Abstract
We report the rare subchronic clinical course of a giant, dissecting pulmonary artery aneurysm in an oligosymptomatic middle-aged woman who had idiopathic pulmonary hypertension. Diagnosis was simple with the use of echocardiography and multislice computed tomography. Conversely, deciding on the treatment was difficult, because prominent surgeons declined to perform surgical repair of the aneurysm and recommended heart–lung transplantation. Therefore, we were forced to treat our patient medically. She survived for 1 year, including 8 months of treatment with sildenafil, and then died suddenly while awaiting transplantation.
Our patient, who had a dissecting, high-pressure pulmonary artery aneurysm, had an unexpectedly stable and uneventful clinical course for 1 year, which, under more favorable circumstances, might have provided enough time for heart–lung transplantation to be performed.
Key words: Aneurysm, dissecting/diagnosis/etiology, hypertension, pulmonary/complications/therapy, pulmonary artery/pathology, sildenafil, vasodilator agents/therapeutic use
A dissecting pulmonary artery aneurysm in a patient with severe pulmonary hypertension is very rare, even at referral institutions.1 When such an aneurysm is diagnosed, the treatment strategy is uncertain, because surgery is associated with a high degree of risk, and the experience of many surgeons with such procedures is limited. Pulmonary artery surgery can prevent catastrophic rupture;2 however, the mortality rate associated with such surgery is high, and its benefits are time-limited because of pulmonary hypertension. Heart–lung transplantation may be more beneficial than other treatments, but donor organs are not always available.3
We report herein the course of a patient who had primary pulmonary hypertension and a huge, dissecting pulmonary artery aneurysm. She was treated medically, because surgery to repair the aneurysm was considered too dangerous.
Case Report
Our patient, a 44-year-old woman, was hospitalized for the 1st time at the age of 11 years with the presumptive diagnosis of primary pulmonary hypertension. She underwent heart catheterization at the age of 15, when her pulmonary systolic pressure was found to be 65 mmHg, without intracardiac shunting. We have no record of the pulmonary vascular resistance at that time; however, the pulmonary artery was dilated to a diameter of 5 cm. When the patient was 34 years old, echocardiography showed that the diameter of the pulmonary artery had increased to 7 cm.
By the age of 44, the patient had been virtually oligosymptomatic for years. She had been experiencing fatigue and dyspnea only upon strenuous exercise (New York Heart Association functional class II). However, she was admitted to a regional hospital center with symptoms of respiratory infection and atypical chest pain. Echocardiography and computed tomographic (CT) scanning showed striking dilatation (diameter, 11 cm) of the pulmonary artery, with dissection. The patient's condition improved after successful treatment of the respiratory infection, but she would not consider undergoing any type of surgery. After 4 months, she changed her mind and was referred to our institution.
Upon her arrival in May 2003, the patient was observed to be lean, with long, slim limbs—an appearance that suggested the possibility of Marfan syndrome. However, this diagnosis was not confirmed. She was mildly cyanotic and hypoxemic, with clubbing of the fingers, but lively, without the appearance of illness or signs of heart failure. Physical and electrocardiographic examination indicated the presence of right ventricular and right atrial hypertrophy. Signs of pulmonary and tricuspid regurgitation and of left-sided pleural effusion were also noted.
Echocardiography showed an extremely dilated pulmonary artery, 15 cm in diameter, with a torn intimal flap and a very thin remaining wall (Figs. 1–3). The main branches of the pulmonary artery were also very wide (4–5 cm; Fig. 1). The right side of the heart was enlarged, and moderate pulmonary and tricuspid insufficiency indicated severe pulmonary hypertension. Mild pericardial effusion and some degree of pleural effusion were also detected.
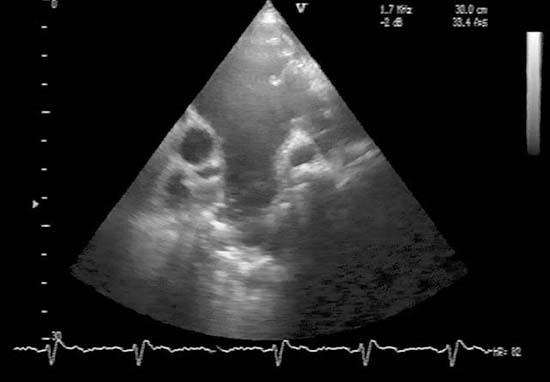
Fig. 1 Cross-sectional echocardiogram through the base of the heart, parasternal short-axis view. A giant pulmonary artery aneurysm (PAA) with a torn intimal flap (IF) is much larger in diameter than the ascending aorta (Ao). The main branches of the pulmonary artery, shown in the lower part of the figure, are also very wide.
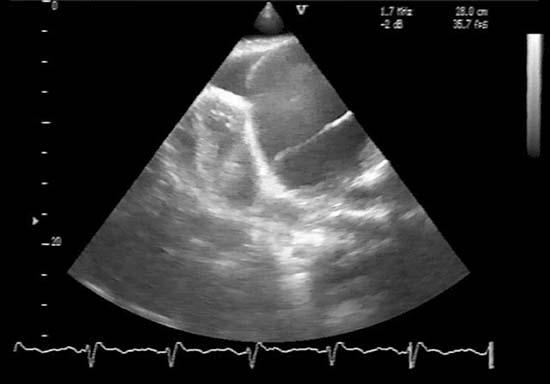
Fig. 2 Cross-sectional echocardiogram from an atypical left low parasternal (almost apical) acoustic window shows a large pulmonary artery aneurysm divided into 2 compartments by a torn intimal flap (IF). Color-flow Doppler echocardiography identified a true lumen (TL) and false lumen (FL). The left ventricle (LV) is quite small in comparison with the pulmonary artery aneurysm.
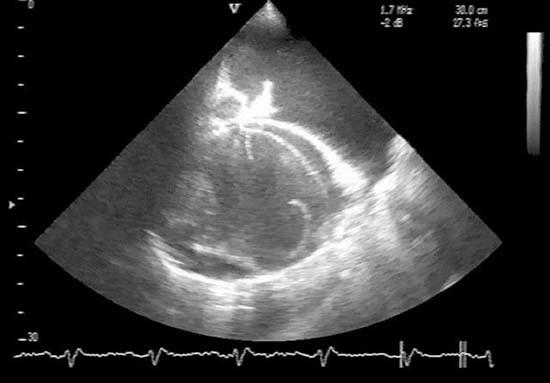
Fig. 3 Echocardiogram from an atypical acoustic window (posterior view) shows the pulmonary artery aneurysm (PAA) through the pleural effusion (PE). Thrombotic mass (Thr) and torn intimal flaps (IF) are clearly visible.
Chest radiography showed right atrial and right ventricular enlargement, and enormous dilatation of the pulmonary artery and its branches. Some left-sided pleural effusion was also visible.
Multislice CT scans confirmed the presence of a dissecting aneurysm (15.7 × 14.2 cm) of the pulmonary artery. The dissection continued into the enormously wide (6 cm) and partially thrombosed left pulmonary artery; the branches to the upper and lower left lobe were also very wide and partially thrombosed. Segmental branches were not only thrombosed but were obliterated. The right pulmonary artery was also very broad (4–5 cm) and was partially thrombosed; its branches to the upper, middle, and lower lobes were dilated but not thrombosed. The right lung was well aerated except for subsegmental atelectasis in the middle lobe, whereas the left lung was compressed by a large pleural effusion. The huge pulmonary artery aneurysm had pushed the entire heart to the right side of the chest cavity (Fig. 4).
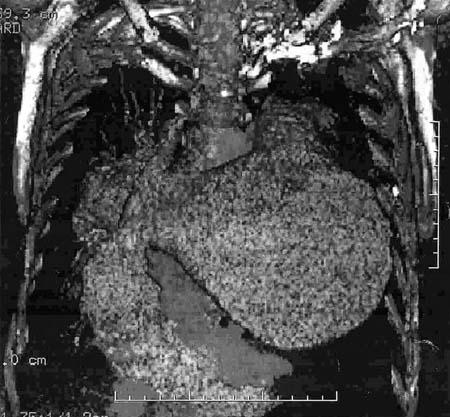
Fig. 4 Multislice computed tomographic scan provides a 3-dimensional reconstruction of a large pulmonary artery aneurysm (PAA) that dominates the thorax and covers the heart.
Digital pulmonary arteriography showed a huge pulmonary artery aneurysm and scant opacification of its branches with contrast dilution.
Catheterization of the right side of the heart demonstrated a systolic pulmonary artery pressure of 80 mmHg; this pressure was not substantially reduced by the infusion of prostaglandin. Pulmonary vascular resistance was not estimated because of the risk of aneurysmal rupture.
This patient's case was presented to several cardiac surgeons, some of whom were world famous. All of them declined to perform surgical correction of the dissecting pulmonary artery aneurysm—despite the possibility of impending rupture—because of the high risk to a patient with severe pulmonary hypertension and because of the poor chance of survival without heart–lung transplantation. The only remaining alternative was conservative treatment of the pulmonary hypertension by pharmacologic vasodilation.
The pulmonary vascular resistance was tested by intravenous injection of iloprost, with findings monitored by pulmonary artery catheter. This test demonstrated that the pulmonary hypertension could not be substantially reversed.
The patient was treated with sildenafil (Viagra®, Pfizer; New York, NY) at a daily dosage that was gradually increased from 75 mg to 150 mg over a period of 8 months. The patient's quality of life improved moderately, although improvements in gas exchange values were barely perceptible. The right ventricular systolic pressure, as estimated by Doppler echocardiography, gradually decreased from 120 mmHg to 97 mmHg. However, this level was still higher than it had been at the time of admission (when these echocardiographic results were compared with those of catheterization on admission). The patient's shuttle-walk test results improved from 200 meters in 4 min 17 sec to 350 meters in 6 min 15 sec.
The patient did quite well for 8 months, continuing treatment with sildenafil. She then died suddenly at home, while watching television. Her family declined an autopsy, because the patient's diagnosis was clearly known.
Discussion
In contrast to aneurysms in the vessels of the system-ic circulation, true pulmonary artery aneurysms are rare.4–9 Only 8 cases were detected in a series of more than 100,000 necropsies reported in 1947.10 Whether such aneurysms are more common among patients of 1 sex than the other has not been ascertained.5 Pulmonary hypertension is an important causative factor and is a predictor of prognosis; therefore, this condition must be considered when clinical decisions are being made.4,5 An aggressive surgical approach has been advocated for patients with pulmonary hypertension because of the risk of impending dissection and rupture of the aneurysm.1,5 For patients with a low-pressure pulmonary artery aneurysm without left-to-right shunting, a more cautious approach may be warranted.4 Other factors leading to aneurysmal dilatation of the pulmonary artery are weakness of its wall (for example, in patients with Marfan syndrome or some other connective-tissue diseases) and hemodynamic load (due to shunting or pulmonary valve abnormality).1,4,5
Since the 1st description by Walshe in 1862,11 only about 50 cases of pulmonary artery dissection have been reported.1,12–25 Almost all of these aneurysms were discovered postmortem; only a few were recognized clinically.1,2,6 Fortunately, the introduction of modern diagnostic imaging methods such as echocardiography,1,16,25 CT scanning,2,7 and magnetic resonance imaging2 have enabled the clinical recognition of pulmonary artery dissection.
According to published reports, pulmonary artery dissection occurs almost exclusively in an artery dilated by an aneurysm rather than in a normal-sized artery.1,5,24 Dissection of a markedly dilated pulmonary artery is a rare and usually fatal complication of chronic pulmonary arterial hypertension.19,24 The dissection may be associated with congenital heart lesions that have led to sustained high pulmonary flow rates and pulmonary hypertension.12–15 To our knowledge, few-er than 10 cases of pulmonary artery dissection have been described in connection with primary pulmonary hypertension.1,5,16,17,22,23 Idiopathic and inflammation-related pulmonary artery dissection among patients without underlying pulmonary hypertension is extremely unusual.24 However, iatrogenic pulmonary artery dissection has been reported as a complication of pulmonary angiography.21
The symptoms of pulmonary artery dissection are nonspecific.1,5 Dyspnea, retrosternal chest pain, cyanosis, hemorrhagic shock, acute pericardial tamponade, and sudden death have been reported.2,25 In our patient, the clinical diagnosis was easy to make because of the results of echocardiographic imaging. Nonetheless, the clinical decision regarding treatment was difficult. Surgical repair seemed almost mandatory because of the exceedingly high risk of rupture of the huge, dissecting, high-pressure pulmonary artery aneurysm. However, the chances of our patient's surviving such an operation were very poor because of her primary pulmonary hypertension. To our knowledge, there had been only 2 previous reports of success-ful pulmonary artery reconstruction of a dissecting pulmonary artery aneurysm.1 The 1st patient had chronic dissection of the pulmonary artery without pulmonary hypertension and underwent arterial reconstruction. The 2nd patient, who was in unstable condition with primary pulmonary hypertension, underwent successful 2-staged surgery (pulmonary artery reconstruction first, followed by lung transplantation).1 Even if our patient had survived the hazards associated with reconstruction of the pulmonary artery and its branches, her length of survival would have been limited by the primary pulmonary hypertension. Therefore, it was not surprising that surgeons declined to perform reconstructive surgery. Because heart–lung transplantation was not feasible, the only remaining possibility was to decrease the risk of impending pulmonary artery rupture by use of pharmacologic vasodilation.
We accepted the previously suggested diagnosis of primary or idiopathic26 pulmonary hypertension, which had been made primarily on the basis of clinical presentation and the absence of any other cause of pulmonary hypertension.26–30 The gradual progression of pulmonary hypertension had been documented since the patient's childhood, although she had been examined with duplex ultrasonography of the pelvic and leg veins and lacked signs and symptoms of venous thrombosis and pulmonary embolism. Lung biopsy seemed to be neither relevant to the treatment strategy nor predictive of vasodilatory response.31,32
The response to sildenafil, albeit positive occasionally in other conditions,33 supported the diagnosis of idiopathic pulmonary hypertension.34–37 The patient's negative vasodilatory response to iloprost versus the positive response to sildenafil is attributable to the different modes of action of the 2 drugs.38,39 The endothelin receptor antagonist bosentan can be combined with both agents,40–45 but its use has been limited because it is expensive. Sildenafil has been reported to improve quality of life and exercise tolerance in patients with primary pulmonary hypertension.35 Both of these factors have become accepted measures of efficacy in the treatment of pulmonary hypertension.46
Our patient's clinical course was quite prolonged and mild, considering her generally bleak prognosis and the short survival times of patients with primary pulmonary hypertension. A full year of reasonable-quality life for a patient with a huge, dissecting, high-pressure pulmonary artery aneurysm was an exceptional and noteworthy outcome. Eventual rupture of the aneurysm was unavoidable without surgical intervention.
The immediate cause of sudden death in this patient could not be ascertained without autopsy but was most likely the rupture of the pulmonary artery aneurysm, an outcome that had long been feared. Other possible causes of death included the formation of an additional thrombus or the dislodgment of pulmonary artery thrombi that further obstructed the pulmonary circulation; however, these causes are less likely to cause sudden death. The same applies to malignant ventricular arrhythmia.
A dissecting pulmonary artery aneurysm in a patient with primary pulmonary hypertension is so rare that no optimal treatment strategy has been established; we relied on the few available case reports and a review of the world medical literature for guidance.1,5,17,22,23
Physicians may conclude that surgery is the only treatment that carries the hope of long-term benefits for patients such as ours.8,15 Pulmonary artery reconstruction and heart–lung transplantation are very demanding and risky in these patients and are performed only at the best centers; however, they are possible.1 We have shown, albeit inadvertently, that a patient with a huge, dissecting, high-pressure pulmonary artery aneurysm can survive for a relatively long time, even without surgery, and that the disease may have a prolonged oligosymptomatic course. A similar patient with a year-long uneventful course has been described previously.17 Such a stable and prolonged course in an oligosymptomatic patient should not be regarded as a mere curiosity that seems to defy the laws of physics, nor should it be considered analogous to the course in patients with aortic dissection. A dissecting pulmonary artery aneurysm in a patient with irreversible pulmonary hypertension is a specific clinical entity with some similarities to the more common aortic dissection but also with important differences.
Immediate and risky surgical reconstruction of the pulmonary artery, followed by lung transplantation at a later opportunity, offers the only chance for survival in patients who have a high-pressure, dissecting pulmonary artery aneurysm and who are in an unstable condition.1 However, a period of stability such as that seen in our patient should be regarded as an opportunity to sustain the patient as he or she awaits transplantation.
Footnotes
Address for reprints: Anton Smalcelj, MD, PhD, FESC, Department for Cardiovascular Diseases, Zagreb University Hospital Centre, Kispaticeva 12, Zagreb 10000, Croatia
E-mail: anton.smalcelj@kbc-zagreb.hr
References
- 1.Senbaklavaci O, Kaneko Y, Bartunek A, Brunner C, Kurkciyan E, Wunderbaldinger P, et al. Rupture and dissection in pulmonary artery aneurysms: incidence, cause, and treatment—review and case report. J Thorac Cardiovasc Surg 2001;121:1006–8. [DOI] [PubMed]
- 2.Song EK, Kolecki P. A case of pulmonary artery dissection diagnosed in the Emergency Department. J Emerg Med 2002;23:155–9. [DOI] [PubMed]
- 3.Klepetko W, Mayer E, Sandoval J, Trulock EP, Vachiery JL, Dartevelle P, et al. Interventional and surgical modalities of treatment for pulmonary arterial hypertension. J Am Coll Cardiol 2004;43(12 Suppl S):73S–80S. [DOI] [PubMed]
- 4.Veldtman GR, Dearani JA, Warnes CA. Low pressure giant pulmonary artery aneurysms in the adult: natural history and management strategies. Heart 2003;89:1067–70. [DOI] [PMC free article] [PubMed]
- 5.Axmann C, Theuerkauf I, Flacke S. Delineated aneurysms of the large pulmonary arteries. A rare sequela of pulmonary hypertension [in German]. Rofo 2002;174:1460–1. [DOI] [PubMed]
- 6.Lopez-Candales A, Kleiger RE, Aleman-Gomez J, Kouchoukos NT, Botney MD. Pulmonary artery aneurysm: review and case report. Clin Cardiol 1995;18:738–40. [DOI] [PubMed]
- 7.Iula G, Ziviello R, Del Vecchio W. Aneurysms of proximal pulmonary arteries: CT diagnosis and preoperative assessment. Eur Radiol 1996;6:730–3. [DOI] [PubMed]
- 8.Kuwaki K, Morishita K, Sato H, Urita R, Abe T. Surgical repair of the pulmonary trunk aneurysm. Eur J Cardiothorac Surg 2000;18:535–9. [DOI] [PubMed]
- 9.Wu WS. Images in cardiovascular medicine. Huge calcified pulmonary arterial aneurysm. Circulation 2003;107:2280–1. [DOI] [PubMed]
- 10.Deterling RA, Clagett OT. Aneurysm of the pulmonary artery: review of the literature and report of a case. Am Heart J 1947;34:471–99. [DOI] [PubMed]
- 11.Shilkin KB, Low LP, Chen BT. Dissecting aneurysm of the pulmonary artery. J Pathol 1969;98:25–9. [DOI] [PubMed]
- 12.Epstein S, Naji AF. Pulmonary artery aneurysm with dissection after Blalock operation for tetralogy of Fallot. Am J Cardiol 1960;5:560–3. [DOI] [PubMed]
- 13.D'Arbela PG, Mugerwa JW, Patel AK, Somers K. Aneurysm of pulmonary artery with persistent ductus arteriosus and pulmonary infundibular stenosis. Fatal dissection and rupture in pregnancy. Br Heart J 1970;32:124–6. [DOI] [PMC free article] [PubMed]
- 14.Placik B, Rodbard S, McMahon J, Swaroop S. Pulmonary artery dissection and rupture in Eisenmenger's syndrome. Vasc Surg 1976;10:72–80. [DOI] [PubMed]
- 15.Hankins GD, Brekken AL, Davis LM. Maternal death secondary to a dissecting aneurysm of the pulmonary artery. Obstet Gynecol 1985;65(3 Suppl):45S–48S. [PubMed]
- 16.Campeanu A, Dragoncea C, Socaciu VI, Ardeleanu M. Pulmonary artery dissection in inexplicable pulmonary arterial hypertension (a case presentation) [in Romanian]. Rev Med Interna Neurol Psihiatr Neurochir Dermatovenerol Med Interna 1985;37:179–86. [PubMed]
- 17.Steurer J, Jenni R, Medici TC, Vollrath T, Hess OM, Siegenthaler W. Dissecting aneurysm of the pulmonary artery with pulmonary hypertension. Am Rev Respir Dis 1990; 142:1219–21. [DOI] [PubMed]
- 18.Walley VM, Virmani R, Silver MD. Pulmonary arterial dissections and ruptures: to be considered in patients with pulmonary arterial hypertension presenting with cardiogenic shock or sudden death. Pathology 1990;22:1–4. [DOI] [PubMed]
- 19.Stern EJ, Graham C, Gamsu G, Golden JA, Higgins CB. Pulmonary artery dissection: MR findings. J Comput Assist Tomogr 1992;16:481–3. [DOI] [PubMed]
- 20.Kameyama T, Nakayama S, Okabayashi H, Nomoto S, Okamoto Y, Ban T. A case report of successful repair of an aortopulmonary fistula with partial dissection of the pulmonary artery [in Japanese]. Nippon Kyobu Geka Gakkai Zasshi 1992;40:432–4. [PubMed]
- 21.van Beek EJ, Kuyer PM, Reekers JA. Dissection of pulmonary artery as a complication of pulmonary angiography. Rofo 1993;158:599–600. [DOI] [PubMed]
- 22.Masuda S, Ishii T, Asuwa N, Ishikawa Y, Kiguchi H, Uchiyama T. Concurrent pulmonary arterial dissection and saccular aneurysm associated with primary pulmonary hypertension. Arch Pathol Lab Med 1996;120:309–12. [PubMed]
- 23.Wunderbaldinger P, Bernhard C, Uffmann M, Kurkciyan I, Senbaklavaci O, Herold CJ. Acute pulmonary trunk dissection in a patient with primary pulmonary hypertension. J Comput Assist Tomogr 2000;24:92–5. [DOI] [PubMed]
- 24.Inayama Y, Nakatani Y, Kitamura H. Pulmonary artery dissection in patients without underlying pulmonary hypertension [published erratum appears in Histopathology 2001; 39:550]. Histopathology 2001;38:435–42. [DOI] [PubMed]
- 25.Areco D, Pizzano N. Pulmonary artery dissection: echocardiographic findings and diagnosis. Echocardiography 2003; 20:375–7. [DOI] [PubMed]
- 26.Simonneau G, Galie N, Rubin LJ, Langleben D, Seeger W, Domenighetti G, et al. Clinical classification of pulmonary hypertension. J Am Coll Cardiol 2004;43(12 Suppl S):5S–12S. [DOI] [PubMed]
- 27.Rich S. Pulmonary hypertension. In: Braunwald E, Zipes DP, Libby P, editors. Heart disease: a textbook of cardiovascular medicine. Vol 1. 6th ed. Philadelphia: WB Saunders; 2001. p. 1908–35.
- 28.British Cardiac Society Guidelines and Medical Practice Committee, and approved by the British Thoracic Society and the British Society of Rheumatology. Recommendations on the management of pulmonary hypertension in clinical practice. Heart 2001;86 Suppl 1:I1–13. [PMC free article] [PubMed]
- 29.Fishman AP. Primary pulmonary arterial hypertension: a look back. J Am Coll Cardiol 2004;43(12 Suppl S):2S–4S. [DOI] [PubMed]
- 30.Barst RJ, McGoon M, Torbicki A, Sitbon O, Krowka MJ, Olschewski H, Gaine S. Diagnosis and differential assessment of pulmonary arterial hypertension. J Am Coll Cardiol 2004;43(12 Suppl S):40S–47S. [DOI] [PubMed]
- 31.Hillis LD, Lange RA, Winniford MD, Page RL. Manual of clinical problems in cardiology: with annotated key references. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2003. p. 509–13.
- 32.Pietra GG, Capron F, Stewart S, Leone O, Humbert M, Robbins IM, et al. Pathologic assessment of vasculopathies in pulmonary hypertension. J Am Coll Cardiol 2004;43(12 Suppl S):25S–32S. [DOI] [PubMed]
- 33.Angel Gomez-Sanchez M, Saenz De La Calzada C, Escribano Subias P, Francisco Delgado Jimenez J, Lazaro Salvador M, Albarran Gonzalez A, Cea Calvo L. Pilot assessment of the response of several pulmonary hemodynamic variables to sublingual sildenafil in candidates for heart transplantation. Eur J Heart Fail 2004;6:615–7. [DOI] [PubMed]
- 34.Leuchte HH, Schwaiblmair M, Baumgartner RA, Neurohr CF, Kolbe T, Behr J. Hemodynamic response to sildenafil, nitric oxide, and iloprost in primary pulmonary hypertension. Chest 2004;125:580–6. [DOI] [PubMed]
- 35.Sastry BK, Narasimhan C, Reddy NK, Raju BS. Clinical efficacy of sildenafil in primary pulmonary hypertension: a randomized, placebo-controlled, double-blind, crossover study. J Am Coll Cardiol 2004;43:1149–53. [DOI] [PubMed]
- 36.Karatza AA, Narang I, Rosenthal M, Bush A, Magee AG. Treatment of primary pulmonary hypertension with oral sildenafil. Respiration 2004;71:192–4. [DOI] [PubMed]
- 37.Nagaya N. Drug therapy of primary pulmonary hypertension. Am J Cardiovasc Drugs 2004;4:75–85. [DOI] [PubMed]
- 38.Badesch DB, McLaughlin VV, Delcroix M, Vizza CD, Olschewski H, Sitbon O, Barst RJ. Prostanoid therapy for pulmonary arterial hypertension. J Am Coll Cardiol 2004; 43(12 Suppl S):56S–61S. [DOI] [PubMed]
- 39.Ghofrani HA, Pepke-Zaba J, Barbera JA, Channick R, Keogh AM, Gomez-Sanchez MA, et al. Nitric oxide pathway and phosphodiesterase inhibitors in pulmonary arterial hypertension. J Am Coll Cardiol 2004;43(12 Suppl S):68S–72S. [DOI] [PubMed]
- 40.Channick RN, Sitbon O, Barst RJ, Manes A, Rubin LJ. Endothelin receptor antagonists in pulmonary arterial hypertension. J Am Coll Cardiol 2004;43(12 Suppl S):62S–57S. [DOI] [PubMed]
- 41.Rubin LJ, Badesch DB, Barst RJ, Galie N, Black CM, Keogh A, et al. Bosentan therapy for pulmonary arterial hypertension [published erratum appears in N Engl J Med 2002;346:1258]. N Engl J Med 2002;346:896–903. [DOI] [PubMed]
- 42.Sitbon O, Badesch DB, Channick RN, Frost A, Robbins IM, Simonneau G, et al. Effects of the dual endothelin receptor antagonist bosentan in patients with pulmonary arterial hypertension: a 1-year follow-up study. Chest 2003; 124:247–54. [DOI] [PubMed]
- 43.O'Callaghan D, Gaine SP. Bosentan: a novel agent for the treatment of pulmonary arterial hypertension. Int J Clin Pract 2004;58:69–73. [DOI] [PubMed]
- 44.Galie N, Seeger W, Naeije R, Simonneau G, Rubin LJ. Comparative analysis of clinical trials and evidence-based treatment algorithm in pulmonary arterial hypertension. J Am Coll Cardiol 2004;43(12 Suppl S):81S–88S. [DOI] [PubMed]
- 45.Channick RN, Simonneau G, Sitbon O, Robbins IM, Frost A, Tapson VF, et al. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomised placebo-controlled study. Lancet 2001; 358:1119–23. [DOI] [PubMed]
- 46.Hoeper MM, Oudiz RJ, Peacock A, Tapson VF, Haworth SG, Frost AE, Torbicki A. End points and clinical trial designs in pulmonary arterial hypertension: clinical and regulatory perspectives. J Am Coll Cardiol 2004;43(12 Suppl S):48S–55S. [DOI] [PubMed]


