Abstract
Objective To evaluate two commercial stool tests for detection of secretory IgA antibodies against gliadin and human tissue transglutaminase for diagnosis of coeliac disease in children with symptoms.
Setting Tertiary care children's hospital.
Participants Coded stool samples from 20 children with newly diagnosed coeliac disease and 64 controls. Six children with coeliac disease had stool tests every two weeks for three months after starting a gluten-free diet.
Main outcome measures Secretory IgA antibodies against gliadin and human tissue transglutaminase in stool samples, determined in duplicate by using recommended cut-off limits.
Results Sensitivity of faecal antibodies against human tissue transglutaminase was 10% (95% confidence interval 1% to 32%), and specificity was 98% (91% to 100%). For antibodies against gliadin, sensitivity was 6% (0% to 29%) and specificity was 97% (89% to 100%). Optimisation of cut-off limits by receiver operating characteristic analysis and use of results of both tests increased sensitivity to 82%, but specificity decreased to 58%. All follow-up stool tests remained negative, except for two positive anti-gliadin results in one patient, six and 10 weeks after the gluten-free diet was started.
Conclusions Neither stool test was suitable for screening for coeliac disease in children with symptoms.
Introduction
Serological screening for antibodies against gliadin, endomysium, or tissue transglutaminase before the diagnostic biopsy is done is well established practice in patients with suspected coeliac disease. These antibodies can be detected in faecal supernatants,1 and commercial stool tests have been developed and offered by many laboratories. However, no validation data on these tests have been published. We evaluated two stool tests (Immundiagnostik GmbH, Bensheim, Germany) in comparison with serological results and duodenal histology as “gold standard” in children who had had upper endoscopy for different abdominal conditions.
Methods
The study cohort consisted of 20 children with newly diagnosed coeliac disease (median age 5.4 (range 0.9-14.1) years), all with duodenal villous atrophy (Marsh III)2 plus positive endomysium antibodies in serum, and 64 control children (5.6 (0.9-17.5) years) with normal histology (Marsh 0) and negative endomysium antibodies (61/61 tested). We excluded patients with selective IgA deficiency, previously diagnosed coeliac disease, or bloody diarrhoea.
We analysed coded stool samples for secretory IgA antibodies against recombinant human tissue transglutaminase in all 20 children with coeliac disease and 62/64 children without coeliac disease. We analysed samples for antibodies against gliadin in 17/20 children with coeliac disease and 61/64 controls.
Results
Faecal tissue transglutaminase antibodies were positive in two children with coeliac disease and two children without coeliac disease (sensitivity 10%, 95% confidence interval 1% to 32%; specificity 98%, 91% to 100%). Faecal anti-gliadin antibodies were positive in one child with coeliac disease and one control patient (sensitivity 6%, 0% to 29%; specificity 97%, 89% to 100%). Six patients with coeliac disease provided stool samples before and every two weeks for three months after starting a gluten-free diet, which all remained negative, except for two positive anti-gliadin test results in one patient, six and 10 weeks after starting the gluten-free diet.
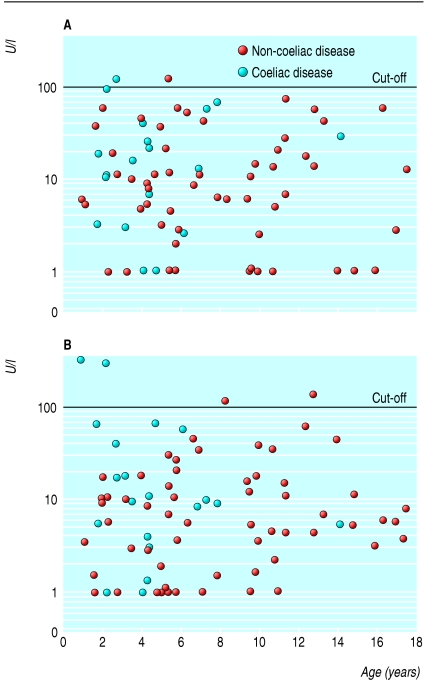
The κ values between histology and stool test were 0.093 (-0.033 to 0.219) for tissue transglutaminase antibodies and 0.062 (-0.027 to 0.151) for anti-gliadin antibodies, indicating no agreement. The figure gives the individual titres in relation to age. When we optimised cut-off limits by receiver operating characteristic analysis and combined both tests, sensitivity increased to 82% but specificity decreased to 58%, with positive and negative predictive values of 37% and 92%. These figures may change when the tests are used prospectively on new cases. The prevalence of coeliac disease in our cohort was 29% (17/59), but in the general population, with an assumed prevalence of 0.5%, the positive predictive value would decrease to 1%, with marginal improvement of the negative predictive value compared with the pre-test situation (from 99.5% to 99.8%).
Discussion
Both stool tests were negative in most cases of coeliac disease and hence are not reliable as screening tests. We have validated these stool tests against the accepted diagnostic “gold standard” for coeliac disease. In many European countries, validation of a diagnostic test in the target population is not required before commercialisation, or diagnostic tests are marketed for years without any evaluation. Many paediatric gastroenterologists share our experience of receiving referrals with a request to do endoscopy on the basis of a positive stool test result. Even worse, children have been started on a gluten-free diet on the basis of positive stool test results alone.
Figure 1.
Results of individual stool samples: (A) secretory IgA antibodies against gliadin from 17 patients with coeliac disease and 61 control children with gastrointestinal diseases other than coeliac disease but normal duodenal histology; (B) secretory IgA antibodies against human tissue transglutaminase from 20 patients with coeliac disease and 62 controls. Marked cut-off value of 100 U/l suggested by manufacturer. Values <1 U/l plotted as 1 U/l
The tests in our study measure secretory IgA antibodies, in contrast to specific IgA antibodies used in a previous investigation in adults with coeliac disease.1 Attempts to measure specific secretory IgA in saliva and small intestinal aspirates found them to be less sensitive than determination of antibodies in serum.3 Another explanation for the poor sensitivity could be the digestion of antibodies along the bowel passage. We conclude that laboratory tests for clinical purposes need to be evaluated before their release for routine use. We propose that only adequately validated diagnostic tests should be reimbursed by health insurance.
What is already known on this topic
New commercial stool tests are promoted for non-invasive screening of patients suspected of having coeliac disease, but these tests have not been validated
What this study adds
Determination of faecal IgA antibodies against gliadin and human tissue transglutaminase failed to detect symptomatic coeliac disease in children
This article was posted on bmj.com on 23 December 2005: http://bmj.com/cgi/doi/10.1136/bmj.38688.654028.AE
Contributors: MK designed the study, did statistical analysis, and wrote the manuscript with SK. SK-E helped with the study design and supervised the test procedures in the laboratories. VD helped HZ to do the stool tests, collected clinical data from CRF, helped with the statistical analysis, and recruited the coeliac patients for the follow-up part of the study. HZ did the stool tests. SK is the study coordinator and guarantor, designed the study protocol, and wrote the final manuscript with MK.
Funding: Immundiagnostik, Bensheim, Germany provided test kits for antibody determinations in stool samples. Otherwise, the company gave no financial support for the study, except for reimbursement of travel costs to MK, who reported the results at two scientific meetings. Immundiagnostik was not involved in the study design, the collection and interpretation of data, the writing of the report, or the decision to submit the paper for publication.
Competing interests: MK has been reimbursed by Immundiagnostik, the manufacturer of the test system, for attending two conferences. All other authors: none declared.
Ethical approval: The ethical committee of the Ludwig Maximilians University approved the use of anonymised frozen stool and serum samples for the purpose of this study.
References
- 1.Picarelli A, Sabbatella L, Di TM, Di CT, Vetrano S, Anania MC. Antiendomysial antibody detection in fecal supernatants: in vivo proof that small bowel mucosa is the site of antiendomysial antibody production. Am J Gastroenterol 2002;97: 95-8. [DOI] [PubMed] [Google Scholar]
- 2.Marsh MN. Gluten, major histocompatibility complex, and the small intestine: a molecular and immunobiologic approach to the spectrum of gluten sensitivity (`celiac sprue'). Gastroenterology 1992;102: 330-54. [PubMed] [Google Scholar]
- 3.Patinen P, Bjorksten F, Malmstrom M, Savilahti E, Reunala T. Salivary and serum IgA antigliadin antibodies in dermatitis herpetiformis. Eur J Oral Sci 1995;103: 280-4. [DOI] [PubMed] [Google Scholar]