Abstract
The optimal management of renal replacement therapy (RRT) in acute renal failure (ARF) is uncertain. The VA/NIH Acute Renal Failure Trail Network Study (ATN Study) tests the hypothesis that a strategy of intensive RRT will decrease 60-day all-cause mortality in critically ill patients with ARF. Dose separation between the two treatment arms is achieved by increasing the frequency of intermittent hemodialysis (IHD) and sustained low efficiency dialysis (SLED) treatments from three times per week to six times per week, and by increasing continuous venovenous hemodiafiltration (CVVHDF) effluent volume from 20 mL/kg/hr to 35 mL/kg/hr. In both treatment arms, subjects convert between IHD and CVVHDF or SLED as hemodynamic status changes over time. This strategy attempts to replicate the conversion between modalities of RRT that occurs in clinical practice. However, in order to implement this strategy, flexible criteria needed to be developed to provide a balance between the need for uniformity of treatment between groups and practitioner discretion regarding modality of RRT to maintain patient safety. In order to address safety and ethical issues similar to those raised by the Office of Human Research Protections in its review of the ARDS Network studies, a survey of practitioner practices was performed and observational data on the management of RRT in comparable critically ill patients with ARF managed outside of the research context is being collected prospectively. These data will help inform the study’s DSMB and site IRB’s of the relationship between the study’s treatment arms and concurrent clinical practice.
Introduction
Acute renal failure (ARF) is an abrupt loss of renal function resulting in the failure of the kidneys to excrete urea and other nitrogenous waste products. Despite substantial advances in our understanding of the pathogenesis of ARF, clinical advances in treatment have been limited, and morbidity and mortality remain high. Although multiple pharmacologic interventions have shown promise in animal models, no agents have proven to be effective in clinical practice [1,2]. As a result, the management of ARF is primarily supportive, with renal replacement therapy (RRT) serving as the mainstay of treatment in patients with severe renal failure. Despite more than a half-century of experience, many fundamental issues regarding the management of RRT in ARF remain to be resolved, including the indications for and timing of initiation of therapy, the selection of modality of RRT, and the optimal dosing of therapy [3,4].
In patients with ARF, RRT is commonly initiated either to treat overt manifestations of renal failure (i.e., uremic symptoms, volume overload, hyperkalemia and metabolic acidosis) or, in the absence of overt symptoms, in response to progressive azotemia [5]. An increasing number of modalities of RRT are used in clinical practice. Intermittent hemodialysis is the most commonly prescribed form of renal support, usually provided on a three to four times per week schedule. Other modalities, such as the continuous renal replacement therapies (CRRT) and sustained low efficiency dialysis (SLED) have gained increasing acceptance in the management of hemodynamically unstable patients. Although several recent clinical studies have suggested that more intensive renal support may improve survival [6-8], these data have not been widely accepted in clinical practice in the USA [4,9]. In addition, these studies evaluated individual modalities of therapy in isolation rather than evaluating strategies of care that parallel clinical practice.
In light of the lack of consensus regarding best practice of renal support in ARF, the VA/NIH Acute Renal Failure Trial Network Study (ATN Study) was conceived to address the question of whether there is a benefit to delivering more intensive RRT in critically ill patients. The ATN Study is a prospective, randomized trial involving protocol-driven treatment strategies of titrated therapies. It compares a strategy of intensive renal support to more conventionally utilized (conventional) management of RRT, utilizing multiple modalities of RRT within each treatment arm. The primary study hypothesis is that intensive renal support will decrease mortality in critically ill patients with ARF as compared to more conventional management of RRT. Secondary hypotheses are that intensive renal support will shorten the duration of ARF, will decrease the incidence and duration of nonrenal complications, and will be cost-effective. The study is jointly funded by the Cooperative Studies Program of the Department of Veterans Affairs Office of Research and Development and by the National Institute of Diabetes, Digestive and Kidney Diseases. Subject enrollment initiated in November 2003, with a planned close of enrollment in November 2006.
In this report we describe the design, interventions and analysis plan of the ATN Study. In addition, strategies to address concerns raised by the Office of Human Research Protections (OHRP) regarding other studies comparing protocol-driven treatment strategies conducted in the setting of uncertainty regarding prevailing standards of practice [10] are discussed, including the use of practitioner surveys prior to study initiation and the inclusion of an observational cohort to assess processes of care outside of the research setting.
Methods
The complete study protocol is posted online at http://www.atnstudy.org/description.html and is summarized below.
Study setting
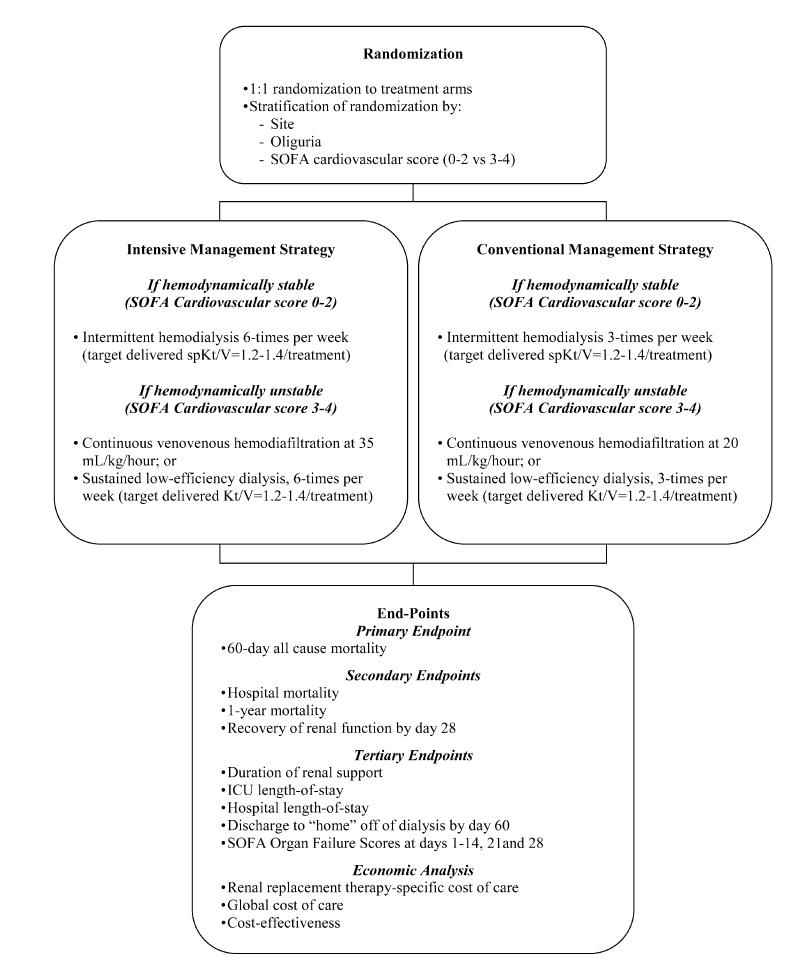
The ATN Study is a multicenter, prospective, randomized, parallel-group trial of two strategies for management of RRT in ARF in critically ill patients being conducted within a network of tertiary care VA and University Medical Centers in the United States (see Appendix 1 for a listing of participating sites) (Figure 1). The study was approved by the Human Rights Committee at the West Haven VA Cooperative Studies Program Coordinating Center, by the Institutional Review Board at the VA Pittsburgh Healthcare System and by the Institutional Review Boards of participating study sites.
Figure 1.
Schematic overview of study design
Population
Eligible subjects are critically ill adults (age ≥ 18 years) with ARF due to acute tubular necrosis (ATN) who require support with RRT. For the purpose of this study, ARF is defined as an increase in serum creatinine of 2.0 mg/dL in men, and 1.5 mg/dL in women, over no more than four days, or the presence of oliguria (average urine volume ≤ 20 mL/hr) for more than 24 hours despite volume resuscitation. The specific inclusion and exclusion criteria are listed in Table 1. Operational criteria for the exclusion of etiologies of ARF other than ATN are summarized in Table 2.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria |
| 1) Acute renal failure clinically consistent with a diagnosis of acute tubular necrosis, defined as: |
| a) Clinical setting of ischemic or nephrotoxic injury AND |
| b) Oliguria (average urine output ≤20 mL/hr) for >24 hours or an increase in serum creatinine of ≥2 mg/dL in males or ≥1.5 mg/dL in females over a period of ≤4 days |
| 2) Plan for renal replacement therapy by the clinical team |
| 3) Receiving care in a critical care unit |
| 4) One nonrenal organ failure (SOFA organ system score ≥2) or the presence of sepsis |
| 5) Age ≥ 18 years |
| 6) Subject/surrogate willing to provide informed consent |
| Exclusion criteria |
| 1) Baseline serum creatinine > 2 mg/dL in males, > 1.5 mg/dL in females |
| 2) Acute renal failure clinically believed to be due to an etiology other than ATN |
| 3) More than 72 hours since meeting both of the following conditions: |
| a) Fulfillment of the definition of ARF; and |
| b) BUN > 100 mg/dL |
| 4) More than one hemodialysis treatment or more than 24 hours since starting CRRT |
| 5) Prior kidney transplant |
| 6) Pregnancy |
| 7) Prisoner |
| 8) Weight > 128.5 kg |
| 9) Noncandidacy for renal replacement therapy |
| 10) Moribund state |
| 11) Subject not expected to survive 28 days because of underlying terminal chronic medical condition |
| 12) Comfort-measures only status |
| 13) Participation in a concurrent interventional study |
| 14) Subject/surrogate refusal |
| 15) Physician refusali |
Table 2.
Clinical criteria for diagnosis of etiologies of ARF other than ATN
| Etiology of ARF | Clinical criteria |
|---|---|
| Prerenal azotemia | 1) Underlying absolute or hypovolemia |
| 2) Improvement in renal function with volume loading or inotropic support | |
| 3) Fractional excretion of sodium <1% and/or fractional excretion of urea <35% | |
| 4) Bland urine sediment | |
| Obstructive uropathy | 1) Bladder outlet obstruction diagnosed by elevated postvoid residual bladder function |
| 2) New or progressive hydronephrosis on renal ultrasound or other imaging or | |
| 3) Improvement in renal function following decompression of urinary collecting system | |
| Allergic interstitial nephritis | 1) Appropriate clinical setting (e.g., drug exposure, infection) |
| 2) Clinical syndrome of fever and/or skin rash and/or eosinophilia | |
| 3) Urine sediment with hematuria, pyuria, or leukocyte casts and | |
| 4) Eosinophiluria | |
| Acute or rapidly progressive glomerulonephritis | 1) Positive serologic marker(s) |
| 2) Urine sediment with dysmorphic red blood cells or red blood cell casts and/or | |
| 3) Renal biopsy demonstrating proliferative or crescentic glomerulonephritis | |
| Vasculitis | 1) Positive serologic marker(s) |
| 2) Urine sediment with dysmorphic red blood cells or red blood cell casts and/or | |
| 3) Biopsy of kidney or other tissue demonstrating acute vasculitis | |
| Hemolytic-uremic syndrome (HUS)/Thrombotic thrombocytopenic purpura (TTP) | 1) Microangiopathic hemolytic anemia |
| 2) Thrombocytopenia | |
| 3) Absence of disseminated intravascular coagulation (DIC) | |
| Malignant hypertension | 1) Severe (Stage III) hypertension |
| 2) Neurologic changes | |
| 3) Retinal hemorrhages, exudates or papilledema and | |
| 4) Hematuria and/or red blood cell casts | |
| Scleroderma renal crisis | 1) Diagnosis of scleroderma |
| 2) Acute onset of renal failure and | |
| 3) Abrupt onset of moderate to severe hypertension | |
| Atheroembolism | 1) Clinical setting (e.g., recent intra-arterial catheterization, recent vascular surgery or anticoagulation) |
2) Presence of some or all of the following:
|
|
| Multiple myeloma | 1) Known or suspected diagnosis of multiple myeloma |
| 2) Presence of immunoglobulin light chains in the urine on UPEP | |
| 3) Serum paraprotein detected on SPEP | |
| Functional or surgical nephrectomy | 1) Surgical nephrectomy (bilateral) or |
2) Bilateral renal infarction (secondary to thromboemboli, renal artery dissection or renal vein thrombosis) manifested by
|
|
| Cyclosporin or tacrolimus nephrotoxicity | 1) Elevated cyclosporin or tacrolimus drug levels and |
| 2) Improvement in renal function following reduction or discontinuation of drug | |
| Hepatorenal syndrome | 1) Chronic or acute liver disease with advanced hepatic failure and portal hypertension |
| 2) Absence of shock, ongoing bacterial infection, fluid loss and current or recent treatment with nephrotoxic drugs | |
| 3) Absence of ongoing $$Word$$ fluid losses or renal fluid losses | |
| 4) Absence of sustained improvement in renal function after withdrawal of diuretics and expansion of plasma volume with 1.5 L of isotonic saline (administered over 4 to 6 hours) and | |
| 5) Absence of proteinuria >500 mg/d, absence of ultrasound evidence of obstructive uropathy or parenchymal renal disease | |
| Tumor Lysis Syndrome | 1) Rapidly growing malignancy |
| 2) Serum uric acid >20 mg/dL | |
| 3) Urine uric acid to creatinine ratio >1. |
Informed consent is obtained from all study subjects. However, the majority of study subjects enrolled to date have had impaired decision-making capacity at the time of study enrollment and have been enrolled on the basis of consent from legal surrogates. Re-consent is obtained from each subject enrolled on the basis of surrogate consent upon reattainment of decision-making capacity.
Design
Randomization
Subjects fulfilling the inclusion and exclusion criteria and providing informed consent are randomized equally to the two treatment arms. Randomization is stratified by site, and within sites by SOFA Cardiovascular Organ Failure Score (0-2 versus 3-4) and by the presence or absence of oliguria. A centralized, automated telephone system isused to access a computer-generated adaptive randomization scheme.
Interventions
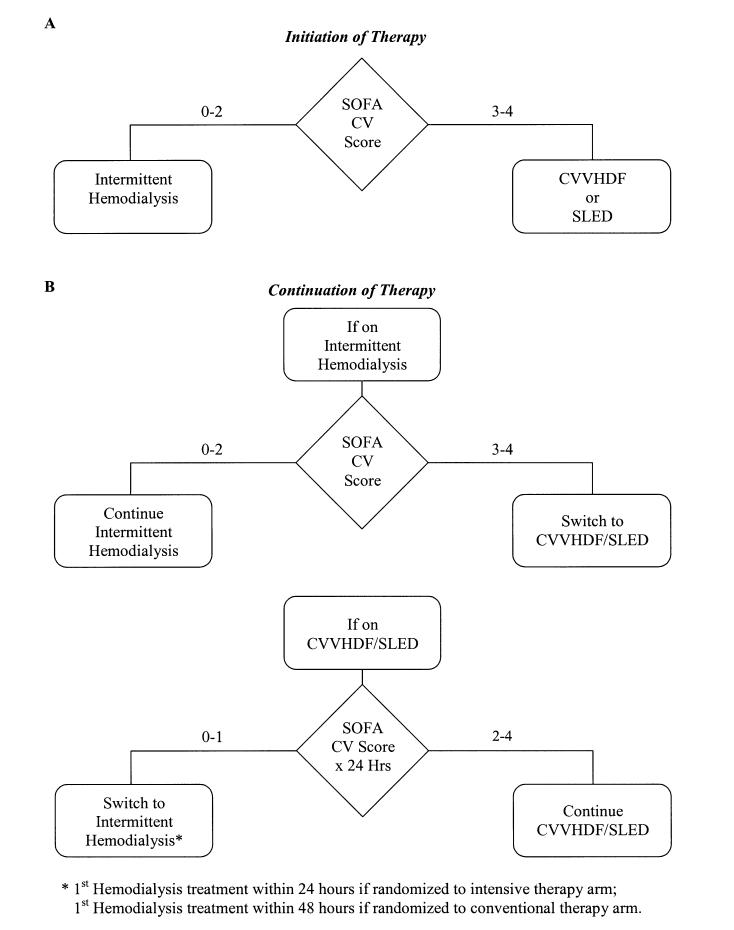
The management of RRT is standardized across study sites, subject to individualized clinical judgment of patient safety. Intermittent hemodialysis (IHD), continuous venovenous hemodiafiltration (CVVHDF) and sustained low efficiency dialysis (SLED) are used in both treatment arms, with the modality of treatment dictated by the subject’s hemodynamic status (Figure 2). The use of either CVVHDF or SLED is determined by site-specific practice. Intermittent hemodialysis is used in hemodynamically stable subjects; CVVHDF and SLED is reserved for subjects in whom hemodynamic instability (SOFA Cardiovascular Score of 3-4) proscribes the use of intermittent hemodialysis. Subjects receiving CVVHDF or SLED are converted to intermittent hemodialysis when hemodynamic instability has resolved (SOFA Cardiovascular Score of 0-1 for >24 hours). While these guidelines for selection of modality are designed to ensure similar management between the two treatment arms, practitioner discretion is permitted to assure optimal patient safety.
Figure 2.
Selection of modality of renal replacement therapy within each treatment arm. Panel A. Initial selection of modality of renal replacement therapy. Panel B. Subsequent assignment of modality of renal replacement therapy
In the intensive RRT strategy, IHD and SLED are provided six times per week (Monday through Saturday) and CVVHDF is dosed to provide a total effluent flow rate (i.e., the sum of dialysate and ultrafiltrate flow rates) of 35 mL/kg/hr. In the conventional RRT strategy intermittent hemodialysis and SLED are provided three times per week (Monday, Wednesday and Friday or Tuesday, Thursday and Saturday) and CVVHDF is dosed to provide a total effluent flow rate of 20 mL/kg/hr. Isolated ultrafiltration is provided on nondialysis days if necessary for volume management. In both treatment arms, IHD and SLED are prescribed to deliver a target single-pool (sp) Kt/Vurea of 1.2 to 1.4 per treatment. The delivered spKt/Vurea is measured at least three times per week during the first two weeks and weekly thereafter, and the treatment prescription adjusted as needed.
Renal replacement therapy is continued as per study protocol until renal function recovers, a decision is made by the subject or surrogate decision-maker to withdraw life-sustaining therapy, or the subject dies. For the purpose of discontinuation of RRT, assessment of renal recovery is based on an increase in measured creatinine clearance (based on six hour timed urine collection) to greater than 12 to 20 mL/min or a spontaneous fall in serum creatinine. Subjects who have persistent renal failure at day 28 postrandomization or at the time of discharge from acute care, whichever comes first, are taken off protocol treatment and prescribed further dialysis at the discretion of the primary treatment team.
Data collection
Baseline data collection includes demographic data, history and physical examination, medications, comprehensive laboratory assessment, hemodynamic assessment and assessment of nutritional management. Chronic comorbidities and acuity of illness are assessed using standard assessment scores [11-14]. Detailed data on renal replacement therapy are collected on a daily basis through to day 28 or the end of dialysis dependence, whichever comes first. Laboratory data collection, hemodynamic assessment and assessment of nutritional management are completed on study days 1-14, 21 and 28. Follow-up outcome data are collected at day 60 (primary end-point) and at hospital discharge. As most subjects are not hospitalized at day 60, these data are collected by telephone or mail. Follow-up at one-year is performed by telephone or mail. In addition, survival at one-year will be ascertained based on vital statistic registries, including the VA Beneficiary Identification and Records Locator System (BIRLS), the National Center for Health Statistics’ National Death Index database and the Social Security Administration’s Death Master File.
Endpoints
The primary study endpoint is 60-day all-cause mortality. Secondary endpoints include all-cause hospital mortality, one-year mortality, and recovery of renal function (defined as lack of need for continuing dialysis support, with a minimum creatinine clearance of 20 mL/min) by day 28. Recovery of renal function will be categorized as complete or partial with complete recovery of renal function defined as a serum creatinine that is no more than 0.5 mg/dL greater than baseline and partial recovery as a serum creatinine >0.5 mg/dL greater than base-line but not dialysis-dependent. Subjects who remain dialysis dependent at study completion or at time of death will be categorized as having no recovery of renal function.
Tertiary outcomes to be evaluated include duration of renal support, ICU length-of-stay, hospital length-of-stay, and SOFA Scores at days 1-14, day 21 and day 28. The ability of the subject to return to his or her prior living situation (“home”) without requiring ongoing renal replacement therapy will be assessed using the combined endpoint of discharge to home off dialysis by day 60, where home is defined as the subject’s premorbid living situation.
Biorepository
Serum, plasma and DNA samples from subjects participating in the study will be maintained in a biorepository for future use. Plasma and serum are obtained prior to the initiation protocol therapy and on study day 8. Biorepository samples are stored at the Massachusetts Veterans Epidemiology Research and Information Center (MAVERIC) Laboratory at the VA Boston Healthcare System. Biorepository samples will be accessible to all qualified investigators. Linkage to clinical information will be provided using a deidentified data set linked to the coded sample ID numbers after completion of a data-use agreement. The clinical data provided in this data set will include the minimum data elements required by the investigator.
A separate informed consent is utilized for the DNA repository. For subjects lacking decision-making capacity, informed consent to obtain the DNA sample is obtained from the legally identified surrogate decision-maker; however, the DNA sample is not logged into the DNA repository until the subject regains decision-making capacity and provides consent. If the subject does not provide consent, the sample is destroyed. If the subject expires prior to regaining decision-making capacity, further consent is not required and the specimen is logged into the DNA repository.
Observational cohort
In order to ascertain the relationship between the study treatment arms and the standard of care for management of RRT outside of the research context, observational data are being collected on the management of RRT in patients excluded from the primary study as the result of inability to obtain informed consent within the eligibility window. Demographic data collected include age, gender, race, and etiology of ARF. Clinical data include the timing of initiation of RRT, the indications for RRT, and the blood urea nitrogen concentration and SOFA cardiovascular score on the day RRT was initiated. Detailed treatment data, analogous to that collected on subjects in the intervention trial, are collected for each RRT treatment for two weeks following screening.
Data management
All data are collected at study sites using scannable case report forms and are centrally submitted to the VA CSP Coordinating Center in West Haven, Connecticut. Submitted forms are reviewed, scanned, verified and exported into a data file using an optical character recognition software package (Teleform® Elite v 8.1, Verity, Inc., Sunnyvale, CA). Once data forms are processed, they are exported to an in-house computer system. On a weekly basis the accumulated subject information is transferred to SAS® version 8.2 data sets (SAS Institute, Inc., Cary, NC). Newly entered information is screened for missing or out-of-range values and computer-generated notices are sent to the participating investigators requesting completion, correction, or verification of specific data items. A computer-generated edit message indicating the questionable data is used to monitor coding errors and edit the data on the main computer file when the requested information is returned. A computerized record is kept of the number and types of errors to ensure a high level of data integrity. Interim progress reports of cumulative errors and overall data quality are sent to the investigators and the Executive Committee. To maintain a consistent quality of measurement and protocol adherence among study sites and to avoid systematic errors, frequency distributions of key clinical variables and protocol adherence reports are generated and communicated with medical sites on a routine basis.
Planned statistical analysis
Sample size and power
Sample size and power calculations were based on the primary endpoint, 60-day all-cause mortality. A meta-analysis of 11 published studies [6-8,15-22] encompassing 2534 critically ill patients with ARF performed during the development of the study protocol demonstrated an estimated mortality of approximately 55%. It was determined that 1164 subjects will be necessary to detect a reduction in mortality to 45% (10% absolute reduction in mortality) with a power of 0.90 at a two-sided significance level of 0.05, allowing for a 10% dropout rate.
Interim monitoring and analyses
Interim monitoring will focus on both the efficacy and safety of the study. Trial safety is being monitored after 60-day follow-up of each 200-subject block, or every 6 months, whichever comes first. At these interim safety analyses, a one-sided significance level of 0.00005 is used as the criterion for assessment of efficacy, even though no assessment of efficacy is intended. The inflated type-1 error will be ignored.
Planned interim efficacy analyses will be performed when 600 and 900 subjects have been enrolled and followed for 60 days. For the interim efficacy analyses, a wide boundary such as that proposed by Haybittle and Peto will be used [23]. The one-sided significance level in favor of intensive treatment for the interim analyses will be 0.0005. Feasibility monitoring will be performed at the two interim efficacy analyses based on the conditional power for the trend.
Final analysis
All analyses will be performed based on intention-to-treat. Analysis of the primary endpoint, 60-day all-cause mortality, will be performed using a conditional logistic regression for a binary endpoint. Two analyses will be carried out: 1) treatment adjusted for the study design (cardiovascular SOFA score, oliguric status and site); and 2) treatment adjusted for the study design and for a set of prespecified explanatory variables. Treatment by explanatory variable interactions will be examined in exploratory analyses. These explanatory variables include gender, age at randomization, primary diagnosis, Charlson Comorbidity score, etiology of acute renal failure, presence of oliguria, acuity of illness scores, use of mechanical ventilation, and presence of sepsis. Prespecified subgroup analyses will be performed for oliguric status, cardiovascular SOFA score, and gender.
A significance level of 0.05 (two-sided) will be used for all secondary outcomes. All-cause hospital mortality by day 60 will be analyzed in a manner similar to the primary outcome. One-year all-cause mortality will be analyzed using Kaplan-Meier survival curves, adjusted for censoring due to loss to follow-up. Treatment group comparisons will be based on the stratified log-rank test. The Cox proportional hazards model will be used to test the effect of treatment adjusted for the study design and for the prespecified set of covariates. A similar analysis will be conducted for 60-day all-cause mortality. Recovery of renal function by 28 days is a three-level ordinal measurement: none, partial, and complete recovery. A conditional odds ratio model will be used to investigate the effect of treatment on recovery of renal function.
Economic analysis
This study will include cost-outcome and cost-effectiveness analyses. The cost-outcome analysis will compare the difference in total costs between the intensive and conventional treatment arms to the difference in the primary outcome, 60-day mortality. The cost-effectiveness analysis will compare the change in quality-adjusted life years (QALYs) between the arms to the difference in costs. Economic data will include vital status, health care utilization, costs, and preferences (utilities). Vital status and health care utilization will come from study forms, hospital data systems, and public records. Costs will be extracted from providers’ electronic data systems. Actual cost estimates will be available from VA sites; non-VA sites will provide patient charges that will then be adjusted using facility-specific Medicare cost-to-charge ratios. The Health Utilities Index® (HUI) will be administered at 60 days and 12 months after randomization to measure utility. HUI scores will be converted to utility scores (range 0.0-1.0) based on surveys of general populations [24]. A societal viewpoint will be adopted for the economic analyses. The range of costs considered will include direct inpatient and outpatient care costs, indirect costs for travel, and the value of patients’ and informal caregivers’ time spent obtaining or delivering care [25].
Discussion
The ATN Study is designed to compare two management strategies for renal replacement therapy in critically ill patients with acute renal failure to determine if increased intensity of therapy is associated with improved outcomes.
Limitations in the design of prior studies
Prior studies have suggested that greater intensity of renal replacement therapy in ARF is associated with improved patient survival [6-8]; however, these have been limited in number and have had significant limitations in study designs. Ronco et al. [8] compared three doses of continuous venovenous hemodiafiltration in 425 subjects with ARF at a single center. An effluent flow rate of 20 mL/kg/min was associated with a patient survival of 41% as compared to survivals of 57% and 58% with effluent flow rates of 35 mL/kg/hr and 45 mL/kg/hr, respectively. A subsequent study by Bouman et al. [26] did not confirm this benefit, however, this study was underpowered and its observed 28-day patient survival of 72.6% suggests inclusion of a less critically ill study population. Schiffl et al. [7] compared daily hemodialysis to every-other-day hemodialysis in 160 subjects. Although there was a reduction in mortality from 46% with every-other-day hemodialysis to 28% in the daily treatment group, several methodological concerns have been raised about this study [4]. Subjects were assigned to therapy on an alternating basis, rather than by random assignment, although their baseline characteristics were comparable. More importantly, the delivered dose of dialysis was substantially lower than the target spKt/Vurea of 1.2, resulting in an elevated time-averaged blood urea nitrogen concentration (104 ± 18 mg/dL) and a high frequency of uremic complications in the every-other-day treatment arm. The results of this study may have reflected less than adequate therapy in the every-other-day treatment arm rather than an actual benefit of intensive therapy [4]. In order to avoid this issue, the delivered dose of hemodialysis in the present study will be intensively monitored and the prescription adjusted to ensure delivery of an adequate dose of therapy [27].
In none of these studies were subjects permitted to transfer between modalities of treatment in response to changes in hemodynamic status, as commonly occurs in clinical practice, leading to restricted subject eligibility in some studies [7] and limited generalizability. In contrast, the ATN Study was designed with the expectation that subjects’ hemodynamic status will change over the course of the study, necessitating conversion between modalities of therapy. This use of integrated management strategies combining intermittent hemodialysis and CVVHDF or SLED, yet maintaining separation of intensity of therapy for each modality between strategies represents a unique innovation in the design of the study. While this design will make the results of the study more immediately generalizable to clinical practice, the combination of multiple modalities of RRT within each treatment arm introduced several issues that needed to be explicitly addressed in the study’s design.
Comparability of dose of RRT between modalities
The first issue was the comparability of dose between modalities of RRT. Although several mathematical models has been developed to correlate the dose of RRT given on different schedules, none of these models has been validated in clinical practice [28-30]. As a result, the doses of continuous and intermittent therapy selected for the conventional treatment arm were based on an assessment of current clinical practice [9], rather than on theoretical assessment of equivalence of dose. In the intensive treatment arm, the dosing of intermittent hemodialysis and SLED was established by doubling the frequency of treatment while the dose of CVVHDF was increased slightly less than twofold, as published data do not suggest further improvement in outcome with doses of CRRT beyond 35 mL/kg/hr [8].
Integration of RRT modalities within treatment arms
A second issue was the potential for confounding that could result if the patterns of switching between modalities differed between treatment arms. Although prior studies have not demonstrated differences in survival between intermittent and continuous therapy [19,31-33], significant differences in the pattern of utilization of CVVHDF and SLED as compared to intermittent hemodialysis between the groups could introduce bias and confound interpretation of the results. For this reason, an algorithm for daily determination of modality of therapy was developed based on each day’s cardiovascular SOFA score. Implementation of this algorithm has, however, required a degree of flexibility to accommodate practitioner assessment of patient safety. Deviations from the algorithm have been necessary primarily in subjects who have been assessed to be more unstable than predicted by the cardiovascular SOFA score. These deviations are closely monitored to ensure that they do not introduce bias.
Issues derived from OHRP’s review of the ARDS Network studies
In July 2003, several months prior to the initiation of this study’s enrollment, the Office of Human Research Protections (OHRP) of the United States Department of Health and Human Services issued findings in response to concerns that had been raised regarding two studies conducted by the Acute Respiratory Distress Syndrome (ARDS) Network [10]. The ARDS Network is a clinical trials network funded by the National Heart, Lung and Blood Institute of the National Institutes of Health. In May 2000 the ARDS Network published the findings of a study demonstrating improved survival with lower tidal volume mechanical ventilation in patients with ARDS [34]. This trial utilized two protocol-driven treatment strategies: an “experimental” arm with a lower tidal volume (6 mL/kg) and a “control” arm with a higher tidal volume (12 mL/kg), which the investigators believed corresponded to traditional recommendations for the management of mechanical ventilation. Two years after publication of the study results, the use of the protocol-driven higher tidal volume treatment arm as the control group was criticized as not representative of the best practice standards prevailing at the time of the trial [35]. The authors of this critique stated that this “study design may have resulted in substantial numbers of control subjects receiving inferior treatment” and contended that a nonprotocol-driven control group representing “what is believed by participating physicians to be the best current care” (“wild-type” therapy) should have been included to provide generalizable results and to safeguard patient safety [35]. Furthermore, they suggested that the same design issues were present in an ongoing ARDS Network study evaluating the use of hemodynamic monitoring and fluid management strategies. Prompted by these criticisms, OHRP initiated an investigation of the two ARDS Network studies and, at the request of OHRP, NHLBI suspended the FACTT Trial.
In its opinion, issued in a letter dated 3 July 2003, OHRP did not directly comment on the appropriateness of the design of the two trials, deferring to the near unanimous opinion of a panel of outside consultants that the risks to subjects participating in the trials “were minimized and reasonable” [10]. However, OHRP faulted the institutional review boards (IRBs) for their oversight of the studies, stating that they had failed to obtain sufficient information required to assess the risks to subjects [10]. Specifically, OHRP stated that: “the IRBs should have received information adequate to assess the risks and potential benefits of each of the interventions for each arm of the ... trial relative to concurrent routine clinical practice outside of the research context” [10].
The design of the ATN Study has many similarities to these two ARDS Network trials. All three studies compare protocol-driven treatment strategies of titrated therapies; there is no clear consensus regarding best practice or precise knowledge of current practice patterns for the therapies being evaluated; and none of the trials was designed with a “wild-type” treatment arm as a control group.
Following the release of the OHRP findings, we considered multiple strategies to address these issues. The addition of a “wild-type” treatment arm was considered but was not feasible due to budgetary constraints. In addition, the scientific validity of a “wild-type” treatment arm was felt to be questionable given the likelihood of drift in treatment practice over time due to a Hawthorne effect. As an alternative, we implemented two strategies to assure IRBs at the participating institutions that the conventional treatment arm paralleled clinical practice. First, as a review preparatory to research, practitioners at participating study sites were surveyed regarding their management of RRT in critically ill patients with ARF [9]. The results of this survey were provided to the study’s Data and Safety Monitoring Board (DSMB) and the West Haven VA CSP Coordinating Center’s Human Rights Committee, and aggregate and site-specific data were provided to each participating site for review by their IRB. Secondly, the study protocol was amended to include the observational cohort. This cohort will provide an ongoing, objective assessment of the management of RRT in the study population outside of the research context. Observational data will be collected throughout the duration of the study to detect changes in practice patterns over time. Because this cohort is not randomized, and may not be fully comparable to the study population, only process of care data is being collected, and no outcome data will be obtained. As with the practitioner survey, the data from the observational cohort will be reported to the study’s DSMB, the West Haven VA CSP Coordinating Center’s Human Rights Committee and to each participating institution’s IRB in order to document the relationship between the study’s treatment arms and concurrent clinical practice.
Summary
The ATN Study is a multicenter, randomized, parallel group trial comparing an intensive to a more conventional dosing strategy for the management of RRT in ARF. The study is the largest clinical trial of RRT in ARF. Unlike prior studies that have focused on dosing of single modalities of therapy, or comparisons between modalities of therapy, the study was designed based on the paradigm of RRT as a multimodality therapy, with subjects converting between modalities on the basis of changes in hemodynamic status over time. The development of a dosing trial based on this paradigm necessitated pragmatic decisions regarding comparability of dosing between modalities within each treatment arm and the development of explicit rules for conversion between modalities of therapy. In addition, the study has incorporated both practitioner surveys and an observational cohort to monitor the process of care of patients with ARF who receive RRT outside of the research setting in order to address the concerns raised by OHRP regarding assurance of patient safety in studies comparing protocol-driven treatment strategies. The design and execution of the ATN Study should be informative for the development of future clinical trials.
Acknowledgement
This study is supported by the Cooperative Studies Program of the Department of Veterans Affairs Office of Research and Development and by the National Institute of Diabetes, Digestive and Kidney Diseases by interagency agreement Y1-DK-3508-01.
Appendix 1
VA/NIH Acute Renal Failure Trial Network (ATN) Study
Planning/executive committee
*Paul M Palevsky, MD, Chairman, VA Pittsburgh Healthcare System, Pittsburgh, PA
*Theresa Z O’Connor, PhD, CSP Coordinating Center, VA Connecticut Healthcare System, West Haven, CT
*Jane H Zhang, PhD, CSP Coordinating Center, VA Connecticut Healthcare System, West Haven, CT
*Glenn M Chertow, MD, MPH, University of California, San Francisco, San Francisco, CA
*Susan Crowley, MD, VA Connecticut Healthcare System, West Haven, CT
*Devasmita Choudhury, MD, VA North Texas Healthcare System, Dallas, TX
John Daugirdas, MD, University of Illinois, Chicago, IL
David Goldfarb, MD, New York VA Medical Center, New York, NY
*John Kellum, MD, University of Pittsburgh, Pittsburgh, PA
Bruce Molitoris, MD, Indiana University, Indianapolis, IN
*Emil Paganini, MD, Cleveland Clinic Foundation, Cleveland, OH
*Roland MH Schein, MD, Miami VA Medical Center, Miami, FL
John B Stokes, University of Iowa, Iowa City, IA
*B Taylor Thompson, MD, Massachusetts General Hospital, Boston, MA
*Mark W Smith, PhD, Health Economics Resource Center, VA Palo Alto Health Care System, Menlo Park, CA
*Kathy Swanson, RPh, CSP Research Pharmacy Coordinating Center, New Mexico VA Healthcare System, Albuquerque, NM
*Peter Peduzzi, PhD, (Ex Officio), Director CSP Coordinating Center, VA Connecticut Healthcare System, West Haven, CT
*Robert Star, MD (Ex Officio), Senior Scientific Advisor, NIDDK, Bethesda, MD
*Executive Committee member.
Participating Sites (Primary Site Investigator)
VA Ann Arbor Healthcare System, Ann Arbor, MI (E Young, MD)
VA Baltimore Maryland Healthcare System, Baltimore, MD (M Hise, MD)
VA Western NY Healthcare System, Buffalo, NY (J Lohr, MD)
VA North Texas Healthcare System, Dallas, TX (D Choudhury, MD)
VA Eastern Colorado Health Care System, Denver, CO (M Chonchol, MD)
Houston VA Medical Center, Houston, TX (G Dolson, MD)
Richard L Roudebush VA Medical Center, Indianapolis, IN (R Bacallao, MD)
Central Arkansas Veterans Healthcare Center, Little Rock, AK (M Krause, MD)
West Los Angeles VA Healthcare Center, Los Angeles, CA (J Kraut, MD)
Miami VA Medical Center, Miami, FL (RMH Schein, MD)
VA Tennessee Valley Healthcare System, Nashville, TN (TA Ikizler, MD and W Stone, MD)
New Orleans VA Medical Center, New Orleans, LA (V Batuman, MD)
VA Pittsburgh Healthcare System, Pittsburgh, PA (M Ramkumar, MD)
Portland VA Medical Center, Portland, OR (S Watnick, MD)
Hunter Holmes McGuire VA Medical Center, Richmond, VA (G Feldman, MD)
VA San Diego Healthcare System, San Diego, CA (F Gabbai, MD)
San Francisco VA Medical Center, San Francisco, CA (K Johansen, MD)
San Juan VA Medical Center, San Juan, PR (C Rosado-Rodriguez, MD)
VA Puget Sound Healthcare System, Seattle, WA (D Andress, MD)
VA Connecticut Healthcare System, West Haven, CT (S Crowley, MD)
Cleveland Clinic Foundation, Cleveland, OH (E Paganini, MD)
Johns Hopkins University (H Rabb, MD)
Massachusetts General Hospital, Boston, MA (J Niles, MD)
Medical College of Georgia, Augusta, GA (H Szerlip, MD)
University of California, San Francisco, San Francisco, CA (G Chertow, MD)
University of Miami, Miami, FL (G Contreras, MD, MPH)
University of Pittsburgh, Pittsburgh, PA (M Unruh, MD)
University of Texas at Houston, Houston, TX (K Finkel, MD)
M.D. Anderson Cancer Center, Houston, TX (A Shaw, MD)
Wake Forest University, Winston-Salem, NC (M Rocco, MD)
Washington University at St. Louis, St. Louis, MO (A Vijayan, MD)
References
- Star RA. Treatment of acute renal failure. Kidney Int. 1998;54:1817–31. doi: 10.1046/j.1523-1755.1998.00210.x. [DOI] [PubMed] [Google Scholar]
- Lameire N, Vanholder R. Pathophysiologic features and prevention of human and experimental acute tubular necrosis. J Am Soc Nephrol. 2001;12(Suppl 17):S20–S32. [PubMed] [Google Scholar]
- Karsou SA, Jaber BL, Pereira BJG. Impact of intermittent hemodialysis variables on clinical outcomes in acute renal failure. Am J Kidney Dis. 2000;35:980–991. doi: 10.1016/s0272-6386(00)70276-9. [DOI] [PubMed] [Google Scholar]
- Mehta RL, Letteri JM. Current status of renal replacement therapy for acute renal failure. A survey of US nephrologists. Am J Nephrology. 1999;19:377–82. doi: 10.1159/000013481. [DOI] [PubMed] [Google Scholar]
- Bonventre JV. Daily hemodialysis - will treatment each day improve the outcome in patients with acute renal failure. N Engl J Med. 2002;346:632–34. doi: 10.1056/NEJM200201313460512. [DOI] [PubMed] [Google Scholar]
- Paganini EP, Tapolyai M, Goormastic M, et al. Establishing a dialysis therapy/patient outcome link in intensive care unit acute dialysis for patients with acute renal failure. Am J Kidney Dis. 1996;28(Suppl 3):S81–S89. [Google Scholar]
- Schiffl H, Lang SM, Fischer R. Daily hemodialysis and the outcome of acute renal failure. N Engl J Med. 2002;346:305–10. doi: 10.1056/NEJMoa010877. [DOI] [PubMed] [Google Scholar]
- Ronco C, Bellomo R, Homel P, et al. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomized trial. Lancet. 2000;356:26–30. doi: 10.1016/S0140-6736(00)02430-2. [DOI] [PubMed] [Google Scholar]
- Pesacreta M, Overberger P, Palevsky PM, the VA/NIH Acute Renal Failure Trial Network Management of renal replacement therapy in acute renal failure: A survey of practitioner prescribing practices. J Am Soc Nephrol. 2004;15:350A. doi: 10.2215/CJN.00780207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borror K, Carome MA.Human research subject protections under federalwide assurance (FWA) 3136, multiple project assurances (MPA) M-1331, M-1363, and M-1338 and the OHRP approved assurances for all ARDS Network institutions July2003Massachusetts General Hospital; Lee E. Limbard, Vanderbilt University; and Robert Kay, Cleveland Clinic Foundation. Office for Human Research Protections, Department of Health and Human Services; Available at http://www.hhs.gov/ohrp/detrm_letrs/YR03/jul03a.pdf. Accessed 3 March 2005 [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- Knaus W, Draper E, Wagner D, Zimmerman J. APACHE II: severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- Paganini EP, Halstenberg WK, Goormastic M. Risk modeling in acute renal failure requiring dialysis: the introduction of a new model. Clin Nephrol. 1996;46:206–11. [PubMed] [Google Scholar]
- De Mendonça A, Vincent JL, Suter PM, et al. Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intens Care Med. 2000;26:915–21. doi: 10.1007/s001340051281. [DOI] [PubMed] [Google Scholar]
- Chertow GM, Christiansen CL, Cleary PD, Munro C, Lazarus JM. Prognostic risk stratification in critically ill patients with acute renal failure requiring dialysis. Arch Int Med. 1995;155:1505–11. [PubMed] [Google Scholar]
- Liano F, Pascual J, the Madrid Acute Renal Failure Study Group Epidemiology of acute renal failure: a prospective, multicenter, community-based study. Kidney Int. 1996;50:811–18. doi: 10.1038/ki.1996.380. [DOI] [PubMed] [Google Scholar]
- Johnson JP, Johnston JR, Flick R, Singh A, Angus D, Greenberg A. Acute renal failure in recipients of organ transplantation and non-transplantation patients: comparison of characteristics and mortality. Ren Fail. 1997;19:461–73. doi: 10.3109/08860229709047732. [DOI] [PubMed] [Google Scholar]
- Mehta R, McDonald B, Gabbai F, et al. A randomized clinic trial of continuous versus intermittent dialysis for acute renal failure. Kidney Int. 2001;60:1154–63. doi: 10.1046/j.1523-1755.2001.0600031154.x. [DOI] [PubMed] [Google Scholar]
- Liano F, Junco E, Pascual J, Madero R, Verde E, the Madrid Acute Renal Failure Study Group The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. Kidney Int. 1998;53(Suppl 66):S16–S24. [PubMed] [Google Scholar]
- Van Bommel EF, Bouvey ND, Hop WC, Bruining HA, Weimar W. Use of APACHE II classification to evaluate outcome and response to therapy in acute renal failure patients in a surgical intensive care unit. Ren Fail. 1995;17:731–42. doi: 10.3109/08860229509037641. [DOI] [PubMed] [Google Scholar]
- Fiaccadori E, Maggiore U, Lombardi M, Leonardi S, Rotelli C, Borghetti A. Predicting patient outcome from acute renal failure comparing three general severity of illness scoring systems. Kidney Int. 2000;58:283–92. doi: 10.1046/j.1523-1755.2000.00164.x. [DOI] [PubMed] [Google Scholar]
- Lakatos E. Sample size based on the log-rank statistics in complex clinical trials. Biometrics. 1988;44:229–241. [PubMed] [Google Scholar]
- Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): concepts, measurement properties and applications. Health and Quality of Life Outcomes. 2003;1:54–66. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. Oxford University Press; New York: 1996. [Google Scholar]
- Bouman CSC, Oudemans-van Straaten HM, Tijssen JGP, Zandstra DF, Kesecioglu J. Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: a prospective, randomized trial. Crit Care Med. 2002;30:2205–11. doi: 10.1097/00003246-200210000-00005. [DOI] [PubMed] [Google Scholar]
- Kellum JA, Mehta RL, Angus DC, Palevsky P, Ronco C, the ADQI Workgroup The first international consensus conference on continuous renal replacement therapy. Kidney Int. 2002;62:1855–63. doi: 10.1046/j.1523-1755.2002.00613.x. [DOI] [PubMed] [Google Scholar]
- Keshaviah P, Nolph K, Van Stone J. The peak concentration hypothesis: a urea kinetic approach to comparing the adequacy of continuous ambulatory peritoneal dialysis (CAPD) and hemodialysis. Perit Dial Int. 1989;9:257–60. [PubMed] [Google Scholar]
- Gotch F. The current place of urea kinetic modeling with respect to different dialysis schedules. Nephrol Dial Transplant. 1998;13(Suppl 6):10–14. doi: 10.1093/ndt/13.suppl_6.10. [DOI] [PubMed] [Google Scholar]
- Casino F, Lopez F. The equivalent renal urea clearance: a new parameter to assess dialysis dose. Nephrol Dial Transplant. 1996;11:1574–81. [PubMed] [Google Scholar]
- Augustine JJ, Sandy D, Seifert TH, Paganini EP. A randomized controlled trial comparing intermittent with continuous dialysis in patients with ARF. Am J Kidney Dis. 2004;44:1000–1007. doi: 10.1053/j.ajkd.2004.08.022. [DOI] [PubMed] [Google Scholar]
- Kellum JA, Angus DC, Johnson JP, et al. Continuous versus intermittent renal replacement therapy: a meta-analysis. Intens Care Med. 2002;28:29–37. doi: 10.1007/s00134-001-1159-4. [DOI] [PubMed] [Google Scholar]
- Tonelli M, Manns B, Feller-Kopman D. Acute renal failure in the intensive care unit: a systematic review of the impact of dialytic modality on mortality and renal recovery. Am J Kidney Dis. 2002;40:875–85. doi: 10.1053/ajkd.2002.36318. [DOI] [PubMed] [Google Scholar]
- The Acute Respiratory Distress Syndrome Network Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- Eichacker PQ, Gerstenberger EP, Banks SM, Cui X, Natanson C. Meta-analysis of acute lung injury and acute respiratory distress syndrome trials testing low tidal volumes. Am J Respir Crit Care Med. 2002;16:1510–14. doi: 10.1164/rccm.200208-956OC. [DOI] [PubMed] [Google Scholar]