Abstract
Objective: To test whether an intervention to improve primary care depression management significantly improves productivity at work and absenteeism over 2 years.
Setting and Subjects: Twelve community primary care practices recruiting depressed primary care patients identified in a previsit screening.
Research Design: Practices were stratified by depression treatment patterns before randomization to enhanced or usual care. After delivering brief training, enhanced care clinicians provided improved depression management over 24 months. The research team evaluated productivity and absenteeism at baseline, 6, 12, 18, and 24 months in 326 patients who reported full-or part-time work at one or more completed waves.
Results: Employed patients in the enhanced care condition reported 6.1% greater productivity and 22.8% less absenteeism over 2 years. Consistent with its impact on depression severity and emotional role functioning, intervention effects were more observable in consistently employed subjects where the intervention improved productivity by 8.2% over 2 years at an estimated annual value of $1982 per depressed full-time equivalent and reduced absenteeism by 28.4% or 12.3 days over 2 years at an estimated annual value of $619 per depressed full-time equivalent.
Conclusions: This trial, which is the first to our knowledge to demonstrate that improving the quality of care for any chronic disease has positive consequences for productivity and absenteeism, encourages formal cost-benefit research to assess the potential return-on-investment employers of stable workforces can realize from using their purchasing power to encourage better depression treatment for their employees.
Keywords: primary care, depression, absenteeism, productivity, quality improvement
Depression substantially reduces an employee's ability to work, as evidenced by increased absenteeism1-7 and reduced productivity during days at work.8-11 Whether depression interventions that enhance general functioning12-15 also improve productivity and absenteeism has not been well studied. In a sample of depressed patients working for multiple companies across the country, we tested the hypothesis that an intervention to enhance primary care depression management would significantly improve productivity and absenteeism over 2 years. We explored this hypothesis in consistently and inconsistently employed patients separately, because inconsistently employed patients have barriers to work that the intervention did not address.16-22
METHODS
Our methods, described in detail elsewhere,23 are summarized here. Following approval by the Human Research Advisory Committee of the University of Arkansas for Medical Sciences and the Colorado Multi-Institutional Review Board, the research team conducted the study in 12 community primary care practices across the United States, none of which employed onsite mental health professionals to treat depression. The first author matched the 12 mixed-model practices into 6 blocks by depression treatment patterns; then, one practice from each block was randomly assigned to enhanced care. This randomization method produced within-group balance for all sociodemographic, occupational, and clinical characteristics listed in Table 1 and within-block balance for all characteristics except minority status, which was slightly unbalanced in 2 blocks in opposite directions. Patients presenting for routine visits at these practices between April 1996 and September 1997 were asked to complete a 2-stage screener that identified patients reporting 5 or more of the 9 Diagnostic and Statistical Manual–III Revised criteria for major depression in the past 2 weeks. Screen-positive patients meeting criteria for bereavement, mania, alcohol dependence, pregnancy/postpartum, or life-threatening physical illness were excluded from the study, as were patients who did not intend to use the clinic as their usual source of care during the year following the index visit, patients who did not have telephone access, patients who were illiterate in English, or patients who were cognitively impaired. As shown in Figure 1, 73.4% (479/653) of depressed patients agreed to participate in the longitudinal study. Sixty-eight percent (326/479) of participating patients reporting full- or part-time employment at one or more completed waves constitute the sample for analyzing intervention effects on productivity and absenteeism; 198 participating patients reporting full- or part-time employment at every completed wave over 2 years constitute the sample for the consistently employed subgroup analysis; and 128 participating patients reporting full- or part-time employment at one or more completed waves and no employment at one or more completed waves constitute the sample for the inconsistently employed group.
TABLE 1.
Comparison of Baseline Sociodemographic and Clinical Characteristics Between Enhanced and Usual Care Patients
| Total Group | Consistently Employed | Inconsistently Employed‡ | ||||
|---|---|---|---|---|---|---|
| Enhanced Care n = 158 | Usual Care n = 168 | Enhanced Care n = 96 | Usual Care n = 102 | Enhanced Care n = 62 | Usual Care n = 66 | |
| Mean age (SD) | 37.9 (10.9) | 40.2 (10.3) | 37.6 (9.5) | 40.1 (10.3) | 38.3 (12.8) | 40.4 (10.5) |
| Female, % | 84.2 | 85.7 | 84.4 | 82.4 | 83.8 | 90.9 |
| Minority, % | 13.3 | 13.1 | 14.6 | 11.8 | 11.3 | 15.2 |
| Currently married, % | 44.9 | 51.2 | 39.6 | 52.0 | 53.2 | 50.0 |
| High school educated, % | 85.4 | 86.3 | 88.5 | 93.1 | 80.7 | 75.8 |
| Health insured, % | 84.8 | 82.1 | 86.5 | 85.3 | 82.3 | 77.3 |
| Professional/administrators, %† | 18.0 | 28.3 | 19.8 | 29.4 | 12.5 | 25.0 |
| Managers/salespeople, %† | 34.4 | 38.4 | 35.4 | 37.3 | 31.3 | 41.7 |
| Clerical/services, %† | 47.6 | 33.3 | 44.8 | 33.3 | 56.2 | 33.3 |
| Employed full time, %† | 81.3 | 74.6 | 85.4 | 74.5 | 68.8 | 72.2 |
| Paid sick leave benefits, %† | 49.2 | 51.4 | 53.1 | 51.0 | 37.5 | 52.8 |
| Mean depression symptoms (SD) | 6.8 (1.4) | 6.6 (1.4) | 6.7 (1.4) | 6.6 (1.4) | 6.8 (1.4) | 6.6 (1.5) |
| Comorbid dysthymia, % | 14.6 | 17.9 | 13.5 | 16.7 | 16.1 | 19.7 |
| Mean physical comorbidities (SD) | 1.1 (0.8) | 1.2 (0.8) | 1.1 (1.2)* | 1.5 (1.4) | 1.4 (0.8) | 1.4 (0.8) |
P < 0.05.
60 inconsistently employed subjects unemployed at baseline have missing data.
Inconsistently employed subjects were employed an estimated 11.7 months (SD = 7.5) over 2 years.
FIGURE 1.
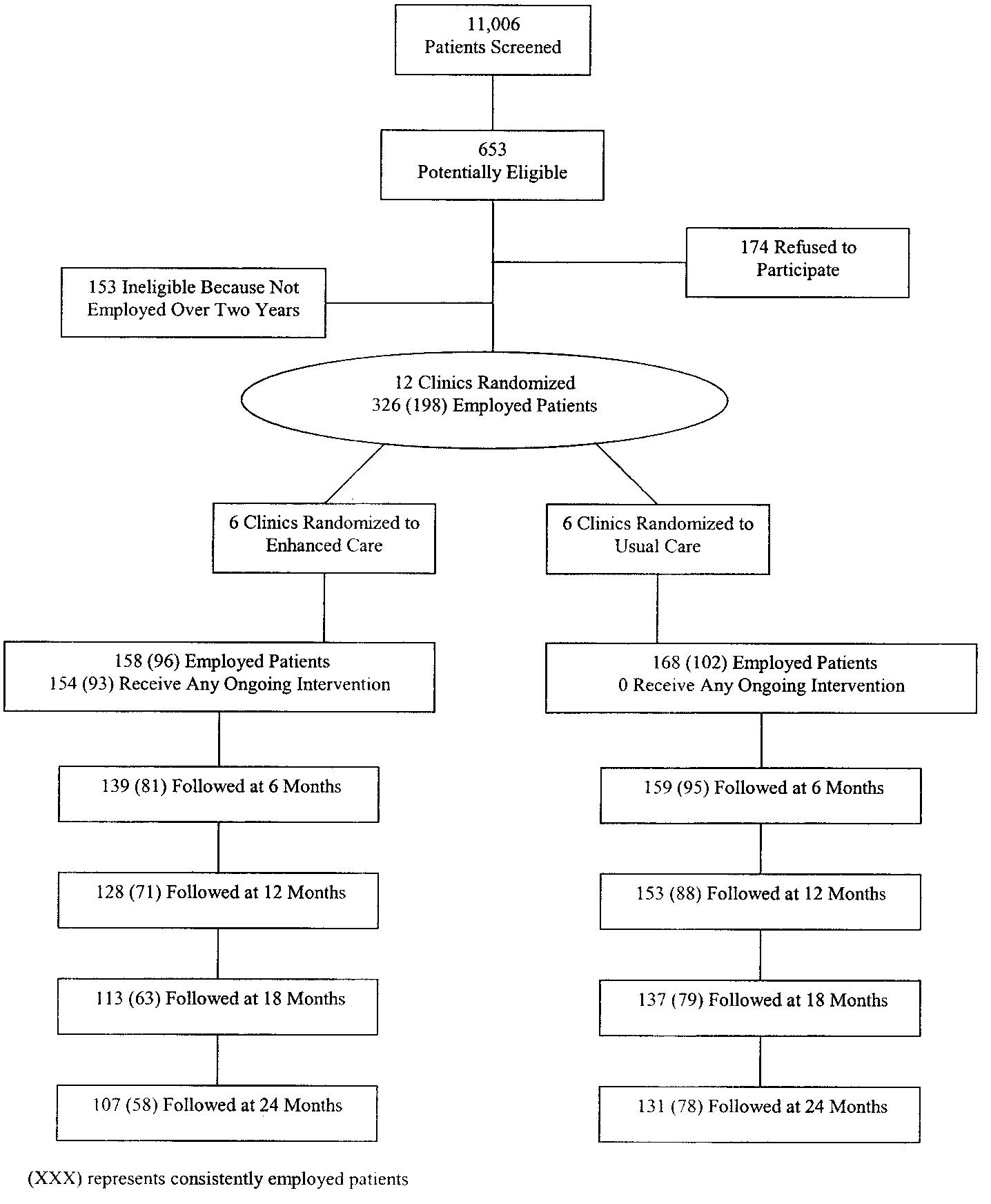
Patient recruitment and follow-up.
Prior to patient enrollment, the research team provided brief training23 to physicians and care managers in enhanced care practices to provide high-quality depression care to patients with current major depression during the acute and continuation phase of treatment. Training emphasized the need for physicians and care managers to encourage patients to initiate guideline-concordant pharmacotherapy or psychotherapy during the acute phase of treatment. To accomplish this, the care manager contacted patients in person or by phone to reassess their depressive symptoms, to educate them about depression and its treatment, and to ask the patient to complete “homework” assignments to increase their readiness to engage in active treatment. Training also emphasized the need for physicians and care managers to encourage continued treatment adherence if symptoms were resolving, to adjust treatment if symptoms were not resolving, and to terminate treatment when remitted patients did not require maintenance therapy following the continuation phase.24,25 To accomplish this, care managers contacted patients who reported 3 or more of 9 depressive symptoms every month, and patients who reported 2 or fewer depressive symptoms every 3 months. Primary care physicians received a summary of patient's symptom/treatment status, along with reminders to adjust treatment for symptomatic patients. Care managers reached 97.5% of 158 enhanced care patients one or more times, providing an average of 11.9 telephone or in-person sessions of 10–15 minutes duration over 2 years. Care manager contact rates were virtually identical between consistently and inconsistently employed patients (data available from authors upon request).
Data were collected by telephone using structured instruments administered by an independent member of the research team blinded to intervention status except for 5 subjects for whom primary care practices had to be contacted to request updated location information. The research team conducted 6-, 12-, 18-, and 24-month follow-up interviews between October 1996 and September 1999, achieving response rates of 92.3%, 86.2%, 76.7%, and 73.0% respectively (see Fig. 1).
Operational Definitions of Major Constructs
Labor Outcomes
Productivity
We defined productivity as effectiveness at work over the past 2 weeks. Reflecting that subject ratings of work productivity are not biased by depression severity,26 we measured the construct by subject rating of their productivity at work during the previous 2 weeks on a 0 (nothing at all accomplished) to 10 (best possible work performance) scale at 6, 12, 18, and 24 months. Because this item was not available from the baseline interview, we used regression-based statistical forecasting methods to estimate its baseline value (details available from the authors upon request).
Absenteeism
We defined absenteeism as the total number of work hours lost due to illness or doctor visits over the past 4 weeks. We measured absenteeism at baseline, 6, 12, 18, and 24 months by calculating lost work hours from employee reports of how many full workdays and part workdays they missed due to illness or doctor visits, reflecting that employee reports demonstrate high agreement with employer records of absenteeism.27
Full-Time Equivalent (FTE) Daily Earnings
For consistently employed subjects, daily earnings were estimated by dividing the sum of annual baseline wages plus self-employment income by 240 days. FTE daily earnings were estimated by multiplying daily earnings by 40/hours worked per week at baseline and inflated to Year 2000 dollars using the Consumer Price Index. For inconsistently employed subjects, daily earnings were conservatively estimated by multiplying the Year 2000 minimum wage by 8 hours for full-time employees and by 4 hours for part-time employees. FTE daily earnings were estimated by multiplying minimum wage by 8 hours/day.
Treatment and Clinical Outcomes
Treatment
We measured antidepressant medication use by summing patient reports of the number of months during the past 6 months they took antidepressants at guideline-concordant doses at the 6-, 12-, 18-, and 24-month interview. We measured specialty care counseling by asking patients whether they had any counseling from a mental health professional during the past 6 months at the 6-, 12-, 18-, and 24-month interview. Because these measures were constructed to characterize treatment intensity over a 2-year period, we conservatively assigned patients a value of zero for antidepressant medication months and specialty care counseling use for those waves patients were not interviewed.
Depression Severity
Depression severity was measured by a 100-point Center for Epidemiological Studies –Depression (CES-D) scale12 adapted to measure all DSM-IV depression criteria with higher scores indicating worse depressive symptoms.
Emotional Role Functioning
Role functioning was measured by the SF-36 emotional role functioning scale,28 with higher scores indicating better functioning.
Covariates
We selected covariates listed under Table 2 from more than 20 sociodemographic, occupational, and clinical characteristics by using stepwise regression methods to identify all variables that entered all dependent variable analyses at P < 0.20. Insurance was entered as a time-varying covariate to accommodate the changing insurance status of inconsistently employed patients.
TABLE 2.
Intervention Impact on Productivity and Absenteeism Over 2 Years
| All Employed Patients (n = 326) | Consistently Employed Patients (n = 198) | Inconsistently Employed Patients (n = 128) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | P | Est. | SE | P | Est. | SE | P | |
| Productivity† | |||||||||
| Intercept | 7.3223 | 0.98 | 0.0001 | 5.7981 | 1.24 | 0.0001 | 10.0882 | 1.69 | 0.0001 |
| Time | 0.0925 | 0.18 | 0.8729 | −0.1838 | 0.21 | 0.3708 | 0.6294 | 0.40 | 0.1163 |
| Time × time | −0.0306 | 0.05 | 0.4949 | 0.0124 | 0.05 | 0.8053 | −0.1498 | 0.10 | 0.1175 |
| Interv | −0.4749 | 0.24 | 0.0444 | −0.4294 | 0.27 | 0.1096 | −0.4485 | 0.51 | 0.3791 |
| Interv × time | 0.3170 | 0.27 | 0.2406 | 0.4451 | 0.30 | 0.1426 | −0.0791 | 0.57 | 0.8894 |
| Interv × time × time | −0.0325 | 0.07 | 0.6239 | −0.0524 | 0.07 | 0.4845 | 0.0272 | 0.14 | 0.8429 |
| −2LL | χ2 = 6.0, P < 0.05 | χ2 = 7.8, P = 0.02 | χ2 = 0.0, P = 0.99 | ||||||
| Absenteeism† | |||||||||
| Intercept | 0.4711 | 0.31 | 0.1343 | 0.6619 | 0.36 | 0.0652 | 0.0541 | 0.59 | 0.9273 |
| Time | −0.2204 | 0.06 | 0.0002 | −0.1814 | 0.06 | 0.0043 | −0.3168 | 0.14 | 0.0206 |
| Time × time | 0.0435 | 0.01 | 0.0024 | 0.0378 | 0.02 | 0.0149 | 0.0547 | 0.03 | 0.0923 |
| Interv | 0.1265 | 0.08 | 0.0952 | 0.1239 | 0.08 | 0.1245 | 0.1998 | 0.18 | 0.2581 |
| Interv × time | −0.0296 | 0.09 | 0.7308 | −0.0542 | 0.09 | 0.5627 | −0.0201 | 0.19 | 0.9172 |
| Interv × time × time | −0.0076 | 0.02 | 0.7184 | −0.0022 | 0.02 | 0.9249 | −0.0086 | 0.05 | 0.8537 |
| −2LL | χ2 = 5.6, P < 0.06 | χ2 = 5.1, P = 0.08 | χ2 = 0.9, P = 0.64 | ||||||
Controlling for baseline measures of age, minority status, education, comorbid dysthymia, treatment resistant depression risk, emotional functioning, physical comorbidity, full- or part-time employment, paid sick leave benefits, and time covarying health insurance status.
Data Analysis
Using post-hoc analysis of randomized controlled trial data to analyze intervention impact on process and outcomes, we conducted intent-to-treat analyses using time-trend (growth curve) models29 with an unstructured variance-covariance matrix in SAS 8.0 PROC MIXED for all waves subjects were employed. These models did not employ clustering because multilevel modeling indicated that the intraclass correlation for absenteeism or productivity by practice or physician was negligible. Absenteeism, productivity, and emotional role functioning were modeled with a random intercept across all employed waves as a function of intervention, time, time × time, intervention × time, intervention × time × time and covariates. We tested intervention effect by a likelihood ratio test comparing models with and without intervention × time and intervention × time × time terms. Because quadratic terms did not improve the model fit, depression severity was modeled with a random intercept across all employed waves as a function of intervention, time, intervention × time, and covariates. We tested intervention effect by examining the statistical significance of the intervention × time coefficient. Because we expected the intervention would have a different impact in consistently and inconsistently employed subjects, we repeated the analysis in these 2 subgroups. Using 2-sided t-tests with a significance level of 0.05, nonclustered power analyses indicated that we had 80% power to detect an intervention effect size of 0.35 in the full sample, 0.45 in consistently employed patients, and 0.51 in inconsistently employed patients at any wave. Because analysis of missing data patterns produced no evidence of nonignorable missingness, we present unweighted models, noting that weighted models produce closely comparable results.
To quantify the intervention's impact on productivity, we compared area under the curve for the productivity functions over 2 years for enhanced and usual care patients, calculating the proportion gain in 24-month productivity in the enhanced care group. To quantify the intervention's impact on absenteeism, we employed parallel methods. To monetize the intervention's impact on productivity, we multiplied the proportion gain in 24-month productivity in the enhanced care group × average work-days over 24 months in the usual care group × average FTE daily earnings and divided this product by 2 to estimate the annual value of improved productivity per depressed subject. To monetize the intervention's impact on absenteeism, we multiplied the proportion reduction in 24-month absenteeism in the enhanced care group × average absenteeism days over 24 months in the usual care group × average FTE daily earnings and divided this product by 2 to estimate the annual value of reduced absenteeism per depressed subject. Further information on variable derivation and data analysis is available upon request.
RESULTS
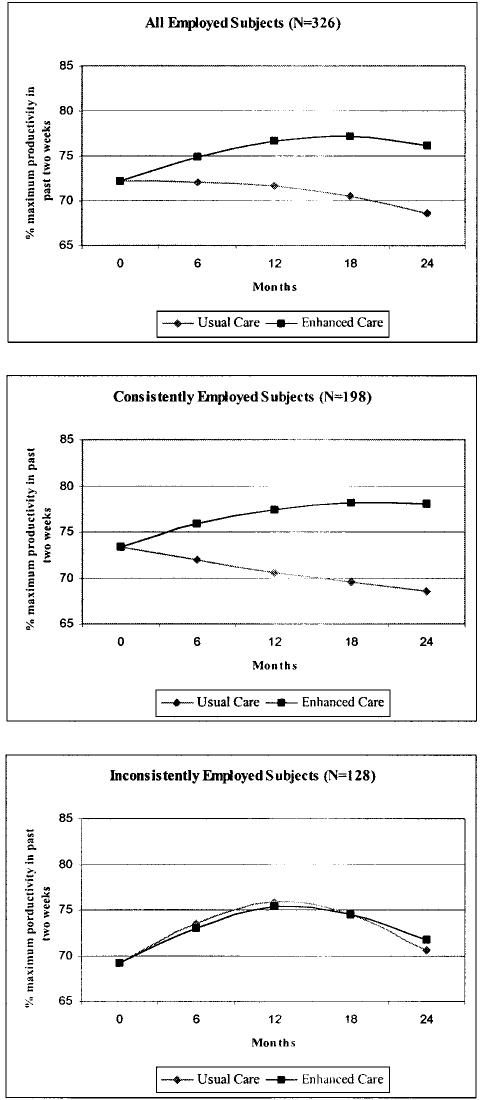
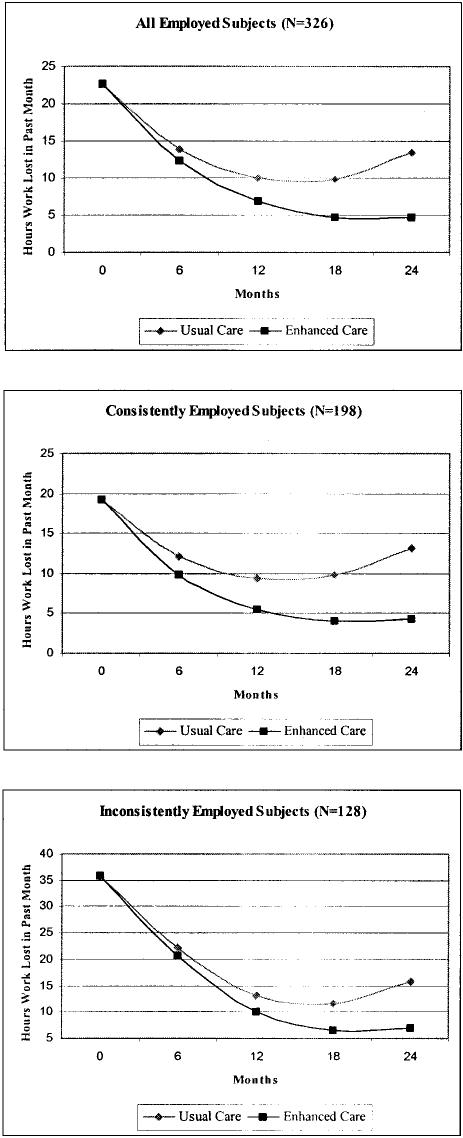
In the analysis of the entire cohort, Table 1 displays that the 158 enhanced care employees were statistically comparable to the 168 usual care employees on all baseline characteristics. The intervention increased antidepressant medication months (8.9 versus 8.0, P = 0.10) and any specialty care counseling (40.9% versus 25,8%, P < 0.05) over 2 years. Table 2 shows that with a limited impact on depression severity (F = 2.72, P = 0.09, df = 1799) and no impact on emotional role functioning (−2LL χ2 = 1.8, P = 0.41, df = 2), the intervention significantly improved productivity (−2LL χ2 = 6.0, P < 0.05, df = 2) and tended to improve absenteeism (−2LL χ2 = 5.6, P = 0.06, df = 2). Figure 2 illustrates that the intervention improved productivity by 6.1% over 2 years at an estimated annual value of $1491 per depressed FTE. Figure 3 illustrates that the intervention tended to reduce absenteeism by 22.8% or 10.6 days over 2 years at an estimated annual value of $539 per depressed FTE. Sensitivity analyses indicated that intervention effects on productivity and absenteeism were comparable across occupational categories and paid sick leave benefits.
FIGURE 2.
Intervention effects on productivity.
FIGURE 3.
Intervention effects on absenteeism.
In the analysis of consistently employed subjects, Table 1 shows that the 96 enhanced care employees were comparable to the 102 usual care subjects on all baseline characteristics except physical comorbidities (included as a covariate in all models). The intervention significantly increased antidepressant medication months (9.1 versus 7.8, P < 0.05) and any specialty care counseling (41.3% versus 23.2%, P < 0.05) over 2 years. Table 2 shows that with a significant impact on depression severity (F = 5.15, P = 0.02, df = 1609) and emotional role functioning (−2LL χ2 = 8.1, P < 0.03, df = 2), the intervention significantly improved productivity (−2LL χ2 = 7.8, P = 0.03, df = 2) and tended to improve absenteeism (−2LL χ2 = 5.1, P = 0.08, df = 2). Figure 2 illustrates that the intervention improved productivity by 8.2% over 2 years at an estimated annual value of $1982 per depressed FTE. Figure 3 illustrates that the intervention tended to reduce absenteeism by 28.4% or 12.3 days over 2 years at an estimated annual value of $619 per depressed FTE.
In the analysis of inconsistently employed subjects, Table 1 displays that enhanced and usual care employees were statistically comparable on all baseline characteristics. The intervention did not increase antidepressant medication months (8.3 versus 8.7, P > 0.20) or any specialty care counseling (36.7% versus 35.1%, P > 0.20) over 2 years. Table 2 demonstrates that concurrent with its insignificant effect on depression severity (F = 0.24, P = 0.62, df = 1188) and emotional role functioning (−2LL χ2 = 3.6, P = 0.16, df = 2), the intervention had no significant impact on productivity (−2LL χ2 = 0.0, P = 0.99, df = 2) or absenteeism (−2LL χ2 = 0.9, P = 0.64, df = 2). Figures 2 and 3 illustrate the magnitude of the intervention's nonsignificant effects on productivity and absenteeism.
DISCUSSION
Employers have repeatedly asked for evidence of the value of health interventions using business-relevant metrics.30 Productivity at work is an important business-relevant metric whose depression-specific costs to corporate America are beginning to be convincingly quantified.11 As hypothesized, the intervention increased productivity over 2 years by 6.1% in all depressed workers and 8.2% in consistently employed depressed workers, improvements comparable to the gains associated with the introduction of medications with reduced side effect profiles.31,32 The annual economic benefit associated with this improvement in consistently employed populations is substantial, estimated at $1982 per depressed FTE. Over the short term, improvements in productivity generally benefit the majority of American employers who pay salaries rather than reimburse workers for piecework or by commission. Over the longer term, improvements in productivity may translate into employee raises.33
Absenteeism is a second important business-relevant metric, reflecting that employers spend an average of 1.9% of payroll expenditures on sick leave benefits.34 Major depression is a substantial but addressable contributor to absenteeism. Improved depression management reduces absenteeism by 22.8% in all depressed workers and by 28.4% in consistently employed depressed workers. The intervention provides annual economic benefits from reduced absenteeism estimated at $619 per depressed FTE to employers who provide sick leave to consistently employed subjects. Employers who pay replacement workers overtime, hire temporary workers, or incur productivity losses from coworkers when depressed workers are absent may realize additional benefits.
The improvements in absenteeism and productivity we observed in the total cohort were largely due to the improvements consistently employed workers realized from intervention. The intervention we tested improved depression treatment and outcomes in consistently employed workers, but not in inconsistently employed workers. Recognizing that we had limited power to find statistically significant differences in this subgroup, we suspect that inconsistently employed workers have barriers to high quality depression treatment that quality improvement interventions like ours have not adequately addressed. Further research is needed to develop and test a refined intervention for its ability to improve treatment and labor outcomes in this potentially vulnerable population.
These findings suggest that formal cost-benefit analyses from the employer perspective need to be undertaken to determine whether employers achieve a cost offset from efforts to improve depression management in consistently employed workforces. These evaluations would be strengthened by better estimates of how improved depression treatment impacts short/long-term disability35,36 and workplace injury. If the accumulating evidence establishes clear economic incentives for companies to advocate for better mental health treatment for their workers, employers may find it useful to: (1) select (or encourage employees to select) health plans that provide the high quality care these interventions produce; (2) encourage current plans to select depression as the focus for already budgeted quality improvement initiatives; or (3) pay current plans to sponsor depression quality improvement initiatives. Interested employers should assure themselves that depression quality improvement initiatives are at or above the intensity and duration tested here since less intensive initiatives generally have little to no impact on functioning.37-41 Health plans may also wish to direct existing quality improvement resources or allocate new resources to provide depression quality improvement initiatives to increase their marketability to employers.
The internal validity of findings characterizing the effects of ongoing intervention on productivity and absenteeism is strengthened by conducting an intent to treat analysis of data from a randomized study that included employees regardless of the intervention dose they received or the duration of their employment. Because the study was conducted in workers employed across the occupational spectrum by companies across the country, we relied on self-report to measure productivity and absenteeism. While we employed a carefully validated measure of absenteeism,27 we were not able to differentiate absenteeism due to depression from absenteeism due to other health problems. While this is clearly a limitation in understanding how the intervention worked, it is less of an issue for employers who realize benefits from reduced absenteeism for any health problem. Widely used32,42-44 but less psychometrically established, the self-report productivity item we used correlates 0.76 in this population with the self-reported Work Limitation Questionnaire,45 which predicts objectively measured productivity without bias from depression severity.26 Future investigations are encouraged to use more extensively validated indicators of productivity to obtain better estimates of the intervention's economic impact. Although we could not observe productivity or absenteeism between waves, we suspect that the indicators we analyzed do not bias our estimate of intervention effectiveness because they introduce comparable amounts of measurement error to both enhanced and usual care groups. Noting that the intervention does not increase consistent employment over 2 years (data available from authors on request), we recognize the possibility that the intervention increased the outcomes we measured at the expense of other outcomes we did not measure (eg, enhanced care patients moved to jobs with less responsibility); however, we think this possibility is remote. The study was not designed to identify which component(s) of the intervention account for the improved outcomes, although previous experimental research37,38 allows us to confidently rule out the ‘active ingredient’ was feeding back the diagnosis to the PCP. Sensitivity analyses excluding part-time employees produce virtually identical findings for full-time employees, reflecting that almost 80% of the sample was employed full time at baseline.
The external generalizability of our findings is strengthened because we tested a practical intervention implemented by primary care professionals under naturalistic practice conditions in a diverse group of workers employed at a variety of levels by multiple companies across the country. Baseline productivity rates in this sample appear to be comparable to previously published depressed primary care samples,42 while baseline absenteeism rates are slightly higher than community-sampled workers with major depression.2 While we acknowledge our sample was not selected to be representative of all occupations and industries across the country, it is encouraging that the intervention effect on absenteeism and productivity is robust across diverse occupational groups and across employees with and without sick leave benefits. Because the wage rates of subjects in this study are only 82% of the national average46 and we do not include fringe benefits in our FTE daily wage estimate, our characterization of the economic value of this intervention is probably conservative. We did not require patients to be employed at baseline because we wanted to study how depression interventions impact labor outcomes in inconsistently as well as consistently employed individuals. While we achieved comparable 2-year follow-up rates to other effectiveness studies in this area,47 we attempted to enhance generalizability by using modeling techniques for projecting trends over time in longitudinal studies with sample attrition and found no evidence of nonignorable missingness. We note that enhanced care sites probably changed their practice following brief training in ways that nonresearch sites might not because enhanced care sites recognized they were part of a study, suggesting that the type, intensity, and duration of care management needs to be monitored as primary care depression interventions are adopted into routine care settings.
To our knowledge, this is the first trial to demonstrate that interventions to improve the quality of care provided workers for any chronic disease have positive consequences for productivity and absenteeism. Corporations employing stable workforces whose business interests are served by present and productive workers have reason to encourage health plans to improve primary care depression treatment. In ensuring benefits for themselves, corporations may also contribute to improving their employees' lives.
ACKNOWLEDGMENTS
The authors wish to acknowledge the physicians, office staff, and patients of participating primary care practices: Chatham Primary Care, Siler City, North Carolina; Dunes Family Health Care, Reedsport, Oregon; Eau Claire Family Medicine, Eau Claire, Wisconsin; Enid Family Medicine Clinic, Enid, Oklahoma; Fergus Falls Medical Group, Fergus Falls, Minnesota; Health East Eastside Medical Center, St. Paul, Minnesota; Lynchburg Family Practice, Lynchburg, Virginia; Mile Bluff Clinic, Mauston, Wisconsin; Mountain Area Family Health, Asheville, North Carolina; Northern Colorado Family Medicine, Greeley, Colorado; Oakwood Health Care Center, Westland, Michigan; Somerset Family Practice, Somerville, New Jersey; and University of North Dakota Center for Family Medicine, Minot, North Dakota. Lastly, we acknowledge our colleagues in the Quality in Depression (QID) Cooperative Agreement, Naihua Duan, Carl Elliott, Richard Frank, Robert Gibbons, Willard Manning, Debra Lerner, Hong Chang, Paul Nutting, and Stephanie Mitchell for their sound advice and assistance.
Footnotes
Supported by the National Institute of Mental Health MH54444, MH63651, the MacArthur Foundation, and the Robert Wood Johnson Foundation.
Selected components of this analysis have been presented at the National Health Care Purchasing Institute (Robert Wood Johnson Foundation) Conference on Making the Business Case for Improving Mental Health Care, Washington, DC, in December 2002, and the NIMH Fifteenth Biennial International Conference on Mental Health ‘Evidence in Mental Health Services Research: What Types, How Much, and Then What?’ Washington, DC, in April 2002.
REFERENCES
- 1.Druss BG, Marcus SC, Olfson M, et al. Comparing the national economic burden of five chronic conditions. Health Aff. 2001;20:233–241. doi: 10.1377/hlthaff.20.6.233. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Psychol Med. 1997;27:861–873. doi: 10.1017/s0033291797004807. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Barber C, Birnbaum HG, et al. Depression in the workplace: effects on short-term disability. Health Aff. 1999;18:163–171. doi: 10.1377/hlthaff.18.5.163. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Mickelson KD, Barber C, et al. The effects of chronic medical conditions on work impairment. In: Rossi AS, editor. Caring and Doing for Others: Social Responsibility in the Domains of the Family, Work and Community. University of Chicago Press; Chicago: 1999. [Google Scholar]
- 5.Greenberg PE, Kessler RC, Nells TL, et al. Depression in the workplace: an economic perspective. In: Feighner JP, Boyer WF, editors. Selective Serotonin Re-Uptake Inhibitors: Advances in Basic Research and Clinical Practice. John Wiley & Sons, Ltd.; Chichester, West Sussex, UK: 1996. [Google Scholar]
- 6.Russell JM, Patterson J, Baker AM. Depression in the workplace: epidemiology, economics and effects of treatment. Disease Manage Health Outcomes. 1998;4:135–142. [Google Scholar]
- 7.Conti DJ, Burton WN. Behavioral health disability management. In: Oher JM, editor. The Employee Assistance Handbook. John Wiley & Sons, Inc.; New York: 1999. [Google Scholar]
- 8.Martin JK, Blum TC, Beach SRH, et al. Subclinical depression and performance at work. Social Psychiatry Psychiatric Epidemiol. 1996;31:3–9. doi: 10.1007/BF00789116. [DOI] [PubMed] [Google Scholar]
- 9.Burton WN, Conti DJ. The real measure of productivity. Business & Health. 1999;17:34–36. [PubMed] [Google Scholar]
- 10.Burton WN, Conti DJ, Chen C, et al. The role of health risk factors and disease on worker productivity. J Occup Environ Med. 1999;41:863–877. doi: 10.1097/00043764-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Stewart WF, Ricci JA, Chee E, et al. Cost of lost productive work time among US workers with depression. JAMA. 2003;289:3135–3144. doi: 10.1001/jama.289.23.3135. [DOI] [PubMed] [Google Scholar]
- 12.Rost K, Nutting P, Smith J, et al. Improving depression outcomes in community primary care practice: A randomized trial of the QuEST intervention. J Gen Intern Med. 2001;16:143–149. doi: 10.1111/j.1525-1497.2001.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coulehan JL, Schulberg HC, Block MR, et al. Treating depressed primary care patients improves their physical, mental, and social functioning. Arch Intern Med. 1997;157:1113–1120. [PubMed] [Google Scholar]
- 14.Katzelnick DJ, Simon GE, Pearson SD, et al. Randomized trial of a depression management program in high utilizers of medical care. Arch Fam Med. 2000;9:345–351. doi: 10.1001/archfami.9.4.345. [DOI] [PubMed] [Google Scholar]
- 15.Wells KB, Sherbourne CD, Schoenbaum M, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000;283:212–220. doi: 10.1001/jama.283.2.212. [DOI] [PubMed] [Google Scholar]
- 16.Nutting PA, Rost K, Dickinson M, et al. Barriers to initiating depression treatment in primary care practice. J Gen Intern Med. 2002;17:103–111. doi: 10.1046/j.1525-1497.2002.10128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith LA, Romero D, Wood PR, Nutting PA, Rost K, Dickinson M. Employment barriers among welfare recipients and applicants with chronically ill children. Am J Public Health. 2002;92:1453–1457. doi: 10.2105/ajph.92.9.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson SG, Julnes G, Schuldt R. Job stability and wage progression patterns among early TANF leavers. J Sociol Social Welfare. 2000;27:39–59. [Google Scholar]
- 19.Bound J, Schoenbaum M, Waidmann T. Race and education differences in disability status and labor force attachment in the Health and Retirement Survey. J Human Resources. 1995;30:S227–S267. [Google Scholar]
- 20.Connelly R. The effects of child care costs on married women's labor force participation. Rev Econ Stat. 1992;74:83–90. [Google Scholar]
- 21.Danziger SK, Kalil A, Anderson NJ. Human capital, physical health, and mental health of welfare recipients: co-occurrence and correlates. J Soc Issues. 2000;56:635–654. [Google Scholar]
- 22.Kessler RC, House JS, Turner JB. Unemployment and health in a community sample. J Health Soc Behav. 1987;28:51–59. [PubMed] [Google Scholar]
- 23.Rost K, Nutting PA, Smith J, et al. Designing and implementing a primary care intervention trial to improve the quality and outcome of care for major depression. Gen Hosp Psychiatry. 2000;22:66–77. doi: 10.1016/s0163-8343(00)00059-1. [DOI] [PubMed] [Google Scholar]
- 24.Depression Guideline Panel: Depression in Primary Care: Volume 1. Detection and Diagnosis. Clinical Practice Guideline, Number 5. US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; Rockville, MD: 1993. (AHCPR Publication No. 93–0550). [Google Scholar]
- 25.Depression Guideline Panel: Depression in Primary Care: Volume 2. Treatment of Major Depression. Clinical Practice Guideline, Number 5. US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; Rockville, MD: 1993. (AHCPR Publication No. 93–0551). [Google Scholar]
- 26.Lerner D, Amick BC, III, Lee JC, et al. Relationship of employee-reported work limitations to work productivity. Med Care. 2003;41:649–659. doi: 10.1097/01.MLR.0000062551.76504.A9. [DOI] [PubMed] [Google Scholar]
- 27.Revicki DA, Irwin D, Reblando J, et al. The accuracy of self-reported disability days. Med Care. 1994;32:401–404. doi: 10.1097/00005650-199404000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Ware JE, Jr, Kosinski M, Bayliss MS, et al. Comparison of methods for the scoring and statistical analysis of the SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. >Med Care. 1995;33:AS264–AS279. [PubMed] [Google Scholar]
- 29.Bryk AS, Raudenbush SW. Hierarchical Linear Models: Applications and Data Analysis Methods. 1st Sage Publications; Newbury Park: 1992. [Google Scholar]
- 30.Lynch W, Reidel JE. Measuring Employee Productivity: A Guide to Self-Assessment Tools. Institute for Health and Productivity Management; Denver, CO: 2001. [Google Scholar]
- 31.Meltzer EO, Casale TB, Nathan RA, et al. Once-daily fexofenadine HCI improves quality of life and reduces work and activity impairment in patients with seasonal allergic rhinitis. Ann Allergy Asthma Immunol. 1999;83:311–317. doi: 10.1016/S1081-1206(10)62671-3. [DOI] [PubMed] [Google Scholar]
- 32.Dasbach EJ, Carides GW, Gerth WC, et al. Work and productivity loss in the rizatriptan multiple attack study. Cephalalgia. 2000;20:830–834. doi: 10.1046/j.1468-2982.2000.00126.x. [DOI] [PubMed] [Google Scholar]
- 33.Sturm R, Wells KB. How can care for depression become more cost-effective? J Am Med Assoc. 1995;273:51–58. [PubMed] [Google Scholar]
- 34.CCH, Inc. CCH Unscheduled Absence Survey 2003http://onlinestore.cch.com.Accessed September 13, 2004
- 35.Birnbaum HG, Cremieux PY, Greenberg PE, et al. Management of major depression in the workplace: Impact on employee work loss. Dis Manage Heath Outcomes. 2000;7:163–171. [Google Scholar]
- 36.Salkever DS, Goldman H, Purushothaman M, et al. Disability management, employee health and fringe benefits, and long-term-disability claims for mental disorders: An empirical exploration. Milbank Q. 2000;78:79–113. doi: 10.1111/1468-0009.00162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dowrick C, Buchan I. Twelve month outcome of depression in general practice: Does detection or disclosure make a difference? Br Med J. 1995;311:1274–1276. doi: 10.1136/bmj.311.7015.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Linn LS, Yager J. The effect of screening, sensitization, and feedback on notation of depression. J Med Educ. 1980;55:942–949. doi: 10.1097/00001888-198011000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Brown JB, Shye D, McFarland BH, et al. Controlled trials of CQI and academic detailing to implement a clinical guideline for depression. Jt Comm J Q Improv. 2000;26:39–54. doi: 10.1016/s1070-3241(00)26004-5. [DOI] [PubMed] [Google Scholar]
- 40.Thompson C, Kinmonth AL, Stevens L, et al. Effects of a clinical-practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire Depression Project randomised controlled trial. Lancet. 2000;355:185–191. doi: 10.1016/s0140-6736(99)03171-2. [DOI] [PubMed] [Google Scholar]
- 41.Lin EHB, Katon WJ, Simon GE, et al. Achieving guidelines for the treatment of depression in primary care: Is physician education enough? Med Care. 1997;35:831–842. doi: 10.1097/00005650-199708000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Kroenke K, West SL, Swindle R, et al. Similar effectiveness of paroxetine, fluoxetine, and sertraline in primary care: a randomized trial. JAMA. 2001;286:2947–3004. doi: 10.1001/jama.286.23.2947. [DOI] [PubMed] [Google Scholar]
- 43.Jacobs RJ, Davidson JRT, Gupta S, et al. The effects of clonazepam on quality of life and work productivity in panic disorder. Am J Manage Care. 1997;3:1187–1196. [PubMed] [Google Scholar]
- 44.Laloux P, Vakaet A, Monseu G, et al. Subcutaneous sumatriptan compared with usual acute treatments for migraine: Clinical and pharmaco-economic evaluation. Acta Neurol Belgica. 1998;98:332–341. [PubMed] [Google Scholar]
- 45.Lerner D, Amick BC, III, Rogers WH, et al. The Work Limitations Questionnaire. Med Care. 2000;39:72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 46.Bureau of Labor Statistics National Compensation Survey: Occupational Wages in the United States, 2000. Summary. 2002:01–04. [Google Scholar]
- 47.Sherbourne CD, Wells KB, Duan N, et al. Long-term effectiveness of disseminating quality improvement for depression in primary care. Arch Gen Psychiatry. 2001;58:696–703. doi: 10.1001/archpsyc.58.7.696. [DOI] [PubMed] [Google Scholar]