Abstract
Coronary arteriovenous fistula is a rare congenital heart disease. A 71-year-old woman suffered from heart failure due to massive coronary arteriovenous fistulae from the right coronary artery and left circumflex artery to the coronary sinus. Using the off-pump technique, we successfully performed Starfish-assisted obliteration of the fistulae. Intraoperative transesophageal echocardiography was used to confirm the complete elimination of the abnormal shunt flow.
Key words: Arteriovenous fistula/therapy, cardiac surgery, off-pump, coronary vessel anomalies, echocardiography, transesophageal, heart defects, congenital
Coronary arteriovenous fistula is a rare congenital heart disease in which 1 of the 3 coronary arteries drains either into a right-heart chamber or into a vein.1 Only 5% of coronary arteriovenous fistulae arise from both the right and left coronary arteries, and only 7% drain into the coronary sinus.2 We report the case of a patient in whom congenital coronary arteriovenous fistulae arose from both the right and left coronary arteries and drained into the coronary sinus. The patient underwent fistula obliteration with the assistance of the Starfish™ Heart Positioner (Medtronic, Inc.; Minneapolis, Minn).
Case Report
A 71-year-old woman had begun to notice progressive exertional dyspnea when she was 66 years old. Upon her presentation at that time, a grade 2/6 continuous murmur was audible on auscultation, and echocardiography showed mild cardiomegaly without valvular abnormality or septal defect. Coronary arteriovenous fistula was diagnosed by means of coronary angiography. Surgical intervention was suggested, but the patient refused.
Over the next 5 years, her symptoms of exertional dyspnea worsened, and her cardiac function progressed from New York Heart Association (NYHA) functional class II to III. Repeat echocardiography revealed dilatation of all 4 cardiac chambers. The left ventricular ejection fraction was 0.70. Computed tomographic scanning of the chest showed a dilated right coronary artery, 1.5 cm in diameter. When cardiac catheterization and coronary angiography were repeated, a markedly dilated and tortuous right coronary artery was seen to drain into the coronary sinus. Another, smaller coronary arteriovenous fistula drained from the left circumflex artery to the coronary sinus (Fig. 1). The pulmonary artery pressure was elevated to 43/11 mmHg. A step-up of oxygen saturation was found between the vena cava and the right atrium. The pulmonary-to-systemic flow ratio was 1.72.
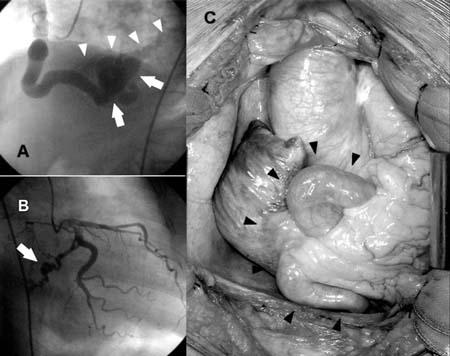
Fig. 1 The coronary angiograms and the operative findings of the coronary arteriovenous fistulae. Panel A shows the dilated right coronary artery with aneurysmal formation (arrows), draining into the coronary sinus (arrowheads). Panel B reveals the smaller fistula from the left circumflex artery (arrow). Panel C shows the dilated and tortuous right coronary artery (arrowheads).
In February 2003, she underwent fistula ligation through a median sternotomy with the assistance of the Starfish Heart Positioner. For clearer visualization of the posteroinferior wall of the heart and the coronary arteriovenous fistulae, we applied the Starfish device and placed the patient in the Trendelenburg position (Fig. 2). We found a dilated and tortuous right coronary artery with aneurysmal malformation near its drainage site into the coronary sinus. The smaller fistula lay more posteriorly. Although intraoperative transesophageal echocardiography demonstrated turbulent flow in the coronary sinus, it could not clearly illustrate which vessel was draining. To confirm the location of the fistula, we temporarily occluded several suspected vascular segments until we eliminated the shunt flow that was shown by transesophageal echocardiography. Each fistula was ligated by means of several over-and-over 3-0 Prolene sutures, reinforced with pledgetted sutures. Complete obliteration of the left-to-right shunt was confirmed intraoperatively by transesophageal echocardiography. The patient recovered smoothly and was discharged 10 days after the operation. Follow-up echocardiography did not demonstrate turbulent flow in the coronary sinus.
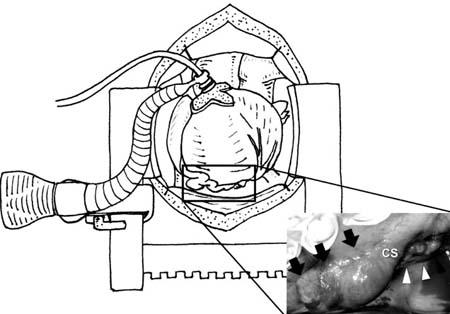
Fig. 2 The use of the Trendelenburg position and the application of the Starfish™ on the apex, in order to lift the heart, enable the management of a deeply seated coronary arteriovenous fistula without cardiopulmonary bypass. The arrows indicate the location of the right coronary artery aneurysm, close to the drainage site into the coronary sinus (CS). The arrowheads point to the location of the fistula from the left circumflex artery.
Discussion
Coronary arterial fistula is a rare congenital heart disease. The incidence was 0.13% in a consecutive series of 14,708 coronary angiograms.3 The fistulae are usually small and of little hemodynamic significance. Approximately half of all such fistulae arise from the right coronary artery and somewhat less than half from the left coronary artery. Only 5% arise from both sides. Over 90% of coronary arterial fistulae drain into the systemic venous side of the circulation. Around 40% drain into the right ventricle, 25% drain into the right atrium, 15% drain into the pulmonary trunk, and only 7% drain into the coronary sinus.2 Most patients with congenital coronary arteriovenous fistulae are asymptomatic.3 In the presence of congestive heart failure, significant left-to-right shunt, or arrhythmia, closure of coronary fistula is suggested.4 Our patient had massive coronary fistulae with a left-to-right shunt of 1.72 and progressive symptoms of heart failure, which fulfilled the indications for surgical obliteration.
Possible therapeutic options in the management of coronary arteriovenous fistulae include transcatheter embolization and surgical correction. Although Reidy and colleagues5 reported successful transcatheter embolization of coronary fistulae in 6 patients in 1991, complications might occur. Major complications accompanied 17% of the successful closures reported by Qureshi and Tynan,6 although their overall success rate was high (37 of 40 patients). Mavroudis and coworkers7 found coil embolization to be possible in only 6 of 16 patients with coronary arterial fistulae. In contrast, they found surgical management to be a safe and effective treatment that yielded 100% survival and 100% closure rates. Those authors suggested that surgical obliteration should be considered the standard.7
In most cases, surgical treatment is performed with the patient on extracorporeal circulation, especially when treatment involves deeply seated coronary fistulae that drain into the coronary sinus. Due to the advance of off-pump techniques in coronary artery bypass and to the development of new heart positioners, the ligation of fistulae located at the posterior and inferior wall has become possible without cardiopulmonary bypass. Also, intraoperative transesophageal echocardiography has become a routine procedure during cardiac operation in our institution, where it plays an important role in evaluating the efficacy of fistula obliteration, thus facilitating our application of the off-pump technique. We have also used the Starfish heart positioner to facilitate our work on coronary arteriovenous fistula.
In summary, surgical ligation is still the standard treatment method for coronary arteriovenous fistula. The results of the present case support the applicability of the Starfish heart positioner to facilitate fistula obliteration and to avoid cardiopulmonary bypass.
Footnotes
Address for reprints: Jiun-Yi Li, MD, Department of Surgery, Mackay Memorial Hospital, No. 92, Sec. 2, Chung-Shan N. Rd., Taipei, Taiwan, Republic of China
E-mail: jyl5891@ms2.mmh.org.tw
References
- 1.Hakim F, Madani A, Goussous Y, Cao QL, Hijazi ZM. Transcatheter closure of a large coronary arteriovenous fistula using the new Amplatzer Duct Occluder. Cathet Cardiovasc Diagn 1998;45:155–7. [DOI] [PubMed]
- 2.Perloff JK. Congenital coronary arterial fistula. In: Perloff JK, editor. The clinical recognition of congenital heart disease. 4th ed. Philadelphia: WB Saunders; 1994. p. 562–80.
- 3.Gillebert C, Van Hoof R, Van de Werf F, Piessens J, De Geest H. Coronary artery fistulas in an adult population. Eur Heart J 1986;7:437–43. [DOI] [PubMed]
- 4.Tkebuchava T, Von Segesser LK, Vogt PR, Jenni R, Arbenz U, Turina M. Congenital coronary fistulas in children and adults: diagnosis, surgical technique and results. J Cardiovasc Surg (Torino) 1996;37:29–34. [PubMed]
- 5.Reidy JF, Anjos RT, Qureshi SA, Baker EJ, Tynan MJ. Transcatheter embolization in the treatment of coronary artery fistulas. J Am Coll Cardiol 1991;18:187–92. [DOI] [PubMed]
- 6.Qureshi SA, Tynan M. Catheter closure of coronary artery fistulas. J Interv Cardiol 2001;14:299–307. [DOI] [PubMed]
- 7.Mavroudis C, Backer CL, Rocchini AP, Muster AJ, Gevitz M. Coronary artery fistulas in infants and children: a surgical review and discussion of coil embolization. Ann Thorac Surg 1997;63:1235–42. [DOI] [PubMed]


