Abstract
Problem Illicit use of injected drugs is linked with high rates of HIV infection and fatal overdose, as well as community concerns about public drug use. Supervised injecting facilities have been proposed as a potential solution, but fears have been raised that they might encourage drug use.
Design A before and after study.
Participants and setting 871 injecting drug users recruited from the community in Vancouver, Canada.
Key measures for improvement Rates of relapse into injected drug use among former users and of stopping drug use among current users.
Strategies for change Local health authorities established the Vancouver supervised injecting facility to provide injecting drug users with sterile injecting equipment, intervention in the event of overdose, primary health care, and referral to external health and social services.
Effects of change Analysis of periods before and after the facility's opening showed no substantial increase in the rate of relapse into injected drug use (17% v 20%) and no substantial decrease in the rate of stopping injected drug use (17% v 15%).
Lessons learnt Recently reported benefits of supervised injecting facilities on drug users' high risk behaviours and on public order do not seem to have been offset by negative community impacts.
Background
Outline of the problem
Cities throughout the world are experiencing high rates of HIV infection related to injected drug use, and drug overdoses are a leading cause of death in many urban settings.1,2 Infections from non-sterile injection and the unsafe public disposal of used syringes are also major concerns.3,4 To address these problems, various initiatives such as methadone maintenance therapy and needle exchange programmes have been established.5
Despite these interventions, ongoing infectious disease and overdose rates, as well as concerns related to the public use of injected drugs, have persisted.6 This is particularly true of Vancouver, Canada, which has experienced some of North America's highest rates of HIV infection and overdose despite an array of interventions.6,7
Strategy for change
In an effort to reduce the community and public health impacts of injected drug use, health authorities in Vancouver established North America's first medically supervised injection facility in September 2003. Within the facility, drug users can inject pre-obtained illicit drugs under the supervision of medical staff.8 The facility also provides sterile injecting equipment for users and intervention in the event of overdose, as well as primary health care, addictions counselling, and referral to external health and social services.9
Although similar facilities have been established in Europe and Australia,10 this intervention remains highly controversial.11-15 In particular, the dearth of formal evaluations has led to fears that such facilities may encourage drug use, increasing rates of relapse among former injecting drug users,16 and, by facilitating drug use, discourage current users from seeking treatment.16,17
Key outcome measures
We sought to determine if the supervised injection facility was associated with increased rates of relapse among former injecting drug users or reduced rates of cessation among current drug users. We also sought to assess the impact of the facility on several secondary end points.
Information gathering
We report on data derived from the Vancouver injecting drug users study, an ongoing prospective observational study of injecting drug users recruited through self referral and street outreach since May 1996.18 As part of the study, all subjects provide blood samples and complete an interviewer administered questionnaire at six-monthly follow-up visits so that drug use can be tracked longitudinally.
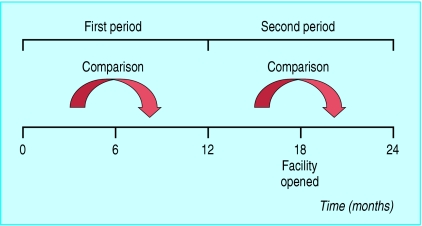
For the present study, we examined individual changes in drug use during a one-year period before the opening of the supervised injection facility (as a control period) and the one-year period that spanned the opening of the supervised injection facility on 22 September 2003 (see figure). In each one-year period we examined annual changes in injected drug use by comparing participants' behaviours in the first six months of the period with their behaviours in the final six months.
Figure 1.
Time periods used to compare changes in illicit drug use before and during the opening of the Vancouver supervised injection facility
End points of interest were defined a priori and included the rates of relapse into and of stopping injected drug use. Relapse was defined as changing from reported non-injection throughout the first six months of an annual period to reported injecting in the final six months, and stopping was defined as changing from reported injecting during the first six months of a period to reported non-injection throughout the final six months. We also examined changes in initiating and stopping crack cocaine smoking, binge drug use,8 and methadone use.
Data analysis
Since we examined individual changes in drug use, to be eligible for the present study, participants had to have been followed up at both six-monthly follow-up visits in at least one of the one year periods. We expected that most participants would be seen in all four follow-up visits, but we also performed sub-analyses restricted to those participants who were seen in all four visits.
Because of the lack of independence between data points across periods and the differing denominators (pertaining to eligible individuals) used to calculate the rates, we were unable to devise a formal method for testing significance. We recognised that the observational nature of the study meant that differences could emerge by chance or from confounding effects unrelated to the supervised injection facility, but we wanted to set a low threshold for detecting what could be a meaningful negative change in community drug use. We therefore selected a change of 5% as the cut-off point, and if any behaviour changed by more than this level, we viewed it as a substantial change worthy of further investigation. Equally, small fluctuations that might be expected in this type of study would not be misinterpreted as meaningful changes.
Effects of change
Overall, 871 participants were eligible for the study, with 674 individuals completing both follow-up interviews during the first one-year period (22 March 2002 to 22 March 2003), and 700 individuals completing both interviews in the second period (22 March 2003 to 22 March 2004). The participants in the first period had a median age of 35.3 years (interquartile range 28.6-41.3), 260 of them (39%) were women, and 206 (31%) were of aboriginal ancestry. Participants in the second period had a median age of 34.1 years (26.6-40.8), 286 (41%) were women, and 223 (32%) were of aboriginal ancestry.
As the table indicates, comparison of changes in drug use in the two one-year periods shows no substantial differences in rates of relapse into injected drug use (17% v 20%) or stopping injected drug use (17% v 15%). Similarly, there were no substantial differences in rates of stopping binge drug use (58% v 63%) or crack cocaine smoking (12% v 14%), nor in rates of starting or stopping methadone use (11% v 7% and 13% v 11% respectively). The only differences that exceeded the 5% cut-off were in the decrease in number of participants who relapsed into binge drug use in the second period (13% v 8%) and in the increase in number who started smoking crack cocaine (21% v 29%). Results were similar in the sub-analyses restricted to the 562 participants who attended all four follow-up visits (table).
Table 1.
Changes in drug use among injecting drug users in Vancouver in one-year period before the supervised injection facility opened and in the one-year period when the facility opened. Values are numbers (percentages) of participants unless stated otherwise
|
Change in drug use
|
% difference between periods
|
|||
|---|---|---|---|---|
| Variable | Before facility opened (n=674) | When facility opened (n=700) | All participants (674 v 700) | Participants in both periods (562 v 562)* |
| Using injected drugs | ||||
| Started: | ||||
| Yes | 29/174 (17) | 41/201 (20) | 3.7 | 3.5 |
| No | 145/174 (83) | 160/201 (80) | ||
| Stopped: | ||||
| Yes | 68/404 (17) | 51/348 (15) | −2.1 | −1.5 |
| No | 336/404 (83) | 297/348 (85) | ||
| Binge drug use | ||||
| Started: | ||||
| Yes | 63/468 (13) | 33/434 (8) | −5.9 | −6.4 |
| No | 405/468 (87) | 401/434 (92) | ||
| Stopped: | ||||
| Yes | 64/110 (58) | 72/115 (63) | 4.4 | 3.9 |
| No | 46/110 (42) | 43/115 (37) | ||
| Smoking crack cocaine | ||||
| Started: | ||||
| Yes | 47/225 (21) | 52/181 (29) | 7.8 | 7.3 |
| No | 178/225 (79) | 129/181 (71) | ||
| Stopped: | ||||
| Yes | 43/353 (12) | 50/368 (14) | 1.4 | 1.9 |
| No | 310/353 (88) | 318/368 (86) | ||
| Using methadone | ||||
| Started: | ||||
| Yes | 24/216 (11) | 22/302 (7) | −3.8 | −2.3 |
| No | 192/216 (89) | 280/302 (93) | ||
| Stopped: | ||||
| Yes | 26/206 (13) | 27/247 (11) | −1.7 | −3.5 |
| No | 180/206 (87) | 220/247 (89) | ||
Denominators vary because only some individuals were eligible for each change considered (for example, analyses of stopping use of injected drugs were restricted to those who were injecting at the start of the period considered).
Refers to the 562 individuals who contributed data to all four follow-up visits during the two study periods.
Lessons learnt and next steps
Our study indicates that the opening of North America's first supervised injection facility was not associated with measurable negative changes in the use of injected drugs. Indeed, we found a substantial reduction in the starting of binge drug use after the opening of the facility, suggesting that it had not prompted “risk compensation” among local injecting drug users, whereby the benefits of a safer environment are overcome by more risky behaviours such as higher intensity drug use.19 Although there was a substantial increase in the number of participants who started smoking crack cocaine, it is unlikely that the facility, which does not allow smoking in the facility, prompted this change. These findings are relevant to a recent review of supervised injection facilities by the European Monitoring Centre on Drugs and Drug Addiction, which highlighted concerns that these facilities could potentially “encourage increased levels of drug use” and “make drug use more acceptable and comfortable, thus delaying initiation into treatment.”17
Key learning points
Supervised injection facilities are associated with improved public order and reduced syringe sharing, but their impact on community drug use has not been evaluated
This study shows that the opening of a supervised injection facility did not adversely affect community drug use, including relapse into injected drug use, stopping injected drug use, and seeking treatment
Given the international public health emergency presented by injected drug use, it is not surprising that the merits of supervised injection facilities are being hotly debated.11-15,20 Evaluation of the Vancouver facility has shown that its opening has been associated with reductions in public drug use and publicly discarded syringes8 and reductions in syringe sharing among local injecting drug users.9 Our study suggests that these benefits have not been offset by negative changes in community drug use. The next step will involve further prospective evaluation of injecting drug users in the community to examine the impact of the supervised injection facility on rates of bloodborne infections and drug overdoses.
Our study has several limitations. Firstly, study participants were not a random sample, although they seemed to be representative of injecting drug users in the community.21 Secondly, we relied on drug users' reports of their own behaviour. Although studies have shown that drug users may under-report some socially undesirable behaviours,19 self reporting of illicit drug use has largely been shown to be valid.22 Furthermore, our study was designed after these data were collected, and thus the participants and interviewers were essentially blinded to this eventual use of the data. As such, we believe this eliminates interviewer bias or socially desirable responding as an explanation for our findings.
We thank the study participants for their cooperation as well as the staff of the InSite supervised injecting facility and Vancouver Coastal Health (Chris Buchner, David Marsh, Heather Hay). We also thank Kevin Craib, Richard Harrigan, Robert Hogg, Martin Schechter, Patricia Spittal, David Patrick, Calvin Lai, and Steffanie Strathdee for their research assistance, and Deborah Graham, Bonnie Devlin, John Charette, Cody Callon, Caitlin Johnston, Vanessa Volkommer, Kathy Churchill, Steve Kain, Dave Isham, Nancy Laliberte, Sue Currie, and Peter Vann for administrative help.
Contributors: TK and EW designed the study. KL, RZ, and TK conducted the statistical analyses. TK and EW drafted the manuscript and incorporated all suggestions. JM, MT, and JS contributed to the conception and design of the analyses, interpretation of the data, and drafting of the manuscript, and all authors approved the version to be published. TK is guarantor of this study.
Funding: The study was made possible through a financial contribution from Health Canada.
Competing interests: None declared.
Ethical approval: The study was approved by the University of British Columbia/Providence Health Care Research Ethics Board.
References
- 1.Des Jarlais DC, Hagan H, Friedman SR, Friedmann P, Goldberg D, Frischer M, et al. Maintaining low HIV seroprevalence in populations of injecting drug users. JAMA 1995;274: 1226-31. [DOI] [PubMed] [Google Scholar]
- 2.Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990-98. Addiction 2003;98: 739-47. [DOI] [PubMed] [Google Scholar]
- 3.Kerr T, Wood E, Grafstein E, Ishida T, Shannon K, Lai C, et al. High rates of primary care and emergency department use among injection drug users in Vancouver. J Public Health (Oxf) 2005;27: 62-6. [DOI] [PubMed] [Google Scholar]
- 4.Doherty MC, Garfein RS, Vlahov D, Junge B, Rathouz PJ, Galai N, et al. Discarded needles do not increase soon after the opening of a needle exchange program. Am J Epidemiol 1997;145: 730-7. [DOI] [PubMed] [Google Scholar]
- 5.Des Jarlais DC. Structural interventions to reduce HIV transmission among injecting drug users. AIDS 2000;14(suppl 1): S41-6. [DOI] [PubMed] [Google Scholar]
- 6.Wood E, Kerr T, Montaner JS, Strathdee SA, Wodak A, Hankins CA, et al. Rationale for evaluating North America's first medically supervised safer injecting facility. Lancet Infect Dis 2004;4: 301-6. [DOI] [PubMed] [Google Scholar]
- 7.Wood E, Spittal PM, Small W, Kerr T, Li K, Hogg RS, et al. Displacement of Canada's largest public illicit drug market in response to a police crackdown. CMAJ 2004;170: 1551-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kerr T, Tyndall M, Li K, Montaner J, Wood E. Safer injection facility use and syringe sharing in injection drug users. Lancet 2005;366: 316-8. [DOI] [PubMed] [Google Scholar]
- 9.Wood E, Kerr T, Small W, Li K, Marsh D, Montaner JS, et al. Changes in public order after the opening of a medically supervised safer injecting facility for illicit injection drug users. CMAJ 2004;171: 731-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kimber J, Dolan K, van Beek I, Hedrich D, Zurhold H. Drug consumption facilities: an update since 2000. Drug Alcohol Rev 2003;22: 227-33. [DOI] [PubMed] [Google Scholar]
- 11.Strang J, Fortson R. Supervised fixing rooms, supervised injectable maintenance clinics-understanding the difference. BMJ 2004;328: 102-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wright NM, Tompkins CN. Supervised injecting centres. BMJ 2004;328: 100-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yamey G. UN condemns Australian plans for “safe injecting rooms.” BMJ 2000;320: 667. [PMC free article] [PubMed] [Google Scholar]
- 14.Bula F. Drug plan waste of resources, city told. More drug users will come here, U.S. official warns. Vancouver Sun 2002. Nov 21: 1.
- 15.International Narcotics Control Board. Report of the International Narcotics Control Board for 2000. Geneva: United Nations, 2003.
- 16.Gandey A. U.S. slams Canada over new drug injection site. CMAJ 2003;169: 1063. [PMC free article] [PubMed] [Google Scholar]
- 17.Hedrich D. European report on drug consumption rooms. Lisbon: European Monitoring Centre for Drugs and Drug Addiction, 2004.
- 18.Wood E, Tyndall MW, Spittal PM, Li K, Kerr T, Hogg RS, et al. Unsafe injection practices in a cohort of injection drug users in Vancouver: could safer injecting rooms help? CMAJ 2001;165: 405-10. [PMC free article] [PubMed] [Google Scholar]
- 19.Hedlund J. Risky business: safety regulations, risk compensation, and individual behavior. Inj Prev 2000;6: 82-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martinuk S. Safe-injection sites won't work. Province 2002. Nov 20: 20.
- 21.Tyndall MW, Craib KJ, Currie S, Li K, O'Shaughnessy MV, Schechter MT. Impact of HIV infection on mortality in a cohort of injection drug users. J Acquir Immune Defic Syndr 2001;28: 351-7. [DOI] [PubMed] [Google Scholar]
- 22.Mensch BS, Kandel DB. Underreporting of substance use in a national longitudinal youth cohort, individual and interviewer effects. Public Opin Q 1988;52: 100-24. [Google Scholar]