Abstract
Background and Purpose
The relationship between abnormal postural coordination and back pain is unclear. The Alexander Technique (AT) aims to improve postural coordination by using conscious processes to alter automatic postural coordination and ongoing muscular activity, and it has been reported to reduce low back pain. This case report describes the use of the AT with a client with low back pain and the observed changes in automatic postural responses and back pain.
Case Description
The client was a 49-year-old woman with a 25-year history of left-sided, idiopathic, lumbrosacral back pain. Automatic postural coordination was measured using a force plate during horizontal platform translations and one-legged standing.
Outcomes
The client was tested monthly for 4 months before AT lessons and for 3 months after lessons. Before lessons, she consistently had laterally asymmetric automatic postural responses to translations. After AT lessons, the magnitude and asymmetry of her responses and balance improved and her low back pain decreased.
Discussion
Further research is warranted to study whether AT lessons improve low back pain–associated abnormalities in automatic postural coordination and whether improving automatic postural coordination helps to reduce low back pain. [Cacciatore TW, Horak FB, Henry SM. Improvement in automatic postural coordination following Alexander Technique lessons in a person with low back pain.
Keywords: Back pain, Balance, Motor control, Motor learning, Posture
A growing number of studies have suggested that people with low back pain (LBP) may have deficits in postural coordination, such as deficits in the coordination of whole-body, voluntary movements (including restricted kinematics1–8 and increased muscular activity6–11). People with LBP also have deficits in standing and seated balance compared with people without LBP12–15 and may have deficits in automatic postural coordination.16 In particular, anticipatory postural adjustments, which precede voluntary movements to stabilize the body in advance, are abnormally coordinated in people with LBP, notably for deep trunk muscles.16–18 Preliminary evidence also suggests that automatic postural responses to externally applied perturbations, such as surface translations, may be abnormally coordinated in people with LBP.15,19,20 Despite evidence that postural coordination is abnormal in people with LBP, how deficits in postural coordination relate to LBP and the implications of altered postural coordination for intervention still are not clear.
The Alexander Technique aims to improve postural coordination by consciously altering automatic responses and tonic muscular activity.
Currently, whether abnormal postural coordination can cause or contribute to LBP is not known. Some authors21–24 have hypothesized that poor coordination could lead to pain, for instance, by producing greater loading within the trunk. In support of this hypothesis, people with LBP have greater muscular activity and greater spinal loading than people without LBP.11 Alternatively, abnormal postural coordination could result from the pain itself (eg, splinting to avoid pain).25,26
We were interested in exploring whether improved postural coordination can reduce LBP; however, how deficits in postural coordination can be improved is not clear. One method that may improve deficits in postural coordination is the Alexander Technique (AT), which aims to alter habitual faulty postural behavior to increase the efficiency of postural coordination. The AT aims to improve postural coordination by teaching a person to consciously assume a state of postural readiness that, in turn, affects automatic postural coordination and ongoing muscular activity (referred to as “tonic muscular activity”). The AT is particularly concerned with the control of postural readiness and tonic muscular activity in relationship to action, such as movement (although its scope is broader than this, as described in this report). Despite its widespread use in the performing arts to improve coordination and performance, few controlled investigations into the AT have been conducted. The few studies that have been performed on the AT suggest that the AT improves functional reach,27 breathing capacity,28 and symptoms of Parkinson disease29,30; alters the coordination of sit-to-stand31–34; and reduces the sense of effort to perform movements.33 Currently, the scientific basis of the AT and its relationship to LBP are not understood. The AT may improve abnormal postural coordination associated with LBP because it addresses aspects of postural coordination that are abnormal with LBP, such as automatic postural coordination, and it has been reported to improve LBP.35–37 Proponents claim that reduction in LBP occurring from AT lessons is due to improved postural coordination38; the AT does not directly address or aim to reduce pain.39,40
To date, it is not clear whether the abnormal postural coordination in people with LBP can be improved. Some studies41,42 have shown that people without LBP can alter many aspects of their postural coordination—even automatic postural coordination. One study43 suggested that sustained alterations to automatic postural coordination can be achieved through training for people without LBP. Although abnormal automatic postural coordination cannot be reproduced or mimicked voluntarily, people without LBP can alter their automatic postural coordination indirectly by changing their central set. Central set is a central, preparatory state within the nervous system related to higher-level task-related intentions and expectations.44 Central set can shape automatic postural coordination, such as anticipatory postural adjustments in preparation for voluntary arm movement,45 automatic postural responses in response to surface translations,46 and tonic muscular activity.47,48 Because the AT addresses automatic postural coordination and tonic muscular activity using conscious, high-level processes, the AT may act by changing central set.32,33
Frederick Matthias Alexander, an actor and reciter born in Tasmania in 1869, developed the AT to overcome his vocal difficulties. Independent of contemporary scientific theory,40 he developed his technique after extensive observations of his postural behavior and his own preparatory automatic reactions to the act of speaking. In 1904, Alexander moved to England, where he taught the AT until his death in 1955. Alexander taught that tonic muscular activity, kinesthetic perception, and reactivity to contextual stimuli are interrelated fundamental aspects of an individual, which he collectively referred to as the “use of the self.”40 In particular, Alexander taught that automatic responses to stimuli can become habitual and lead to long-term adaptations of tonic muscular activity that are inefficient and to related decreases in the accuracy of kinesthetic perception. Alexander thought that these adaptations, in turn, reinforce excessive automatic responses and underlie numerous psychophysical conditions such as anxiety disorders and back pain.
Teachers complete a 3-year training course to acquire practical competence of the AT in themselves as a basis for teaching. Training courses are overseen by the Society for Teachers of the Alexander Technique (STAT, United Kingdom) and its international affiliated societies, such as the American Society for the Alexander Technique (AmSAT).
The AT aims to improve the “use of the self” by teaching conscious control of tonic muscular activity in relation to actions and events through 2 main principles: (1) the prevention of undesirable increases in tonic muscular activity that are triggered by actions and events (“inhibition”) and (2) the use of conscious, spatially directed motor commands to influence tonic muscular activity (“direction”). Alexander claimed that these principles, when integrated, achieve and maintain a definite, balanced organization of tonic muscle activity that underlies efficient coordination.39,40 These principles are summarized below in reverse order; more detailed descriptions are available elsewhere.38–49
Direction
Direction describes the process of sending conscious motor commands to influence tonic muscular activity. These commands specify a state of postural readiness to allow body segments to expand relative to one another. For example, a direction that is commonly given is to allow the spine to lengthen (“let the spine lengthen”). Alexander claimed that a state of postural readiness that allows expansion, favorably organizes tonic muscular activity so that it is neither “over-tense” nor slack and readily adapts to changes in position. For example, directing along the spine is thought to create an elongated state of the neck and back that is naturally balanced and supple. Although directing is thought to redistribute tonic muscle activity, it does not explicitly specify changes in muscular activity, such as tensing or relaxing abdominal or back muscles. Furthermore, direction does not specify a particular position or overt movement, but can be given within any position or movement.
Alexander determined specific directions for the head, neck, and back, whose tonic muscular relationship he considered to be the most influential, which is referred to as “primary control.” These primary directions specify allowing the head to release forward (anterior) and up (along the axis of the spine) and for the spine to lengthen and the back to widen. Alexander taught that other, secondary directions are important, such as, when seated, directing the knees forward and away from the hip joint and the heels downward into the ground.
Directing is taught experientially through manual guidance and verbal instruction that provide a person with sensorimotor experiences that convey and clarify the nature of the desired motor commands, as well as through feedback about the person’s ability to direct. Directing is a distinct process from making overt movements involving a spatially oriented bodily attention that produces a barely perceptible shift in tonic muscle activity.50 To convey the intention for a particular direction (eg, directing the head forward and up from the spine), the teacher suggests this direction with sustained hand contact on the head while simultaneously describing the desired change in postural readiness (eg, “allow the neck to be free to allow the head to move forward and up from the spine”). The teacher may vary the hand contact or the explanation to best convey the spatial intention to the person, which may include increasing the person’s body awareness. The teacher provides feedback when the person makes a desired change in tonic muscular activity, which is detected through the teacher’s hands as a subtle expansion and redistribution of tension along with a lively, adaptive quality that responds dynamically to changes in position. In their training, teachers are taught to recognize these qualities, which are claimed by proponents of the AT to be clearly distinguishable from an overt movement, a change in posture, or a relaxing of tension.50
Alexander taught that tonic muscular activity is closely related to kinesthetic sensory perception.39,40 He claimed that a poor distribution of tonic muscular activity occurs with an inaccurate perception of the spatial and tensional relationships between body segments, which is referred to as “unreliable sensory appreciation.” Alexander taught that this interrelation between kinesthetic perception and tonic muscular activity confounds learning to direct because a person’s directions are based on inaccurate perceptions of segmental and tensional relationships.39,40 A person, for example, may have a laterally asymmetric habitual orientation of the trunk but perceive the trunk to be vertical. For this person, an attempt at directing along the spine would be carried out along the wrongly perceived axis and not produce the desired change in tonic muscular activity. Furthermore, a change in the organization of tonic muscular activity that brings the person more upright may feel crooked. Because of this failure to distinguish desirable tensional patterns, people are not given exercises to practice, but instead, in learning to direct, are taught to rely on experiences and feedback provided by a teacher, which are thought to gradually improve tonic muscular activity and kinesthetic perception in tandem.39,40
Inhibition
The AT principle of inhibition is a decision to withhold the habitual response to a stimulus to prevent disruptions to tonic muscular activity, which are automatically triggered by contextual cues. Alexander claimed that the context of engaging in an activity, such as playing an instrument or using a computer, commonly brings out an associated individual, habitual “set” of tonic, preparatory activities or changes in postural readiness that increases tension and interferes with the performance of the action.39,40 Alexander observed that nonmotor stimuli, such as stressful events or interpersonal interactions, also can trigger undesirable changes in tonic muscle activity.39,40 He claimed these triggered changes are a fundamental impediment to controlling tonic muscular activity because of their pervasiveness and their close ties to actions or events, which makes them difficult to change.39,40 Furthermore, Alexander claimed that undesirable changes in tonic muscular activity become worse with compulsiveness to perform an act or achieve an end.39,40 Alexander claimed that performing an activity without attention to inhibition and direction, referred to as “end-gaining,” produces undesirable disruptions of tonic muscular activity.39,40
Inhibition is practiced by first providing a contextual cue to trigger undesirable, habitual changes in tonic muscular activity followed by instructing the person to inhibit these undesirable responses and maintain direction. A teacher guides a person to inhibit by having them dissociate the actual response from the contextual cue. Two strategies used for this are: (1) having the person withhold the entire, immediate response to the cue, to make the person aware of triggered increases in tension and enable a change in response and (2) guiding an unpredictable sequence of actions, to discourage the person from expecting or predicting outcomes based on context. For example, the teacher may provide a contextual cue by asking the person to perform an action, such as standing up from a seated position, which has been reported to commonly evoke an unnecessary tensing of the neck.32 The teacher will ask the person to prevent the initial, impulsive response to stand up (ie, not “end-gain”) and instead maintain directing. The teacher will then guide the person among several different actions, such as leaning backward, actually standing up, or maintaining a seated position, while continually indicating desired tensional relationships through sustained hand contact. In total, this teaching process aims to convey a general ability for inhibition that can be learned and applied across different contexts.38,39,49
Alexander Technique lessons are taught individually and last 30 to 45 minutes. A course of 20 to 25 lessons is thought to convey a basic proficiency in the principles.38,49 In a lesson, an AT teacher selects lesson procedures and instructs, evaluates, and provides feedback to the person. In general, these different aspects are not performed separately, but occur simultaneously and continuously during the lesson. For example, a teacher’s hand contact simultaneously analyzes tensional patterns, makes the person aware of these patterns, guides the directional intentions, and prevents undesired increases in tension.49 Moreover, guiding a person through a movement is evaluative and instructive and provides feedback.
Because inhibition and direction are general principles that can be applied in any activity, they also can be taught in any activity; however, a few standard procedures are most commonly used in a lesson.49 These standard procedures are basic positions and movements that are thought to be most effective for evaluating habitual, tensional patterns; triggering preparatory tensing; and conveying the primary directions. The most commonly used procedure is transitioning between sitting and standing (this is referred to as “chair work”).
In chair work, a teacher guides the person to stand up and sit down, emphasizing inhibition and direction as appropriate. Typically, teachers gently place their hands on people’s heads, necks, or other body segments to evaluate the organization of tonic muscular activity and guide direction along the length of the spine throughout these actions. A teacher may have a person stand up and sit down many times during a lesson and may vary the movement trajectory to alter the demands of the task (eg, by guiding reduced forward trunk inclination at seat liftoff). The aim is not to achieve a particular “ideal” trajectory, but to teach the person to maintain direction throughout a task. The teacher may guide the person to pause or alter the trajectory at any point in mid-movement to convey the desired neutrality and adaptability of equilibrium, claimed to result from inhibition and direction.49
In addition to chair work, a number of other procedures are commonly used during a lesson, such as performing a knee-bend, squat, and rising up onto the toes.49 In addition, most teachers also work with a person lying in a semisupine position (supine, with knees flexed and feet on the floor), which is thought to be an advantageous position while directing tonic muscular activity because the person’s back is supported and balance requirements are minimal. The act of speaking is considered to be a strong trigger of undesired habitual tensing, and teachers often work with people while speaking or singing.38,39,49 A procedure for breaking down the sequence of opening the mouth and vocalizing while maintaining the directions is considered beneficial. Many teachers work with people directly in activities that are important to them or problematic for them, such as playing an instrument or washing dishes. Although offering the advantage of working directly with the activity, this is commonly only done with advanced students because the contextual cues are often considered to be too strong to teach inhibition and direction effectively.
The scientific basis for the AT is not understood; however, the method appears consistent with changing central set. Inhibition and direction both use conscious intentions to alter a preparatory state of postural readiness, thought to affect tonic muscular activity and postural coordination. Similarly, central set is influenced by conscious intention as well as context and, in turn, influences tonic muscular activity and automatic postural coordination.44,46–48,51 Tonic muscular activity has long been hypothesized to closely relate to the state of postural readiness.52–54 More specifically, direction is consistent with changing central set by producing a preparatory state that allows positional changes in segments. Inhibition is consistent with changing central set by changing a person’s sensorimotor expectations and intentions in relation to context.
Although the AT addresses automatic preparation prior to voluntary movements or anticipatory postural adjustments, it is not known whether the AT changes automatic postural responses to external perturbations. If the AT changes automatic postural responses to external perturbations, this would support the ability of the AT to change central set, as opposed to solely changing postural orientation or the trajectory of voluntary movement.
The AT has been claimed to improve different types of musculoskeletal pain, such as LBP and repetitive strain disorders.55 People commonly take lessons especially for alleviating pain; however, the AT is not intended to be therapeutic in that it does not directly address pain. The AT addresses pain indirectly only through teaching the control over tonic muscular activity. An AT teacher does not diagnose the cause of pain, nor does the teacher base lesson procedures or evaluate progress based on pain. However, an AT teacher will inquire about a person’s pain to determine limitations to lesson procedures, which may indirectly shape the teacher’s approach. The AT’s aims are broader than improving pain or even the control over tonic muscular activity and coordination. Alexander taught that learning to control tonic muscular activity through inhibition and direction conveys the close relationship between mental and physical processes, which leads to a specific type of self-awareness and control that can be applied to the whole range of human activities.39,40,50
We were interested in whether the AT alters automatic postural coordination and LBP. The purpose of this case report is to describe how we followed automatic postural coordination and pain before and after AT lessons in a person with long-standing idiopathic LBP.
Case Description
Client Description
The client was a 49-year-old woman. At the time of the first examination, she had a 25-year history of left-sided, idiopathic, lumbrosacral pain. She reported that her pain occurred daily. The client was employed as a neuroscientist and spent much of her day sitting at a computer and giving talks. Standing for more than 30 minutes exacerbated her pain. She would walk to obtain pain relief. At least once a week her pain was so severe that she had to lie down in hip flexion for relief. She had not undergone surgery for her LBP and took no medication for her pain except occasional Advil.* The client had not been referred for physical therapy but was selected because of her long history of LBP and her availability for lengthy testing sessions and for AT lessons. Her goals were to become able to perform activities of daily living, such as standing, without pain and to improve her overall pain level.
Examination
The client’s posture was observed, and qualitative judgments were made as described by Kendall et al.56 She had pelvic obliquity with the left iliac crest lower than the right and pelvic counterclockwise rotation. She had increased thoracic kyphosis and mild left thoracic and right lumbar curvature. She also had increased pronation at the subtalar joint and knee hyperextension bilaterally. Reliability for the visual examination of posture as described has not been reported.56
Trunk range of motion was assessed as described by Frost et al,57 except measurement of fingertip position was made relative to the lateral knee joint line and tibial bone instead of to the floor. The client had asymmetrical lateral lumbar flexion: to the left, the fingertip reached 7.6 cm (3 in) above the knee joint line and lateral flexion occurred primarily at L1–L2 and above; to the right, the fingertips reached the knee joint line and lateral flexion occurred at L3–L4 and above. During forward flexion, the fingertip reached mid-shin. During trunk extension, the lumbar spine extended primarily at the L4–L5 segments, with no extension above. Frost et al57 reported single measurement reliability for forward flexion of r = .91; however, because our procedure for measuring trunk range of motion was modified from Frost et al,57 reliability is not known.
Abdominal muscle force was measured as Nelson and Nestor58 described. The client had weakness in abdominal muscles (3/5 on trunk curl test; the lumbar spine extended between 60° and 90° on the double leg-lowering test). Interrater reliability of data obtained with this measurement protocol has been reported in subjects with LBP, with an intraclass correlation coefficient (ICC) of greater than .80.58 Force of trunk extensors and hip abductors was measured as Kendall et al56 described. Trunk extensor muscle force was 5/5, and hip abductor muscle force was 4/5 bilaterally. Kendall et al56 did not report reliability for this measurement procedure of trunk and hip muscle force.
The client’s pain was located in the left lumbrosacral area, and she described it as a deep ache. At the time of initial testing, prior to AT lessons, she was asked to rate her pain by placing a mark on a 10-cm line according to the visual analog scale (VAS).59 The client rated her pain as 8.3 cm. The test-retest reliability for the VAS has been reported to be between .71 and .99 in subjects with chronic pain,60 rheumatoid arthritis,61,62 and cancer.63
Lower-extremity deep tendon reflexes were tested for the quadriceps femoris and gastrocnemius-soleus muscles with the client sitting relaxed with her thighs resting on a table and her knees flexed 90 degrees.64 The muscle being tested was palpated to ensure that it was relaxed. To determine whether the gastrocnemius-soleus muscle was relaxed while she was in the sitting position, her ankle joint was dorsiflexed passively to 90 degrees and the tibialis anterior muscle was palpated. The patellar tendon or Achilles tendon was tapped with a reflex hammer 5 times, and the muscle response with each tap was noted. The patellar tendon and Achilles tendon reflexes were judged to be normal and symmetrical: 2 on a scale from 0 (“absent”) to 4 (“very brisk, clonus”). The reliability of data obtained with this technique is not known. Lower-extremity sensation was intact to light touch; no abnormal sensations were reported. The client gave consent in accordance with the Oregon Health & Sciences University internal review board protocol.
Intervention
We selected the AT as an intervention because we were interested in whether it could improve automatic postural coordination and pain in someone with longstanding LBP. The client received 20 AT lessons from an AmSAT-certified teacher. Lessons lasted approximately 45 minutes each and occurred approximately every week over a 6-month period. The client was taught to achieve and maintain a balanced and elongated state of tonic muscular activity through the principles of the AT. She was taught mainly while she was seated, standing, or lying down. The teacher emphasized anatomical relationships in explaining the directions and used mirrors to demonstrate to the client that her self-perception of body configuration was not accurate. In later lessons, the teacher worked with the client during activities of daily life (eg, gardening, typing at the computer). She was not given exercises to perform outside lessons, but was told to apply the principles in lessons to daily life. The lessons did not specifically train for or practice the outcome measures described in this report.
Outcome Measures
We measured postural coordination and pain before and after the client received a series of AT lessons. We examined the client’s postural coordination using 2 primary tasks: automatic responses to surface translations and one-legged balance. In addition to these 2 primary measures, we also examined the lateral curvature within the client’s trunk during quiet stance, which the AT considers to be related to the distribution of tonic muscle activity and important. Measures of postural coordination in the tasks were quantified using kinematics and surface forces. If the AT changes central set, we would expect changes to occur across these different tasks.
Equipment
A computer-controlled, movable, hydraulic platform was used to produce the surface translations. Force plates embedded in the platform under each foot were used to measure surface forces. A 6-camera passive marker motion capture system (Motion Analysis†) was used to measure kinematics. At the beginning of each testing session, kinematic markers were placed on the client at the following locations: C7, T4, T7, L1, L4, sacrum, and vertex of the head and bilaterally on the posterior superior iliac spines, posterior upper thigh, middle of the popliteal line, posterior calcaneus, and base of the skull 5 cm lateral to the midline (Fig. 1).
Figure 1.
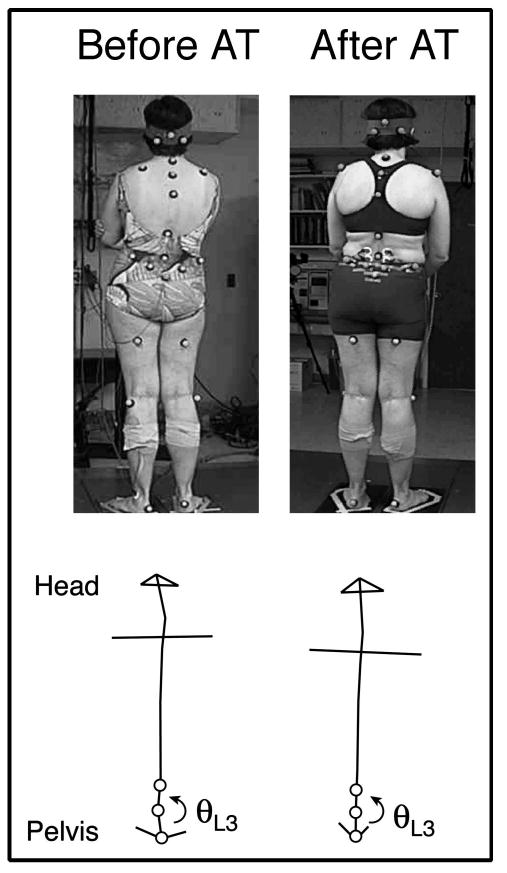
Lateral standing lumbar curvature. The client is shown standing with kinematic reflective markers. Top panels show standing posture before and after Alexander Technique (AT) lessons. Bottom panels show stick figures of the upper body before and after AT lessons, with the measurement of lateral lumbar curvature at L3 indicated. For the time line of measurements across testing sessions, refer to Fig. 2.
Protocols
During the first 3 months, the client participated in 4 testing sessions, each 1 month apart, to provide baseline measurements in the tasks described in this report (automatic responses to surface translations, one-legged balance, and lateral curvature during quiet stance) before lessons. For each testing session, she stood on the movable platform and performed the tasks. During the last 6 months, she received AT lessons, and during the last 3 months, she also participated in 3 testing sessions to examine her postural coordination following lessons. The post–AT lesson testing sessions were separated by 1 month and consisted of the same tasks.
Platform translations
Horizontal platform translations were chosen to elicit automatic postural responses. Although automatic postural responses are triggered within 100 milliseconds, faster than voluntary reaction times, they can be influenced by expectations or instruction.42,65 In particular, central set affects the kinetics and kinematics of responses to translations, such as the center-of-pressure (CoP) displacement under the feet and joint displacement.42,46,65,66 Lateral translations were chosen because the client’s back pain was lateralized on the left side and large lateral asymmetries in automatic postural responses could reveal aspects of postural coordination related to LBP. Automatic postural responses to lateral surface translations were quantified using lateral trunk flexion because this reflects the postural responses within the trunk. The CoP displacement under the feet also was examined because this reflects the overall stability and organization of a person’s automatic postural responses. The displacement of the CoP in response to lateral surface translations has been found to be consistent within subjects across testing sessions (.15<P<.99),67 which suggests that subjects without LBP respond in a consistent manner. The client was instructed to stand relaxed on the platform with arms crossed and to restrict using the arms to balance. The platform then was translated, sliding horizontally, at an unexpected time for 9 cm over 300 milliseconds with a maximum acceleration of 1.0 m/s2. Three trials were performed in each direction in a randomized order.
One-legged standing
The client performed one-legged stance to measure her balance, which was quantified using root-mean-square (RMS) shear (horizontal) forces under the feet because these forces reflect the acceleration of the center of mass and overall stability. The client was instructed to stand on each leg individually for 30 seconds. Three trials were performed on each leg. This task was not performed during the first 2 testing sessions because a colleague (VS Gurfinkel) suggested including this task only after the second session. Test-retest reliability of sway acceleration during one-legged stance has been found to have an ICC of .84 in 19 subjects without LBP.68
Quiet stance
The client’s standing lateral trunk curvature was measured during the 200 milliseconds of baseline quiet stance, prior to platform translation. This quantified her typical stance, because she was unaware that her postural orientation was being measured. This curvature was quantified at L3 using kinematic markers, the spinal level where she had the largest lateral curvature and that was near to her pain.
Pain evaluation
The client was asked to rate her level of back pain by placing a mark on the VAS, a 10-cm line, from 0 cm (“no pain”) to 10 cm (“maximal pain”), on the first testing session, prior to AT lessons, and on the last testing session following AT lessons.
Data Analysis
Kinematics
Kinematic data were collected at 60 Hz, combined across the 6 cameras (using Real-Time software†) to produce 3-dimensional positions for each marker, and filtered at 10 Hz prior to processing. Joint angles were computed in the frontal plane to quantify the lateral trunk flexion in 4 different regions of the spine: L3, L1, T7, and T4 (Fig. 1). For example, flexion at L3 was calculated as the angle between the sacral, L3, and L1 markers. The magnitude of trunk flexion to platform translations was computed for each trial as the maximal deviation from the average baseline value before the translation began. Total trunk flexion was computed by summing the individual angles (L3+L1+T7+T4) at each time point.
Forces
Vertical force, frontal- and sagittal-plane moments, and shear forces were sampled from each force plate at 480 Hz and low-pass filtered at 20 Hz. The CoP under the foot was computed, by dividing the moment by the vertical force, as the maximal deviation from the baseline value.
Outcomes
Lateral Curvature During Quiet Stance
During quiet stance prior to AT lessons, the client had pronounced trunk asymmetries in the frontal plane, including leftward lumbar curvature (leftward convexity) as well as leftward pelvic obliquity and rightward cervical curvature (Fig. 1). In particular, the lateral lumbar curvature at L3, near to her LBP, was on average (±SEM) 6.8±1.0 degrees before lessons. After AT lessons, the average magnitude of L3 lumbar curvature decreased to 1.6±0.8 degrees and reversed direction. On the first and third testing sessions after AT lessons, this curvature was near zero; however, during the second session after AT lessons, she had rightward L3 curvature. Figure 2A shows the average curvature for each testing session. Other features that were asymmetric in the frontal plane before AT lessons, such as pelvic obliquity and cervical curvature, were not quantified but appeared to become more symmetric overall after AT lessons.
Figure 2.
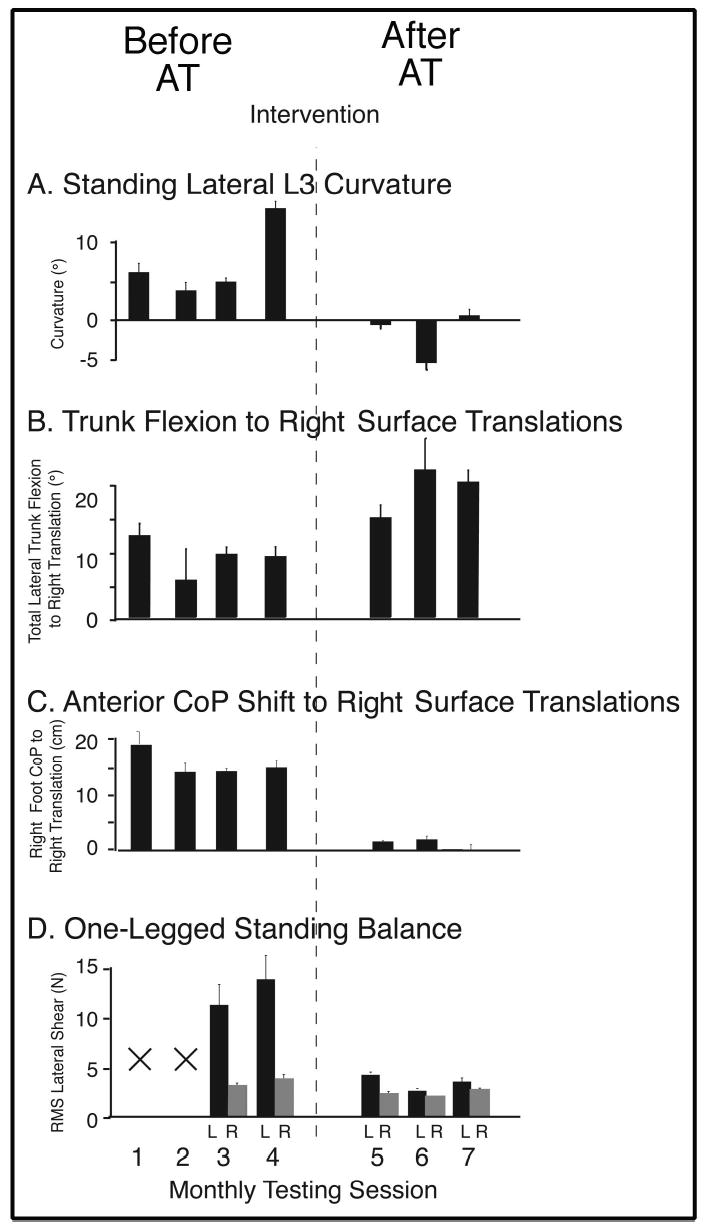
Time line of measurements across testing sessions. Average values of dependent variables are shown for each testing session. Error bars are ± SEM. Alexander Technique (AT) lessons began after the fourth testing session. A—Standing L3 lumbar curvature is given as deviation from 180 degrees. Positive values refer to leftward convexity. B—The average total lateral trunk flexion (summed across spinal levels) to rightward translations. Positive values indicate leftward flexion. C—Anterior center-of-pressure (CoP) movement under the right foot to rightward translations. Positive values indicate maximal anterior CoP movement. D—The average root-mean-square (RMS) lateral shear force for each leg during one-legged balance. L (left) and R (right) indicate the foot the subject stood on. Note that this task was not performed during the first 2 testing sessions.
Surface Translations
During the pre–AT lesson period, the client’s automatic postural responses to rightward versus leftward horizontal surface translations were qualitatively different; in comparison, responses to rightward translations (causing leftward lateral trunk flexion) consistently appeared jerky, uncoordinated, and unstable. She reported feeling unstable during rightward translations.
Prior to AT lessons, the client had asymmetric trunk flexion in her automatic postural responses to rightward versus leftward surface translations; in particular, trunk flexion was reduced to rightward translations (Fig. 3A). Averaged across the pre–AT lesson testing sessions, the total trunk flexion was 35% less for rightward translations (8.9°±2.3°) than for leftward translations (13.7°±1.4°). At the individual spinal levels that were measured (L3, L1, T7, and T4) all had reduced lateral trunk flexion to rightward translations when compared with leftward translations (Table, Fig. 3B). At these individual spinal levels, the time course of flexion also was shorter in duration and more erratic to rightward translations than to leftward translations.
Figure 3.
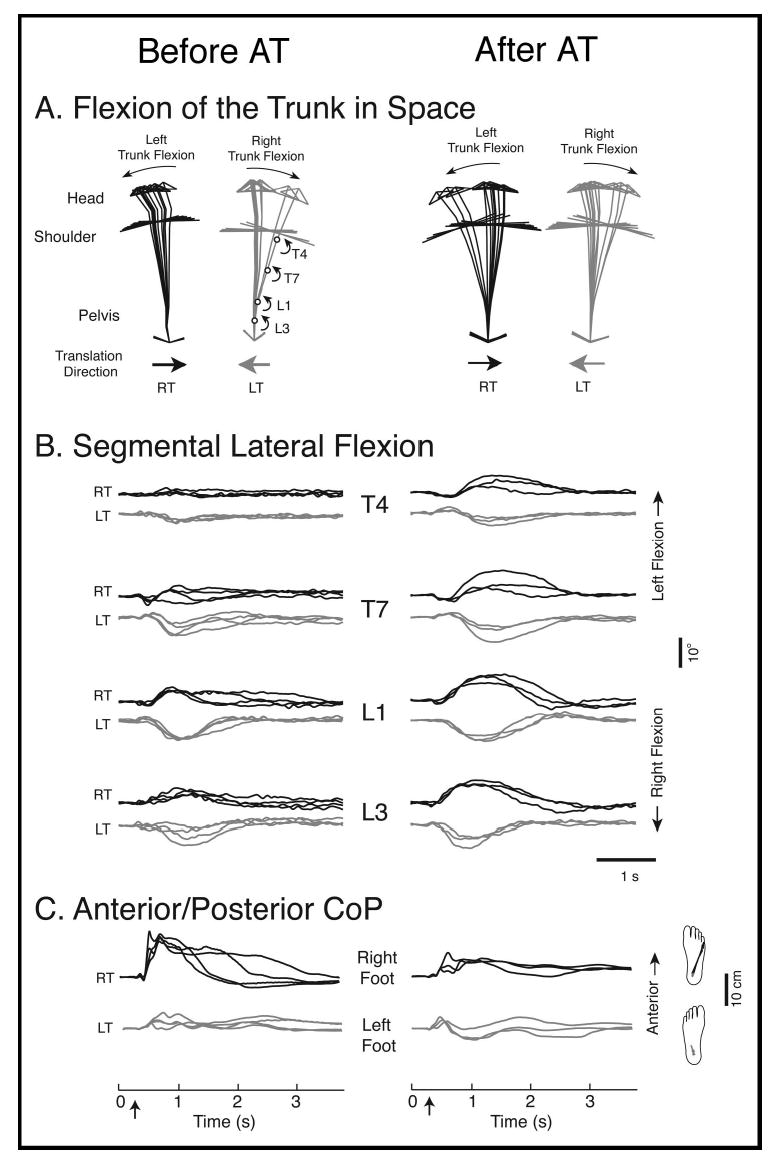
Automatic postural responses to lateral surface translations. The left and right columns show responses before and after Alexander Technique (AT) lessons, respectively, for all panels. Responses to rightward translations (RT) are shown in black, and responses to leftward translations (LT) are shown in gray. A—Stick figures (using markers shown in Fig. 1) during RT and LT show the movement of the trunk in space for a single trial at 340-millisecond intervals, before and after AT lessons. The arrows below indicate the direction of platform translation. Note that surface translations cause lateral trunk flexion in the direction opposite to platform movement. The client had reduced lateral trunk flexion to RT before AT lessons. B—The time course of lateral trunk flexion is shown for the individual spinal levels of L3, L1, T7, and T4 to RT (black) and LT (gray) before and after AT lessons. Leftward flexion is upward. One trial from each testing session is superimposed (4 pre–AT lesson traces, 3 post–AT lesson traces). Platform translations were initiated at 200 milliseconds, as indicated by the arrow on the axes in the bottom panel. Note the reduced magnitude of leftward lateral trunk flexion to RT across spinal levels before AT lessons. C—The anterior center-of-pressure (CoP) displacement is shown for the right and left feet to RT and LT, respectively. One trial from each testing session is superimposed (4 pre–AT lesson traces, 3 post–AT lesson traces). The trajectory along the surface of the foot for one trial (prior to AT lessons) is shown to the right of the figure. Note the large, anterior displacement of the CoP under the right foot shortly after platform translation prior to AT lessons that was not present after AT lessons.
Table.
Average (±SEM) Lateral Trunk Flexion (in Degrees) to Translation Across Spinal Levelsa
| Spinal Level | Before AT Lessons | After AT Lessons | |
|---|---|---|---|
| T4 | RT | 0.7±1.3 | 3.4±1.5 |
| LT | 2.1±0.4 | 2.6±0.9 | |
| T7 | RT | −0.3±2.1 | 4.7±2.2 |
| LT | 3.6±0.9 | 4.2±2.2 | |
| L1 | RT | 4.0±1.3 | 6.1±1.2 |
| LT | 5.9±0.7 | 6.1±0.7 | |
| L3 | RT | 3.6±1.4 | 5.1±1.1 |
| LT | 3.8±1.9 | 5.2±0.7 |
The average lateral trunk flexion to surface translations is given for different spinal levels before and after Alexander Technique (AT) lessons. RT (rightward translation) and LT (leftward translation) refer to the direction of platform translation. Positive values correspond to flexion in the direction opposite to translation. Prior to lessons, lateral trunk flexion was smaller for RT than for LT at every spinal level. Following AT lessons, the magnitude of flexion increased at all levels in both translation directions.
To examine whether the client’s limitation to leftward spinal flexion, in response to rightward translations, was caused by mechanical restriction or pain, we asked her to perform voluntary, leftward lateral bends of a comfortable magnitude during pre–AT lesson testing sessions. The client’s voluntary, leftward lateral trunk flexion was substantially greater than that evoked by rightward translations across spinal levels: L3=10±1.2 degrees, L1=6.9±1.0 degrees, and T7=5.8±1.1 degrees (compared with values for rightward translations shown in the Table), suggesting that the reduced flexion to rightward translations was not caused by mechanical restriction or pain, but by her automatic postural responses within the trunk.
Before AT lessons, the client had a large anterior displacement of CoP under the right foot in response to rightward translations (Fig. 3C). This displacement was 15.9±1.9 cm on average across the pre–AT lesson testing sessions and occurred immediately following platform translation as the right foot was being unweighted, due to rightward platform movement. In contrast, the analogous response to leftward translations, under her unweighted, left foot, was approximately 4 times smaller (4.5±1.5 cm).
After AT lessons, the magnitude of lateral trunk flexion in response to translations increased for both perturbation directions (Table, Fig. 3A). Total trunk flexion increased from 8.9±2.3 to 18.7±3.2 degrees for rightward translations and from 13.7±1.4 to 17.1±1.8 degrees for leftward translations. The client’s trunk flexion also became more symmetric because there was a greater increase during rightward translations. Figure 4B shows the average values of lateral flexion for rightward translations for each testing session, relative to the start of AT lessons. Increases in trunk flexion and symmetry of leftward and rightward responses were apparent at the spinal levels of L3, L1, T7, and T4 (Table, Fig. 3B). The time course of the flexion at the individual levels changed after AT lessons as well; flexion was larger, smoother, and longer in duration. For example, the erratic response at T7 to rightward translations disappeared.
Figure 4.

One-legged standing balance before and after Alexander Technique (AT) lessons. Stick figures are shown every 800 milliseconds during stance on the left foot (black) and right foot (gray) before and after AT lessons for individual trials. The corresponding lateral shear force traces are shown below the stick figures.
After AT lessons, the large, anterior CoP displacement under the client’s right leg to rightward translations decreased over 3-fold from 15.9±1.9 to 4.8±2.1 cm (Figs. 2C and 3C). The analogous CoP displacement to leftward translations, under the left foot, also decreased from 4.5±1.5 to −0.2±2.2 cm.
One-Legged Stance
Before AT lessons, the client’s one-legged balance was markedly asymmetric between legs. Balance ability on the left leg was poor, as evidenced by large, lateral deviations in body position and large shear forces in the frontal plane (Fig. 4). In particular, the RMS magnitude of lateral shear force was larger for left-legged stance (12.3±3.7 N) than right-legged stance (3.2±0.7 N), indicating the larger accelerations of the center of mass on the left leg.
Following AT lessons, RMS shear for left-legged balance decreased from 12.3±3.7 to 3.2±0.5 N (Fig. 2D). The magnitude of RMS shear for right-legged balance also decreased from 3.2±0.7 to 2.1±0.3 N following AT lessons, indicating that her balance ability improved for both legs.
Pain
The client reported a substantial sustained reduction in pain on the VAS from 8.3 cm before AT lessons to 1.9 cm after AT lessons. Before AT lessons, she reported that her pain occurred daily. She typically had pain with activities of daily living; for example, standing for a period of minutes caused discomfort. After lessons, her pain was limited to 1 to 2 days a month and never was so severe that it required lying down. She reported being able to stand for several hours without pain.
Discussion
Prior to intervention, the client had abnormal, laterally asymmetric features of postural coordination in all the outcome measures, which were consistent across the pre–AT lesson period. These features included abnormal automatic postural responses to rightward surface translations, in particular, limited leftward trunk flexion and large anterior CoP deviations under the right foot; instability in one-legged balance when standing on the left leg; and a pronounced, leftward lateral lumbar curvature during quiet standing. It is possible that these features of postural coordination were not independent deficits, but stemmed from a common underlying cause.
For instance, overall poor control of the trunk could have caused the client’s asymmetric responses to surface translations, her poor one-legged balance, and her lateral lumbar curvature. Poor control of the trunk also could have underlaid the large, anterior CoP movement under her right foot to rightward translations, through a compensatory strategy to shift the center of mass leftward, without laterally flexing the trunk, by plantar flexing the right ankle to effectively lengthen this leg.
The client’s abnormalities in postural coordination are consistent with previous reports of coordination deficits in subjects with LBP. Her abnormal automatic postural responses to surface translations suggests that central set was altered, which is consistent with the abnormal anticipatory postural adjustments reported in subjects with LBP.16–18 The client’s poor one-legged balance also is consistent with other reports of poor balance in subjects with LBP.12–15 In addition, the findings of one preliminary study19 suggest that, in response to surface translations, subjects with LBP have decreased latencies for automatic postural responses in trunk muscles, when compared with controls without LBP. Decreased latencies for automatic postural responses of trunk muscles are consistent with the reduced trunk flexion observed in the client.
The abnormalities in the client’s postural coordination that were present during the pre–AT lesson period were substantially improved following AT lessons. Specifically, her automatic postural responses to rightward translations improved, her lateral trunk flexion increased, and the large CoP displacement under the right foot decreased. In addition, her left-legged balance improved, and her lateral lumbar curvature decreased. Although changes in the post–AT lesson period were mostly to the client’s “bad” side, making her responses more symmetric overall, postural coordination on her “good” side improved as well. All of the improvements in postural coordination occurred between the fourth and fifth testing sessions, after the client had begun AT lessons (Fig. 2), which is consistent with our assumption that deficits in postural coordination associated with LBP, in particular deficits in automatic postural coordination, can be changed through intervention. Her improvement was not likely due to practice of the tasks described in this report because trends were not apparent during the pre–AT lesson period and the AT lessons did not include practice of the these tasks. Because multiple features of the client’s postural coordination improved across tasks that were not practiced, the changes in her postural coordination were likely global in nature and not task specific. The global nature of changes in postural coordination and, in particular, the change in automatic postural responses suggest that the client changed her central set, which is consistent with our assumption that the AT improves tonic muscular activity and postural coordination by altering central set. However, the improvements in her postural coordination could have been caused by other factors besides the intervention. For example, the placebo effect may have caused a spontaneous reduction in her pain and thereby produced the observed improvements in postural coordination.
The reduction in the client’s pain following AT lessons is consistent with the assumption that improving postural coordination may be a useful intervention approach for LBP. Although lessons in the AT appeared to improve this person’s postural coordination and pain, research is needed to determine whether the AT can improve postural coordination in people with LBP and whether improving postural coordination can reduce LBP. Research also is needed to examine the mechanisms that would account for the reduction in pain and changes in postural coordination observed in this person.
Acknowledgments
All authors provided concept/idea/project design and writing. Dr Cacciatore and Dr Horak provided data collection and analysis, project management, and fund procurement. Dr Horak provided the client, facilities/equipment, and clerical support. Dr Henry provided consultation (including review of manuscript before submission). The authors thank Barbara Conable for donating the series of Alexander Technique lessons, Dr Victor S Gurfinkel and Sandra Oster for discussion, and Shoshana Kaminitz and Rebecca Robbins for their feedback and contribution regarding the Alexander Technique description.
Footnotes
A poster was given on the data presented in this article at the 2001 meeting of the International Society of Posture and Gait, Maastricht, the Netherlands.
Wyeth Pharmaceuticals, Div of Wyeth, PO Box 8299, Philadelphia, PA 19101.
Motion Analysis Corp, 3636 N Laughlin Rd, Suite 110, Santa Rosa, CA 95403.
References
- 1.Boston J. A measure of body movement coordination during repetitive dynamic lifting. IEEE Trans Rehabil Eng. 1993;1:137–144. [Google Scholar]
- 2.Michaud J, Moffet H, McFadyen B. Trunk control during level and stair gait in normal and low-back pain subjects. Neuroscience Abstracts. 2000;26:1232. [Google Scholar]
- 3.Nilsson-Wikmar H, Hirschfeld H. Center of pressure and center of mass interaction during a whole body lifting task in women postpartum with and without back pain. Neuroscience Abstracts. 2000;26:1233. [Google Scholar]
- 4.Rudy TE, Boston JR, Lieber SJ, et al. Body motion patterns during a novel repetitive wheel-rotation task: a comparative study of healthy subjects and patients with low back pain. Spine. 1995;20:2547–25. doi: 10.1097/00007632-199512000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Movement system impairment-based categories for low back pain, stage 1: validation. J Orthop Sports Phys Ther. 2003;33:126–112. doi: 10.2519/jospt.2003.33.3.126. [DOI] [PubMed] [Google Scholar]
- 6.Triano JJ, Schultz AB. Correlation of objective measure of trunk motion and muscle function with low-back disability ratings. Spine. 1987;12:561–565. doi: 10.1097/00007632-198707000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Boline PD, Keating JC, Jr, Haas M, Anderson AV. Interexaminer reliability and discriminant validity of inclinometric measurement of lumbar rotation in chronic low-back pain patients and subjects without low-back pain. Spine. 1992;17:335–338. doi: 10.1097/00007632-199203000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Jayaraman G, Nazre AA, McCann V, Redford JB. A computerized technique for analyzing lateral bending behavior of subjects with normal and impaired lumbar spine: a pilot study. Spine. 1994;19:824–832. doi: 10.1097/00007632-199404000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Lariviere C, Gagnon D, Loisel P. The comparison of trunk muscles EMG activation between subjects with and without chronic low back pain during flexion-extension and lateral bending tasks. J Electromyogr Kinesiol. 2000;10:79–91. doi: 10.1016/s1050-6411(99)00027-9. [DOI] [PubMed] [Google Scholar]
- 10.Ebenbichler GR, Oddsson LI, Kollmitzer J, Erim Z. Sensory-motor control of the lower back: implications for rehabilitation. Med Sci Sports Exerc. 2001;33:1889–1898. doi: 10.1097/00005768-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Marras WS, Davis KG, Ferguson SA, et al. Spine loading characteristics of patients with low back pain compared with asymptomatic individuals. Spine. 2001;26:2566–2574. doi: 10.1097/00007632-200112010-00009. [DOI] [PubMed] [Google Scholar]
- 12.Byl N, Sinnott P. Variations in balance and body sway in middle-aged adults: subjects with healthy backs compared with subjects with low-back dysfunction. Spine. 1991;16:325–330. doi: 10.1097/00007632-199103000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Mientjes MI, Frank JS. Balance in chronic low back pain patients compared to healthy people under various conditions in upright standing. Clin Biomech. 1999;14:710–716. doi: 10.1016/s0268-0033(99)00025-x. [DOI] [PubMed] [Google Scholar]
- 14.Alexander KM, LaPier TL. Differences in static balance and weight distribution between normal subjects and subjects with chronic unilateral low back pain. J Orthop Sports Phys Ther. 1998;28:378–383. doi: 10.2519/jospt.1998.28.6.378. [DOI] [PubMed] [Google Scholar]
- 15.Radebold A, Cholewicki J, Polzhofer GK, Greene HS. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine. 2001;26:724–730. doi: 10.1097/00007632-200104010-00004. [DOI] [PubMed] [Google Scholar]
- 16.Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain: a motor control evaluation of transversus abdominis. Spine. 1996;21:2640–2650. doi: 10.1097/00007632-199611150-00014. [DOI] [PubMed] [Google Scholar]
- 17.Hodges PW, Richardson CA. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehabil. 1999;80:1005–1012. doi: 10.1016/s0003-9993(99)90052-7. [DOI] [PubMed] [Google Scholar]
- 18.Hodges PW, Richardson CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. J Spinal Disord. 1998;11:46–56. [PubMed] [Google Scholar]
- 19.Henry S. Postural responses in people with low back pain. In: Duysens J, Smits-Engelsman B, Kingma H, eds. Control of Posture and Gait International Society for Posture and Gait Research; 2001:651–655.
- 20.Newcomer KL, Jacobson TD, Gabriel DA, et al. Muscle activation patterns in subjects with and without low back pain. Arch Phys Med Rehabil. 2002;83:816–821. doi: 10.1053/apmr.2002.32826. [DOI] [PubMed] [Google Scholar]
- 21.Alaranta H, Moffroid M, Elmqvist L, et al. Postural control of adults with musculoskeletal impairment. Critical Reviews in Physical Rehabilitation Medicine. 1994;6:337–370. [Google Scholar]
- 22.Hodges PW. The role of the motor system in spinal pain: implications for rehabilitation of the athlete following lower back pain. J Sci Med Sport. 2000;3:243–253. doi: 10.1016/s1440-2440(00)80033-x. [DOI] [PubMed] [Google Scholar]
- 23.Richardson C. Muscle imbalance: principles of treatment and assessment. In: Proceedings of the New Zealand Society of Physiotherapists Challenges Conference; Christchurch, New Zealand; 1992. Wellington, New Zealand: New Zealand Society of Physiotherapists; 1992.
- 24.White S, Sahrmann S. A movement system balance approach to management of musculoskeletal pain. In: Grant R. Physical Therapy of the Cervical and Thoracic Spine New York, NY: Churchill Livingstone Inc; 1994:339–357.
- 25.Lund JP, Donga R, Widmer CG, Stohler CS. The pain-adaptation model: a discussion of the relationship between chronic musculoskel-etal pain and motor activity. Can J Physiol Pharmacol. 1991;69:683–694. doi: 10.1139/y91-102. [DOI] [PubMed] [Google Scholar]
- 26.Zedka M, Prochazka A, Knight B, et al. Voluntary and reflex control of human back muscles during induced pain. J Physiol (Lond) 1999;520:591–604. doi: 10.1111/j.1469-7793.1999.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dennis RJ. Functional reach improvement in normal older women after Alexander Technique instruction. J Gerontol A Biol Sci Med Sci. 1999;54:M8–M11. doi: 10.1093/gerona/54.1.m8. [DOI] [PubMed] [Google Scholar]
- 28.Austin JH, Ausubel P. Enhanced respiratory muscular function in normal adults after lessons in proprioceptive musculoskeletal education without exercises. Chest. 1992;102:486–490. doi: 10.1378/chest.102.2.486. [DOI] [PubMed] [Google Scholar]
- 29.Stallibrass C, Sissons P, Chalmers C. Randomized controlled trial of the Alexander Technique for idiopathic Parkinson’s disease. Clin Rehabil. 2002;16:695–708. doi: 10.1191/0269215502cr544oa. [DOI] [PubMed] [Google Scholar]
- 30.Stallibrass C. An evaluation of the Alexander Technique for the management of disability in Parkinson’s disease: a preliminary study. Clin Rehabil. 1997;11:8–12. doi: 10.1177/026921559701100103. [DOI] [PubMed] [Google Scholar]
- 31.Jones F, Gray F, Hanson J, O’Connell D. An experimental study of the effect of head balance on patterns of posture and movement in man. J Psychol. 1959;47:247–258. [Google Scholar]
- 32.Jones F. The influence of postural set on pattern of movement in man. International Journal of Neurology. 1963;4:60–71. [PubMed] [Google Scholar]
- 33.Jones F. Method for changing stereotyped response patterns by the inhibition of certain postural sets. Psychol Rev. 1965;72:196–214. doi: 10.1037/h0021752. [DOI] [PubMed] [Google Scholar]
- 34.Stevens C, Bojsen-Moller F, Soames R. Influence of initial posture on the sit-to-stand movement. Eur J Appl Physiol. 1989;58:687–692. doi: 10.1007/BF00637377. [DOI] [PubMed] [Google Scholar]
- 35.Elkayam O, Ben Itzhak S, Avrahami E, et al. Multidisciplinary approach to chronic back pain: prognostic elements of the outcome. Clin Exp Rheumatol. 1996;14:281–288. [PubMed] [Google Scholar]
- 36.Fisher K. Early experiences in a multidisciplinary pain management programme. Holistic Medicine. 1988;3:47–56. [Google Scholar]
- 37.Cottingham JT, Maitland J. A three-paradigm treatment model using soft tissue mobilization and guided movement-awareness techniques for a patient with chronic low back pain: a case study. J Orthop Sports Phys Ther. 1997;26:155–167. doi: 10.2519/jospt.1997.26.3.155. [DOI] [PubMed] [Google Scholar]
- 38.Jones F. Freedom to Change: The Development and Science of the Alexander Technique London, United Kingdom: Mouritz; 1976.
- 39.Alexander FM. Constructive Conscious Control of the Individual New York, NY: EP Dutton & Co Inc; 1923.
- 40.Alexander FM. The Use of the Self New York, NY: EP Dutton & Co Inc; 1932.
- 41.Buchanan JJ, Horak FB. Voluntary control of postural equilibrium patterns. Behav Brain Res. 2003;143:121–140. doi: 10.1016/s0166-4328(03)00038-x. [DOI] [PubMed] [Google Scholar]
- 42.Burleigh AL, Horak FB, Malouin F. Modification of postural responses and step initiation: evidence for goal-directed postural interactions. J Neurophysiol. 1994;72:2892–2902. doi: 10.1152/jn.1994.72.6.2892. [DOI] [PubMed] [Google Scholar]
- 43.Mouchnino L, Aurenty R, Massion J, Pedotti A. Coordination between equilibrium and head-trunk orientation during leg movement: a new strategy build up by training. J Neurophysiol. 1992;67:1587–1598. doi: 10.1152/jn.1992.67.6.1587. [DOI] [PubMed] [Google Scholar]
- 44.Brooks VB. The Neural Basis of Motor Control New York, NY: Oxford University Press; 1986.
- 45.Cordo PJ, Nashner LM. Properties of postural adjustments associated with rapid arm movements. J Neurophysiol. 1982;47:287–302. doi: 10.1152/jn.1982.47.2.287. [DOI] [PubMed] [Google Scholar]
- 46.Horak FB, Diener HC, Nashner LM. Influence of central set on human postural responses. J Neurophysiol. 1989;62:841–853. doi: 10.1152/jn.1989.62.4.841. [DOI] [PubMed] [Google Scholar]
- 47.Davidoff RA. Skeletal muscle tone and the misunderstood stretch reflex. Neurology. 1992;42:951–963. doi: 10.1212/wnl.42.5.951. [DOI] [PubMed] [Google Scholar]
- 48.Miscio G, Pisano F, Del Conte C, et al. The shortening reaction of forearm muscles: the influence of central set. Clin Neurophysiol. 2001;112:884–894. doi: 10.1016/s1388-2457(01)00468-0. [DOI] [PubMed] [Google Scholar]
- 49.de Alcantara P. Indirect Procedures: A Musician’s Guide to the Alexander Technique New York, NY: Clarendon Press; 1996.
- 50.Macdonald P. The Alexander Technique As I See It Brighton, United Kingdom: Rahula Books; 1989.
- 51.Horak FB, Macpherson J. Postural orientation and equilibrium. In: Rowell LB, Shepherd JT, eds. Exercise: Regulation and Integration of Multiple Systems New York, NY: Oxford University Press (for the American Physiological Society); 1996:255–292.
- 52.Bernstein N. Studies of the biodynamics of walking, running and jumping. In: Whiting H. Human Motor Actions: Bernstein Reassessed Amsterdam, the Netherlands: North-Holland; 1984:171–222.
- 53.Gurfinkel VS. The mechanisms of postural regulation in man. Sov Sci Rev F Phys Gen Biol. 1994;7:61–89. [Google Scholar]
- 54.Gurfinkel VS, Ivanenko YP, Levik YS. The influence of head rotation on human upright posture during balanced bilateral vibration. Neuroreport. 1995;7:137–140. [PubMed] [Google Scholar]
- 55.Tinbergen N. Ethology and stress diseases. Science. 1974;185:2027. doi: 10.1126/science.185.4145.20. [DOI] [PubMed] [Google Scholar]
- 56.Kendall F, McCreary E, Provance P. Muscles: Testing and Function Baltimore, Md: Williams & Wilkins; 1999.
- 57.Frost M, Stuckey S, Smalley L, Dorman G. Reliability of measuring trunk motions in centimeters. Phys Ther. 1982;62:1431–1437. doi: 10.1093/ptj/62.10.1431. [DOI] [PubMed] [Google Scholar]
- 58.Nelson R, Nestor D. Atlas of standardized low-back test and measures of the National Institute for Occupational Safety and Health. Scandanavian Journal of Work, Environment and Health. 1988;14:82–84. [PubMed] [Google Scholar]
- 59.Gift A. Visual analog scales: measurement of subjective phenomenon. Nurs Res. 1989;38:286. [PubMed] [Google Scholar]
- 60.Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976;2:175–184. [PubMed] [Google Scholar]
- 61.Scott J, Huskisson EC. Vertical or horizontal visual analogue scales. Ann Rheum Dis. 1979;38:560. doi: 10.1136/ard.38.6.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ferraz MB, Quaresma MR, Aquino LR, et al. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol. 1990;17:1022–1024. [PubMed] [Google Scholar]
- 63.Ahles TA, Ruckdeschel JC, Blanchard EB. Cancer-related pain, II: assessment with visual analogue scales. J Psychosom Res. 1984;28:121–124. doi: 10.1016/0022-3999(84)90004-7. [DOI] [PubMed] [Google Scholar]
- 64.Magee D. Orthopedic Physical Assessment Philadelphia, Pa: WB Saunders Co; 2002:34–36.
- 65.Chong RK, Horak FB, Woollacott MH. Time-dependent influence of sensorimotor set on automatic responses in perturbed stance. Exp Brain Res. 1999;124:513–519. doi: 10.1007/s002210050647. [DOI] [PubMed] [Google Scholar]
- 66.Horak FB, Nashner LM. Central programming of postural movements: adaptation to altered support-surface configurations. J Neurophysiol. 1986;55:1369–1381. doi: 10.1152/jn.1986.55.6.1369. [DOI] [PubMed] [Google Scholar]
- 67.Henry SM, Fung J, Horak FB. Control of stance during lateral and anterior/posterior surface translations. IEEE Trans Rehabil Eng. 1998;6:32–42. doi: 10.1109/86.662618. [DOI] [PubMed] [Google Scholar]
- 68.Moe-Nilssen R. Test-retest reliability of trunk accelerometry during standing and walking. Arch Phys Med Rehabil. 1998;79:1377–1385. doi: 10.1016/s0003-9993(98)90231-3. [DOI] [PubMed] [Google Scholar]


