Abstract
The 1952 Copenhagen poliomyelitis epidemic provided extraordinary challenges in applied physiology. Over 300 patients developed respiratory paralysis within a few weeks, and the ventilator facilities at the infectious disease hospital were completely overwhelmed. The heroic solution was to call upon 200 medical students to provide round-the-clock manual ventilation using a rubber bag attached to a tracheostomy tube. Some patients were ventilated in this way for several weeks. A second challenge was to understand the gas exchange and acid-base status of these patients. At the onset of the epidemic, the only measurement routinely available in the hospital was the carbon dioxide concentration in the blood, and the high values were initially misinterpreted as a mysterious “alkalosis.” However, pH measurements were quickly instituted, the PCO2 was shown to be high, and modern clinical respiratory acid-base physiology was born. Taking a broader view, the problems highlighted by the epidemic underscored the gap between recent advances made by physiologists and their application to the clinical environment. However, the 1950s ushered in a renaissance in clinical respiratory physiology. In 1950 the coverage of respiratory physiology in textbooks was often woefully inadequate, but the decade saw major advances in topics such as mechanics and gas exchange. An important development was the translation of the new knowledge from departments of physiology to the clinical setting. In many respects, this period was therefore the beginning of modern clinical respiratory physiology.
Keywords: pulmonary gas exchange, pulmonary mechanics, mechanical ventilation, acid-base balance, clinical physiology
IN 1952, COPENHAGEN was struck by a severe epidemic of poliomyelitis that included a large number of cases of bulbar polio resulting in respiratory paralysis. During the period from August to December, about 3,000 patients with polio were admitted, mainly to one infectious disease hospital, the Blegdam Hospital, and of these, about 1,250 had some type of paralysis (Fig. 1). Some 345 patients had bulbar polio affecting the respiratory and swallowing muscles (19, 21). For several weeks, 30–50 patients with bulbar symptoms were admitted daily and 6–12 of these were desperately ill. During the first 3 wk of the epidemic 27 of 31 patients with bulbar polio died, 19 of them within 3 days of admission. Clearly a catastrophe was in the making. Indeed Henry Cai Alexander Lassen (1900–1974), chief physician at the hospital stated “Although we thought we knew something about the management of bulbar and respiratory poliomyelitis it soon became clear that only very little of what we did know at the beginning of the epidemic was really worth knowing” (21).
Fig. 1.
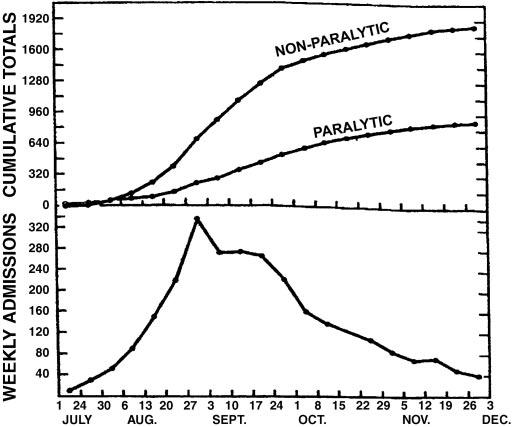
Weekly admissions of patients with poliomyelitis to the Blegdam Hospital in Copenhagen in July to December 1952. Note the very rapid increase in the first part of August. The figure also shows that about half of the patients had some paralysis. From Lassen (19).
The epidemic resulted in two enormous challenges in applied physiology. The hospital lacked ventilators. The stunningly innovative solution was to use manual positive pressure administered by a roster of 200 medical students who repeatedly squeezed a rubber bag attached to a tracheostomy tube around the clock. The second challenge was understanding the life-threatening abnormalities of pulmonary gas exchange and acid-base status. At the start of the epidemic, the only laboratory test available was the total carbon dioxide concentration of the blood, and the high values were interpreted as a mysterious “alkalosis.” Aspects of the epidemic are discussed elsewhere (4, 20, 21, 27, 30, 33, 34).
The problems posed by the epidemic are interesting in their own right. However, the thesis here is that the situation was symptomatic of the parlous state of clinical physiology in the early 1950s. Great advances in respiratory physiology had been made in the 1940s, partly in response to the demands of World War II, but many had not been translated into the clinical setting. The coverage of respiratory physiology in medical student textbooks around 1950 was generally abysmal.
But in the early part of the decade a renaissance occurred that can be exemplified by the publication in 1955 of The Lungby Julius Comroe and his coauthors (9). Indeed the decade ushered in a revolution in applied respiratory physiology that lasted for much of the remainder of the century.
THE POLIOMYELITIS EPIDEMIC
Mechanical ventilation. In the initial stages of the epidemic there was some confusion about the need to ventilate patients with bulbar polio and respiratory insufficiency. Some patients were said to have polioencephalitis or “cerebralia” with a constellation of symptoms and signs, including haziness of consciousness, increased secretions in the airways, long periods of apnea punctuated by occasional inspirations, and obtunding of consciousness from which they could be aroused by verbal stimulation. The relative importance of hypoxia, carbon dioxide retention, fever, and uremia as a cause of this condition was debated (21). There was an impression that some patients had an overwhelming viral bulbar infection for which little could be done, and this led to therapeutic nihilism (20). This group had a very high mortality, and, in retrospect, many of these patients should probably have been ventilated much earlier than they were, if indeed they were ventilated at all.
When it was recognized that many of these patients could not survive without mechanical ventilation, the lack of machines became a serious crisis. At the outbreak of the epidemic the Blegdam Hospital had only one Emerson tank respirator and six cuirass respirators. The latter consisted of jackets that fitted around the chest and assisted ventilation by changing the pressure outside the thorax. Although these were useful for patients with mild respiratory impairment, they were utterly inadequate for cases with respiratory paralysis.
The bold solution was to manually ventilate the patients by squeezing a rubber bag attached to a tracheostomy tube inserted through an incision just below the larynx. The bag was connected to a tank of 50% oxygen in nitrogen together with a soda lime absorber to remove carbon dioxide (Figs. 2 and 3). The logistical problem was solved by having a roster of 200 medical students who operated in relays. At the height of the epidemic, 70 patients had to be manually ventilated around the clock. The medical students worked 6- or 8-h shifts so that three or four shifts were needed in the 24 h. It is daunting to think of the responsibility of these students who were essentially ventilating blind with only the patient’s appearance to guide them, at least in the initial stages. One account refers to a patient rolling her eyes up to signal that she needed more ventilation. Nevertheless the mortality rate is said to have dropped from ∼90% to ∼25% as a result of this heroic intervention.
Fig. 2.
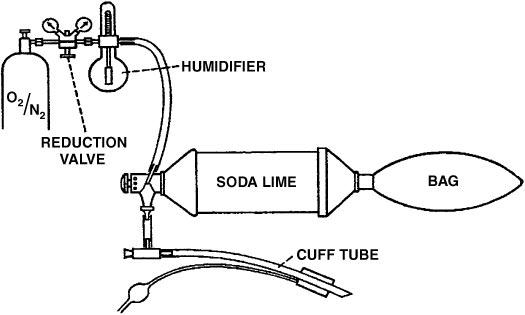
Apparatus for manual mechanical ventilation. The tank was 50% O2-50% N2. At the bottom is the cuffed endotracheal tube that was inserted through a tracheotomy. From Lassen (19).
Fig. 3.

Photograph of a patient being manually ventilated with the apparatus shown in Fig. 2. From Lassen (21).
The demands were so great that the supply of medical students dwindled, and a number of lectures were given at the university to encourage more to volunteer (23). Students from the dental school were also recruited. One report states that 1,500 students in all took part in this activity with a total of 165,000 h (16).
The introduction of manual bag ventilation early in the epidemic was due to the anesthesiologist Bjørn Ibsen (born: 1915) (Fig. 4). He was a Dane who had spent a period in the Department of Anesthesia at the Massachusetts General Hospital under Henry Knowles Beecher (1904–1976). Earlier in 1952, Ibsen had been involved in the treatment of a child with tetanus who was curarized and ventilated manually through a tracheostomy (34). There was a dramatic meeting at the Blegdam Hospital on August 25, 1952, when, as stated earlier, 31 patients with bulbar polio had been treated with the tank and cuirass respirators in the preceding 3 wk but 27 had died. On that day alone, four patients were autopsied, one of them a 12-yr-old boy who died with a “bicarbonate level in the serum far above the normal level.” The attendees included Lassen, Poul Astrup (1915–2000) (Fig. 5), chief of the hospital laboratory, Mogens Bjørneboe, a member of the hospital’s medical staff, and Ibsen, who had apparently somewhat reluctantly been invited to attend by Lassen at the urging of Bjørneboe. Ibsen soon recognized that the high blood bicarbonate levels were not an alkalosis of unknown origin but were caused by severe carbon dioxide retention (4, p. 258). He recommended immediate manual ventilation via a tracheostomy. It is interesting that no successful treatment by positive pressure ventilation given continuously over a long period had been reported by 1950 (12).
Fig. 4.
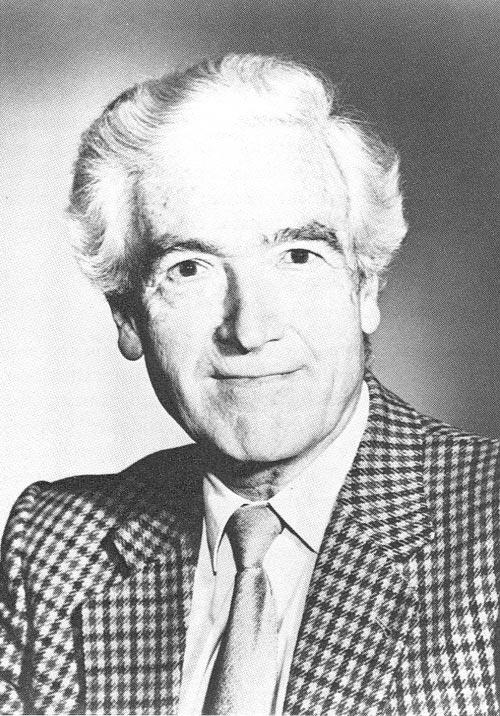
Bjørn Ibsen (1915- ), Danish anesthesiologist who suggested positive pressure ventilation for the patients with respiratory paralysis. From Zorab (36).
Fig. 5.

Poul Astrup (1915–2000) who ushered in the modern period of clinical acid-base physiology. From Severinghaus and Astrup (28).
Ibsen related how the first patient was a 12-year-old girl who had paralysis of all four extremities, had atelectasis of the left lung, and who was gasping for air and drowning in her own secretions (1, 17). She was pyrexic, cyanotic, and sweating. A tracheotomy was done under local anesthesia, a cuffed endotracheal tube was placed, and she was eventually ventilated satisfactorily. This event was a turning point in critical care medicine, partly because it was one of the first occasions when an anesthesiologist moved out of the operating room into another environment. Positive pressure ventilation had previously been used for short periods in a polio epidemic in Los Angeles in 1948–1949 (7, 8), but this work had been published in an obscure journal and was not well known.
The ventilation circuit shown in Figs. 2 and 3 was a semi-closed system similar to that used in many anesthetic machines with the advantage that it required less fresh gas from the tank than an open circuit. The physicians also felt that the buffering effect of the large volume of the circuit made it easier for inexperienced medical students to maintain the appropriate ventilation. The flow meter was set to 5–10 l/min. However, the CO2 absorber incorporated in the circuit caused some problems because of potential aspiration of soda lime particles into the lung. In later versions, the absorber was removed from the circuit and there was simply an inspiratory/expiratory valve at the tracheostomy tube so that expired gas was vented directly into the outside air. This required a higher flow rate from the oxygen/nitrogen tank.
It is interesting to look back at a contemporary discussion of the principles of mechanical ventilation in the clinical setting, for example, Rattenborg (26). There was confusion about the mode of action of positive pressure vs. negative pressure ventilation, and the role of airway resistance on the one hand and lung and chest wall compliance on the other in limiting inflation of the lung. The analysis included a curious statement that negative pressure inflation was unsatisfactory because it did not ensure a constant rate of inspiratory airflow. The reader today is aware of the great contrast between this discussion and the work done in departments of physiology a few years before when the relevant principles of the mechanics of respiration had been clearly enunciated by such groups as Fenn, Otis, and Rahn in the University of Rochester, New York (13), and Mead and Whittenberger and their colleagues at the Harvard School of Public Health (22). This is an example of the prevailing dissociation in the early 1950s between the advances made in departments of physiology on the one hand and their application to clinical situations on the other.
Pulmonary gas exchange and acid-base status. As indicated earlier, a major difficulty in the successful ventilation of these patients was the almost complete lack of laboratory data about pulmonary gas exchange and acid-base status. The clinical symptoms and signs of respiratory insufficiency were vague or simply caused by intense anxiety. Patients felt suffocated and had difficulty in coping with their secretions because they could not swallow, there was cyanosis if they were not being given oxygen, and a clammy skin and hypertension were sometimes seen, presumably the results of increased blood catecholamine levels. The only routine laboratory investigation available was the total carbon dioxide concentration in venous or arterial blood. The clinical laboratory of the Blegdam Hospital had a pH meter that could be used for blood, but it required a large sample volume and could not be used for frequent or routine measurements. As stated earlier, the very high levels of carbon dioxide concentration were initially attributed to a mysterious alkalosis, and it was Ibsen who first recognized at the time of the epidemic that instead they signaled a severe respiratory acidosis although this had previously been suggested (24).
Astrup related that “this outright misinterpretation of a high CO2 content as alkalosis in patients with respiratory insufficiency produced a very deep impression on me as a laboratory man” (4, p. 258). Astrup was able to persuade the Radiometer A/S in Copenhagen to provide him with a smaller pH meter that could be used for blood (27). A quick measurement of blood pH at 38°C soon proved Ibsen right, and this led to the 12-yr-old girl being tracheotomized and given manual positive pressure ventilation that immediately caused the “alkalosis” to disappear. Astrup noted that the value of the carbon dioxide concentration of blood as an index of its alkalinity could be traced all the way back to 1877 when it was described by Friedrich Walter (born: 1850) and in its time was a very valuable contribution, but clearly here was a situation where the concept was misleading. In defense of the misconceptions of the clinicians in the early 1950s, it should be added that it was unusual to request laboratory data in patients with abnormalities of ventilation.
A top priority was to measure the PCO2 in the blood, and this was done using the Henderson-Hasselbalch equation. The graphical depiction of this by Van Slyke and Sendroy (32) was well known to Astrup, and their original diagram is reproduced in Fig. 6. The vertical line on the extreme left shows the total carbon dioxide content of blood both in milliliters of CO2 per deciliter of blood and in micromolar concentrations, whereas the central and right-hand lines show the plasma pH and PCO2, respectively. A line has subsequently been added joining the normal pH of 7.4 and normal PCO2 of 40 mmHg to show a total CO2 content of about 56 ml CO2 per deciliter of blood.
Fig. 6.
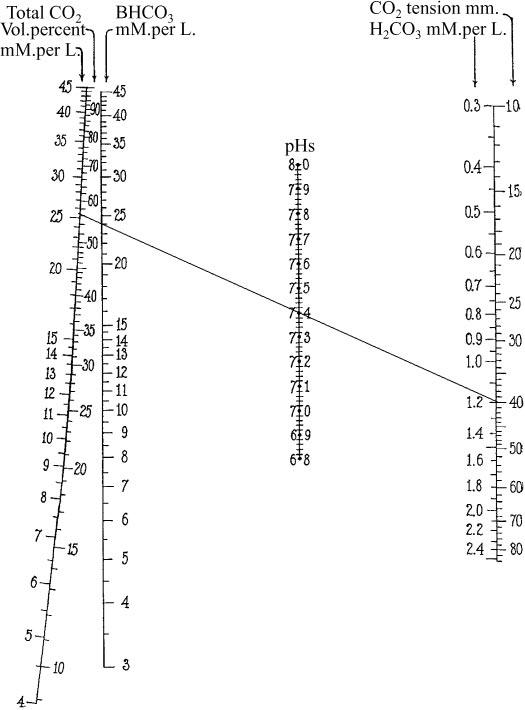
Nomogram that was used for determining the blood PCO2 from the total CO2 content and plasma pH. From Van Slyke and Sendroy (32).
The carbon dioxide concentration was determined using the manometric method described by Van Slyke and O’Neill (31). As mentioned earlier, the normal laboratory blood pH meter at the time required a large sample size. However, when the smaller pH meter became available from Radiometer, more than 700 pH determinations were made in the Blegdam Hospital over the next 4 mo (3).
Nevertheless this method for determining the PCO2 of blood was still cumbersome because the Van Slyke manometric method was so time consuming. Astrup later realized that if a sample of either plasma or whole blood was exposed to different CO2 partial pressures, the resulting change in pH was linearly related to the logarithm of the PCO2 within the clinical range (2). First the pH of the sample of plasma or blood was measured. Then the sample was exposed to gas with high and low PCO2 values (for example, about 80 and 15 mmHg), and the pH for each PCO2 was measured. The actual PCO2 was then obtained by interpolation. This rapid interpolation method was extensively used until the CO2 electrode was eventually introduced several years later.
The early measurements of pH and PCO2 on the patients from the Copenhagen epidemic who were manually ventilated sometimes showed dramatic changes within short periods of time. Table 1 shows an example from a 5-yr-old boy who was almost moribund on admission and then was tracheotomized and manually ventilated (3). Note that the pH rose from 6.99 to 7.65 over a 3.5-h period and the PCO2 fell from 150 (in venous blood) to 14 mmHg (in arterial blood)!
Table 1.
Blood pH and PCO2 values in a 5-yr-old boy after the onset of manual ventilation
| Hour | Blood | pH | PCO2, mmHg | CO2 conc, mmol | Bicarbonate, mmol |
|---|---|---|---|---|---|
| 11:40 AM | venous | 6.99 | 150 | 39.0 | 34.5 |
| 2:10 PM | arterial | 7.52 | 32 | 24.4 | 24.5 |
| 3:05 PM | arterial | 7.65 | 14 | 15.6 | 15.2 |
Modified from Astrup et al. (3).
In another patient, a woman aged 30 yr, the pH and PCO2 were monitored over a series of 13 days (Table 2). The fact that a number of the measurements were made on venous rather than arterial blood complicates the interpretation somewhat, but it can be seen that the PCO2 remained fairly stable in the low 30s until September 10 when, in a venous sample, it had fallen to 17 mmHg! This was the result of a decision made at a conference on September 10 to increase the rate of manual ventilation in all patients from 20 to 30 breaths/min. However, because a number of patients subsequently showed very low PCO2 values, it was then decided to reduce the ventilation frequency to 25 breaths/min. In the patient shown in Table 2, the PCO2 then rose to 23 mmHg.
Table 2.
Blood pH and PCO2 values in a 30-yr-old woman during manual ventilation over 13 days
| Date | Hour | Blood | pH | PCO2, mmHg |
|---|---|---|---|---|
| Sept 1 | 1:00 PM | venous | 7.49 | 32 |
| 4:45 PM | venous | 7.47 | 31 | |
| 2 | 9:15 AM | venous | 7.50 | 32 |
| 10:30 AM | arterial | 7.50 | 36 | |
| 10:35 AM | venous | 7.47 | 34 | |
| 2:15 PM | venous | 7.48 | 36 | |
| 4 | 9:10 AM | venous | 7.55 | 30 |
| 6 | 10:55 AM | arterial | 7.55 | 30 |
| 8 | 12:35 PM | venous | 7.56 | 31 |
| 10 | 10:10 AM | venous | 7.70 | 17 |
| 13 | 10:10 AM | venous | 7.56 | 23 |
Modified from Astrup et al. (3).
Note that all these PCO2 values were abnormally low, and it is likely that most of the patients who were ventilated by the inexperienced medical students were in this situation. Of course, hyperventilation was better than hypoventilation under these conditions. A common observation in patients who are mechanically ventilated over long periods is that they complain of “air hunger” if the PCO2 is allowed to rise to near the normal level of 40 mmHg.
In 1953, there was another poliomyelitis epidemic, this time in Stockholm, and with the experience obtained in Copenhagen in the previous year, the management of patients with respiratory paralysis had improved. Nevertheless several pH values over 7.6 were reported in arterial blood (18).
A further fallout from these early measurements of pH, PCO2, and bicarbonate in blood were other indexes that improved our understanding of the respiratory and metabolic components of acid-base disturbances particularly when complicated mixed situations occurred. One measurement was the “standard bicarbonate,” which was the plasma bicarbonate concentration when the blood was exposed to a gas of normal PCO2 of 40 mmHg. This was often obtained by having the laboratory technician exhale over it! In effect, this measurement removed the respiratory component of the acid-base disturbance and allowed any metabolic compensation to be recognized. A similar concept had been suggested earlier by Van Slyke and also by Hasselbalch.
However, the most useful fallout was the concept of “base excess.” A simple way to represent this is the position of the “blood buffer line” on a diagram relating plasma bicarbonate concentration to pH, often known as the Davenport diagram (11). The blood buffer line shows the relationship between bicarbonate concentration and pH as CO2 (or carbonic acid) is added to or subtracted from a blood sample. The vertical position of the line is a measure of metabolic compensation for acidosis or alkalosis and is measured in milliequivalents per liter. These fundamental advances in our understanding of acid-base physiology by Astrup and collaborators were later amplified by Siggaard-Andersen and others (29).
THE RENAISSANCE IN CLINICAL RESPIRATORY PHYSIOLOGY DURING THE 1950S
Respiratory physiology in textbooks around 1950. The 1952 Copenhagen poliomyelitis epidemic dramatically demonstrated the uncertainties in clinical respiratory physiology in the areas of mechanical ventilation and gas exchange and is remarkable in its own right. However, it was also symptomatic of the slowness in translating important advances that had been made in the 1940s into the clinical setting. One way to emphasize this is to examine textbooks of physiology for medical students published around 1950. A good example is the textbook Physiological Basis of Medical Practice by Charles Herbert Best (1899–1978) and Norman Burke Taylor (born: 1885) which was first published in 1937 and met with great success. New editions appeared in 1939, 1943, and 1945, with a 5th edition in 1950. The book was reprinted 15 times between 1937 and 1950, and the 5th edition probably gives a good overview of what doctors learned at that time. Parenthetically, this was the textbook that I used during my medical course in Australia in the late 1940s.
Several sections were certainly adequate by the standards of the day. The basic gas laws were well summarized and there were good chapters on the carriage of oxygen and carbon dioxide by the blood, because these topics had been well worked out. However, the sections on pulmonary mechanics and pulmonary gas exchange can only be described as abysmal. There is a whole chapter titled “The mechanics of respiration,” but this is mainly concerned with the respiratory muscles, the consequences of pneumothorax, and a discussion of bronchiectasis! The chapter includes two pages on “artificial respiration” with a diagram of the Drinker negative pressure “iron lung,” but the rest of the discussion is about Schafer’s method, which consists of pressing the lower ribs of a prone subject with the hands, and Eve’s rocking method in which the patient is tilted from the head-up to head-down position and back again on a rocking bed, and the diaphragm is displaced by gravity. Positive pressure ventilation is not even mentioned. The only other place where the topic of the mechanics of breathing occurs is in short sections on asthma and “chronic emphysema” with vague references to the resistance of the airways and the elastic properties of the lung. There is no quantitative treatment of these important topics.
Pulmonary gas exchange also gets very short shrift mainly in a section titled “Anoxia.” Again this is entirely qualitative. The importance of ventilation in eliminating carbon dioxide is not appreciated. Indeed one important factor in CO2 retention is thought to be the slower rate of diffusion of CO2 in the alveolar gas because of the large size of the molecule! There is no hint of the alveolar ventilation as determining the alveolar PCO2 nor the alveolar gas equation that relates the alveolar PO2 to the inspired PO2 and alveolar PCO2. It is hardly surprising in view of this state of knowledge that the clinicians faced with patients with respiratory paralysis were at a loss. It is extraordinary that the respiration section of the 5th edition of Best and Taylor published in 1950 is very similar to that in the 1st edition of 1937.
Another popular medical student textbook of physiology current at about the same time in 1948 had similar coverage of the respiratory system (35). In particular, the section on “artificial respiration” included the same procedures and there was a remarkable footnote. “Schafer’s method is, however, frequently not applicable in cases where patients stop breathing on the operating table. Here the prone position on the floor is rarely possible; the rocking method or compression of the chest or abdomen, may have to be employed.” It is extraordinary that even in this situation the possibility of positive pressure ventilation was not envisaged. It was not until the 9th edition published in 1952 that positive pressure ventilation was mentioned and then only in one sentence in the setting of anesthesia.
Contributions of physiologists in the 1940s and early 1950s. This unhappy state of affairs contrasts greatly with the work that was being done in departments of physiology and in some departments of medicine in the 1940s. Just to take a few examples, Wallace Fenn, Hermann Rahn, and Arthur Otis at the University of Rochester, New York, had established many of the principles of pulmonary mechanics and pulmonary gas exchange during the war years with publications occurring during the mid- and late 1940s (15). Much of this work did not appear initially in the open literature but was contained in classified reports that were later released in eight volumes, the first being Fenn et al. (14). Subsequently some, although not all, of the papers were published in the Journal of Applied Physiology and elsewhere. Another productive group included Jere Mead, James Whittenberger, and their colleagues in the Harvard School of Public Health. Julius Comroe had an active research team in the Graduate School of Medicine at the University of Pennsylvania (see below). Richard Riley, Andre Cournand, and their coworkers were breaking new ground in New York on pulmonary gas exchange, and beginning in 1941 Andre Cournand and Dickinson Richards with their colleagues developed cardiac catheterization in humans (10). Incidentally, this Nobel prize work is not mentioned in the 1948 Best and Taylor.
This rapid acceleration of research was not confined to departments of physiology or to the United States. In London, UK, there were active groups at St. Bartholomew’s Hospital Medical School and the Post Graduate Medical School, and in South Wales important advances were made in pulmonary function in occupational lung disease. Other groups were active in Canada, France, and South Africa. Physiologists in Germany contributed developments of oximetry and other measuring devices, and a two-volume account of their work is available (15a).
Stimulated in part by these advances, the Journal of Applied Physiology started publication in 1948. Part of the impetus for this was the desire to release to the open literature work that had been described in classified documents during the war. Other periodicals, such as the Journal of Clinical Investigation, published numerous articles in applied clinical physiology. Many of the advances of the 1940s were brought together by Comroe and colleagues in the book Pulmonary Function Tests: Methods in Medical Research, Volume II, which was published in 1950. Readers of this who compared it with the 5th edition of Best and Taylor, which was published in the same year might wonder if they were produced on the same planet.
The role of the book “The Lung...” by Comroe and others. But the most influential of the books in this renaissance of clinical pulmonary physiology was The Lung: Clinical Physiology and Pulmonary Function Tests by Julius Comroe, Robert Forster, Arthur DuBois, William Briscoe, and Elizabeth Carlsen, which was published in 1955. This book made an enormous impression. Comroe stated in the preface that it was based on the Beaumont lecture that he gave to the Wayne County Medical Society in Detroit in February 1954. However, the main basis was a course for pulmonary physicians that was given in March 1953 by Comroe and colleagues in the Department of Physiology and Pharmacology, Graduate School of Medicine, University of Pennsylvania. Robert Forster covered blood gases and diffusion, William Briscoe dealt with ventilation-perfusion inequality and other aspects of gas exchange, Arthur DuBois discussed the mechanics of breathing, and Comroe covered the control of ventilation. DuBois still has his notes of the course, including a memo from Comroe dated February 13, 1953, about the preparation of the “lantern slides.” Figure 7 shows two sketches made by DuBois for the course, and Figure 8 depicts how they were eventually published in The Lung. The physics-based nature of these diagrams forms a striking contrast to the treatment of these topics in the 5th edition of Best and Taylor (5) or the paper by Rattenborg (26). It is a remarkable coincidence that in early 1953 at the same time that the Danish physicians were struggling with the problems posed by the patients with respiratory paralysis, the group at the University of Pennsylvania were laying the foundations for the renaissance in clinical respiratory physiology.
Fig. 7.

Sketches by Arthur Dubois that were prepared for the course on clinical respiratory physiology given at the University of Pennsylvania in March 1953.
Fig. 8.
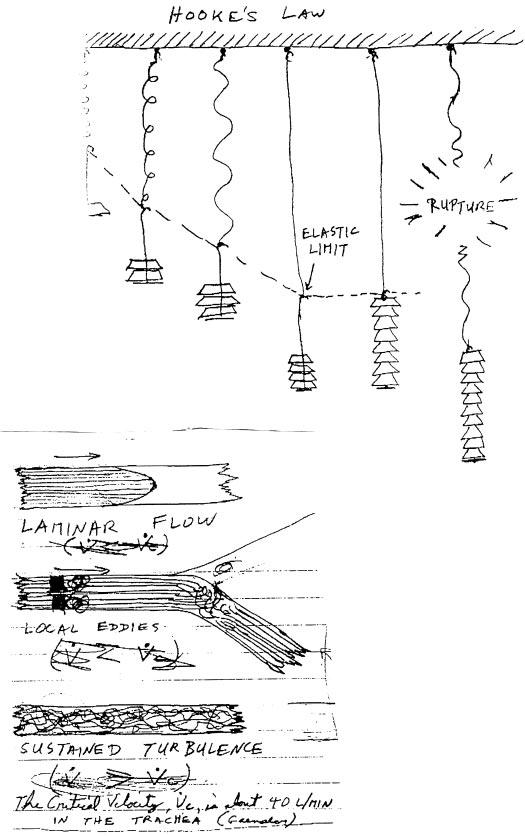
Illustrations from the book The Lung... by Comroe et al. (9) showing how the sketches of Fig. 7 appeared in the book.
The authors of The Lung had no illusions about what they were doing. The preface to the book began “Pulmonary physiologists understand pulmonary physiology reasonably well. Many doctors and medical students do not.” It went on to add “This is not a book for pulmonary physiologists: it is written for doctors and medical students.” This was the quintessential translation from physiology departments where the new work had been done in the 1940s to the medical students and others in the 1950s who desperately needed the new information.
One of the features of the book was the excellent clear illustrations that had been prepared by Carlsen (Fig. 8). The fact that the illustrator, who was a student at the time, was included in the list of authors emphasized the importance that Comroe gave to this feature. Interestingly, although the approach was rigorous and quantitative, the authors were reluctant to include equations in the main text because they felt that most medical students and physicians would be intimidated by these. For example, the alveolar ventilation equation relating the CO2 production to the alveolar ventilation and fraction of CO2 in alveolar gas was given as a footnote. However, all the important equations were summarized in an appendix at the end of the book.
Other seminal publications appeared at about the same time, including the classical short monograph A Graphical Analysis of the Respiratory Gas Exchange: The O2-CO2 Diagram by Rahn and Fenn (25). However, this and similar publications were targeted more at professional physiologists and physiology graduate students than medical students and pulmonary physicians. It was Comroe’s book that really ushered in the renaissance in clinical respiratory physiology.
What was the essential difference between the treatment of pulmonary mechanics and gas exchange in Best and Taylor (5) compared with Comroe et al. (9)? The answer lies in the completely different approaches, one qualitative and the other rigorously quantitative. For example, in Best and Taylor there is not one equation in the sections on airway resistance, elastic properties of the lung, or pulmonary gas exchange. Airway resistance is largely dealt with in a section on asthma where there were statements such as “The expiratory muscles compress the chest and the abdominal muscles contract in the attempt to squeeze the air from the lungs. The intrapulmonary pressure is greatly elevated and the air escapes through the constricted tubes with a distinct wheezing sound.” However, airway resistance is not defined in quantitative terms as the pressure difference divided by flow, and there is no mention of the different modes of air flow such as laminar and turbulent.
The elastic properties of the lung are dealt with in a similar nonquantitative way in the section on “Chronic Emphysema.” For example, a typical statement is “Two factors are concerned in the production of emphysema (a) reduction in the elastic tissue of the lung and (b) increased distension of the alveolar spaces.” There is no mention of the relationship between pressure and volume in an elastic structure nor is the term compliance mentioned.
There is a similar nonquantitative treatment of pulmonary gas exchange mainly in the section on “Chronic Emphysema.” A typical paragraph begins “The cause of the impaired gaseous exchange is not altogether clear. Thickening of the alveolar and capillary walls and the obliteration of capillaries have been considered to be a factor. Yet if this were so one would not expect the retention of carbon dioxide which, owing to its greater solubility (30 times that of oxygen) has a much higher rate of diffusion through the pulmonary membrane, to be so much more pronounced that the anoxia.” Interestingly this passage is followed by a brief statement that uneven ventilation “as a result of the loss of elasticity” could affect gas exchange in some way. However, that is about as far as the text goes on the subject of ventilation-perfusion inequality.
The treatment of these topics in The Lung by Comroe et al. (9) is completely different. The starting point is elementary physics and engineering, and lung elasticity for example is approached through Hooke’s law. The principles of laminar and turbulent flow through tubes are discussed, both of these concepts being alluded to in Figs. 7 and 8. There is a full analysis of the changes in alveolar and intrapleural pressure during the respiratory cycle. Pulmonary gas exchange is dealt with in a quantitative way beginning with the alveolar ventilation equation leading to the alveolar gas equation. The differences between diffusion limitation of gases across the blood-gas barrier and ventilation-perfusion inequality as factors impairing gas exchange are clearly stated. Obviously, there was a revolution in the presentation of the principles of clinical respiratory physiology to medical students and physicians in the early 1950s, and we continue to benefit from this renaissance today.
In summary, the 1952 Copenhagen poliomyelitis epidemic provided momentous challenges in clinical respiratory physiology and is fascinating for that reason. In addition, it underscores the gap that had developed between the rapid advances in respiratory physiology that took place in the 1940s and their application to the clinical environment. This is highlighted by the backward state of respiratory physiology as exemplified in typical medical student textbooks around 1950. However, a remarkable change took place in that decade. The rapid advances made in departments of physiology were translated to the clinical setting with one of the most influential factors being the publication of The Lung by Comroe et al. in 1955. The result was a greatly improved understanding of applied respiratory physiology that continues to benefit patients today.
APPENDIX
Logistics of the long-term manual ventilation. One of the most remarkable features of the epidemic was the way medical students and others were organized to provide round-the-clock, long-term manual ventilation. Information about this is given in three contemporary articles in the Danish medical journal Ugeskrift for Laeger by Thomsen (30), Bjorneboe (6), and Hansen (16). Thomsen was one of the medical student “ventilators,” Bjorneboe was on the medical staff of the Blegdam Hospital, and Hansen was mayor of Copenhagen. Later Wackers (33) interviewed a number of the people involved.
The emotional demands on the patient and student were enormous (30). A young patient would be admitted struggling to breathe, a tracheostomy was performed, and he (or she) would meet the 18- to 19-yr-old students who were to keep him alive by squeezing the bag for an indefinite period. Bonding between the patient and student was strong, especially for young children. Four or five students were allocated to each patient because of the 24-h coverage, but the same students always ventilated the same patient. In the case of young children, the student read to them and played games. If a new student was added to the team for some reason, the patient initially reacted strongly. Communication between the patient and student was difficult because of the tracheostomy tube, but students learned to lip read, and some patients gave information by moving their eyes.
Very early in the epidemic, when it was clear that large numbers of students would be required, the medical student council was involved, and they accepted the responsibility for rostering the students, arranging for them to be excused from otherwise obligatory courses, and negotiating payment for their services. The students worked 6- or 8-h shifts, which was both emotionally and physically demanding. During an 8-h shift, there was a 10-min “smoke” break each hour, and a half-hour meal break in the middle, but otherwise the student was continually compressing the bag.
There were many technical problems connected with the manual ventilation (6). The students first had instruction on the general principles from an anesthesiologist and then 3 or 4 h of practical instruction with the equipment. Equipment problems included unexpected emptying of the oxygen tank, kinking of the tube from the tank, and damage to the ventilating bag. The CO2 absorber had to be changed periodically, and the tracheostomy tube could slip down and occlude a main bronchus. Periodic suctioning of the airways was necessary in some patients.
Observation of the patient was very important, and another student in the team or nurse would monitor the pulse rate and blood pressure from time to time. There was continual surveillance by doctors and nurses walking up and down the wards to give help where needed. Many students found the emotional and physical demands too much and gave up. Also there was a concern about developing polio, although this apparently never happened to any of the students. As the epidemic wore on, the second year students who had done most of the ventilating were partly replaced by first-year students, who, in the European system, would have come straight from high school and might be only 18 yr old.
The economic impact of the epidemic was vast. Very quickly, the Blegdam hospital ran out of beds and three other hospitals were recruited. Large numbers of extra doctors, including anesthesiologists, nurses, and hospital staff were required as well as the medical students. The cost of the epidemic up to April 1953 was estimated to be 5–6 million Danish Kroner (16), that is about 30 million US dollars at today’s exchange rate.
POSTSCRIPT
When this manuscript was being prepared, I wrote to several of the student “ventilators” but received no replies. However, after the paper was accepted for publication, I received a most interesting letter from Dr. Uffe Kirk who was 25 years old in 1952 at the time of the epidemic. He had just finished medical school and was asked to play a major role in organizing the medical student ventilators. Here are some extracts from his account.
“The difference between ordinary patients requiring ventilation and polio patients was characteristic: They were conscious! The students invented ways to communicate with their patients. Some patients holding a small stick in their mouths communicated by pointing at letters on a poster, laboriously spelling what they wanted to say. This went fairly well because the student learned to half-guess what the patient would say after only a few letters. The student would then say out loud what he or she thought the patient meant, and the patient would then wink in one way if the student had guessed right and in another way if not. If the student was in no way near the correct answer, the patient could point at the word “Idiot” written on the poster. This way the student always received a message from the patient if the ventilation required correcting. It was almost a safer way to correct ventilation than laboratory tests, blood pressure, and other medical controls.
The intimate relation made the students very concerned about the well being of their patients. They were exhilarated at every positive sign but were also very sad when things went downhill. And it did for many patients. Even though the students knew that death was a very real option, they were mentally strained when their patients died.
At worst, the patients died during the night. The light in the wards was dimmed in order not to disturb the patients in their sleep. But the faint light and the fact that the students were not able to tell anything from the ventilation made it impossible for the students to know that their patient had died. It was therefore a shock for the student when morning came and he/she realized that the patient had been dead for a while .....
Not so long ago professor Bjørn Ibsen was lauded at a conference here in Denmark. He sat on a chair in the front row when a woman of ∼65 yr quietly went up to him, kissed him on the cheek and said ‘Thank you for my life!’
In 1952 she was the twelve-year old girl whom Bjørn Ibsen was permitted to try and save by means of tracheostomy and a tube through which he wanted to ventilate in replacement of her [paralysed] respiration. He succeeded and the woman was proof of that, and was the direct cause of 1500 medical and dental students ventilating polio patients for 165,000 h at the Blegdam Hospital in 1952 thereby saving ∼100 people who would have been lost without this effort .....”
The complete letter has been placed in an archive in the Mandeville Special Collections Library at the University of California, San Diego.
ACKNOWLEDGMENTS
I thank the following: Arthur DuBois for providing me with a copy of his notes of the course on pulmonary physiology held at the University of Pennsylvania in March 1953; DuBois and Robert Forster for reading the manuscript; Ger Wackers for sending me his doctoral dissertation; and Harrieth Wagner for translating several articles from Danish.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. The article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
GRANTS: The work was supported by National Heart, Lung, and Blood Institute Grant RO1-HL-60698.
REFERENCES
- 1.Andersen EW, Ibsen B. The anaesthetic management of patients with poliomyelitis and respiratory paralysis. Br Med J. 1954;1:786–788. doi: 10.1136/bmj.1.4865.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Astrup P. A simple electrometric technique for the determination of carbon dioxide tension in blood and plasma, total content of carbon dioxide in plasma, and bicarbonate content in separated plasma at a fixed carbon dioxide tension (40 mmHg) Scand J Clin Lab Invest. 1956;8:33–43. doi: 10.3109/00365515609049241. [DOI] [PubMed] [Google Scholar]
- 3.Astrup P, Gotzche H, Neukirch F. Laboratory investigations during treatment of patients with poliomyelitis and respiratory paralysis. Br Med J. 1954;4865:780–786. doi: 10.1136/bmj.1.4865.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Astrup P, Severinghaus J. The History of Blood Gases, Acids and Bases. Munksgaard; Copenhagen: 1986. [Google Scholar]
- 5.Best CH, Taylor NB. The Physiological Basis of Medical Practice. Williams & Wilkins; Baltimore, MD: 1950. [Google Scholar]
- 6.Bjorneboe M. Studenten og poliopatienten. Ugeskr Læger. 1953;115:469–471. [PubMed] [Google Scholar]
- 7.Bower AG, Bennett VR, Dillon JB, Axelrod B. Investigation on the care and treatment of poliomyelitis patients. Ann West Med Surg. 1950;4:561–582. [PubMed] [Google Scholar]
- 8.Bower AG, Bennett VR, Dillon JB, Axelrod B. Investigation on the care and treatment of poliomyelitis patients; II. Physiological studies of various treatment procedures and mechanical equipment. Ann West Med Surg. 1950;4:686–716. [PubMed] [Google Scholar]
- 9.Comroe JH, Forster RE, Dubois AB, Briscoe WA, Carlson RW. The Lung: Clinical Physiology and Pulmonary Function Tests. Year Book; Chicago, IL: 1955. [Google Scholar]
- 10.Cournand A, Ranges HA. Catherization of the right auricle in man. Proc Soc Exp Biol Med. 1941;46:462–466. [Google Scholar]
- 11.Davenport HW. The ABC of Acid-Base Chemistry: the Elements of Physiological Blood-Gas Chemistry for Medical Students and Physicians. University of Chicago Press; Chicago, IL: 1974. [Google Scholar]
- 12.Emerson CG. The clinical application of prolonged controlled ventilation. Acta Anaesthesiol Scand Suppl. 1963;13 [Google Scholar]
- 13.Fenn WO. Mechanics of respiration. Am J Med. 1951;10:77–90. doi: 10.1016/0002-9343(51)90221-5. [DOI] [PubMed] [Google Scholar]
- 14.Fenn WO, Otis AB, Rahn H. AF Technical Report No. 6528. 1951. Studies in Respiratory Physiology. [Google Scholar]
- 15.Fenn WO, Rahn H, Otis AB. A theoretical study of the composition of the alveolar air at altitude. Am J Physiol. 1946;146:637–653. doi: 10.1152/ajplegacy.1946.146.5.637. [DOI] [PubMed] [Google Scholar]
- 15a.German Aviation Medicine: World War II. US Air Force; Washington, DC: 1950. [Google Scholar]
- 16.Hansen J. Den økonomiske baggrund for poliobekæmpelsen. Ugeskr Læger. 1953:471–473. [PubMed] [Google Scholar]
- 17.Ibsen B. The anaesthetist’s viewpoint on the treatment of respiratory complications in poliomyelitis during the epidemic in Copenhagen, 1952. Proc Roy Soc Med. 1954;47:72–74. [PMC free article] [PubMed] [Google Scholar]
- 18.Jungner I, Laurent B. The poliomyelitis epidemic in Stockholm 1953. Biochemical laboratory investigations. Acta Med Scand Suppl. 1956;316:71–79. [PubMed] [Google Scholar]
- 19.Lassen HCA. A preliminary report on the 1952 epidemic of poliomyelitis in Copenhagen with special reference to the treatment of acute respiratory insufficiency. Lancet. 1953;261:37–41. doi: 10.1016/s0140-6736(53)92530-6. [DOI] [PubMed] [Google Scholar]
- 20.Lassen HCA. World Health Organization, Poliomyelitis. World Health Organization; Geneva: 1955. The management of respiratory and bulbar paralysis in poliomyelitis; p. 157. [PubMed] [Google Scholar]
- 21.Lassen HCA. Management of Life-Threatening Poliomyelitis, Copenhagen, 1952–1956, With a Survey of Autopsy-Findings in 115 Cases [translated from the Danish by Hans Andersen and others] Livingstone; Edinburgh: 1956. [Google Scholar]
- 22.Mead J, Whittenberger JL. Physical properties of human lungs measured during spontaneous respiration. J Appl Physiol. 1953;5:779–796. [Google Scholar]
- 23.Medicinske Studenterrådet . En orientering om poliomyelitis. Især med henblik på epidemien 1952. Udarbejdet af de medicinske studenterråd ved Københavns Universitet (på basis af referat fra et møde om poliomyelitis på med. anotomisk institut den 5 november 1952) N. Olaf Møller; København: 1952. [Google Scholar]
- 24.Nielsen HK. Om repiratorbehndling af respirations-pareser ved poliomyelitis anterior acuta. Ugeskr Læger. 1946;108:1341–1348. [Google Scholar]
- 25.Rahn H, Fenn WO. A Graphical Analysis of the Respiratory Gas Exchange. Am. Physiol. Soc.; Washington, DC: 1955. [Google Scholar]
- 26.Rattenborg C.Lassen HCA.Basic mechanics of artificial ventilation Management of Life-Threatening Poliomyelitis 195623.Livingstone; Edinburgh: Copenhagen, 1952–1956, With a Survey of Autopsy-Findings in 115 Cases [translated from the Danish by Hans Andersen and others] [Google Scholar]
- 27.Severinghaus JW, Astrup P, Murray JF. Blood gas analysis and critical care medicine. Am J Respir Crit Care Med. 1998;157:S114–S122. doi: 10.1164/ajrccm.157.4.nhlb1-9. [DOI] [PubMed] [Google Scholar]
- 28.Severinghaus JW, Astrup PB. History of blood gas analysis; II. pH and acid-base balance measurements. J Clin Monit. 1985;1:259–277. doi: 10.1007/BF02832819. [DOI] [PubMed] [Google Scholar]
- 29.Siggaard-Andersen O. The Acid-Base Status of the Blood. Munksgaard; Copenhagen: 1974. [Google Scholar]
- 30.Thomsen VF. Kort redegorelse for den midlertidige studenterhlelp pa blegdamshospitalet. Ugeskr Læger. 1953;115:468–469. [PubMed] [Google Scholar]
- 31.Van Slyke DD, O’Neill JM. The determination of blood gases in blood and other solutions by vacuum extraction and manometric measurement. J Biol Chem. 1924;61:523–573. [PubMed] [Google Scholar]
- 32.Van Slyke DD, Sendroy J., Jr. Studies of gas and electrolyte equilibria in blood; XV. Line charts for graphic calculation by the Henderson-Hasselbalch equation, and for calculating plasma carbon dioxide content from whole blood content. J Biol Chem. 1928;79:781–798. [Google Scholar]
- 33.Wackers GL. Constructivist Medicine (Dissertation) University of Maastricht; Maastricht, The Netherlands: 1994. [Google Scholar]
- 34.Wackers GL. Modern anaesthesiological principles for bulbar polio: manual IPPR in the 1952 polio-epidemic in Copenhagen. Acta Anaesthesiol Scand. 1994;38:420–431. doi: 10.1111/j.1399-6576.1994.tb03923.x. [DOI] [PubMed] [Google Scholar]
- 35.Wright S. Applied Physiology. Oxford University Press; London: 1948. [Google Scholar]
- 36.Zorab J. The resuscitation greats: Bjørn Ibsen. Resuscitation. 2003:57–3. doi: 10.1016/s0300-9572(03)00040-6. [DOI] [PubMed] [Google Scholar]


