Abstract
Coronary artery bypass grafting has been performed predominantly with the use of cardiopulmonary bypass and cardioplegic arrest, which allows optimization of the surgical field and consistent placement of grafts. However, the use of cardiopulmonary bypass is also associated with numerous complications. A surgical technique avoiding cardiopulmonary bypass should, in theory, reduce the incidence of such complications and lead to improved patient outcomes. This assumption has rekindled interest in performing off-pump coronary artery bypass surgery, which is currently the focus of scientific scrutiny. The existing world medical literature contains a staggering amount of research related to this technique. Although the available evidence from a large number of randomized clinical trials, nonrandomized clinical trials, propensity-matched analyses, and experimental data suggests that outcomes are better after off-pump than after on-pump coronary artery bypass surgery, skepticism still exists about the safety and efficacy of the off-pump technique. In the present era of evidence-based medicine, results from randomized clinical trials are given the highest recognition. This review attempts to evaluate the best currently available evidence from clinical trials about the safety and efficacy of off-pump coronary artery bypass surgery.
Key words: Coronary artery bypass, coronary artery bypass, off-pump, randomized controlledtrials/methods/mortality/statistics & numerical data/trends
Conventional coronary artery bypass grafting (CABG) using cardiopulmonary bypass (CPB) and cardioplegic arrest has for many years represented the gold standard of coronary revascularization.1 However, the price of a still and bloodless field is ultimately paid by the patient in the form of negative sequelae of CPB, including blood trauma, activation of a series of inflammatory responses, nonpulsatile flow, and possible embolization of air or débris—most particularly embolization of atherosclerotic débris from the aorta.2 The objective of avoiding these deleterious effects of CPB led to the rediscovery of off-pump coronary artery bypass (OPCAB) surgery. Interestingly, since its rediscovery in the late 1990s, OPCAB has been in search of an identity.2 At present, abundant evidence suggests that excellent results can be achieved when cardiopulmonary bypass is avoided.3 However, for nearly a decade, skeptics have regarded OPCAB as a technique associated with intraoperative myocardial ischemia, suboptimal anastomoses, and a protracted learning curve.3
In the current era of evidence-based medicine, the best strategy for countering skepticism and validating the safety and efficacy of a therapeutic method is to analyze the best available evidence.4 Results from double-blind, randomized controlled trials (RCTs) are seen as most persuasive and are regarded as the best approach to ascertain the value of a particular therapy.5 This review article evaluates the best currently available evidence from RCTs in an attempt to validate the safety and efficacy of OPCAB.
Search Methodology
MEDLINE, EMBASE, Cochrane Controlled Trials Register (CCTR), Cochrane Database of Systematic Reviews (CDSR), Database of Abstracts of Reviews of Effects (DARE), Science Citation Index (SCI), Current Contents, NHS Economic Evaluation Database (NEED), and International Network of Agencies for Health Technology Assessment (INAHTA) databases were searched from the date of their inception to the end of December 2004, using the search terms off-pump, minimally invasive, beating heart, coronary artery bypass, and their variants. The search was undertaken in accordance with Cochrane Collaboration recommendations6 and was aimed at finding all published reports of randomized trials comparing OPCAB with conventional CABG. Articles written in English and in languages other than English were included. Tangential electronic exploration of related articles and hand searches of bibliographies, scientific meeting abstracts, and related journals were also performed.
Inclusion Criteria
All blinded or unblinded RCTs, whether comparing OPCAB or minimally invasive direct coronary artery bypass (MIDCAB) on the beating heart with conventional CABG using CPB and cardioplegia, were included if the trial recruited adult patients undergoing single- or multiple-vessel bypass and reported at least 1 pertinent clinical or economic outcome. Studies evaluating the outcomes of hybrid procedures (that is, OPCAB plus balloon angioplasty) and those studies using robotically assisted surgery or circulatory assist devices were excluded.
Data Extraction and Validation of the Studies
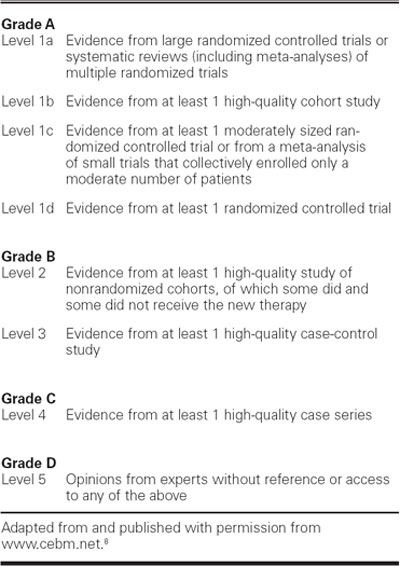
The published reports found by the search strategy were then evaluated. Each paper was subjected to a structured analysis using critical appraisal checklists.7 Such checklists are widely available in several formats and are helpful in assessing the methodological and analytical soundness of a trial and in uncovering any serious methodological flaws.7 The following information was extracted from each published report: 1st author, year of publication, characteristics of the study population, inclusion and exclusion criteria, number of patients who underwent surgery with each technique, and key outcomes. Finally, for each outcome or aspect of OPCAB evaluated, a conclusion was formulated on the basis of the validity of the studies identified, taking into consideration the source and the strength of the evidence by using the grading system proposed by the Oxford Centre for Evidence-Based Medicine (Table I).8
TABLE I. Grading of Recommendations and Levels of Evidence
Results
Of a total of 3,237 citations screened, 67 published reports of RCTs9–73 that fulfilled the inclusion criteria were retrieved for evaluation. One report35 pooled the analyses of 2 trials. Only the trial by Carrier and colleagues29 recruited high-risk patients; most of the other RCTs excluded high-risk patients. Evidence from these RCTs was evaluated to determine the impact of OPCAB on 12 outcomes: systemic inflammation, blood loss and blood transfusion requirements, acute renal failure, myocardial dysfunction, atrial fibrillation, cerebral dysfunction, pulmonary dysfunction, gastrointestinal complications, length of hospital stay, mortality, cost, graft patency, and quality of life.
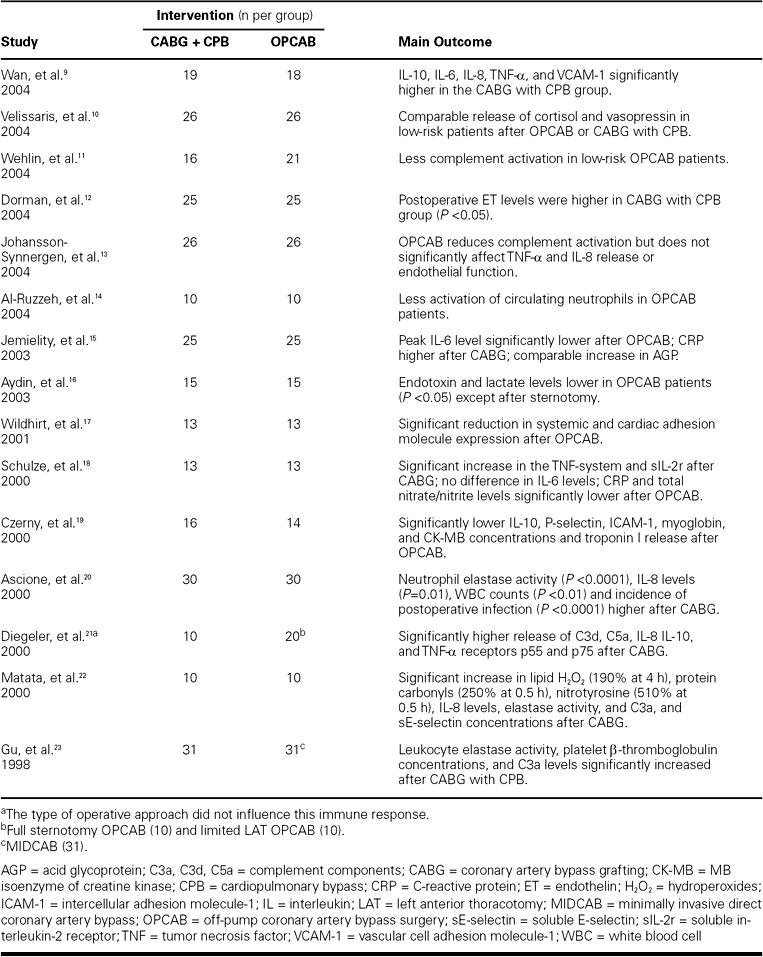
Systemic Inflammation
Cardiopulmonary bypass is associated with an intense inflammatory response because of conversion to laminar flow, blood contact with the artificial bypass surface, cold cardiac ischemia, and hypothermia.74 This inflammatory response, which is characterized by the activation of 5 plasma protein systems and 5 types of blood cells, results in the production of an acute, massive defense reaction that produces a consumptive coagulopathy; circulates more than 70 hormones, cytokines, chemokines, vasoactive substances, cytotoxins, reactive oxygen species, and proteases of the coagulation and fibrinolytic systems; induces mild-to-huge interstitial fluid shifts; generates a host of microemboli (<500 μm); and causes temporary dysfunction of nearly every organ.75
Evidence from a large number of RCTs suggests that, despite comparable surgical trauma, the systemic inflammatory response produced by OPCAB and its associated sequelae are much less severe than those produced by conventional CABG using CPB (Table II). The beneficial effect of OPCAB in blunting this systemic inflammatory response may be attributed to the omission of CPB and the avoidance of global myocardial ischemia.22
TABLE II. Impact of OPCAB on Systemic Inflammatory Response
Blood Loss and Transfusion Requirements
Excessive bleeding is an important cause of morbidity and mortality after CPB.76 Bleeding after cardiac surgery has several causes.77,78 The exposure of blood to synthetic, nonendothelial surfaces causes severe hemostatic defects that inhibit or alter many components of the thrombotic and fibrinolytic systems.79 Because of the associated decrease in hemostatic function and the resultant blood loss, patients undergoing CPB are often given allogeneic blood transfusions.80 Transfusion of allogeneic blood products exposes the patient to additional risks (transfusion reactions, viral transmission, immunosuppression, and increased mortality rates) and increases the cost of the procedure.79 As many as 3% to 5% of patients require surgical re-exploration of the mediastinum because of postoperative hemorrhage.79 Morbidity and mortality rates and hospital costs increase substantially when such re-exploration is necessary.81
A large number of RCTs26–35,62 have shown that OPCAB results in a clinically important decrease in perioperative blood loss. The prospective RCT conducted by Lo and associates24 provided evidence that, compared to OPCAB, the addition of CPB is associated with a substantially more pronounced activation of coagulation and fibrinolysis during the immediate postoperative period. Ascione and coworkers,25 in an RCT specifically designed to investigate the effect of coronary bypass with or without CPB on postoperative blood loss and transfusion requirements, found that the average postoperative blood loss was 1.6 times higher for patients undergoing on-pump CABG than for those undergoing OPCAB. Furthermore, the requirements for fresh frozen plasma and platelets (both P <0.05) and the mean transfusion cost per patient (P <0.01) were significantly lower for the OPCAB patients than for the on-pump patients.25 Avoiding CPB leads to better preservation of hemostasis and less need for allogeneic transfusion.
Acute Renal Failure
Postoperative acute renal failure is a serious complication of CABG and is associated with substantial increases in morbidity and mortality rates.82,83 Depending on the population studied and the definitions used, the reported rates of occurrence of acute renal failure range from 1% to 30%, and the reported risks of death range from 7% to 38%.84 No single mechanism explains the association of renal failure with cardiac surgery; instead, this sequel is caused by a complex interplay of related factors.85 Of these factors, however, renal hypoperfusion and inflammatory damage resulting from CPB are widely regarded as the most important causes of acute renal failure.86,87
To date, 3 small RCTs36–38 have specifically studied the impact of OPCAB on renal function. Loef and associates36 recruited 22 low-risk patients (10 of whom underwent OPCAB and 12, conventional CABG) to an RCT studying the progress and extent of renal damage after bypass surgery. The results showed that OPCAB induced significantly fewer changes in microalbuminuria (P <0.01), free sodium clearance (P <0.05), free water clearance (P <0.01), N-acetyl glucosaminidase activity (P <0.01), and free hemoglobin (P <0.01) than did bypass procedures using CPB. Similar findings were reported by Ascione and coworkers.37 These findings suggested that, for 1st-time coronary bypass patients, OPCAB offers better renal protection than conventional coronary revascularization with CPB and cardioplegic arrest. These findings were contradicted, however, by the results of an RCT conducted by Tang and colleagues,38 who recruited 40 low-risk patients with normal preoperative cardiac and renal function who were awaiting elective CABG. Those researchers found that, although no renal complications or serum markers of kidney dysfunction were present, sensitive indicators detected substantial and similar injury to renal tubules and glomeruli after both conventional CABG and OPCAB. These findings suggest that OPCAB offers no added protection to low-risk individuals against perioperative renal dysfunction; however, the findings may be different for high-risk patients, in whom the avoidance of CPB, thereby eliminating renal hypoperfusion and blunting of the systemic inflammatory response, might prevent progressive renal impairment.88
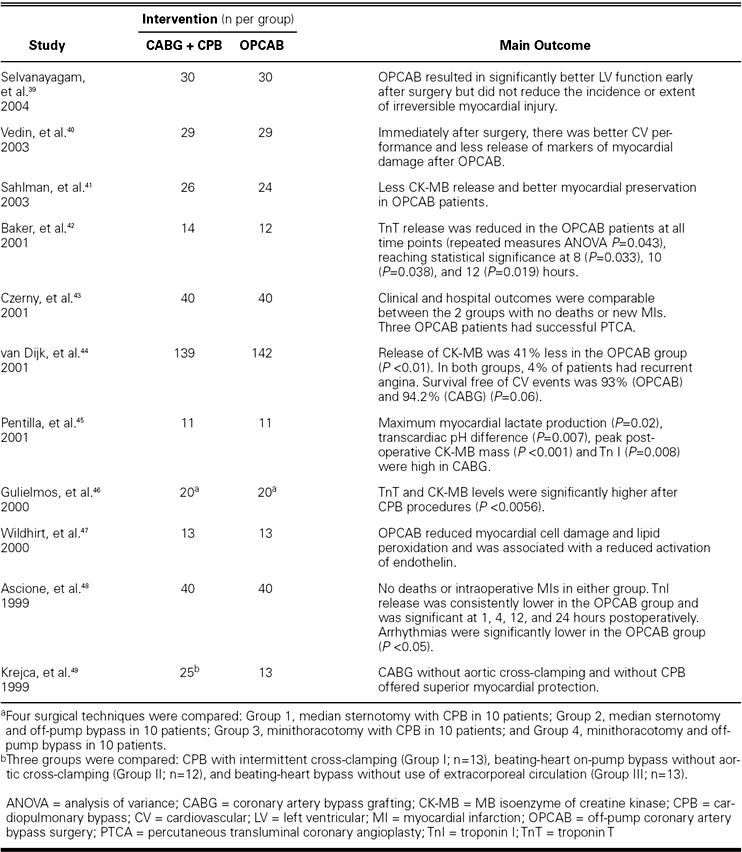
Myocardial Dysfunction
During CPB, before and after cardioplegia or fibrillatory arrest, the heart, like all other organs and tissues, is subject to microemboli, protease and chemical cytotoxins, activated neutrophils and monocytes, and regional hypoperfusion.89 Both myocardial edema and distention of the flaccid cardioplegic heart during aortic cross-clamping reduce myocardial contractility.90 Furthermore, if myocardial contractility is weak, excessive preloading or high afterloading during weaning from CPB increases ventricular end-diastolic volume, myocardial wall stress, and oxygen consumption.89 All of these factors, coupled with reperfusion injury after ischemia, result in postoperative cardiac dysfunction.
Several RCTs (Table III) have found that the incidence of postoperative myocardial infarction is comparable after OPCAB and CABG with CPB but that OPCAB is associated with a more rapid recovery of myocardial oxidative metabolism, better myocardial function, and a lower requirement for inotropic agents. In a recently published study, Selvanayagam and coworkers39 reported the results of an RCT using preoperative and early postoperative contrast-enhanced cardiovascular magnetic resonance imaging (MRI) for the assessment of irreversible myocardial injury and cine MRI for the assessment of global left ventricular function. The results showed that OPCAB is associated with significantly better left ventricular function early after surgery than is CABG with CPB (P = 0.04) but does not reduce the incidence or extent of irreversible myocardial injury. Avoiding aortic cross-clamping and CPB during OPCAB minimizes the risks of global myocardial ischemia and myocardial stunning, as well as the potentially damaging effects of cardioplegia.
TABLE III. Impact of OPCAB on Myocardial Protection
Atrial Fibrillation
Atrial fibrillation (AF), the most common complication of CABG, occurs in 20% to 40% of patients.91 Although the cause of postoperative AF is multifactorial, and the exact pathogenesis of postoperative AF among patients undergoing CABG is still not understood, a large prospective RCT by Ascione and colleagues50 showed that CPB with cardioplegia is the main independent predictor of postoperative AF for patients undergoing coronary revascularization. The “post-pump syndrome” associated with CPB is thought to precipitate AF in patients who have an identifiable electrophysiologic substrate.92
By avoiding the atrial myocyte alterations that result from aortic cross-clamping and avoiding the systemic inflammatory response to CPB, OPCAB should decrease the incidence of postoperative AF. To date, 4 meta-analyses have been performed to evaluate the impact of OPCAB on the incidence of atrial fibrillation,93–96 and all found that the incidence of postoperative AF is substantially lower after OPCAB. It is, however, important to point out that only the meta-analysis by Raja and co-authors93 included solely RCTs. Angelini and colleagues35 performed a pooled analysis of the Beating Heart Against Cardioplegic Arrest Studies (BHACAS 1 and 2) and found that the incidence of AF decreased from 37% to 13% with OPCAB, which was a highly significant finding.
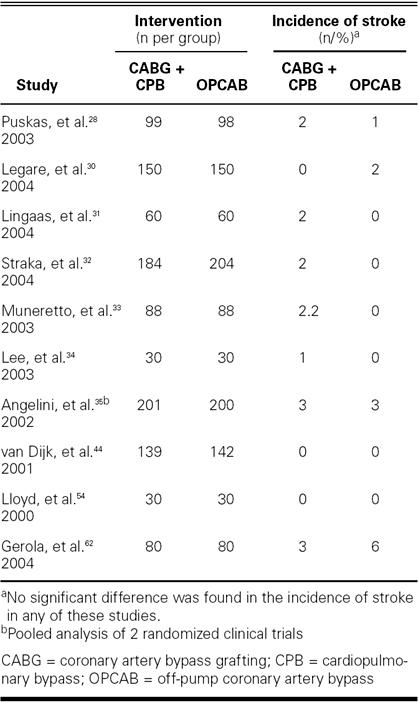
Cerebral Dysfunction
Cerebral injury, an important cause of morbidity and mortality after cardiac surgery, occurs in 2 distinct forms.97 Overt injury, usually a stroke, occurs in 3% of patients undergoing CABG. Injury leading to cognitive impairment, which is detected only by detailed neuropsychologic testing, occurs in as many as 80% of patients soon after surgery and persists in one fourth of these patients 6 months after surgery.97–99 Early postoperative cognitive impairment correlates with a later progression of cognitive decline and impaired quality of life.100 Although the pathogenesis of cerebral injury and cognitive dysfunction after cardiac surgery is multifactorial, there is increasing evidence that multiple microemboli arising from the ascending aorta, the heart chambers, or the bypass circuit are the primary pathophysiologic mechanisms producing diffuse ischemic cerebral injury.101
One can hypothesize that results should be improved by eliminating the source of gaseous and particulate emboli, namely the extracorporeal circuit. In fact, cerebral microembolization is markedly reduced when CPB is avoided.51,102,103 However, reducing cerebral microembolization by avoiding CPB has not resulted in a statistically significant reduction in the incidence of stroke and postoperative neurocognitive dysfunction (Table IV). Available evidence from the RCTs does not unequivocally show that OPCAB is better than conventional CABG with respect to occurrence of stroke and postoperative neurocognitive dysfunction,26,28–35,44,52,54,56,58,59,62 although OPCAB substantially reduces the release of s100 protein and neuron-specific enolase (NSE).53–55,57 The comparable incidence of postoperative stroke after OPCAB may be attributable to aortic manipulation related to the use of a side-biting clamp that is applied during the construction of the proximal anastomoses.104 The adoption of the aortic “no touch” technique, which avoids intraoperative atheromatous embolization from the atherosclerotic aorta into the cerebral circulation, may improve neurologic outcomes after OPCAB.105
TABLE IV. Impact of OPCAB on Incidence of Stroke
Pulmonary Dysfunction
Postoperative pulmonary dysfunction is an important cause of morbidity after surgery with CPB.106 Although severe postoperative acute respiratory distress syndrome is now rare, substantial impairment of pulmonary function does occur and leads to derangements of gas exchange and prolonged extubation times.107
The occurrence of pulmonary impairment after cardiac surgery is believed to be multifactorial. Some of the contributors to the development of lung dysfunction include atelectasis, increased intrapulmonary shunting, and alterations in lung and chest wall mechanics.108 Surgical factors secondary to sternotomy, pleurotomy, and harvesting of the internal mammary artery have also been implicated.107 In addition, it is well accepted that CPB induces an inflammatory response that produces increased pulmonary endothelial permeability, parenchymal damage, and changes in the composition of alveolar surfactant.109,110
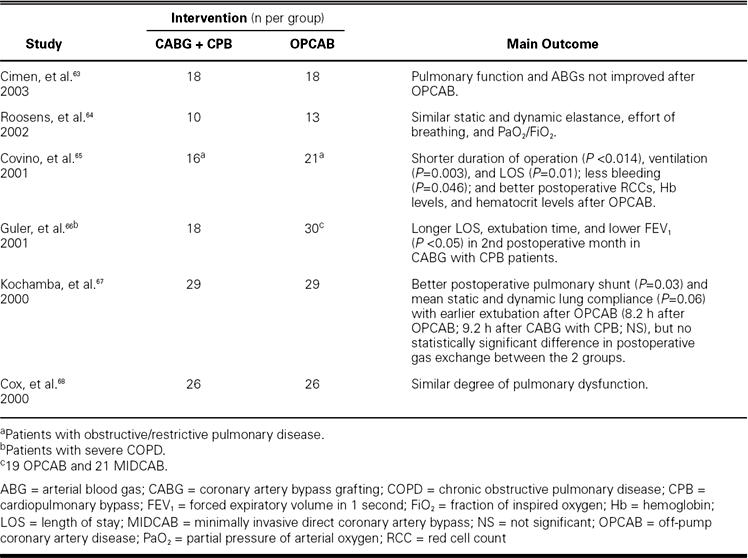
It can be hypothesized that avoiding CPB should lead to less postoperative pulmonary dysfunction, because the CPB-induced systemic inflammatory response will be absent. However, the results of several RCTs (Table V) have produced conflicting evidence in this regard. Most RCTs that have recruited low-risk patients have shown that OPCAB definitely reduces the duration of ventilation and allows earlier extubation of OPCAB patients, yet its effects on respiratory mechanics, oxygenation, and effort of breathing are similar to those in patients undergoing CABG with CPB. On the other hand, the benefits of OPCAB are more pronounced in patients with preexisting pulmonary disease. In these patients, adverse effects on the alveolar stability by activation of the complement cascade, sequestration of the neutrophil in the pulmonary microvascular bed, release of oxygen-derived free radicals, and changes in the composition of alveolar surfactant are not seen, because CPB is avoided.65,66
TABLE V. Impact of OPCAB on Postoperative Pulmonary Dysfunction
Gastrointestinal Complications
Gastrointestinal (GI) complications occur in approximately 2.5% of patients undergoing cardiac surgery, are associated with a high mortality rate (about 33%), and account for approximately 15% of all postoperative deaths.111 Most of the GI complications that occur after CABG have been attributed to low cardiac output and visceral hypoperfusion, which result in mucosal ischemia and necrosis. Cardiopulmonary bypass reduces mucosal blood flow, leads to mesenteric sequestration of neutrophils, and stimulates the systemic inflammatory response.112 Severe intestinal mucosal ischemia can occur during CPB even when the indices of global perfusion remain normal. Factors released during CPB, such as vasopressin, catecholamines, and thromboxane A2 and B2, lead to redistribution of blood flow away from the mucosa because of regional vasoconstriction, and may contribute to mucosal ischemia.113
Velissaris and colleagues69 recruited low-risk patients for an RCT evaluating global oxygen flux and gastric mucosal oxygenation during CABG with and without CPB. Their findings suggested that both procedures are associated with a similar degree of gastric mucosal hypoxia but that the postoperative trends are worse for patients who undergo OPCAB. However, their study did not investigate whether these find-ings relate to the incidence of GI complications after OPCAB or after surgery with CPB; nor did the researchers evaluate whether these findings are applicable to high-risk patients.
To date, only 1 RCT has specifically investigated the incidence of GI complications in similar cohorts of patients: 150 patients (115 men; mean age, 64; range, 45–75 years) undergoing CABG with CPB and cardioplegia, and 150 patients (114 men; mean age, 64; range, 38–66 years) undergoing OPCAB.70 None of the 300 patients had previously undergone abdominal surgery. The overall incidence of GI complications was 4% (11 patients in the on-pump group and 1 patient in the OPCAB group; P <0.0001). Nine (6%) patients in the on-pump group and none in the OPCAB group died. The on-pump patients who experienced GI complications had undergone significantly prolonged periods of both CPB (192.4 ± 83.2 min for patients with GI complications and 112.1 ± 49.6 minutes for patients with no such complications; P <0.0001) and aortic cross clamping (105.3 ± 45.6 min for patients with GI complications and 68.2 ± 35.6 min for patients with no such complications; P <0.0001). The lower incidence of GI complications associated with OPCAB may have occurred because this procedure avoids nonocclusive mesenteric ischemia due to a low cardiac output state or long pump duration, coupled with a reduced systemic inflammatory response.
Length of Hospital Stay and Mortality Rates
The length of hospital stay and the incidence of death after CABG is a function of multiple variables primarily related to a patient's premorbid condition and the morbidity associated with the procedure. Three large meta-analyses96,114,115 have reported that the mortality rate after OPCAB is comparable with that seen after CABG and CPB but that the duration of hospital stay is substantially reduced in patients who undergo OPCAB. Two of these meta-analyses114,115 pooled the results of RCTs only. Similar results were later found by several RCTs.30,32,62,73 By reducing the morbidity rates associated with the procedure and decreasing the incidence of complications, the use of OPCAB has decreased the length of hospital stay.
Cost Savings
The current emphasis on cost containment in health care has stimulated interest in the economics of surgical procedures. Resource utilization is an even more important issue when a new technology is introduced. To date, 5 RCTs have compared the economic outcomes of OPCAB with those of conventional CABG and CPB.32,34,61,71,73 All of these trials have found that OPCAB is less expensive than conventional CABG because of lower complication rates, shorter intubation times, and shorter stays in the ICU and hospital for OPCAB patients.
Graft Patency and Quality of Anastomosis
Reliable graft patency has been the foundation of surgical therapy for coronary artery disease. The goal of off-pump bypass grafting is to minimize procedural complications and patient trauma without compromising the outcomes traditionally achieved by surgical revascularization. One of the main concerns about OPCAB is that performing vascular anastomoses on the small arteries of a beating heart compromises graft patency and results in incomplete myocardial revascularization.3 Four RCTs have evaluated graft patency after OPCAB.27,31,61,73 The 3 larger trials31,61,73 showed no significant differences in patency at various time points. Khan and associates27 found decreased patency 3 months after OPCAB and thus revived the debate about the impact of OPCAB on early and long-term graft patency. However, a closer analysis of this study27 shows that the limited experience of the surgeons, coupled with the intraoperative administration of a relatively low dose of heparin, the absence of aggressive postoperative antiplatelet therapy with clopidogrel, and the failure to use new suction devices to optimize exposure, may have confounded the analyses of graft patency among patients who underwent off-pump procedures.116,117 Furthermore, the design of the study by Khan's group27 did not confer sufficient statistical power to detect differences in graft patency. The study can also be criticized for the nature of its statistical analysis, which appears to be post hoc and parsimonious.1
Quality of Life
Measures of quality of life (QOL) reveal the patient's perception of the burden of disease.118 Because patients are interested not only in survival and relief of angina but also in the resumption of their daily activities, a comprehensive assessment of these aspects of QOL is important. A number of studies have reported improvements in both the physical and mental functional health status of patients after coronary revascularization.119–121 Four RCTs60,61,72,73 have compared patients' reports of QOL after OPCAB and after conventional CABG. Puskas and colleagues73 administered questionnaires to patients, both the EuroQOL-6 and the Short Form-36, 30 days and 1 year postoperatively. That group found that the patients' perception of their QOL improved similarly in the OPCAB group and in the conventional CABG group over time. Van Dijk and coworkers60 and Nathoe and associates61 administered the EuroQOL questionnaire (original version) at baseline and at 1, 3, 6, and 12 months postoperatively and found similar perceived improvements in QOL between the 2 groups over time. In their reports of the Beating Heart Against Cardioplegic Arrest Studies 1 and 2, Ascione and co-authors72 stated that the scores of both groups of patients, calculated from the EuroQOL-5 and Short Form-36 at a median follow-up of 3 years, were very similar and did not differ significantly in any of the dimensions evaluated.
Conclusion
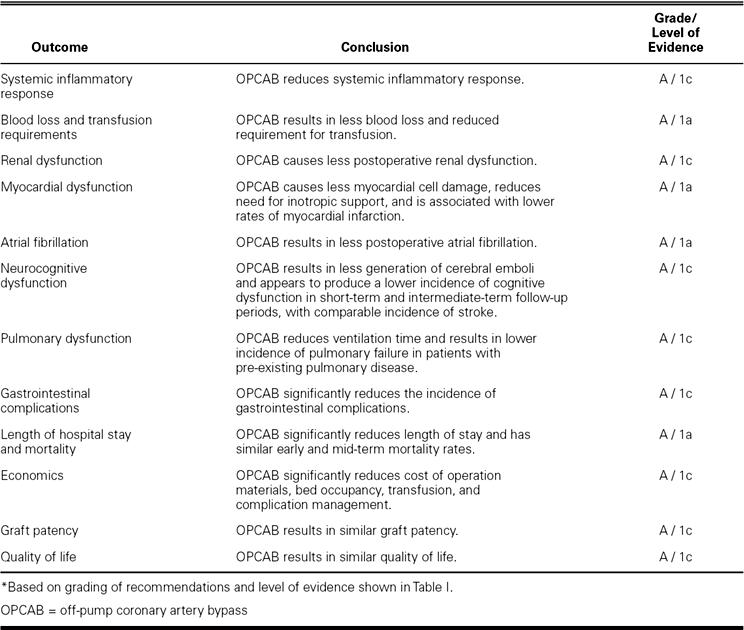
There has been a resurgence of interest in OPCAB during the last decade, and the advantages associated with the use of this technique have been repeatedly emphasized. However, controversies and skepticism still exist concerning the benefits of OPCAB in comparison to those of conventional CABG. An analysis of the best available existing evidence from RCTs clearly suggests that, compared to conventional CABG, OPCAB is associated with lower morbidity rates, similar graft patency, and substantially lower costs (Table VI). In the current era of evidence-based medicine, the rapid acceleration of catheter-based procedures and closer scrutiny of the morbidity associated with CPB appear to threaten the future of coronary artery surgery. The future of such procedures is extremely dependent on surgeons' ability to adapt quickly to change and innovation. Because the safety and efficacy of OPCAB have now been validated, the time has come for its universal adoption as a primary technique for surgical myocardial revascularization.
TABLE VI. Grading of Available Evidence on Safety and Efficacy of OPCAB*
Footnotes
Address for reprints: Shahzad G. Raja, MRCS, Department of Cardiac Surgery, Royal Hospital for Sick Children, Yorkhill NHS Trust, Dalnair Street, Glasgow G3 8SJ, United Kingdom
E-mail: drrajashahzad@hotmail.com
References
- 1.Murphy GJ, Ascione R, Angelini GD. Coronary artery bypass grafting on the beating heart: surgical revascularization for the next decade? Eur Heart J 2004;25:2077–85. [DOI] [PubMed]
- 2.Raja SG. Off-pump and on-pump coronary artery bypass surgery: time to move on. Chin Med J (Engl) 2004;117:959. [PubMed]
- 3.Raja SG. Safety of off-pump coronary artery surgery: no more skepticism please! Eur J Cardiothorac Surg 2004;26:1229. [DOI] [PubMed]
- 4.Raja SG, Dreyfus GD. Off-pump coronary artery bypass surgery: to do or not to do? Current best available evidence. J Cardiothorac Vasc Anesth 2004;18:486–505. [DOI] [PubMed]
- 5.von Segesser LK. Writing off evidence in evidence-based medicine? Interactive Cardiovasc Thorac Surg 2003;2:403–4. [DOI] [PubMed]
- 6.Alderson P, Green S, Higgins JP, editors. Locating and selecting studies for reviews. Cochrane Reviewers' Handbook 4.2.2. [updated March 2004]; Section 5.www.cochraneeyes.org/documents/handbook.pdf. Accessed December 15, 2004. [Now Cochrane Handbook for Systematic Reviews of Interventions]
- 7.Mackway-Jones K, Carley CD, Morton RJ. Best BETs critical appraisal worksheets. Available at http://www.bestbets.org/cgi-bin/public_pdf.pl. Accessed December 17, 2004.
- 8.CEBM. Oxford Centre for Evidence-Based Medicine. Available at www.cebm.net/levels_of_evidence.asp. Accessed December 17, 2004.
- 9.Wan IY, Arifi AA, Wan S, Yip JH, Sihoe AD, Thung KH, et al. Beating heart revascularization with or without cardiopulmonary bypass: evaluation of inflammatory response in a prospective randomized study. J Thorac Cardiovasc Surg 2004;127:1624–31. [DOI] [PubMed]
- 10.Velissaris T, Tang AT, Murray M, Mehta RL, Wood PJ, Hett DA, Ohri SK. A prospective randomized study to evaluate stress response during beating-heart and conventional coronary revascularization. Ann Thorac Surg 2004;78:506–12. [DOI] [PubMed]
- 11.Wehlin L, Vedin J, Vaage J, Lundahl J. Activation of complement and leukocyte receptors during on- and off pump coronary artery bypass surgery. Eur J Cardiothorac Surg 2004;25:35–42. [DOI] [PubMed]
- 12.Dorman BH, Kratz JM, Multani MM, Baron R, Farrar E, Walton S, et al. A prospective, randomized study of endothelin and postoperative recovery in off-pump versus conventional coronary artery bypass surgery. J Cardiothorac Vasc Anesth 2004;18:25–9. [DOI] [PubMed]
- 13.Johansson-Synnergren M, Nilsson F, Bengtsson A, Jeppsson A, Wiklund L. Off-pump CABG reduces complement activation but does not significantly affect peripheral endothelial function: a prospective randomized study. Scand Cardiovasc J 2004;38:53–8. [DOI] [PubMed]
- 14.Al-Ruzzeh S, Hoare G, Marczin N, Asimakopoulos G, George S, Taylor K, Amrani M. Off-pump coronary artery bypass surgery is associated with reduced neutrophil activation as measured by the expression of CD11b: a prospective randomized study. Heart Surg Forum 2003;6:89–93. [DOI] [PubMed]
- 15.Jemielity MM, Perek B, Buczkowski P, Lesniewska K, Wiktorowicz K, Dyszkiewicz W. Inflammatory response following off-pump and on-pump coronary artery bypass grafting. Heart Surg Forum 2003;6(Suppl 1):S40–1.
- 16.Aydin NB, Gercekoglu H, Aksu B, Ozkul V, Sener T, Kiygil I, et al. Endotoxemia in coronary artery bypass surgery: a comparison of the off-pump technique and conventional cardiopulmonary bypass. J Thorac Cardiovasc Surg 2003; 125:843–8. [DOI] [PubMed]
- 17.Wildhirt SM, Schulze C, Schulz C, Egi K, Brenner P, Mair H, et al. Reduction of systemic and cardiac adhesion molecule expression after off-pump versus conventional coronary artery bypass grafting. Shock 2001;16 Suppl 1:55–9. [DOI] [PubMed]
- 18.Schulze C, Conrad N, Schutz A, Egi K, Reichenspurner H, Reichart B, Wildhirt SM. Reduced expression of systemic proinflammatory cytokines after off-pump versus conventional coronary artery bypass grafting. Thorac Cardiovasc Surg 2000;48:364–9. [DOI] [PubMed]
- 19.Czerny M, Baumer H, Kilo J, Lassnigg A, Hamwi A, Vukovich T, et al. Inflammatory response and myocardial injury following coronary artery bypass grafting with or without cardiopulmonary bypass. Eur J Cardiothorac Surg 2000;17:737–42. [DOI] [PubMed]
- 20.Ascione R, Lloyd CT, Underwood MJ, Lotto AA, Pitsis AA, Angelini GD. Inflammatory response after coronary revascularization with or without cardiopulmonary bypass. Ann Thorac Surg 2000;69:1198–204. [DOI] [PubMed]
- 21.Diegeler A, Doll N, Rauch T, Haberer D, Walther T, Falk V, et al. Humoral immune response during coronary artery bypass grafting: A comparison of limited approach, “off-pump” technique, and conventional cardiopulmonary bypass. Circulation 2000;102(19 Suppl 3):III95–100. [DOI] [PubMed]
- 22.Matata BM, Sosnowski AW, Galinanes M. Off-pump bypass graft operation significantly reduces oxidative stress and inflammation. Ann Thorac Surg 2000;69:785–91. [DOI] [PubMed]
- 23.Gu YJ, Mariani MA, van Oeveren W, Grandjean JG, Boonstra PW. Reduction of the inflammatory response in patients undergoing minimally invasive coronary artery bypass grafting. Ann Thorac Surg 1998;65:420–4. [DOI] [PubMed]
- 24.Lo B, Fijnheer R, Castigliego D, Borst C, Kalkman CJ, Nierich AP. Activation of hemostasis after coronary artery bypass grafting with or without cardiopulmonary bypass. Anesth Analg 2004;99:634–40. [DOI] [PubMed]
- 25.Ascione R, Williams S, Lloyd CT, Sundaramoorthi T, Pitsis AA, Angelini GD. Reduced postoperative blood loss and transfusion requirement after beating-heart coronary operations: a prospective randomized study. J Thorac Cardiovasc Surg 2001;121:689–96. [DOI] [PubMed]
- 26.Vural KM, Tasdemir O, Karagoz H, Emir M, Tarcan O, Bayazit K. Comparison of the early results of coronary artery bypass grafting with and without extracorporeal circulation. Thorac Cardiovasc Surg 1995;43:320–5. [DOI] [PubMed]
- 27.Khan NE, De Souza A, Mister R, Flather M, Clague J, Davies S, et al. A randomized comparison of off-pump and on-pump multivessel coronary-artery bypass surgery. N Engl J Med 2004;350:21–8. [DOI] [PubMed]
- 28.Puskas JD, Williams WH, Duke PG, Staples JR, Glas KE, Marshall JJ, et al. Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: a prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg 2003;125:797–808. [DOI] [PubMed]
- 29.Carrier M, Perrault LP, Jeanmart H, Martineau R, Cartier R, Page P. Randomized trial comparing off-pump to on-pump coronary artery bypass grafting in high-risk patients. Heart Surg Forum 2003;6:E89–92. [PubMed]
- 30.Legare JF, Buth KJ, King S, Wood J, Sullivan JA, Friesen CH, et al. Coronary bypass surgery performed off pump does not result in lower in-hospital morbidity than coronary artery bypass grafting performed on pump. Circulation 2004;109:887–92. [DOI] [PubMed]
- 31.Lingaas PS, Hol PK, Lundblad R, Rein KA, Tonnesen TI, Svennevig JL, et al. Clinical and Angiographic Outcome of Coronary Surgery with and without Cardiopulmonary Bypass: A Prospective Randomized Trial. Heart Surg Forum 2004;7:37–41. [PubMed]
- 32.Straka Z, Widimsky P, Jirasek K, Stros P, Votava J, Vanek T, et al. Off-pump versus on-pump coronary surgery: final results from a prospective randomized study PRAGUE-4. Ann Thorac Surg 2004;77:789–93. [DOI] [PubMed]
- 33.Muneretto C, Bisleri G, Negri A, Manfredi J, Metra M, Nodari S, Dei Cas L. Off-pump coronary artery bypass surgery technique for total arterial myocardial revascularization: a prospective randomized study. Ann Thorac Surg 2003;76:778–83. [DOI] [PubMed]
- 34.Lee JD, Lee SJ, Tsushima WT, Yamauchi H, Lau WT, Popper J, et al. Benefits of off-pump bypass on neurologic and clinical morbidity: a prospective randomized trial. Ann Thorac Surg 2003;76:18–26. [DOI] [PubMed]
- 35.Angelini GD, Taylor FC, Reeves BC, Ascione R. Early and midterm outcome after off-pump and on-pump surgery in Beating Heart Against Cardioplegic Arrest Studies (BHACAS 1 and 2): a pooled analysis of two randomised controlled trials. Lancet 2002;359:1194–9. [DOI] [PubMed]
- 36.Loef BG, Epema AH, Navis G, Ebels T, van Oeveren W, Henning RH. Off-pump coronary revascularization attenuates transient renal damage compared with on-pump coronary revascularization. Chest 2002;121:1190–4. [DOI] [PubMed]
- 37.Ascione R, Lloyd CT, Underwood MJ, Gomes WJ, Angelini GD. On-pump versus off-pump coronary revascularization: evaluation of renal function. Ann Thorac Surg 1999; 68:493–8. [DOI] [PubMed]
- 38.Tang AT, Knott J, Nanson J, Hsu J, Haw MP, Ohri SK. A prospective randomized study to evaluate the renoprotective action of beating heart coronary surgery in low risk patients. Eur J Cardiothorac Surg 2002;22:118–23. [DOI] [PubMed]
- 39.Selvanayagam JB, Petersen SE, Francis JM, Robson MD, Kardos A, Neubauer S, Taggart DP. Effects of off-pump versus on-pump coronary surgery on reversible and irreversible myocardial injury: a randomized trial using cardiovascular magnetic resonance imaging and biochemical markers. Circulation 2004;109:345–50. [DOI] [PubMed]
- 40.Vedin J, Jensen U, Ericsson A, Bitkover C, Samuelsson S, Bredin F, Vaage J. Cardiovascular function during the first 24 hours after off pump coronary artery bypass grafting—a prospective, randomized study. Interactive Cardiovasc Thorac Surg 2003;2:489–94. [DOI] [PubMed]
- 41.Sahlman A, Ahonen J, Nemlander A, Salmenpera M, Eriksson H, Ramo J, Vento A. Myocardial metabolism on off-pump surgery: a randomized study of 50 cases. Scand Cardiovasc J 2003;37:211–5. [DOI] [PubMed]
- 42.Baker RA, Andrew MJ, Ross IK, Knight JL. The Octopus II stabilizing system: biochemical and neuropsychological outcomes in coronary artery bypass surgery. Heart Surg Forum 2001;4 Suppl 1:S19–23. [PubMed]
- 43.Czerny M, Baumer H, Kilo J, Zuckermann A, Grubhofer G, Chevtchik O, et al. Complete revascularization in coronary artery bypass grafting with and without cardiopulmonary bypass. Ann Thorac Surg 2001;71:165–9. [DOI] [PubMed]
- 44.van Dijk D, Nierich AP, Jansen EW, Nathoe HM, Suyker WJ, Diephuis JC, et al. Early outcome after off-pump versus on-pump coronary bypass surgery: results from a randomized study. Circulation 2001;104:1761–6. [DOI] [PubMed]
- 45.Penttila HJ, Lepojarvi MV, Kiviluoma KT, Kaukoranta PK, Hassinen IE, Peuhkurinen KJ. Myocardial preservation during coronary surgery with and without cardiopulmonary bypass. Ann Thorac Surg 2001;71:565–71. [DOI] [PubMed]
- 46.Gulielmos V, Menschikowski M, Dill H, Eller M, Thiele S, Tugtekin SM, et al. Interleukin-1, interleukin-6 and myocardial enzyme response after coronary artery bypass grafting - a prospective randomized comparison of the conventional and three minimally invasive surgical techniques. Eur J Cardiothorac Surg 2000;18:594–601. [DOI] [PubMed]
- 47.Wildhirt SM, Schulze C, Conrad N, Sreejayan N, Reichenspurner H, von Ritter C, Reichart B. Reduced myocardial cellular damage and lipid peroxidation in off-pump versus conventional coronary artery bypass grafting. Eur J Med Res 2000;5:222–8. [PubMed]
- 48.Ascione R, Lloyd CT, Gomes WJ, Caputo M, Bryan AJ, Angelini GD. Beating versus arrested heart revascularization: evaluation of myocardial function in a prospective randomized study. Eur J Cardiothorac Surg 1999;15:685–90. [DOI] [PubMed]
- 49.Krejca M, Skiba J, Szmagala P, Gburek T, Bochenek A. Cardiac troponin T release during coronary surgery using intermittent cross-clamp with fibrillation, on-pump and off-pump beating heart. Eur J Cardiothorac Surg 1999;16:337–41. [DOI] [PubMed]
- 50.Ascione R, Caputo M, Calori G, Lloyd CT, Underwood MJ, Angelini GD. Predictors of atrial fibrillation after conventional and beating heart coronary surgery: A prospective, randomized study. Circulation 2000;102:1530–5. [DOI] [PubMed]
- 51.Lund C, Hol PK, Lundblad R, Fosse E, Sundet K, Tennoe B, et al. Comparison of cerebral embolization during off-pump and on-pump coronary artery bypass surgery. Ann Thorac Surg 2003;76:765–70. [DOI] [PubMed]
- 52.Zamvar V, Williams D, Hall J, Payne N, Cann C, Young K, et al. Assessment of neurocognitive impairment after off-pump and on-pump techniques for coronary artery bypass graft surgery: prospective randomised controlled trial. BMJ 2002;325:1268. [DOI] [PMC free article] [PubMed]
- 53.Motallebzadeh R, Kanagasabay R, Bland M, Kaski JC, Jahangiri M. S100 protein and its relation to cerebral microemboli in on-pump and off-pump coronary artery bypass surgery. Eur J Cardiothorac Surg 2004;25:409–14. [DOI] [PubMed]
- 54.Lloyd CT, Ascione R, Underwood MJ, Gardner F, Black A, Angelini GD. Serum S-100 protein release and neuropsychologic outcome during coronary revascularization on the beating heart: a prospective randomized study. J Thorac Cardiovasc Surg 2000;119:148–54. [DOI] [PubMed]
- 55.Zamvar V, Williams D, Hall J, Payne N, Young K, Karthikeyan S, Dunne J. Neurocognitive outcome, s100b and NSE release in coronary artery bypass graft surgery-comparison of the off-pump and on-pump techniques: A randomized controlled study. Heart Surg Forum 2003;6(Suppl 1):S12.
- 56.Gulielmos V, Eller M, Thiele S, Dill HM, Jost T, Tugtekin SM, Schueler S. Influence of median sternotomy on the psychosomatic outcome in coronary artery single-vessel bypass grafting. Eur J Cardiothorac Surg 1999;16 Suppl 2:S34–8. [PubMed]
- 57.Wandschneider W, Thalmann M, Trampitsch E, Ziervogel G, Kobinia G. Off-pump coronary bypass operations significantly reduce S100 release: an indicator for less cerebral damage? Ann Thorac Surg 2000;70:1577–9. [DOI] [PubMed]
- 58.Diegeler A, Hirsch R, Schneider F, Schilling LO, Falk V, Rauch T, Mohr FW. Neuromonitoring and neurocognitive outcome in off-pump versus conventional coronary bypass operation. Ann Thorac Surg 2000;69:1162–6. [DOI] [PubMed]
- 59.Van Dijk D, Jansen EW, Hijman R, Nierich AP, Diephuis JC, Moons KG, et al. Cognitive outcome after off-pump and on-pump coronary artery bypass graft surgery: a randomized trial. JAMA 2002;287:1405–12. [DOI] [PubMed]
- 60.van Dijk D, Moons KG, Keizer AM, Jansen EW, Hijman R, Diephuis JC, et al. Association between early and three month cognitive outcome after off-pump and on-pump coronary bypass surgery. Heart 2004;90:431–4. [DOI] [PMC free article] [PubMed]
- 61.Nathoe HM, van Dijk D, Jansen EW, Suyker WJ, Diephuis JC, van Boven WJ, et al. A comparison of on-pump and off-pump coronary bypass surgery in low-risk patients. N Engl J Med 2003;348:394–402. [DOI] [PubMed]
- 62.Gerola LR, Buffolo E, Jasbik W, Botelho B, Bosco J, Brasil LA, Branco JN. Off-pump versus on-pump myocardial revascularization in low-risk patients with one or two vessel disease: perioperative results in a multicenter randomized controlled trial. Ann Thorac Surg 2004;77:569–73. [DOI] [PubMed]
- 63.Cimen S, Ozkul V, Ketenci B, Yurtseven N, Gunay R, Ketenci B, et al. Daily comparison of respiratory functions between on-pump and off-pump patients undergoing CABG. Eur J Cardiothorac Surg 2003;23:589–94. [DOI] [PubMed]
- 64.Roosens C, Heerman J, De Somer F, Caes F, Van Belleghem Y, Poelaert JI. Effects of off-pump coronary surgery on the mechanics of the respiratory system, lung, and chest wall: Comparison with extracorporeal circulation. Crit Care Med 2002;30:2430–7. [DOI] [PubMed]
- 65.Covino E, Santise G, Di Lello F, De Amicis V, Bonifazi R, Bellino I, Spampinato N. Surgical myocardial revascularization (CABG) in patients with pulmonary disease: beating heart versus cardiopulmonary bypass. J Cardiovasc Surg (Torino) 2001;42:23–6. [PubMed]
- 66.Guler M, Kirali K, Toker ME, Bozbuga N, Omeroglu SN, Akinci E, Yakut C. Different CABG methods in patients with chronic obstructive pulmonary disease. Ann Thorac Surg 2001;71:152–7. [DOI] [PubMed]
- 67.Kochamba GS, Yun KL, Pfeffer TA, Sintek CF, Khonsari S. Pulmonary abnormalities after coronary arterial bypass grafting operation: cardiopulmonary bypass versus mechanical stabilization. Ann Thorac Surg 2000;69:1466–70. [DOI] [PubMed]
- 68.Cox CM, Ascione R, Cohen AM, Davies IM, Ryder IG, Angelini GD. Effect of cardiopulmonary bypass on pulmonary gas exchange: a prospective randomized study. Ann Thorac Surg 2000;69:140–5. [DOI] [PubMed]
- 69.Velissaris T, Tang A, Murray M, El-Minshawy A, Hett D, Ohri S. A prospective randomized study to evaluate splanchnic hypoxia during beating-heart and conventional coronary revascularization. Eur J Cardiothorac Surg 2003;23:917–24. [DOI] [PubMed]
- 70.Raja SG, Haider Z, Ahmad M. Predictors of gastrointestinal complications after conventional and beating heart coronary surgery. Surgeon 2003;1:221–8. [DOI] [PubMed]
- 71.Ascione R, Lloyd CT, Underwood MJ, Lotto AA, Pitsis AA, Angelini GD. Economic outcome of off-pump coronary artery bypass surgery: a prospective randomized study. Ann Thorac Surg 1999;68:2237–42. [DOI] [PubMed]
- 72.Ascione R, Reeves BC, Taylor FC, Seehra HK, Angelini GD. Beating heart against cardioplegic arrest studies (BHACAS 1 and 2): quality of life at mid-term follow-up in two randomised controlled trials. Eur Heart J 2004;25:765–70. [DOI] [PubMed]
- 73.Puskas JD, Williams WH, Mahoney EM, Huber PR, Block PC, Duke PG, et al. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA 2004;291:1841–9. [DOI] [PubMed]
- 74.Larmann J, Theilmeier G. Inflammatory response to cardiac surgery: cardiopulmonary bypass versus non-cardiopulmonary bypass surgery. Best Pract Res Clin Anaesthesiol 2004;18:425–38. [DOI] [PubMed]
- 75.Edmunds LH Jr. Advances in the heart-lung machine after John and Mary Gibbon. Ann Thorac Surg 2003;76:S2220–3. [DOI] [PubMed]
- 76.Nuttall GA, Erchul DT, Haight TJ, Ringhofer SN, Miller TL, Oliver WC Jr, et al. A comparison of bleeding and transfusion in patients who undergo coronary artery bypass grafting via sternotomy with and without cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2003;17:447–51. [DOI] [PubMed]
- 77.Casati V, Gerli C, Franco A, Della Valle P, Benussi S, Alfieri O, et al. Activation of coagulation and fibrinolysis during coronary surgery: on-pump versus off-pump techniques. Anesthesiology 2001;95:1103–9. [DOI] [PubMed]
- 78.Bick RL. Hemostasis defects associated with cardiac surgery, prosthetic devices, and other extracorporeal circuits. Semin Thromb Hemost 1985;11:249–80. [DOI] [PubMed]
- 79.Ereth MH, Nuttall GA, Oliver WC Jr, Santrach PJ, Price RD, Schaff HV. Temperature and duration of cardiopulmonary bypass influence transfusion requirements. J Clin Anesth 1998;10:588–92. [DOI] [PubMed]
- 80.Stensrud PE, Nuttall GA, de Castro MA, Abel MD, Ereth MH, Oliver WC Jr, et al. A prospective, randomized study of cardiopulmonary bypass temperature and blood transfusion. Ann Thorac Surg 1999;67:711–5. [DOI] [PubMed]
- 81.Lytle BW, Loop FD, Cosgrove DM, Taylor PC, Goormastic M, Peper W, et al. Fifteen hundred coronary reoperations. Results and determinants of early and late survival. J Thorac Cardiovasc Surg 1987;93:847–59. [PubMed]
- 82.Chertow GM, Lazarus JM, Christiansen CL, Cook EF, Hammermeister KE, Grover F, Daley J. Preoperative renal risk stratification. Circulation 1997;95:878–84. [DOI] [PubMed]
- 83.Conlon PJ, Stafford-Smith M, White WD, Newman MF, King S, Winn MP, Landolfo K. Acute renal failure following cardiac surgery. Nephrol Dial Transplant 1999;14:1158–62. [DOI] [PubMed]
- 84.Stallwood MI, Grayson AD, Mills K, Scawn ND. Acute renal failure in coronary artery bypass surgery: independent effect of cardiopulmonary bypass. Ann Thorac Surg 2004; 77:968–72. [DOI] [PubMed]
- 85.Mangos GJ, Brown MA, Chan WY, Horton D, Trew P, Whitworth JA. Acute renal failure following cardiac surgery: incidence, outcomes and risk factors. Aust N Z J Med 1995;25:284–9. [DOI] [PubMed]
- 86.Leurs PB, Mulder AW, Fiers HA, Hoorntje SJ. Acute renal failure after cardiovascular surgery. Current concepts in pathophysiology, prevention and treatment. Eur Heart J 1989;10 Suppl H:38–42. [DOI] [PubMed]
- 87.Hashimoto K, Miyamoto H, Suzuki K, Horikoshi S, Matsui M, Arai T, Kurosawa H. Evidence of organ damage after cardiopulmonary bypass. The role of elastase and vasoactive mediators. J Thorac Cardiovasc Surg 1992;104:666–73. [PubMed]
- 88.Bucerius J, Gummert JF, Walther T, Schmitt DV, Doll N, Falk V, Mohr FW. On-pump versus off-pump coronary artery bypass grafting: impact on postoperative renal fail-ure requiring renal replacement therapy. Ann Thorac Surg 2004;77:1250–6. [DOI] [PubMed]
- 89.Hammon JW Jr, Edmunds LH Jr. Extracorporeal circulation: organ damage. In: Cohn LH, Edmunds LH Jr, editors. Cardiac surgery in the adult. 2nd ed. New York: McGraw-Hill Medical Pub; 2003. p. 361–88.
- 90.Downing SW, Savage EB, Streicher JS, Bogen DK, Tyson GS, Edmunds LH Jr. The stretched ventricle. Myocardial creep and contractile dysfunction after acute nonischemic ventricular distention. J Thorac Cardiovasc Surg 1992;104:996–1005. [PubMed]
- 91.Zangrillo A, Landoni G, Sparicio D, Benussi S, Aletti G, Pappalardo F, et al. Predictors of atrial fibrillation after off-pump coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 2004;18:704–8. [DOI] [PubMed]
- 92.Archbold RA, Curzen NP. Off-pump coronary artery bypass graft surgery: the incidence of postoperative atrial fibrillation. Heart 2003;89:1134–7. [DOI] [PMC free article] [PubMed]
- 93.Raja SG, Behranwala AA, Dunning J. Does off-pump coronary artery surgery reduce the incidence of postoperative atrial fibrillation? Interactive Cardiovasc Thorac Surg 2004; 3:647–52. [DOI] [PubMed]
- 94.Athanasiou T, Aziz O, Mangoush O, Al-Ruzzeh S, Nair S, Malinovski V, et al. Does off-pump coronary artery bypass reduce the incidence of post-operative atrial fibrillation? A question revisited. Eur J Cardiothorac Surg 2004;26:701–10. [DOI] [PubMed]
- 95.Athanasiou T, Aziz O, Mangoush O, Weerasinghe A, Al-Ruzzeh S, Purkayastha S, et al. Do off-pump techniques reduce the incidence of postoperative atrial fibrillation in elderly patients undergoing coronary artery bypass grafting? Ann Thorac Surg 2004;77:1567–74. [DOI] [PubMed]
- 96.Reston JT, Tregear SJ, Turkelson CM. Meta-analysis of short-term and mid-term outcomes following off-pump coronary artery bypass grafting. Ann Thorac Surg 2003;76:1510–5. [DOI] [PubMed]
- 97.Murkin JM. Attenuation of neurologic injury during cardiac surgery. Ann Thorac Surg 2001;72:S1838–44. [DOI] [PubMed]
- 98.Taggart DP, Westaby S. Neurological and cognitive disorders after coronary artery bypass grafting. Curr Opin Cardiol 2001;16:271–6. [DOI] [PubMed]
- 99.Taggart DP, Browne SM, Halligan PW, Wade DT. Is cardiopulmonary bypass still the cause of cognitive dysfunction after cardiac operations? J Thorac Cardiovasc Surg 1999;118:414–21. [DOI] [PubMed]
- 100.Newman MF, Grocott HP, Mathew JP, White WD, Landolfo K, Reves JG, et al. Report of the substudy assessing the impact of neurocognitive function on quality of life 5 years after cardiac surgery. Stroke 2001;32:2874–81. [DOI] [PubMed]
- 101.Knipp SC, Matatko N, Wilhelm H, Schlamann M, Massoudy P, Forsting M, et al. Evaluation of brain injury after coronary artery bypass grafting. A prospective study using neuropsychological assessment and diffusion-weighted magnetic resonance imaging. Eur J Cardiothorac Surg 2004; 25:791–800. [DOI] [PubMed]
- 102.Abu-Omar Y, Balacumaraswami L, Pigott DW, Matthews PM, Taggart DP. Solid and gaseous cerebral microembolization during off-pump, on-pump, and open cardiac surgery procedures. J Thorac Cardiovasc Surg 2004;127:1759–65. [DOI] [PubMed]
- 103.Bowles BJ, Lee JD, Dang CR, Taoka SN, Johnson EW, Lau EM, Nekomoto K. Coronary artery bypass performed without the use of cardiopulmonary bypass is associated with reduced cerebral microemboli and improved clinical results. Chest 2001;119:25–30. [DOI] [PubMed]
- 104.Kapetanakis EI, Stamou SC, Dullum MK, Hill PC, Haile E, Boyce SW, et al. The impact of aortic manipulation on neurologic outcomes after coronary artery bypass surgery: a risk-adjusted study. Ann Thorac Surg 2004;78:1564–71. [DOI] [PubMed]
- 105.Leacche M, Carrier M, Bouchard D, Pellerin M, Perrault LP, Paga P, et al. Improving neurologic outcome in off-pump surgery: the “no touch” technique. Heart Surg Forum 2003;6:169–75. [PubMed]
- 106.Shenkman Z, Shir Y, Weiss YG, Bleiberg B, Gross D. The effects of cardiac surgery on early and late pulmonary functions. Acta Anaesthesiol Scand 1997;41:1193–9. [DOI] [PubMed]
- 107.Montes FR, Maldonado JD, Paez S, Ariza F. Off-pump versus on-pump coronary artery bypass surgery and postoperative pulmonary dysfunction. J Cardiothorac Vasc Anesth 2004;18:698–703. [DOI] [PubMed]
- 108.Magnusson L, Zemgulis V, Wicky S, Tyden H, Thelin S, Hedenstierna G. Atelectasis is a major cause of hypoxemia and shunt after cardiopulmonary bypass: an experimental study. Anesthesiology 1997;87:1153–63. [DOI] [PubMed]
- 109.Wan S, LeClerc JL, Vincent JL. Inflammatory response to cardiopulmonary bypass: mechanisms involved and possible therapeutic strategies. Chest 1997;112:676–92. [DOI] [PubMed]
- 110.McGowan FX Jr, Ikegami M, del Nido PJ, Motoyama EK, Kurland G, Davis PJ, Siewers RD. Cardiopulmonary bypass significantly reduces surfactant activity in children. J Thorac Cardiovasc Surg 1993;106:968–77. [PubMed]
- 111.Hessel EA 2nd. Abdominal organ injury after cardiac surgery. Semin Cardiothorac Vasc Anesth 2004;8:243–63. [DOI] [PubMed]
- 112.Tofukuji M, Stahl GL, Metais C, Tomita M, Agah A, Bianchi C, et al. Mesenteric dysfunction after cardiopulmonary bypass: role of complement C5a. Ann Thorac Surg 2000; 69:799–807. [DOI] [PubMed]
- 113.Tao W, Zwischenberger JB, Nguyen TT, Vertrees RA, McDaniel LB, Nutt LK, et al. Gut mucosal ischemia during normothermic cardiopulmonary bypass results from blood flow redistribution and increased oxygen demand. J Thorac Cardiovasc Surg 1995;110:819–28. [DOI] [PubMed]
- 114.Parolari A, Alamanni F, Cannata A, Naliato M, Bonati L, Rubini P, et al. Off-pump versus on-pump coronary artery bypass: meta-analysis of currently available randomized trials. Ann Thorac Surg 2003;76:37–40. [DOI] [PubMed]
- 115.van der Heijden GJ, Nathoe HM, Jansen EW, Grobbee DE. Meta-analysis on the effect of off-pump coronary bypass surgery. Eur J Cardiothorac Surg 2004;26:81–4. [DOI] [PubMed]
- 116.deGuzman BJ, Subramaniam MH. Off-pump versus on-pump coronary bypass surgery. N Engl J Med 2004;350:1791–3. [DOI] [PubMed]
- 117.Dewey TM, Magee MJ, Mack MJ. Off-pump versus on-pump coronary bypass surgery. N Engl J Med 2004;350:1791–3. [PubMed]
- 118.Koch CG, Khandwala F, Cywinski JB, Ishwaran H, Estafanous FG, Loop FD, Blackstone EH. Health-related quality of life after coronary artery bypass grafting: a gender analysis using the Duke Activity Status Index. J Thorac Cardiovasc Surg 2004;128:284–95. [DOI] [PubMed]
- 119.Rumsfeld JS, Ho PM, Magid DJ, McCarthy M Jr, Shroyer AL, MaWhinney S, et al. Predictors of health-related quality of life after coronary artery bypass surgery. Ann Thorac Surg 2004;77:1508–13. [DOI] [PubMed]
- 120.Welke KF, Stevens JP, Schults WC, Nelson EC, Beggs VL, Nugent WC. Patient characteristics can predict improvement in functional health after elective coronary artery bypass grafting. Ann Thorac Surg 2003;75:1849–55. [DOI] [PubMed]
- 121.Pocock SJ, Henderson RA, Seed P, Treasure T, Hampton JR. Quality of life, employment status, and anginal symptoms after coronary angioplasty or bypass surgery. 3-year follow-up in the Randomized Intervention Treatment of Angina (RITA) Trial. Circulation 1996;94:135–42. [DOI] [PubMed]


