]
- 26.Pickler RH, Frankel HB, Walsh KM, et al. Effects of nonnutritive sucking on behavioral organization and feeding performance in preterm infants. Nurs Res. 1996;45:132–135. doi: 10.1097/00006199-199605000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Gill NE, Behnke M, Conlon M, et al. Effect of nonnutritive sucking on behavioral state in preterm infants before feeding. Nurs Res. 1988;37:347–350. [PubMed] [Google Scholar]
- 28.Medoff-Cooper B, McGrath JM, Shults J. Feeding patterns of full-term and preterm infants at forty weeks postconceptional age. Dev Behav Pediatr. 2002;23:231–236. doi: 10.1097/00004703-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 29.McCain GC, Gartside P. Behavioral responses of preterm infants to a standard-care and semi-demand feeding protocol. Newborn Infant Nurs Rev. 2002;2:187–193. [Google Scholar]