Abstract
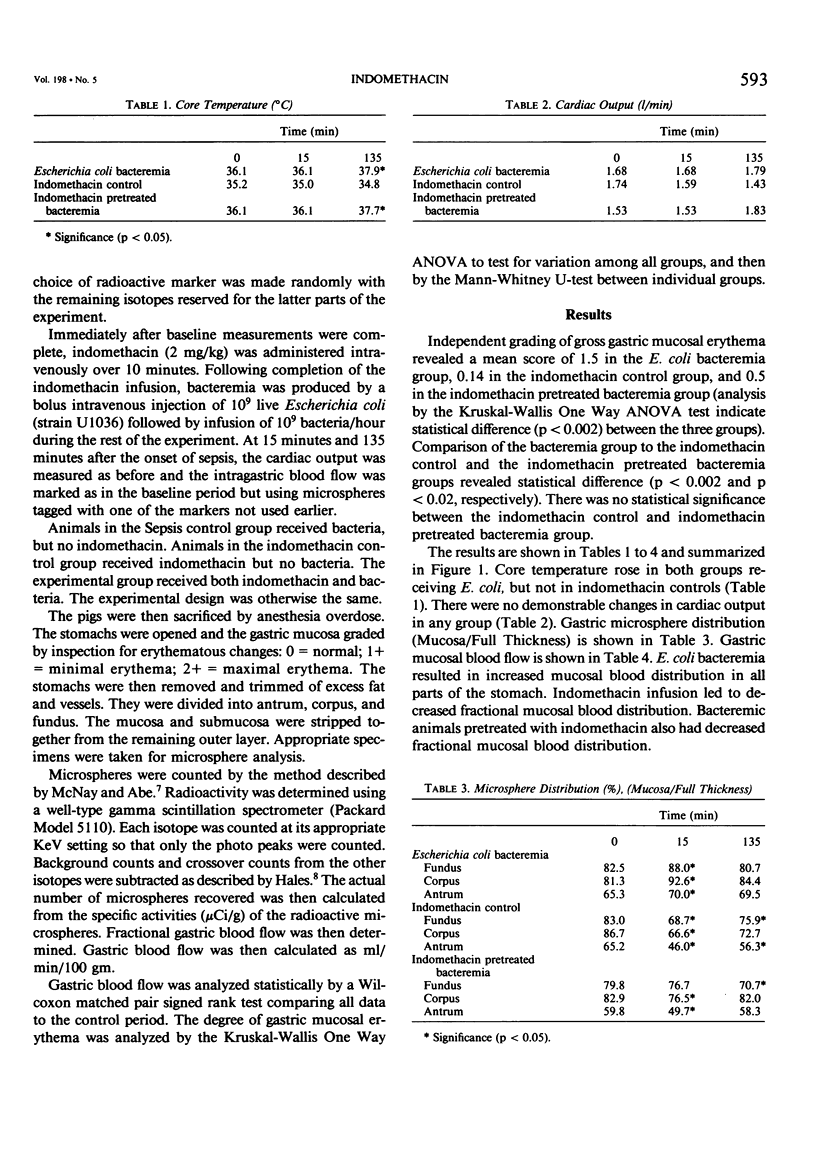
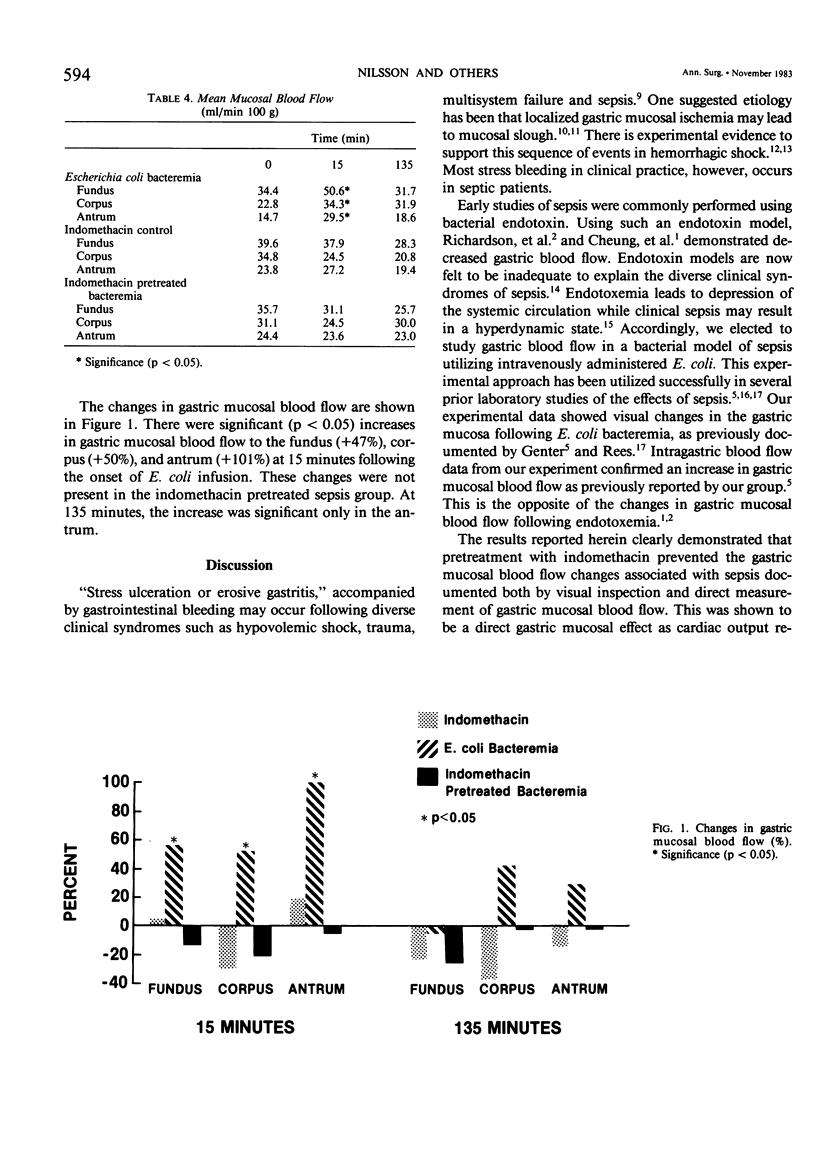
Recent evidence suggests that sepsis results in increased gastric mucosal blood flow (GMBF). To investigate the possible role of prostaglandins in mediating this response, the GMBF was measured in the fundus, corpus, and antrum of pig stomachs with and without pretreatment with indomethacin, an inhibitor of prostaglandin synthesis, before and after the induction of bacteremia. The studies were done in 22 piglets (seven sepsis controls, seven indomethacin controls and eight experimental [indomethacin pretreated sepsis] ). Sepsis was produced in piglets by bolus intravenous injection of 10(9) live Escherichia coli followed by an infusion of 10(9) E. coli/hr. Cardiac output (C.O.) was measured by thermodilution. GMBF was measured by microsphere trapping. Following sacrifice, hyperemia was noted in the sepsis group but not in the other groups. GMBF was determined by standard techniques (expressed as ml/min/100 gm tissue). There were significant (p less than 0.05) increases in gastric mucosal blood flow to the fundus (+47%), corpus (+50%), and antrum (+101%) at 15 minutes following the onset of E. coli infusion. At 135 minutes, the increase was only significant in the antrum. GMBF, however, did not change in the indomethacin control or indomethacin pretreated sepsis groups. These data demonstrate GMBF in the stomach following sepsis. The changes were not present in the indomethacin control or in the indomethacin pretreated sepsis groups. Since indomethacin is an inhibitor of prostaglandin synthesis, the results suggest that the GMBF may be a prostaglandin mediated response.
Full text
PDF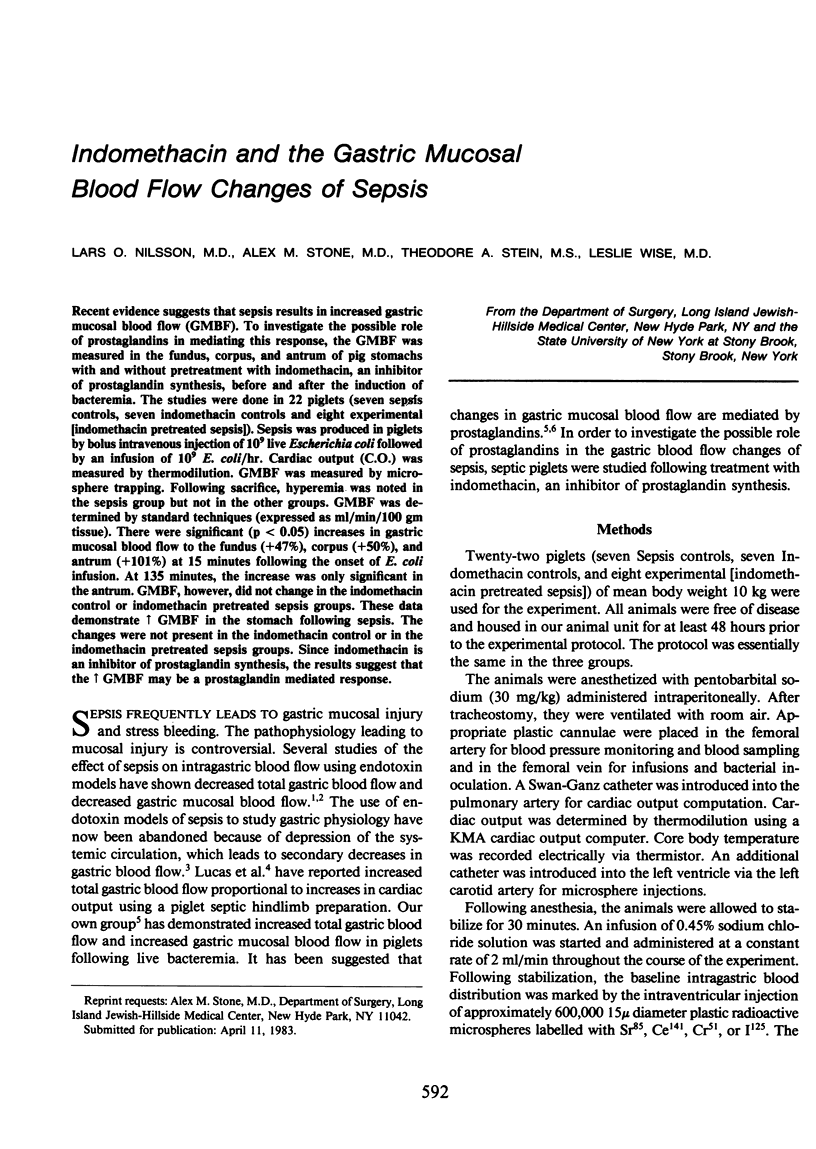
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cheung L. Y., Reese R. S., Moody F. G. Direct effect of endotoxin on the gastric mucosal microcirculation and electrical gradient. Surgery. 1976 May;79(5):564–568. [PubMed] [Google Scholar]
- Clowes G. H., Jr, O'Donnell T. F., Jr, Ryan N. T., Blackburn G. L. Energy metabolism in sepsis: treatment based on different patterns in shock and high output stage. Ann Surg. 1974 May;179(5):684–696. doi: 10.1097/00000658-197405000-00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskill H. V., 3rd, Sirinek K. R., Levine B. A. Prostacyclin-mediated gastric cytoprotection is dependent on mucosal blood flow. Surgery. 1982 Aug;92(2):220–225. [PubMed] [Google Scholar]
- Genter B., Stone A. M., Stein T. A., Wise L. Gastric mucosal blood flow and Escherichia coli bacteremia. Am J Surg. 1983 Mar;145(3):364–368. doi: 10.1016/0002-9610(83)90201-5. [DOI] [PubMed] [Google Scholar]
- Hinshaw L. B., Benjamin B., Holmes D. D., Beller B., Archer L. T., Coalson J. J., Whitsett T. Responses of the baboon to live Escherichia coli organisms and endotoxin. Surg Gynecol Obstet. 1977 Jul;145(1):1–11. [PubMed] [Google Scholar]
- Hinshaw L. B., Solomon L. A., Holmes D. D., Greenfield L. J. Comparison of canine responses to Escherichia coli organisms and endotoxin. Surg Gynecol Obstet. 1968 Nov;127(5):981–988. [PubMed] [Google Scholar]
- Hottenrott C., Seufert R. M., Becker H. The role of ischemia in the pathogenesis of stress induced gastric lesions in piglets. Surg Gynecol Obstet. 1978 Feb;146(2):217–220. [PubMed] [Google Scholar]
- Kivilaakso E., Ahonen J., Aronsen K. F., Höckerstedt K., Kalima T., Lempinen M., Suoranta H., Vernerson E. Gastric blood flow, tissue gas tension and microvascular changes during hemorrhage-induced stress ulceration in the pig. Am J Surg. 1982 Mar;143(3):322–330. doi: 10.1016/0002-9610(82)90101-5. [DOI] [PubMed] [Google Scholar]
- Lucas C. E., Ravikant T., Walt A. J. Gastritis and gastric blood flow in hyperdynamic septic pigs. Am J Surg. 1976 Jan;131(1):73–77. doi: 10.1016/0002-9610(76)90424-4. [DOI] [PubMed] [Google Scholar]
- McGiff J. C. Prostaglandins, prostacyclin, and thromboxanes. Annu Rev Pharmacol Toxicol. 1981;21:479–509. doi: 10.1146/annurev.pa.21.040181.002403. [DOI] [PubMed] [Google Scholar]
- McNay J. L., Abe Y. Redistribution of cortical blood flow during renal vasodilatation in dogs. Circ Res. 1970 Dec;27(6):1023–1032. doi: 10.1161/01.res.27.6.1023. [DOI] [PubMed] [Google Scholar]
- Menguy R. Role of gastric mucosal energy metabolism in the etiology of stress ulceration. World J Surg. 1981 Mar;5(2):175–180. doi: 10.1007/BF01658282. [DOI] [PubMed] [Google Scholar]
- Messina E. J., Weiner R., Kaley G. Arteriolar reactive hyperemia: modification by inhibitors of prostaglandin synthesis. Am J Physiol. 1977 Jun;232(6):H571–H575. doi: 10.1152/ajpheart.1977.232.6.H571. [DOI] [PubMed] [Google Scholar]
- Moody F. G., Zalewsky C. A., Larsen K. R. Cytoprotection of the gastric epithelium. World J Surg. 1981 Mar;5(2):153–163. doi: 10.1007/BF01658278. [DOI] [PubMed] [Google Scholar]
- Muryobayashi T., Okada K., Shingae J. Effects of new synthetic analogues of prostaglandin E2 on gastric acid secretion and gastric ulceration. Adv Prostaglandin Thromboxane Res. 1976;2:541–545. [PubMed] [Google Scholar]
- Rees M., Bowen J. C. Stress ulcers during live Escherichia coli sepsis. The role of acid and bile. Ann Surg. 1982 May;195(5):646–652. doi: 10.1097/00000658-198205000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson R. S., Norton L. W., Sales J. E., Eiseman B. Gastric blood flow in endotoxin-induced stress ulcer. Arch Surg. 1973 Feb;106(2):191–195. doi: 10.1001/archsurg.1973.01350140049015. [DOI] [PubMed] [Google Scholar]
- Robert A., Nezamis J. E., Lancaster C., Hanchar A. J. Cytoprotection by prostaglandins in rats. Prevention of gastric necrosis produced by alcohol, HCl, NaOH, hypertonic NaCl, and thermal injury. Gastroenterology. 1979 Sep;77(3):433–443. [PubMed] [Google Scholar]
- Rutherford R. B., Balis J. V., Trow R. S., Graves G. M. Comparison of hemodynamic and regional blood flow changes at equivalent stages of endotoxin and hemorrhagic shock. J Trauma. 1976 Nov;16(11):886–897. doi: 10.1097/00005373-197611000-00007. [DOI] [PubMed] [Google Scholar]
- Sales J., Norton L., Nolan P., Rankin J., Eiseman B. Gastric mucosal ischemia in experimental stress ulcer. J Surg Res. 1975 Jan;18(1):65–74. doi: 10.1016/0022-4804(75)90142-0. [DOI] [PubMed] [Google Scholar]
- Silen W., Merhav A., Simson J. N. The pathophysiology of stress ulcer disease. World J Surg. 1981 Mar;5(2):165–174. doi: 10.1007/BF01658279. [DOI] [PubMed] [Google Scholar]


