Abstract
A total of 92 clinical isolates of dermatophytes (52 of Trichophyton rubrum and 40 of Trichophyton mentagrophytes) were selected for testing with six antifungal drugs (terbinafine, griseofulvin, clotrimazole, miconazole, isoconazole, and fluconazole) and two pairs of drug combinations (ketoconazole-cyclopiroxolamine and itraconazole-cyclopiroxolamine). Two methods of inoculum preparation for susceptibility testing were evaluated that used (i) inocula consisting only of microconidia of dermatophytes filtered in Whatman filter model 40 and (ii) unfiltered inocula consisting of hyphae and microconidia. We followed the recommendations of approved document M38-A of CLSI (formerly NCCLS) with some adaptations, including an incubation period of 7 days and an incubation temperature of 28°C. Reference strains of Candida parapsilosis, Candida krusei, Trichophyton rubrum, and Trichophyton mentagrophytes were included as quality-control strains. MICs were consistently higher (usually 1 to 2 dilutions for drugs tested individually) when nonfiltered inocula were tested (P < 0.01) except for terbinafine. Larger MICs were seen when testing drugs with nonfiltered inocula. The curves of drug interaction were used to analyze the reproducibility of the test, and it was shown that high levels of reproducibility were achieved using the methodology that included the filtration step. The standardization of methodologies is the first step to yield reliability of susceptibility testing and to proceed with clinical laboratory studies to correlate MICs with clinical outcomes.
Dermatophytoses are among the world's most common diseases, and dermatophytes constitute an important public health problem as yet unresolved (7). Because dermatophytes require keratin for growth, they are commonly restricted to hair, nails, and superficial skin. Transmission can occur by direct contact or from exposure to desquamated cells. Direct inoculation through breaks in the skin often occurs in individuals with depressed cell-mediated immunity. The choice of appropriate treatment is determined by the site and extent of the infection and the species involved as well as by the efficacy, safety profile, and kinetics of the available drugs (8). Dermatophytoses generally respond well to topical antifungal therapy, although local therapy may be inappropriate for extensive infections or infections affecting the nails or the scalp (9). Onychomycosis is a common condition that represents up to 50% of all nail problems and 30% of all cases of dermatophytoses (6).
The prevalence of fungal infections in humans and the development of new antifungal agents have increased the interest in antifungal susceptibility testing for dermatophytes. Despite much effort, there are still some methodological problems (14). Work on the development of standardized procedures for testing filamentous fungi has led to the publication by CLSI (formerly NCCLS) (15) of the approved reference document M38-A, which recommends the use of standard RPMI 1640 broth, nongerminated conidial inoculum suspensions of approximately 104 CFU/ml, and incubation at 35°C for periods ranging from 24 to 72 h (4). In previous work (18), we studied and adapted these testing conditions for Trichophyton rubrum; briefly, the best conditions were RPMI 1640 standard broth, incubation at 28 or 35°C for 7 days, and an inoculum consisting only of microconidia.
One of the most important aspects of antifungal susceptibility testing is inoculum preparation. For some fungi, including several dermatophytes, the wall of the macroconidia is considerably thicker than the hyphae, and it is not known whether the antifungal susceptibilities of these two morphological forms are different (7). Cultures of T. rubrum and Trichophyton mentagrophytes are formed by hyphae and microconidia and rarely by macroconidia, and the separation of these structures would make a homogenous inoculum, which might influence the reproducibility and reliability of susceptibility testing.
The aim of this study was to evaluate the variability and reproducibility of different methods for inoculum preparation for determining MICs of six antifungal drugs and two-drug combinations for 52 clinical isolates of T. rubrum and 40 of T. mentagrophytes.
MATERIALS AND METHODS
Isolates.
We selected 52 clinical isolates of T. rubrum and 40 of T. mentagrophytes. All isolates were maintained in sterile saline solution (0.9%) at 4°C until testing was performed. The strains Candida parapsilosis (ATCC 22019), Candida krusei (ATCC 6258), Trichophyton rubrum (ATCC 40051), and Trichophyton mentagrophytes (ATCC 40004) were included as quality-control strains.
Preparation of inocula.
First of all, isolates of dermatophytes were transferred from sterile saline solution (0.9%) to potato dextrose agar and incubated at 28°C for 7 days using the previously tested procedure to produce conidia (18). The fungal colonies were covered with 5 ml of sterile saline solution (0.9%), and suspensions were made by gently probing the surface with the tip of a Pasteur pipette, generating a mixture of conidial and hyphal fragments. This procedure was undertaken with two tubes with colonies of the same isolate treated separately as follows. (i) The contents of the first tube were filtered with a Whatman filter model 40 (pore size, 8 μm), which retains hyphal fragments and permits passage only of dermatophyte microconidia (18). (ii) In the other tube, heavy particles (hypha fragments and macroconidia, if produced) were allowed to settle for 15 to 20 min at room temperature as recommended by CLSI (M38-A). The densities of these suspensions were adjusted with a spectrophotometer at a wavelength of 520 nm to a transmittance level of 70 to 72%. Inoculum quantification was made by plating 0.01 ml of each kind of inoculum suspension (filtered and nonfiltered) in Sabouraud dextrose agar. The plates were incubated at 28°C and were examined daily for the presence of fungal colonies. The inoculum suspensions were diluted (1:50) in RPMI 1640 buffered with 0.165 M morpholinepropanesulfonic acid (MOPS) (34.54 g per liter) at a pH of 7.0.
Antifungal drugs.
Antifungal drugs were donated as follows: ketoconazole was donated by Janssen-Cilag, fluconazole by Pfizer, terbinafine by Novartis, griseofulvin by Schering-Plough, clotrimazole by Bayer, isoconazole and miconazole by Cristália, and cyclopiroxolamine by Pratti, Donaduzzi. Itraconazole was used in its commercial formulation (Janssen-Cilag). All drugs were dissolved in 100% dimethyl sulfoxide (Gibco) following the protocol of CLSI and were prepared in stock solutions of 1,000 μg/ml, which were diluted in RPMI 1640 test medium (buffered with morpholinepropanesulfonic acid) to yield twice (when a drug was tested individually) or four times (when a drug was tested in combination with another drug) the final strength required for the test.
Test procedure.
The tests were performed in sterile, flat-bottomed, 96-well microplates.
(i) Antifungal susceptibility testing.
The individual MICs were determined following the microdilution method recommended by CLSI, approved standard M38-A, as modified by Santos and Hamdan (18). Each microdilution well containing 100 μl of the twofold drug concentration was inoculated with 100 μl of the diluted inoculum suspension. For each test plate, two drug-free controls were included, one with the medium alone (sterile control) and the other with 100 μl of medium plus 100 μl of inoculum suspension (growth control). Each kind of inoculum suspension (filtered and nonfiltered) was tested with all the drugs. The concentrations assayed ranged from 0.031 to 16.0 μl/ml for terbinafine, miconazole, clotrimazole, and isoconazole and from 0.125 to 64.0 μl/ml for fluconazole and griseofulvin.
(ii) Interactions of drugs in vitro.
Drug interaction was tested for cyclopiroxolamine with ketoconazole and for cyclopiroxolamine with itraconazole for all tested isolates. The medium used and preparations of inoculum were the same as for susceptibility testing. However, a checkerboard microdilution method (12), which provides a matrix of all possible drug combinations in the required concentration range, was utilized to test the susceptibility of drugs in double combinations. One microplate was used to test each kind of inoculum of each strain for each pair of drug combinations. The final concentrations assayed ranged from 0.015 to 1.0 μg/ml for cyclopiroxolamine, 0.003 to 2.0 μg/ml for itraconazole, and 0.007 to 4.0 μg/ml for ketoconazole. All tests were performed in duplicate.
Incubation time and temperature.
The microdilution plates were incubated at 28°C and were read visually after 7 days of incubation.
Reading and interpretation.
For drugs tested individually, endpoint determination values were read visually with the aid of an inverted reading mirror. For azole derivatives and griseofulvin, the MIC was the lowest concentration showing a prominent growth inhibition (approximately 80% of inhibition when compared to growth control results). For terbinafine, the MIC was defined as the lowest concentration showing 100% growth inhibition. MIC ranges and geometric means were obtained for each drug to facilitate comparisons of the activities of tested drugs as well as readings of the MIC50, at which 50% of the isolates were inhibited; similarly, the MIC90 is the MIC at which 90% of the isolates were inhibited. For drug combinations, endpoint determination was obtained visually as the lowest concentration showing prominent growth inhibition for each pair of drug concentrations. Modes of interaction between drugs were classified as synergism, additivism, or antagonism based on the profile of the interaction drug curves and by means of the fractional inhibitory concentration index (FIC), which was calculated by the following formula: (MIC A in combination/MIC A) + (MIC B in combination/MIC B). The interaction was defined as synergistic when the FIC was ≤0.5, indifferent when the FIC was >0.5 but <4.0, and antagonistic when the FIC was >4.0 (10).
Data analysis.
When drugs were tested individually, the influence of the method of inoculum preparation on MICs was performed using Wilcoxon (Mann-Whitney) and Kruskal-Wallis tests. When drugs were tested in combination, the curves were analyzed by simple linear regression and by Pearson's correlation to verify the influence of inocula on test reproducibility. A P value of <0.01 was considered to be significant.
RESULTS
All organisms tested produced detectable growth after 7 days of incubation. According to statistical analyses, MICs for clinical and reference isolates of T. rubrum and T. mentagrophytes were similar for all tested drugs. Fluconazole and itraconazole MICs for Candida parapsilosis (ATCC 22019) and Candida krusei (ATCC 6258) control isolates were within the expected range (2). Table 1 summarizes susceptibility data for 92 dermatophyte clinical isolates tested. In general, drug MICs for filtered inocula were significantly correlated with lower MICs whereas drug MICs for unfiltered inocula were significantly correlated with higher MICs with no dilution interval (P < 0.01), except for terbinafine, which presented MICs of <0.031 μg/ml for all tested isolates. Readings were easier to perform when filtered inocula were used in tests, because the growth of filtered suspensions in microplates was more homogenous. Individual MICs for reference dermatophyte isolates were similar to the previous study results (18).
TABLE 1.
Fluconazole, griseofulvin, miconazole, isoconazole and clotrimazole in vitro susceptibility data for 92 dermatophyte isolates with different methods for inoculum preparation
| Tested agent | MIC data (μg/ml)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Filtered inocula
|
Nonfiltered inocula
|
|||||||
| Range | Ga | MIC50b | MIC90c | Range | Ga | MIC50b | MIC90c | |
| Fluconazole | 0.125->64.0 | 64.0 | 64.0 | >64.0 | 0.125->64.0 | >64.0 | >64.0 | >64.0 |
| Griseofulvin | 0.125-4.0 | 0.75 | 1.0 | 2.0 | 0.125-8.0 | 1.5 | 2.0 | 4.0 |
| Miconazole | 0.031-0.5 | 0.25 | 0.25 | 0.5 | 0.031-1.0 | 0.37 | 0.5 | 1.0 |
| Isoconazole | 0.031-0.5 | 0.09 | 0.0625 | 0.25 | 0.031-2.0 | 0.19 | 0.25 | 1.0 |
| Clotrimazole | 0.031-0.5 | 0.0625 | 0.0625 | 0.5 | 0.031-1.0 | 0.16 | 0.25 | 1.0 |
Geometric means.
MIC at which 50% of the isolates were inhibited.
MIC at which 90% of the isolates were inhibited.
The statistical analysis revealed that inoculum sizes of filtered suspensions and nonfiltered suspensions were significantly different (data not shown) (P < 0.01).
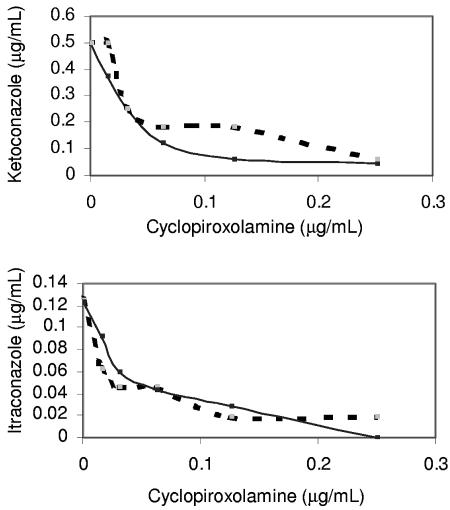
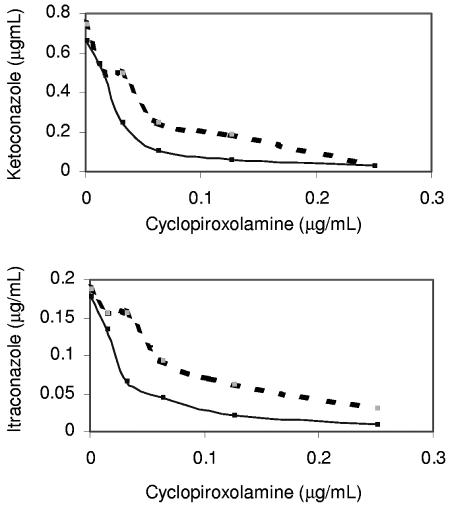
Figures 1 and 2 demonstrate the influence of the method of inoculum preparation in drug combinations for Trichophyton rubrum (ATCC 40051) and Trichophyton mentagrophytes (ATCC 40004). Growth observed in wells of microdilution plates was more homogenous when filtered suspensions were tested. Statistical analyses revealed that methods compared in this work were different and that tests performed with filtered inocula exhibited results with better linear correlation (Pearson's correlation) between the MICs of each drug for both pairs of drug combinations. According to these data, reproducibility of tests using only microconidia as inocula was considerably higher than for nonfiltered suspensions (P < 0.01). These figures represent the results that were obtained for all tested isolates. All tested drug combinations showed synergistic interaction (FIC < 0.5) for all isolates when filtered suspensions were used, confirming theoretical synergism between tested drugs, but this was not true when nonfiltered suspensions were used in the tests (data not shown). According to this, unfiltered inocula didn't confirm the theoretical synergism, revealing less reproducibility when linear regression and Pearson's correlation tests were used. For terbinafine all isolates exhibited high-susceptibility profiles in which all the MICs were <0.031; therefore, when this drug was tested the method of inoculum preparation had no influence.
FIG. 1.
Combinations of two pairs of drugs (ketoconazole-cyclopiroxolamine and itraconazole-cyclopiroxolamine) tested with Trichophyton rubrum (ATCC 40051) by use of different methods of inoculum preparation. Full lines represent data obtained with filtered inocula, and dashed lines represent data obtained with nonfiltered inocula. Irregular curves were obtained when unfiltered suspensions were tested. Results obtained with filtered inocula confirm the theoretical synergism for both pairs of drug combinations and exhibited high reproducibility.
FIG. 2.
Combinations of two pairs of drugs (ketoconazole-cyclopiroxolamine and itraconazole-cyclopiroxolamine) tested with Trichophyton mentagrophytes (ATCC 40004) by use of different methods of inoculum preparation. Full lines represent data obtained with filtered inocula, and dashed lines represent data obtained with nonfiltered inocula. Irregular curves were obtained when unfiltered suspensions were tested. Results obtained with filtered inocula confirm the theoretical synergism for both pairs of drug combinations and exhibited high reproducibility.
DISCUSSION
An increasing number of antimycotics have become available for the treatment of dermatophytoses; at the same time, however, there are reports suggesting recalcitrance or possibly even resistance to drug therapy of dermatophytes. In vitro analysis of the antifungal activity of these agents enables a comparison between different antimycotics, which in turn may clarify the reasons for the lack of clinical response and assist clinicians in choosing an effective therapy for their patients (12). One of the most important aspects of antifungal susceptibility testing is inoculum size and constitution, which can have an influence on susceptibility results.
Recently, several groups have adapted the reference method for broth dilution antifungal susceptibility testing of conidium-forming filamentous fungi (15) to develop a more specific assay for dermatophytes (7). Some studies testing Aspergillus spp. have compared MICs obtained with hyphal suspensions to those obtained with conidial suspensions by using both forms of inocula and found similar MICs (3, 5, 17). Aberkane et al. (1) compared inoculum sizes obtained by spectrophotometric adjustment and hemacytometer counting of a large range of filamentous fungi, and although dermatophytes were not included in that study, the information is useful for analysis of inoculum preparation methodology.
Colonies of T. rubrum and T. mentagrophytes are generally formed by hyphae and microconidia; macroconidia is rarely formed in conventional culture media (13) used in this work. Although the invasive forms of filamentous fungi are generally hyphae, the reference method (15) recommends the use of conidial suspensions for inocula. The CLSI-approved guidelines recommend separation of the fungal structures (hyphae and conidia) through sedimentation for 15 to 20 min and use of the upper part of the suspension for susceptibility testing (15). This sedimentation step is not totally efficient in removing hyphae from the inoculum suspension, as demonstrated in a pilot experiment by counting dermatophyte structures by use of a hemacytometer (data not shown). We consider the separation of hyphae and conidia a crucial step for the determination of MICs for dermatophytes.
Some researchers (7, 11, 14) have proposed that hyphae of dermatophytes could be removed by using a filtration process with sterile gauze, but the pore diameter of this material is unstandardized and variable. Nimura et al. (16) used a filter from Becton Dickinson Labware (pore size, 40 μm) to separate hyphae from conidia of Trichophyton spp. Aberkane et al. (1) used another filter with a pore size of 11 μm in the study mentioned above. Since the dimensions of microconidia of T. rubrum and T. mentagrophytes range from 2 by 3 μm to 3 by 5 μm (13) and since hyphae have variable dimensions depending on whether they are intact or fragmented, filters with a pore size of 40 or 11 μm would probably permit passage of fragments of hyphae and microconidia, constituting an inhomogeneous inoculum. We used a filter with a pore size of 8 μm, which considerably reduces the possibility of presence of hyphae fragments in inocula. The presence of macroconidia was not considered because macroconidia are rarely produced by tested species in the media used, but if they were formed they would probably be retained in the filtration process.
In the present work, the method of inoculum preparation significantly influenced the MIC determinations for T. rubrum and T. mentagrophytes (P < 0.01). First of all, when inocula were filtered with Whatman filter model 40, growth in microplates was more homogenous than was seen with nonfiltered inocula, which makes reading easier. When drugs were tested individually, MICs were considerably higher (P < 0.01) (usually 1 to 2 dilutions) when inocula were not filtered (with no dilution interval), suggesting that microconidia of tested species could present more susceptibility to antifungal drugs than hyphae. A possible explanation of these data is the thinner cell wall of microconidia in comparison to hyphae. This is not true for dermatophytes with thick-wall macroconidia, as demonstrated by Fernández-Torres et al. (7), who found that macroconidia are more resistant to antifungal agents than hyphae, which influences results of susceptibility testing for this group of fungi; differences of susceptibility were attributed to thickness of cell wall.
Reproducibility of any analytical methodology has great influence on its reliability. Simple linear regression and Pearson's correlation were used to analyze this parameter, and values of Pearson's correlation for filtered inocula were generally higher than for nonfiltered inocula (P < 0.01) (data not shown), revealing greater reproducibility when the filtration step was included. In addition, the profiles of curves of drug interactions for all tested isolates were different, as illustrated in Fig. 1 and 2 for reference dermatophytes, demonstrating a lower level of reproducibility when inocula were constituted by hyphae and microconidia. We expected a synergism profile to result from tests of azoles with cyclopiroxolamine, but it was exhibited only when filtered inocula were tested. Unfiltered inocula demonstrated irregular curves of drug interaction for all tested isolates (data not shown), as illustrated in Fig. 1 and 2 for reference dermatophytes. This reinforces the need for separation of structures in susceptibility testing for dermatophytes that are producers of microconidia. Overall, we think that the method of inoculum preparation requires a species-dependent or group-dependent standardization process, especially for filamentous fungi, since they can be constituted of two or more structures.
In conclusion, the results detailed above show that a filtration process is useful to separate hyphal fragments from microconidia of T. rubrum and T. mentagrophytes, providing greater reproducibility and reliability of susceptibility-resistance determination. In addition, the standardization of methodologies is the first step in efforts to ensure the reliability of any antifungal susceptibility testing which will allow clinical laboratory studies to correlate MICs with clinical outcomes.
Acknowledgments
We thank Walkíria Lopes Borges for outstanding technical assistance. Our thanks also to Agostinho Jairo Santos Machado and Isabela da Costa César for critical comments.
REFERENCES
- 1.Aberkane, A., M. Cuenca-Estrela, A. Gomez-Lopes, E. Petrikkou, E. Mellado, A. Mozón, J. L. Rodríguez-Tudella, and Eurofung Network. 2002. Comparative evaluation of two different methods of inoculum preparation for antifungal susceptibility testing of filamentous fungi. J. Antimicrob. Chemother. 50:719-722. [DOI] [PubMed] [Google Scholar]
- 2.Barry, A. L., M. A. Pfaller, S. D. Brown, A. Espinel-Ingroff, M. A. Ghannoum, C. Knapp, R. P. Rennie, J. H. Rex, and M. G. Rinaldi. 2000. Quality control limits for broth microdilution susceptibility tests of ten antifungal agents. J. Clin. Microbiol. 38:3457-3459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Espinel-Ingroff, A. 2003. Evaluation of broth microdilution testing parameters and agar diffusion Etest procedure for testing susceptibilities of Aspergillus spp. to caspofungin acetate (MK-0991). J. Clin. Microbiol. 41:403-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Espinel-Ingroff, A. 2001. Comparison of the E-test with the NCCLS M38-P method for antifungal susceptibility testing of common and emerging pathogenic fungi. J. Clin. Microbiol. 39:1360-1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Espinel-Ingroff, A., M. Bartlett, R. Bowden, N. X. Chin, C. Cooper, Jr., A. Fothergill, M. R. McGinnis, P. Menezes, S. A. Messer, P. W. Nelson, F. C. Odds, L. Pasarell, J. Peter, M. A. Pfaller, J. H. Rex, M. G. Rinaldi, G. S. Shankland, T. J. Walsh, and I. Weitzman. 1997. Multicenter evaluation of proposed standardized procedure for antifungal susceptibility testing of filamentous fungi. J. Clin. Microbiol. 35:139-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faergemann, J., and R. Baran. 2003. Epidemiology, clinical presentation and diagnosis of onychomycosis. Br. J. Dermatol. 149:1-4. [DOI] [PubMed] [Google Scholar]
- 7.Fernández-Torres, B., I. Inza, and J. Guarro. 2003. Comparison of in vitro antifungal susceptibilities of conidia and hyphae of dermatophytes with thick-wall macroconidia. Antimicrob. Agents Chemother. 47:3371-3372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernández-Torres, B., F. J. Cabañes, A. J. Carrillo-Muñoz, A. Esteban, I. Inza, L. Abarca, and J. Guarro. 2002. Collaborative study of optimal antifungal susceptibility testing conditions for dermatophytes. J. Clin. Microbiol. 40:3999-4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernández-Torres, B., A. J. Carrilo, E. Martín, A. Del Palácio, M. K. Moore, A. Valverde, M. Serrano, and J. Guarro. 2001. In vitro activities of 10 antifungal drugs against 508 dermatophyte strains. Antimicrob. Agents Chemother. 45:2524-2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gómez-López, A., M. Cuenca-Estrella, E. Mellado, and J. L. Rodriguez-Tudella. 2003. In vitro evaluation of combination of terbinafine with itraconazole or amphotericin B against Zygomycota. Diagn. Microbiol. Infect. Dis. 45:199-202. [DOI] [PubMed] [Google Scholar]
- 11.Guarro, J., C. Llop, C. Aguilar, and I. Pujol. 1997. Comparison of in vitro antifungal susceptibilities of conidia and hyphae of filamentous fungi. Antimicrob. Agents Chemother. 41:2760-2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta, A. K., and Y. Kohli. 2003. In vitro susceptibility testing of ciclopirox, terbinafine, ketoconazole and itraconazole against dermatophytes and nondermatophytes, and in-vitro evaluation of combination antifungal activity. Br. J. Dermatol. 149:296-305. [DOI] [PubMed] [Google Scholar]
- 13.Lacaz, C. S., E. Porto, J. E. C. Martins, E. M. Heins-Vaccari, and N. T. Melo. 2002. Micoses superficiais, p. 252-340. In Tratado de micologia médica lacaz, 9th ed. Sarvier, São Paulo, Brazil.
- 14.Llop, C., I. Pujol, C. Aguilar, J. Sala, D. Riba, and J. Guarro. 2000. Comparison of three methods of determining MICs for filamentous fungi using different end point criteria and incubation periods. Antimicrob. Agents Chemother. 44:239-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Committee for Clinical Laboratory Standards. 2002. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi. Approved standard M38-A. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 16.Nimura, K., Y. Niwano, S. Ishiduka, and R. Fukumoto. 2001. Comparison of in vitro antifungal activities of topical antimycotics launched in 1990s in Japan. Int. J. Antimicrob. Agents 18:173-178. [DOI] [PubMed] [Google Scholar]
- 17.Pujol, I., J. Capilla, B. Fernández-Torres, M. Ortoneda, and J. Guarro. 2002. Use of the sensititre colorimetric microdilution panel for susceptibility testing of dermatophytes. J. Clin. Microbiol. 40:2618-2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Santos, D. A., and J. S. Hamdan. 2005. Evaluation of broth microdilution antifungal susceptibility testing conditions for Trichophyton rubrum. J. Clin. Microbiol. 43:1917-1920. [DOI] [PMC free article] [PubMed] [Google Scholar]