Abstract
Background
Ataxic hemiparesis is a classic lacunar syndrome that most often localizes to the pons.
Results
We report 3 patients who presented with left-sided ataxic hemiparesis and were found on imaging to have small right frontal subcortical white matter infarcts in similar locations by diffusion-weighted MRI. [99mTc]hexamethylpropylenamine oxime single-photon emission computed tomography (SPECT) scans in all 3 patients showed decreased metabolism in the contralateral cerebellar hemisphere, indicative of crossed cerebellar diaschisis (CCD).
Conclusion
CCD is under-recognized in ataxic hemiparesis and may have implications for functional recovery after this type of ischemic stroke.
Keywords: ataxia, lacunar infarction, magnetic resonance imaging, tomography, emission computed, stroke
Results
Case 1
A 62-year-old right-handed man with a history of hypertension, type 2 diabetes mellitus, and hypercholesterolemia presented with sudden onset of left-sided weakness and clumsiness of the arm and leg. There was no history of atrial fibrillation, no history of previous stroke, and no family history of stroke. On examination, power was 4 out of 5 in the left arm and leg on the Medical Research Council scale and a mild left-sided upper-motor neuron facial paresis. There was only subtly decreased sensation on the left side of the body compared with the right. The reflexes were brisk on the left side, and there was an extensor plantar response on the left. He had left-sided dysmetria, dysdiadochokinesis, and marked end point tremor out of proportion to his weakness. MRI showed a small acute infarct in the right periventricular posterior frontal white matter on diffusion-weighted imaging (DWI). There was no abnormality of the cerebellum or brain stem on MRI. A brain SPECT scan on day 3 demonstrated hypoperfusion of the left cerebellar hemisphere (Figure, case 1), consistent with the phenomenon of crossed cerebellar diaschisis (CCD). Ultrasonographic evaluation of the heart and cervical vessels revealed no source of emboli, confirming the lacunar/small vessel stroke subtype in this patient. The National Institutes of Health Stroke Scale (NIHSS) score on admission was 4, and the modified Rankin Scale (mRS) on discharge was 3.
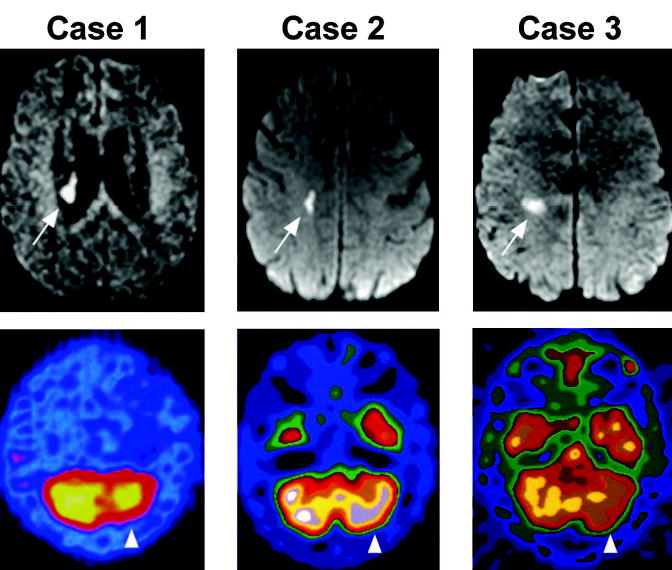
DWI (black and white panels) and [99mTc]hexamethylpropylenamine oxime SPECT (color panels) from each of the 3 cases (case 1 to case 3). Arrows indicate the region of the infarct detected by DWI, and arrowheads indicate the area of hypoperfusion detected by SPECT. The calculated asymmetry index (affected cerebellar hemisphere SPECT intensity/unaffected cerebellar hemisphere SPECT intensity ×100) was 51.5% in Case 1, 84.8% in Case 2, and 48.7% in Case 3.
Case 2
A 72-year-old right-handed man presented with sudden onset of left-sided clumsiness and gait ataxia. On examination, he had mild left pronator drift but no weakness on confrontation. The sensory examination and reflexes were normal. Coordination testing showed mild left-sided dysmetria, dysdiadochokinesis, and end point tremor. Brain MRI demonstrated a very small right subcortical white matter acute infarct on DWI, with no MRI abnormalities in the cerebellum or brain stem. A brain SPECT scan done on day 3 showed subtle hypoperfusion of the left cerebellar hemisphere that was consistent with his subtle ataxia. Ultrasonographic evaluation of the heart and cervical vessels revealed no source of emboli. The NIHSS score on admission was 3, and the mRS on discharge was 1.
Case 3
A 49-year-old right-handed man awoke with left arm and leg weakness and left-sided clumsiness and gait imbalance. On examination, he had a left pronator drift, decreased fine motor movements with the left hand, and mild (four fifths) weakness of the proximal left leg. The sensory examination and reflexes were normal. There was profound left-sided dysmetria, dysdiadochokinesis, failure of checking, and end point tremor, with veering to the left on attempted ambulation. Brain MRI showed a small right subcortical white matter infarct on DWI, with no abnormalities in the cerebellum or brain stem. Brain SPECT done on day 4 showed hypoperfusion of the left cerebellar hemisphere. As with the first 2 cases, ultrasonographic evaluation of the heart and cervical vessels revealed no source of emboli. The NIHSS score on admission was 3, and the mRS on discharge was 2.
Discussion
Ataxic hemiparesis (AH) is one of the classic lacunar syndromes. The “lacunar hypothesis” is fulfilled for AH, in that the majority of cases are caused by lacunar (small vessel) infarction.1 Small vessel infarctions producing AH are reported most commonly in the pons or the internal capsule/corona radiata. In one series of AH, 40% of patients had infarcts in the internal capsule or corona radiata, 31% had infarcts in the pons, 14% had infarcts in the basal ganglia, 11% had infarcts in thalamus, and 3% had infarcts in other brain stem locations.1 In another large series of AH, the infarct localizations were similar (43% pons, 13% internal capsule only, 33% thalamocapsular, and 10% striatocapsular).2 In another series, the most common infarct locations were internal capsule, pons, and corona radiata.3 The corona radiata localization of the lacunar infarcts seen in our 3 cases is thus not an uncommon cause of AH. Any of the common infarct locations that cause AH may affect the corticopontocerebellar or dentatorubralthalamocortical pathways to cause ataxia, but explicit demonstration of a resultant crossed cerebellar diaschisis (CCD) in such lacunar infarcts has not, to our knowledge, been reported.
CCD is thought to result from deafferentation of the affected cerebellar hemisphere attributable to contralateral interruption of corticopontocerebellar fibers. The hemispheric locations most likely to cause CCD after infarction appear to include the postcentral and supramarginal areas,4 but it is unknown how small of a cortical or subcortical infarct might give rise to the phenomenon of CCD.
CCD is most often reported in association with large cerebral hemispheric infarcts.5–7 Most series have reported patients with dense hemiparesis, thus preventing assessment for ipsilateral hemiataxia. However, in some cases with milder hemispheric strokes, ipsilateral ataxia has been reported.8
The 3 cases of AH presented here show that a small stroke in the right subcortical white matter can be sufficient to cause CCD. It is likely that the infarcts in these patients involved the corticopontocerebellar projections but had only a minimal effect on the descending corticospinal tract, thus producing hemiataxia out of proportion to hemiparesis.
The degree of CCD may provide useful information about potential for recovery.5 Further studies are needed to clarify the relationship between small vessel strokes, diaschesis, and recovery potential.
References
- 1.Gan R, Sacco RL, Kargman DE, Roberts JK, Boden-Albala B, Gu Q. Testing the validity of the lacunar hypothesis: the Northern Manhattan Stroke Study experience. Neurology. 1997;48:1204–1211. doi: 10.1212/wnl.48.5.1204. [DOI] [PubMed] [Google Scholar]
- 2.Gorman MJ, Dafer R, Levine SR. Ataxic hemiparesis: critical appraisal of a lacunar syndrome. Stroke. 1998;29:2549–2555. doi: 10.1161/01.str.29.12.2549. [DOI] [PubMed] [Google Scholar]
- 3.Arboix A. Clinical study of 23 patients with ataxic hemiparesis. Med Clin (Barc) 2004;122:342–344. doi: 10.1016/s0025-7753(04)74229-3. [DOI] [PubMed] [Google Scholar]
- 4.Komaba Y, Mishina M, Utsumi K, Katayama Y, Kobayashi S, Mori O. Crossed cerebellar diaschisis in patients with cortical infarction: logistic regression analysis to control for confounding effects. Stroke. 2004;35:472–476. doi: 10.1161/01.STR.0000109771.56160.F5. [DOI] [PubMed] [Google Scholar]
- 5.Infeld B, Davis SM, Lichtenstein M, Mitchell PJ, Hopper JL. Crossed cerebellar diaschisis and brain recovery after stroke. Stroke. 1995;26:90–95. doi: 10.1161/01.str.26.1.90. [DOI] [PubMed] [Google Scholar]
- 6.Miyazawa N, Toyama K, Arbab AS, Koizumi K, Arai T, Nukui H. Evaluation of crossed cerebellar diaschisis in 30 patients with major cerebral artery occlusion by means of quantitative i-123 imp SPECT. Ann Nucl Med. 2001;15:513–519. doi: 10.1007/BF02988504. [DOI] [PubMed] [Google Scholar]
- 7.Srinivasan A, Miller W, Stys P, Goyal M. Crossed cerebellar diaschisis in stroke. Neurology. 2004;62:2130. doi: 10.1212/01.wnl.0000123088.81455.f2. [DOI] [PubMed] [Google Scholar]
- 8.Tanaka M, Kondo S, Hirai S, Ishiguro K, Ishihara T, Morimatsu M. Crossed cerebellar diaschisis accompanied by hemiataxia: a PET study. J Neurol Neurosurg Psychiatry. 1992;55:121–125. doi: 10.1136/jnnp.55.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]


