Abstract
Background
Most studies applying the adult-derived ‘expressed emotion’ (EE) measure to children have combined criticism (CRIT) and emotional overinvolvement (EOI). Yet, some of the parent behaviors coded as EOI and shown to have negative implications for parents and their adult children (e.g., multiple positive comments about the son or daughter) may be normative and benign for parents and their juvenile children. Thus, EOI, as currently operationalized, may not be related to child psychopathology in the way CRIT is.
Method
We tested this possibility, separating CRIT and EOI and examining the individual scoring criteria for each in relation to psychopathology factors in a sample of 258 clinically-referred children aged 7–17.
Results
Whereas each of the four CRIT criteria related positively to maternal reports of child psychopathology, especially externalizing problems, only two of the five EOI criteria were positively related to child psychopathology, and one (positive comments) was negatively related. Structural Equation Modeling findings supported a model in which CRIT partially mediates the relation between maternal psychopathology and child externalizing symptoms.
Conclusions
Overall, the results suggest that EE may contribute to the study of parent–child relations and child psychopathology, but that a developmental adjustment may be required in the way EE is operationalized for use with juvenile samples.
Keywords: Assessment, expressed emotion, parent-child
Abbreviations: EE: expressed emotion, CRIT: criticism, EOI: emotional overinvolvement, FMSS: five-minute speech sample
Although studying parental attitudes and behavior appears to be important in expanding our knowledge about child psychopathology, some of the most widely used measures have limitations that constrain their feasibility and information value. Most research in this area involves either self-report data or coded parent–child observations. Self-report data can be problematic in that parents and children may have difficulty providing objective descriptions of their attitudes and behavior. Observational coding requires fewer inferences and may thus provide more objective data, but it requires effort and resources that are usually not feasible for clinical use, may entail demand characteristics regarding the way parents and children interact while being taped or watched by observers, and typically involves brief samples of behavior that may not be fully representative of day-to-day interactions. A few recent studies have employed a different approach to assessment that may address some of these limitations.
This approach, which grows out of a rich tradition in adult psychopathology research, involves assessment of expressed emotion (EE). The initial basis for EE research was the finding that adult schizophrenic patients from families characterized by high levels of emotional involvement, hostility, or criticism – later collectively labeled ‘EE’ – were significantly more likely to relapse than their counterparts from families low on these characteristics (Brown, Monek, Carstairs, & Wing, 1962). Many studies have since replicated the results for schizophrenic patients, finding a robust association between the level of EE expressed by close relatives and patient relapse (Brown, Birley, & Wing, 1972). In a recent meta-analysis of 27 studies, the estimated mean r for the association between EE and outcome for schizophrenic adults was .31 (Butzlaff & Hooley, 1998), falling into what Cohen (1988) classified as the ‘medium’ range in strength of association. EE has also been used to characterize the attitudes of family members toward relatives suffering from other disorders in adulthood – including depression, bipolar disorder, anorexia nervosa, obsessive-compulsive disorder, post-traumatic stress disorder, agoraphobia, obesity, Alzheimer’s disease, and alcoholism (Chambless & Stekette, 1999; Hooley, Orley, & Teasdale, 1986; O’Farrell, Hooley, Fals-Stewart, & Cutter, 1998; Tarrier, Sommerfield, & Pilgrim, 1999; van Furth et al., 1996; Wagner, Logsdon, Pearson, & Teri, 1997), and appears to be a general predictor of poor outcome across a range of psychological conditions in multiple cultures.
Although the relation between parental characteristics and child psychopathology has been a focus of research for some time, the EE measure has only begun to be used with juvenile populations in the past decade. Studies examining the relation between child psychopathology and parental EE cross-sectionally have found higher rates of EE among parents of children with depression (Asarnow, Tompson, Hamilton, Goldstein, & Guthrie, 1994; Schwartz, Dorer, Beardslee, Lavori, & Keller, 1990), disruptive behavior disorders (Hibbs et al., 1991), obsessive-compulsive disorder (Hibbs et al., 1991), overall behavior problems (Baker, Heller, & Henker, 2000), disorganized attachments (Jacobsen, Hibbs, & Ziegenhain, 2000), conduct disorder (Schwartz et al., 1990), and substance abuse (Schwartz et al., 1990). High EE has also been associated with poor metabolic control in diabetic youth (Liakopoulou et al., 2001). In longitudinal studies, high parental EE has been associated with the persistence of children’s mood disorders (Asarnow, Goldstein, Tompson, & Guthrie, 1993), and risk for poorer social-emotional functioning (Seifer, Sameroff, Baldwin, & Baldwin, 1992).
A widely used approach to assessing EE is administration of a Five Minute Speech Sample (FMSS), in which parents are asked to describe their child and their relationship with the child. The FMSS measure comprises two distinct components – criticism (CRIT) and emotional overinvolvement (EOI). High criticism is scored when the first statement is negative, the parent describes a negative relationship with the child, or the parent criticizes the child. Expressing dissatisfaction with the child prompts a borderline critical rating. The EOI component is based on more diverse criteria: 1) crying during the speech sample (an emotional display), 2) expressing very strong feelings of love or willingness to do anything for the child (referred to as a statement of attitude), 3) displaying overprotective or self-sacrificing behavior, 4) giving excessive detail about the child’s birth or infancy, or 5) providing five or more positive remarks about the child (Magana-Amato, 1993).
These criteria were derived empirically from research on adult schizophrenic patients, and have since been directly extended downward for use with younger children, with no concomitant adjustment in administration, scoring, or interpretation. It is possible, though, that the criteria may not be associated with risk or dysfunction in quite the same way for children as for adults with psychiatric disorders. In particular, it appears that some of the parental attitudes indexed by EOI may have negative implications in relation to parents and their adult children, but may be more developmentally appropriate for parents and their juvenile children, who are dependent and need their parents’ emotional support (for a similar perspective, see Wamboldt, O’Connor, Wamboldt, Gavin, & Klinnert, 2000). For example, for parents of children or adolescents, recounting details about the youngster’s birth or infancy, and praising his or her good qualities may be rather normative, and in any event may not necessarily signal a pathological parent attitude or significant problems in the parent–child relationship. By contrast, elements of the CRIT component do seem more likely to indicate a problematic parental attitude or parent–child relationship, regardless of whether the parental comments refer to a child or an adult.
According to this reasoning, understanding the relation between EE and psychopathology in juvenile samples may require separating the two EE components, EOI and CRIT, and examining their scoring criteria more carefully. Most previous studies with young children have followed the tradition established in the use of EE with parents and their adult children, which involves aggregating the two components into an overall EE index. A few studies have separated CRIT and EOI, and findings of these studies do suggest that the two components may have different patterns of association with child psychopathology. High levels of criticism have rather consistently been correlated with disruptive behavior or conduct disorder (Baker et al., 2000; Nelson, 2001; Peris & Baker, 2000; Stubbe, Zahner, Goldstein, & Leckman, 1993; Vostanis, Nicholls, & Harrington, 1994). A recent study also found high maternal criticism to be related to child depression (Asarnow, Tompson, Woo, & Cantwell, 2001). High EOI, on the other hand, has been associated with children’s internalizing problems and disorders (Stubbe et al., 1993); although it was not more prevalent among mothers of children with depression in a different study (Asarnow et al., 2001). These studies have generally not assessed the specific criteria that comprise the two components, nor have they evaluated the psychometric properties of CRIT or EOI. Thus, while EE based on the five-minute speech sample is being used increasingly to study child and adolescent psychopathology, we lack some rather basic information about the measure and its two components.
Published literature does provide a few clues as to what a psychometric assessment focused on EE in relation to minors might show. For example, the number of positive remarks made about a child, one of the EOI scoring criteria, has been found to be more common among mothers of normal children than mothers of psychiatrically-disturbed children using the Camberwell Family Interview (Vostanis et al., 1994), and associated with improvement, rather than decline, in social-emotional functioning over time (Seifer et al., 1992). And another study found that mothers of a community (non-clinical) sample of children generated an average of 5.3 positive comments about their child during the FMSS (Wamboldt et al., 2000); this contrasts with the view that parental EOI is a risk factor for psychopathology, since one of its indicators may in fact be normative.
Another element missing in previous research with children, but potentially important in efforts to properly interpret EE, is maternal psychopathology. Because EE assessment is usually based on mothers’ statements about their children, the mothers’ own adjustment and psychological functioning may be very relevant to an understanding of their expressed attitudes. One might expect that in addition to a direct association between maternal psychopathology and child psychopathology, mothers’ own symptoms may impinge on their views about their child and their relationship with the child, and thus on their statements during EE assessment. Indeed, mothers with a history of depression have been found to express more negative attitudes about their children (Goodman, Adamson, Riniti, & Cole, 1994), and one study found parental psychiatric diagnosis to be a significant predictor of high EE (Hibbs et al., 1991). The findings suggest that the relation of parental psychiatric functioning to CRIT and EOI, considered separately, requires investigation.
Given our developmental concerns noted earlier, and the hints in previous literature, we sought to understand the relations between these potentially distinct maternal attitudes – EOI and CRIT – and child psychopathology in the context of maternal psychopathology. Since the bulk of research using EE with children refers to a broad array of psychiatric problems, we used a diverse clinical sample that included children with internalizing, externalizing, and comorbid types of problems. We began with analyses at the level of each scoring criterion, to assess cross-sectional relations with psychopathology in this sample. Then we used structural equation modeling to test a comprehensive model of the relations among CRIT and maternal and child psychopathology.
The study had certain distinctive features, designed to maximize its contribution. It used the largest clinical sample yet employed in any study of EE and child psychopathology; it was the only study to separate CRIT from EOI at both a component and an individual criteria level; and it was the only study to test a mediating model that included the role of maternal psychopathology.
Method
Participants and procedure
Participants were 165 boys and 93 girls and their mothers. All the children had been referred to one of nine participating outpatient community mental health clinics. Child ages ranged from 7–17 (M = 11.34, SD = 2.56). Mean scores on the Child Behavior Checklist (see below) placed the children at the 93rd percentile of the population on internalizing problems (e.g., anxiety and depression) and at the 96th percentile on externalizing problems (e.g., aggression, delinquency), and the mean number of DSM-III-R diagnoses1 (see procedure below) was 2.5. The sample was ethnically diverse, with 50.4% Caucasian, 11.6% African-American, 17.6% Hispanic/Latino, 1.6% Asian American, and 18.8% multiethnic children. Most of the families were lower-to middle-income, with 43% of the sample having a family income below $15,000, 44% between $15,000 and $45,000, and 12% earning over $45,000 in the past year. Families who agreed to participate were interviewed near the time of clinic intake. The interview involved multiple measures, with child measures and parent measures administered by different interviewers in separate rooms.
Measures
The Diagnostic Interview Schedule for Children (DISC 2.3; Shaffer, Fisher, Dulcan & Davies, 1996; Schwab-Stone et al., 1996).
The DISC interview was chosen because it generates a relatively complete array of DSM-III-R symptom counts and diagnoses, and has somewhat better documented reliability and validity than do other diagnostic interviews (Edelbrock & Costello, 1988; Shaffer et al., 1996; Schwab-Stone et al., 1996). Parents and children were administered the interview separately, with parents receiving the full DISC and children receiving the sections on mood disorders, conduct disorder, and substance use disorders.
Youth Self-Report Form of the Child Behavior Checklist (YSR; Achenbach, 1991a).
The YSR is a 112-item checklist which children rate on a three-point scale as items are read to them. The YSR generates raw and T-scores for total problems, internalizing, externalizing, and narrow-band scores on 8 syndromes (e.g., withdrawn, delinquent, social problems). Evidence on the reliability and validity of these scores is extensive for children aged 11–18. We used the YSR with children under age 11 in this study, as previous analyses suggested that test–retest reliability coefficients and internal consistencies were very similar for 7–10-year-olds and children over age 10 in this sample (see Yeh & Weisz, 2001).
The Child Behavior Checklist (CBCL; Achenbach, 1991b).
The CBCL is a widely used, standardized parent-report measure that lists 118 child behavior problems for parents to rate as not true, somewhat/sometimes true, or very/often true. The CBCL generates the same narrowband and broadband scores as the YSR, and has excellent reliability and validity (as summarized in Achenbach, 1991b).
The Five Minute Speech Sample (Magana et al., 1986).
The FMSS is derived from responses made by the mother when prompted to give her thoughts and feelings about her child. The FMSS has been shown to have concurrent validity with ratings made during a semistructured interview measuring affective attitudes (Camberwell Family Interview, Leeb et al., 1991; Magana et al., 1986; Malla, Kazarian, Barnes, & Cole, 1991). It has demonstrated significant stability over a three- to five-week time period (Leeb et al., 1991; McGuire & Earls, 1994), and is predictive of psychiatric risk in adult samples (Vaughn & Leff, 1976) and of relapse for depressed children (Asarnow et al., 1993). Most studies of expressed emotion using juvenile populations have used the FMSS (e.g., Asarnow et al., 1993, 1994; Baker et al., 2000; Hibbs et al., 1991; Hirshfeld, Biederman, Brody, & Faraone, 1997; Marshall, Longwell, Goldstein, & Swanson, 1990; Stubbe et al., 1993; Wamboldt et al., 2000).
Coding of Speech Samples.
The FMSS tapes were coded according to Magana-Amato’s (1993) manual, using both content and tone to score each tape. Along both CRIT and EOI, mothers are rated as high, borderline or low. To evaluate whether the rates of maternal EE were similar for boys and girls and for different age groups, separate base rate comparisons were conducted in which the subjects were divided based on their membership in the given groups, with gender and age tested as factors in a chi-square test of independence. Neither of these analyses suggested significant differences.
The CRIT code comprises four criteria: initial statement (scored as positive, neutral, or negative), relationship with the child (scored as positive, neutral, or negative), criticism (scored as a frequency count of critical statements), and dissatisfaction (scored dichotomously as present or absent). The EOI score comprises five criteria: emotional display (scored as present or absent), statements of attitude (scored as a frequency count), self-sacrificing/overprotective behavior (scored as present or absent), excessive detail (scored as present or absent), and positive remarks (scored as a frequency count, and considered ‘excessive’ if more than five positive remarks are made). The original developer of the measure and the coding system coded all speech samples, blind to the child’s identity, adjustment, and diagnosis. The first author of this study independently coded a random subset of 47 of the tapes, achieving a weighted kappa reliability of .72 for EOI and .68 for CRIT, both of which are considered ‘substantial’ (Landis & Koch, 1977).
Brief Symptom Inventory (BSI; Derogatis, 1992).
The BSI is a 53-item self-report symptom inventory designed to reflect psychological symptom patterns in adults. The BSI is scored and profiled in terms of nine symptom dimensions and three global indices of distress. This measure has shown impressive convergent validity with Minnesota Multiphasic Personality Inventory scales, has good internal consistency (with alphas ranging from .71 to .85 for the various scales), and appears to give consistent measurement across time, with an overall test–retest stability of .90 (Derogatis, 1992). The total score on the BSI was used as a measure of maternal psychopathology.
Analytic plan
The main purpose of the study was to investigate EOI and CRIT, the two components of expressed emotion as measured by the FMSS, in relation to important variables in the study of child psychopathology. We began by assessing which constructs of child psychopathology should be a focus of our analyses; this was done by conducting a factor analysis to assess the factor structure of child psychopathology within this sample. Then, to clarify the roles of the EOI and CRIT components, the individual criteria comprising EOI and CRIT were examined for their relation to the factors of child psychopathology and to one another. Based on the inconsistency that was evident across the EOI items (see below), further analyses with this composite were deemed inappropriate. Thus, in our final wave of analyses, we tested two models for the relation of CRIT to child psychopathology and maternal psychopathology, looking at mother-reported internalizing and externalizing problems separately.
Results
Derivation of child psychopathology constructs
A factor analysis was conducted on the measures of child psychopathology, using symptom counts from various modules of the DISC and broadband syndrome scores from the YSR and CBCL to create subtypes of child psychopathology. The principal factors procedure was chosen because it is widely understood, and it conforms to the factor analytic model in which common variance is analyzed with unique and error variance removed (Tabachnick & Fidell, 1996). An oblique rotation (direct oblimin) was used because it was expected that the factors would be correlated with one another.
Three factors were extracted from the analysis, using a combination of the Kaiser criterion, a screen test, and interpretabililty criteria: 1) mother-reported externalizing (eigenvalue of 3.35), 2) child-reported problems (2.14), and 3) mother-reported internalizing (1.55). Together, these three factors explained 70% of the variance of the measures. The solution (factor pattern matrix) generated by factor analysis is presented in Table 1. The contributions of different informants were preserved separately in subsequent analyses involving the three factors because (a) child and mother reports separated empirically, forming different factors, and measurement models that attempted to combine the two fit the data poorly (e.g., Comparative Fit Index = .78), due largely to low inter-informant correlations, and (b) previous research with clinic samples has suggested that different informants provide different information about functioning (e.g., Achenbach, McConaughy, & Howell, 1987; Coie & Dodge, 1988).
Table 1.
Factor pattern matrix (principal axis solution)
| Mother-externalizing | Child problems | Mother-internalizing | |
|---|---|---|---|
| Externalizing (CBCL) | .873 | .083 | .385 |
| Oppositional defiant symptoms (DISC-P) | .768 | .009 | .296 |
| Conduct disorder symptoms (DISC-P) | .645 | .170 | .169 |
| Externalizing (YSR) | .436 | .791 | −.070 |
| Internalizing (YSR) | .063 | .736 | .159 |
| Major depression symptoms (DISC-C) | −.057 | .642 | .072 |
| Conduct disorder symptoms (DISC-C) | .338 | .488 | −.193 |
| Internalizing (CBCL) | .405 | .121 | .790 |
| Anxiety symptoms (DISC-P) | .144 | .010 | .770 |
| Major depression symptoms (DISC-P) | .322 | .132 | .708 |
NOTE: Child Behavior Checklist (CBCL), Youth Self-Report (YSR), Diagnostic Interview Schedule for Children (DISC) – Parent/Child.
Analyses of individual criteria
First, to test the concurrent validity of the specific criteria that comprise CRIT and EOI (listed in Table 2), each of the criteria (e.g., number of positive statements, dissatisfaction) was regressed upon each of the three latent factors of child psychopathology, using Weighted Least Squares estimates for criteria that were dichotomous or ordered polytomous variables and Robust Maximum-Likelihood estimates when the criteria were continuous variables. The coefficients and their significance levels are shown in Table 2.
Table 2.
Standardized beta weights regressing the EE criteria on the child psychopathology factors
| Child psychopathology factor
|
|||
|---|---|---|---|
| EE criteria | M-externalizing | Child problems | M-internalizing |
| CRIT criteria | |||
| Negative initial statement | .267** | −.031 | .049 |
| Negative relationship | .486** | −.053 | .193* |
| Number of criticisms | .217** | −.071 | −.001 |
| Dissatisfaction | .478** | −.034 | .177* |
| CRIT OVERALL | .436** | −.099 | .132 |
| EOI criteria | |||
| Emotional display | .274# | .262* | .393** |
| Statement of attitude | .016 | .035 | .075 |
| Overprotection | .113 | .376* | .124 |
| Excessive detail | .064 | −.180 | −.230 |
| Positive remarks | −.329** | −.214** | −.177** |
| EOI OVERALL | −.123 | −.064 | −.010 |
NOTE: CRIT refers to the critical component of EE; whereas EOI refers to emotional overinvolvement. For all nominal variables, positive path coefficients indicate the presence of the EE criteria is associated with higher levels of child psychopathology, as defined by the particular factor.
p < .06,
p < .05,
p < .01.
Generally, the largest coefficients were between the CRIT criteria and mothers’ reports of externalizing behavior. Each of the criterion variables that compose critical EE was significantly associated with mothers’ reports of externalizing problems at the p < .01 level. Mothers’ descriptions of negative relationships and statements of dissatisfaction with their children were also significantly related to maternal reports of internalizing problems. None of the CRIT criteria was associated with children’s reports of their own behavior problems.
The EOI criteria, by contrast, showed much less consistency in the presence and direction of their associations with the child psychopathology factors. For example, the number of positive remarks made by the mother during the FMSS was negatively related to all three indices of child psychopathology, whereas maternal emotional displays were positively related to mothers’ reports of internalizing problems and children’s reports of problems. Maternal overprotection was positively associated with children’s reports of their own problems, but not maternal report of child internalizing or externalizing problems. The other two EOI criteria, statements of attitude and excessive detail were not significantly related to any of the three psychopathology factors.
The pattern of associations shown in Table 2 raised questions about whether the individual criteria for EOI were actually closely related to one another. To follow up, we examined the internal consistency of both the EOI and CRIT components, using Cronbach’s alpha coefficient. With the full sample of 258 cases, the coefficient for the four CRIT criteria was .59, suggesting acceptable cohesiveness among items. By contrast, alpha for the five EOI criteria was poor (−.01), suggesting a lack of internal consistency.
Model testing approach
A conceptual model of the relations between affective attitudes and various components of child psychopathology was evaluated using Structural Equation Modeling (SEM) with the M-Plus Program (Muthén & Muthén, 1998). Using SEM to analyze these data is the preferred technique insofar as it has the capacity to describe indirect effects (mediators), and can decrease the amount of error associated with specific instruments through multi-measured latent variables. All parameter estimates were based on a weighted least squares approach, using a diagonal weight matrix with robust standard errors. Mean and variance-adjusted chi-square test statistics are also provided. Robust z-statistics, based upon corrected standard errors, were used to assess parameter significance, as they are more trustworthy than ordinary z-statistics for non-continuous variables (Chou, Bentler, & Satorra, 1991).
Models were evaluated both by Satorra-Bentler chi-square tests of significance, and by their corresponding Comparative Fit Indexes (CFI) and Root Mean Square Error of Approximation (RMSEA). Values of the CFI range from zero to 1.00 and are derived from the comparison of the hypothesized model with the null model (Bentler, 1990); it has been suggested that values greater than .95 indicate acceptable fit to the data (Hu & Bentler, 1998, 1999). RMSEA compares the fit of the estimated model to a hypothetical perfect model with values close to .06 accepted as indicating good model fit (Hu & Bentler, 1999). In SEM, the chi-square statistic is truly a ‘badness-of-fit’ index; therefore, high p-values and low chi-square values are indicators of good model fit. The structural models were run using the 204 mother–child dyads for whom we had complete data.
EE, child psychopathology, and maternal psychopathology
Given the extant literature demonstrating that maternal psychopathology is a risk factor for children, it was hypothesized that maternal psychopathology would be a significant predictor of mothers’ reports of child internalizing and child externalizing symptoms, and that these relations would be partially mediated through mothers’ affective attitudes. Due to the lack of conceptual and psychometric integrity of EOI, analytic models including the EOI component were seen as inappropriate. As an initial step in the process of analyzing the proposed models, bivariate correlations between pairs of variables were examined. Table 3 presents the correlations and variances for the variables used in the model, upon which analyses are based.
Table 3.
Correlation matrix (with standard deviations on the diagonal)
| Variable | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | Mean |
|---|---|---|---|---|---|---|---|---|---|
| Externalizing (CBCL) | 11.55 | 22.52 | |||||||
| (2) Oppositional (DISC-P) | .760** | 8.66 | 13.91 | ||||||
| Conduct (DISC-P) | .582** | .487** | 2.58 | 2.77 | |||||
| CRIT EE | .415** | .363** | .224** | .90 | 1.81 | ||||
| (5) Internalizing (CBCL) | .522** | .314** | .195** | .141* | 8.32 | 15.96 | |||
| (6) Depression (DISC-P) | .321** | .245** | .249** | .092 | .603** | 5.51 | 9.15 | ||
| (7) Anxiety (DISC-P) | .209** | .184** | .074 | .039 | .581** | .552** | 16.04 | 23.14 | |
| (8) Mat. psychopathology | 381** | .205** | .114 | .196** | .500** | .332** | .353** | 31.98 | 39.01 |
p < .05,
p < .01.
The first model we tested allowed for parameter estimates to be made from maternal criticism to maternal reports of externalizing problems. Maternal psychopathology, as measured by the total score on the BSI, was used as a predictor of both child externalizing problems and mothers’ CRIT. This externalizing model showed a good fit with the data, χ2 (4, n = 204) = 6.74, p = .15, CFI = .995, RMSEA = .058. Standardized path coefficients between variables are given in Figure 1. In the model, maternal psychopathology was found to be positively related to maternal report of child externalizing problems. Moreover, maternal psychopathology predicted maternal critical EE, which in turn predicted maternal report of child externalizing problems. In other words, mothers with more psychological symptoms themselves tended to have more critical attitudes about their children and to perceive more externalizing problems for their children. Together, maternal psychopathology and maternal criticism accounted for about 30 percent of the variance in mother-reported externalizing problems.
Figure 1.
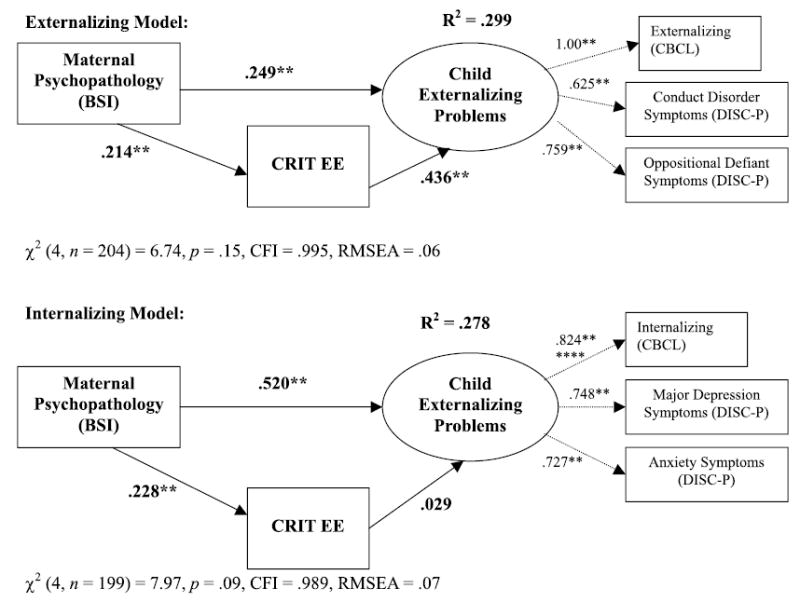
Standardized solution for the Externalizing and Internalizing Models. Coefficients are standardized path coefficients. Dashed lines represent indicators of latent variables. CBCL = Child Behavior Checklist; DISC-P = Diagnostic Interview Schedule for Children – Parent Report. **p < .01.
A similar model was generated to test maternal CRIT as a mediator of maternal psychopathology and mother-reported child internalizing symptoms, and is also depicted in Figure 1. Although the overall model showed a good fit with the data, χ2 (4, n = 199) = 7.97, p = .09, CFI = .989, RMSEA = .070, the small and insignificant path coefficient between maternal CRIT and child internalizing problems suggested that mothers who score higher on CRIT did not report more internalizing problems in their children. Path coefficients (standardized beta weights) can be interpreted both in terms of their significance and magnitude; thus, the relationship between maternal critical EE and mothers’ reports of internalizing problems is very weak in comparison to the relationship between maternal critical EE and mothers’ reports of externalizing problems in the previous model. The internalizing model shows a very strong relationship between maternal psychopathology and child internalizing problems, as well as a substantial relation between maternal psychopathology and CRIT. For completeness, a comprehensive model including a path from EOI to internalizing problems was also run; but, as anticipated, model fit was worse with the inclusion of this measure.
Discussion
This study examined the relation between the EE components, as measured by the FMSS, and both maternal and child psychopathology. The pattern of correlations between the EE criteria and the factors of child psychopathology suggested that the adult-derived EE criteria are quite diverse, with some items related to child externalizing problems, some items related more broadly to child psychopathology, and some items actually unrelated to child psychopathology. The CRIT component appeared to be mainly associated with externalizing problems. In addition to the CRIT summary score, each of the individual scoring criteria for critical EE (negative initial statement, negative relationship, critical comments, and dissatisfaction) was positively related to mothers’ reports of their children’s externalizing behavior. These criteria were also associated with one another, forming a coherent scale, unlike the criteria for EOI.
Consonant with the findings of Seifer et al. (1992), statistically significant relationships were found more frequently between maternal reports and EE measures than between child reports and EE measures. Taken together, these results suggest that mothers’ critical EE is likely to be related to how disruptive and difficult to manage they perceive their children to be, although the causal direction of this relationship cannot be determined from the present study.
Only two of the EOI criteria were positively associated with child psychopathology: 1) mother’s emotional display (crying) during the FMSS, which was related to more problems according to both parent and child informant, and 2) maternal over-protection, which was correlated with children’s report of their problems. The number of positive remarks the mother made about her child during the speech sample was associated with fewer externalizing problems, similar to findings reported by Wamboldt et al. (2000) and Kershner, Cohen, and Coyne (1996). The positive, not negative, valence of more positive remarks is also consonant with the model of EE tested by Chambless and her colleages (Chambless, Bryan, Aiken, Steketee, & Hooley, 1999). Using the Camberwell Family Interview along with observational and relative rating data, these researchers found evidence supporting a three-factor model of expressed emotion – CRIT, EOI, and Positivity. This third factor, Positivity, included the relative’s positive comments about the patient, which has historically been considered an indicator of EOI, and was strongly negatively related to CRIT. In a similar vein, the current study found that the number of positive remarks was related to the absence, rather than the presence of child psychopathology, which contradicts the traditional EE scoring method.
Our findings showed the EOI component of EE to be much less cohesive than the CRIT component. That is, the individual criteria within EOI did not predict child psychopathology in a consistent way and were not internally consistent. The lack of significant correlations between EOI and child psychopathology may indicate that several of the scoring criteria for EOI that have been adapted from parents of adult schizophrenic patients are not appropriate for parents of children and adolescents with emotional and behavioral problems. In particular, expressing love for the child, describing the child’s infancy, and making several positive remarks about the child may be more developmentally appropriate and less ‘pathological’ for parents of juvenile children as opposed to parents of adult children. Thus, the EOI construct may not be measurable with the same indicators for youth as are used with adults.
A recent study by Wamboldt and colleagues (2000) provides converging evidence on this topic, albeit from a different kind of sample than ours. The Wamboldt et al. data on asthmatic children and adolescents suggests that the indicators of emotional display and overprotection may be more valid indicators of EOI than are positive remarks and statements of attitude (Wamboldt et al., 2000). High EOI parents were divided into two subgroups: a) those scored as high EOI on the basis of the presence of a statement of attitude and more than five positive remarks, and b) those scored as high EOI on the basis of the other scoring criteria. Parents in group b reported family functioning problems in the areas of roles, affect responsiveness, and general functioning. Moreover, their parent–child interactions indicated more boundary problems. Yet, no differences were found in interactions for group a, who actually reported better family functioning in the areas of roles and affective involvement.
Our SEM results suggest that maternal attitudes are related to child psychopathology as reported by mothers. Whereas other studies (e.g., Asarnow et al., 2001) have suggested that maternal CRIT is specifically related to youth depression, we found that using a dimensional approach maternal critical attitudes were specifically associated with maternal reports of more child externalizing problems. The model also construes maternal criticism as a partial mediator between maternal psychopathology and maternal report of child externalizing behavior. Mothers who had more psychological symptoms themselves showed higher levels of criticism toward their children, and also had children whom they reported to have more externalizing problems. This work builds on other research finding that parental psychopathology is a determinant of EE in child samples (e.g., Hibbs et al., 1991), but also suggests that this relationship merits further exploration in adult samples.
It is intriguing to consider this pattern in light of Conrad and Hammen’s (1989) findings that depressed mothers were more critical of their children with internalizing or externalizing symptoms than were nondepressed mothers of symptomatic children. Conrad and Hammen suggested that depressed women may be less tolerant of dysfunction in their children. Similarly, the positive association we found between maternal psychopathology and maternal criticism suggests the possibility that, for mothers with their own psychological problems, child misbehavior may be especially salient. Alternatively, the results may indicate a perceptual bias on the part of some mothers; that is, some mothers may tend to be relatively negativistic, inclined to see and report problems in themselves and their children (Richters, 1992), particularly problems that are outwardly visible.
The cross-sectional nature of this study limits our capacity for causal inference. Nonetheless, this study adds substantially to the existing literature on the relation between parental characteristics and child psychopathology. Of all the studies assessing the relation between EE and child psychopathology, this study has the largest sample of clinical youth, is the only study to separate CRIT from EOI at both a component and an individual criteria level, and tests a mediating model of CRIT including the role of maternal psychopathology.
Our findings for CRIT are consistent with other evidence that CRIT is a negative indicator of the parent–child relationship related to child externalizing problems (Stubbe et al., 1993; Baker et al., 2000). But our findings for EOI suggest that this component of EE needs to be revised or reconstrued for use with juvenile samples. Novel approaches to the measurement of parental ‘over’ involvement should be considered, including the Wamboldt et al. (2000) revision that rules out EOI codes that are based solely on statements of attitude paired with five or more positive remarks. Authors of previous studies using global EE with youth may consider revisiting their results, attending separately to the EOI versus CRIT components as well as specific criteria codes. Further longitudinal research is necessary regarding the validity of parental EOI before it can continue to be used ‘as is’ with juvenile samples. More generally, this study reminds us that before measures from research derived with adults are applied to child samples, it is important to examine them from a developmental perspective, considering whether their meaning and implications may be different for children than adults, and exploring potential differences empirically.
Acknowledgments
Carolyn A. McCarty, Department of Psychology, UCLA. John R. Weisz, Departments of Psychology and Psychiatry and Biobehavioral Sciences, UCLA. The study was supported by a National Research Service Award F31 MH11845 [to Carolyn McCarty], and by NIMH grant R01 MH 49522 and Senior Research Scientist Award K05 MH01161 [both to John Weisz], which we gratefully acknowledge. We also wish to thank Joan Asarnow, Peter Bentler, Connie Hammen, and Barbara Henker, who provided thoughtful input and guidance on this study, and Eric Wu, for valuable statistical and technical consultation.
Footnotes
Data collection spanned the last years of DSM-III-R and some years of DSM-IV. For consistency, we used DSM-III-R diagnoses throughout the study. Studies of agreement across versions suggest that most DSM-III-R diagnoses and symptom counts are reasonably generalizable to DSM-IV (e.g., Biederman, Faraone, Weber, Rater, & Park, 1997; Kendall & Warman, 1996).
References
- Achenbach, T.M. (1991a). Manual for the Youth Self Report and 1991 Profile Burlington, VT: University of Vermont Department of Psychiatry.
- Achenbach, T.M. (1991b). Manual for the Child Behavior Checklist/4-18 and 1991 Profile Burlington, VT: University of Vermont Department of Psychiatry.
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101:213–232. [PubMed] [Google Scholar]
- Asarnow JR, Goldstein MJ, Tompson M, Guthrie D. One-year outcomes of depressive disorders in child psychiatric in-patients: Evaluation of the prognostic power of a brief measure of expressed emotion. Journal of Child Psychology and Psychiatry. 1993;34:129–137. doi: 10.1111/j.1469-7610.1993.tb00975.x. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Tompson M, Hamilton EB, Goldstein MJ, Guthrie D. Family-expressed emotion, childhood-onset depression and childhood-onset schizophrenia spectrum disorders: Is expressed emotion a nonspecific correlate of child psychopathology or a specific risk factor for depression? Journal of Abnormal Child Psychology. 1994;22:129–146. doi: 10.1007/BF02167896. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Tompson M, Woo S, Cantwell DP. Is expressed emotion a specific risk factor for depression or a nonspecific correlate of psychopathology? Journal of Abnormal Child Psychology. 2001;29:573–583. doi: 10.1023/a:1012237411007. [DOI] [PubMed] [Google Scholar]
- Baker BL, Heller TL, Henker B. Expressed emotion, parenting stress, and adjustment in mothers of young children with behavior problems. Journal of Child Psychology and Psychiatry. 2000;41:907–915. [PubMed] [Google Scholar]
- Bentler PM. Fit indexes, Lagrange multipliers, constraint changes, and incomplete data in structural models. Multivariate Behavioral Research. 1990;25:163–172. doi: 10.1207/s15327906mbr2502_3. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Weber W, Rater RL, Park K. Correspondence between DSM-III-R and DSM-IV attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1682–1687. doi: 10.1097/00004583-199712000-00016. [DOI] [PubMed] [Google Scholar]
- Brown GW, Birley JL, Wing JK. Influence of family life on the course of schizophrenic disorders: A replication. British Journal of Psychiatry. 1972;121:241–258. doi: 10.1192/bjp.121.3.241. [DOI] [PubMed] [Google Scholar]
- Brown GW, Monek EM, Carstairs GM, Wing JK. Influence of family life on the course of schizophrenic illness. British Journal of Preventative and Social Medicine. 1962;121:241–258. doi: 10.1192/bjp.121.3.241. [DOI] [PubMed] [Google Scholar]
- Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse. Archives of General Psychiatry. 1998;55:547–552. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Bryan AD, Aiken LS, Steketee G, Hooley JM. The structure of expressed emotion: A three-construct representation. Psychological Assessment. 1999;11:67–76. [Google Scholar]
- Chambless DL, Steketee G. Expressed emotion and behavior therapy outcome: A prospective study with obsessive-compulsive and agoraphobic outpatients. Journal of Consulting and Clinical Psychology. 1999;67:658–665. doi: 10.1037//0022-006x.67.5.658. [DOI] [PubMed] [Google Scholar]
- Chou CP, Bentler PM, Satorra A. Scaled test statistics and robust standard errors for nonnormal data in covariance structure analysis: A Monte Carlo study. British Journal of Mathematical and Statistical Psychology. 1991;44:347–357. doi: 10.1111/j.2044-8317.1991.tb00966.x. [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd edn). Hillsdale, NJ: Erlbaum.
- Coie JD, Dodge KA. Multiple sources of data on social behavior and social status in the school: A cross-age comparison. Child Development. 1998;59:815–829. doi: 10.1111/j.1467-8624.1988.tb03237.x. [DOI] [PubMed] [Google Scholar]
- Conrad M, Hammen C. Role of maternal depression in perceptions of child maladjustment. Journal of Consulting and Clinical Psychology. 1989;57:663–667. doi: 10.1037//0022-006x.57.5.663. [DOI] [PubMed] [Google Scholar]
- Derogatis, L.R. (1992). The Brief Symptom Inventory: Administration, Scoring, and Procedures Manual-II Baltimore: Clinical Psychometric Research Inc.
- Edelbrock, C.S., & Costello, A.J. (1988). Structured psychiatric interviews for children. In M. Rutter, A.H. Tuma, & I.S. Lann (Eds.), Assessment and diagnosis in child psychopathology (pp. 87–112). New York: Guilford Press.
- Goodman SH, Adamson LB, Riniti J, Cole S. Mothers’ expressed attitudes: Associations with maternal depression and children’s self-esteem and psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:1265–1274. doi: 10.1097/00004583-199411000-00007. [DOI] [PubMed] [Google Scholar]
- Hibbs ED, Hamburger SD, Lenane M, Rapoport JL, Kruesi MJP, Keysor CS, Goldstein MJ. Determinants of expressed emotion in families of disturbed and normal children. Journal of Child Psychology and Psychiatry. 1991;32:757–770. doi: 10.1111/j.1469-7610.1991.tb01900.x. [DOI] [PubMed] [Google Scholar]
- Hirshfeld DR, Biederman J, Brody L, Faraone SV. Associations between expressed emotion and child behavioral inhibition and psychopathology: A pilot study. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:205–213. doi: 10.1097/00004583-199702000-00011. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Orley J, Teasdale JD. Levels of expressed emotion and relapse in depressed patients. British Journal of Psychiatry. 1986;148:642–647. doi: 10.1192/bjp.148.6.642. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparametized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jacobsen T, Hibbs E, Ziegenhain U. Maternal expressed emotion related to attachment disorganization in early childhood: A preliminary report. Journal of Child Psychology and Psychiatry. 2000;41:899–906. [PubMed] [Google Scholar]
- Kendall PC, Warman MJ. Anxiety disorders in youth: Diagnostic consistency across DSM-III-R and DSM-IV. Journal of Anxiety Disorders. 1996;10:453–463. [Google Scholar]
- Kershner JG, Cohen NJ, Coyne JC. Expressed emotion in families of clinically referred and nonreferred children: Toward a further understanding of the expressed emotion index. Journal of Family Psychology. 1996;10:97–106. [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Leeb B, Hahlweg K, Goldstein MJ, Feinstein E, Mueller U, Dose M, Magana A. Cross-national reliability, concurrent validity, and stability of a brief method of assessing expressed emotion. Psychiatry Research. 1991;39:25–31. doi: 10.1016/0165-1781(91)90005-a. [DOI] [PubMed] [Google Scholar]
- Liakopoulou M, Alifieraki T, Katideniou A, Peppa M, Maniati M, Tzikas D, Hibbs ED, Dacou-Voutetakis C. Maternal expressed emotion and metabolic control of children and adolescents with diabetes mellitus. Psychotherapy and Psychosomatics. 2001;70:78–85. doi: 10.1159/000056230. [DOI] [PubMed] [Google Scholar]
- Magana-Amato, A. (1993). Manual for coding expressed emotion from the Five Minute Speech Sample Unpublished manuscript, University of California at Los Angeles.
- Magana AB, Goldstein MJ, Karno M, Miklowitz DJ, Jenkins J, Falloon RH. A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Research. 1986;17:203–212. doi: 10.1016/0165-1781(86)90049-1. [DOI] [PubMed] [Google Scholar]
- Malla AK, Kazarian SS, Barnes S, Cole JD. Validation of the Five Minute Speech Sample in measuring expressed emotion. Canadian Journal of Psychiatry. 1991;36:297–299. doi: 10.1177/070674379103600411. [DOI] [PubMed] [Google Scholar]
- Marshall VG, Longwell L, Goldstein MJ, Swanson JM. Family factors associated with aggressive symptomology in boys with attention deficit hyperactivity disorder: A research note. Journal of Child Psychology and Psychiatry. 1990;31:629–636. doi: 10.1111/j.1469-7610.1990.tb00802.x. [DOI] [PubMed] [Google Scholar]
- McGuire JB, Earls F. The test–retest stability of the Five Minute Speech Sample in parents of disadvantaged, minority children. Journal of Child Psychology and Psychiatry. 1994;35:971–979. doi: 10.1111/j.1469-7610.1994.tb02306.x. [DOI] [PubMed] [Google Scholar]
- Muthén, L.K., & Muthén, B.O. (1998). Mplus user’s guide Los Angeles: Muthen & Muthen.
- Nelson, D.R. (2001). Children of depressed mothers: The role of expressed emotion Unpublished doctoral dissertation, University of California, Los Angeles.
- O’Farrell TJ, Hooley J, Fals-Stewart W, Cutter HSG. Expressed emotion and relapse in alcoholic patients. Journal of Consulting and Clinical Psychology. 1998;66:744–752. doi: 10.1037//0022-006x.66.5.744. [DOI] [PubMed] [Google Scholar]
- Peris TS, Baker BL. Applications of the expressed emotion construct to young children with externalizing behavior: Stability and prediction over time. Journal of Child Psychology and Psychiatry. 2000;41:457–462. [PubMed] [Google Scholar]
- Richters JE. Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychological Bulletin. 1992;112:485–499. doi: 10.1037/0033-2909.112.3.485. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone ME, Shaffer D, Dulcan MK, Jensen PS, Fisher P, Bird HR, Goodman SH, Lahey BB, Lichtman JH, Canino G, Rubio-Stipec M, Rae DS. Criterion validity of the NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC 2.3) Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:878–888. doi: 10.1097/00004583-199607000-00013. [DOI] [PubMed] [Google Scholar]
- Schwartz CE, Dorer DJ, Beardslee WR, Lavori PW, Keller MB. Maternal expressed emotion and parental affective disorder: Risk for childhood depressive disorder, substance abuse, or conduct disorder. Journal of Psychiatric Research. 1990;24:231–250. doi: 10.1016/0022-3956(90)90013-g. [DOI] [PubMed] [Google Scholar]
- Seifer R, Sameroff AJ, Baldwin CP, Baldwin A. Child and family factors that ameliorate risk between 4 and 13 years of age. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:893–903. doi: 10.1097/00004583-199209000-00018. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Dulcan MK, Davies M. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA study. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Stubbe DE, Zahner GEP, Goldstein MJ, Leckman JF. Diagnostic specificity of a brief measure of expressed emotion: A community study of children. Journal of Child Psychology and Psychiatry. 1993;34:139–154. doi: 10.1111/j.1469-7610.1993.tb00976.x. [DOI] [PubMed] [Google Scholar]
- Tabachnick, B.G. & Fidell, L.S. (1996). Using multivariate statistics (3rd edn). New York: HarperCollins College Publishers.
- Tarrier N, Sommerfield C, Pilgrim H. Relatives’ expressed emotion (EE) and PTSD outcome. Psychological Medicine. 1999;29:801–811. doi: 10.1017/s0033291799008569. [DOI] [PubMed] [Google Scholar]
- Van Furth EF, Van Strien DC, Martina LML, Van Son MJM, Hendrickx JJP, Van Engeland H. Expressed emotion and the prediction of outcome in adolescent eating disorders. International Journal of Eating Disorders. 1996;20:19–31. doi: 10.1002/(SICI)1098-108X(199607)20:1<19::AID-EAT3>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Vaughn CE, Leff JP. The measurement of expressed emotion in the families of psychiatric patients. British Journal of Social and Clinical Psychology. 1976;15:157–165. doi: 10.1111/j.2044-8260.1976.tb00021.x. [DOI] [PubMed] [Google Scholar]
- Vostanis P, Nicholls J, Harrington R. Maternal expressed emotion in conduct and emotional disorders of childhood. Journal of Child Psychology and Psychiatry. 1994;35:365–376. doi: 10.1111/j.1469-7610.1994.tb01168.x. [DOI] [PubMed] [Google Scholar]
- Wagner AW, Logsdon RG, Pearson JL, Teri L. Caregiver expressed emotion and depression in Alzheimer’s disease. Aging and Mental Health. 1997;1:132–139. [Google Scholar]
- Wamboldt FS, O’Connor SL, Wamboldt MZ, Gavin LA, Klinnert MD. The five minute speech sample in children with asthma: Deconstructing the construct of expressed emotion. Journal of Child Psychology and Psychiatry. 2000;41:887–898. [PubMed] [Google Scholar]
- Yeh M, Weisz JR. Why are we here at the clinic? Parent–child (dis)agreement on referral problems at outpatient treatment entry. Journal of Consulting and Clinical Psychology. 2001;69:1018–1025. doi: 10.1037//0022-006x.69.6.1018. [DOI] [PubMed] [Google Scholar]


