Abstract
Objective:
To review the potential and proven benefits and complications of epidural anesthesia/analgesia.
Summary Background Data:
Advances in analgesia/anesthesia have improved patient satisfaction and perioperative outcomes. Epidural anesthesia/analgesia is one of these advances that is gaining rapid acceptance due to a perceived reduction in morbidity and overall patient satisfaction.
Methods:
A MEDLINE search was conducted for all pertinent articles on epidural anesthesia/analgesia.
Results:
Retrospective, prospective, and meta-analysis studies have demonstrated an improvement in surgical outcome through beneficial effects on perioperative pulmonary function, blunting the surgical stress response and improved analgesia. In particular, significant reduction in perioperative cardiac morbidity (∼30%), pulmonary infections (∼40%), pulmonary embolism (∼50%), ileus (∼2 days), acute renal failure (∼30%), and blood loss (∼30%) were noted in our review of the literature. Potential complications related to epidural anesthesia/analgesia range from transient paresthesias (<10%) to potentially devastating epidural hematomas (0.0006%).
Conclusions:
Epidural anesthesia/analgesia has been demonstrated to improve postoperative outcome and attenuate the physiologic response to surgery.
Epidural anesthesia and analgesia have been noted to improve surgical outcome by inhibiting physiologic perturbations related to surgical stress. We review the evidence of epidural anesthesia/analgesia potential benefits on each physiologic system and rationale for their use.
Advances in perioperative anesthesia and analgesia have improved pain relief and satisfaction in surgical patients. Opioid administered via patient-controlled analgesia (IV-PCA) provides better analgesia and patient satisfaction than conventional delivery. However, IV-PCA has not been demonstrated to affect postoperative outcome significantly. Recent studies suggest that advances in anesthesia and postoperative analgesia can affect postoperative outcome.1–3 Epidural anesthesia and analgesia have the potential to reduce or eliminate the perioperative physiologic stress responses to surgery and thereby decrease surgical complications and improve outcomes.1–3 The purposes of this review are to integrate experimental and clinical data addressing the physiologic effects of epidural anesthesia and postoperative epidural analgesia on surgical patients and to review the real and potential benefits of this technology with respect to patient outcomes. The effects of epidural anesthesia and analgesia on cardiovascular, coagulation, pulmonary, and gastrointestinal physiology; the surgical stress response; immune function; cognition; complications; and surgical outcomes will be reviewed separately.
CARDIOVASCULAR SYSTEM
Cardiac morbidity is the most common cause of death after major surgical procedures. Anesthetic techniques that reduce cardiac morbidity will therefore have potential for improving surgical morbidity and mortality. Thoracic epidural anesthesia (TEA) with local anesthetics (eg, lidocaine) can produce a selective segmental blockade of the cardiac sympathetic innervations (T1-T5).1 Since perioperative sympathetic activation plays a causative role in the development of myocardial ischemia and infarction, inhibition of this activation would be expected to reduce cardiac morbidity. Excessive activation of the cardiac (T1-T5) sympathetic nervous system by surgical stress has been demonstrated to increase indices of myocardial oxygen demand, while inducing coronary artery vasoconstriction (decreasing supply), thus resulting in clinical correlates of myocardial ischemia such as ST segment changes, angina, and arrhythmias.1,4 Furthermore, sympathetic activation also plays a role in the development of postoperative hypercoagulable state (see below), further contributing to coronary artery thrombosis.5 Thoracic epidural anesthesia with local anesthetics, by selectively blocking cardiac sympathetic nerve fibers, blunts these adverse effects of surgical stress. Although total coronary blood flow typically remains unchanged when TEA is administered, blood flow to ischemic regions of myocardium may increase.6 By blocking sympathetically mediated coronary constriction, endocardial to epicardial blood flow ratio is improved, thus optimizing the regional distribution of myocardial blood flow. Thoracic sympathetic blockade also reduces the major determinants of myocardial oxygen demand, such as blood pressure, heart rate, and contractility. TEA thus improves the balance between cardiac supply and demand. Animal models convincingly demonstrate that TEA during acute coronary artery occlusion is associated with decreased myocardial infarct size.4,7 Similarly, TEA has been used as an effective treatment of refractory myocardial ischemia in humans.6,8 Smeets et al9 studied a small group of patients undergoing aortic reconstructions and found significantly lower levels of urinary catecholamine excretion in epidural patients compared with general anesthesia patients. Gold et al10 also compared catecholamine release in patients undergoing abdominal aortic aneurysm repairs randomized to lumbar epidural or general anesthesia. They reported a large increase in serum catecholamine levels in the general anesthesia group but not the epidural group.
Studies of high-risk surgical patients randomized to TEA plus general anesthesia or general anesthesia alone have demonstrated fewer cardiac complications in TEA patients (Table 1). 11,12 These studies suggest that there is approximately a 4-fold reduction in the incidences of postoperative congestive heart failure, myocardial infarction, and death in patients treated with epidural local anesthetics compared with those treated with balanced general anesthetics.12 A nonrandomized study (n = 198) also suggested that TEA patients have fewer episodes of myocardial ischemia than a cohort of general anesthesia patients (5% versus 17%, P < 0.04).13 Although the data from relatively small studies clearly suggest that intraoperative TEA and postoperative thoracic epidural analgesia with local anesthetics are associated with reduced cardiac morbidity and mortality, most studies are insufficiently powered to demonstrate clinically and statistically significant benefits.13 It is important to emphasize that the beneficial effects of regional anesthetics on cardiac morbidity are likely limited to thoracic epidural techniques with local anesthetics. Lumbar epidural anesthesia or TEA with narcotics only (eg, fentanyl) will not block cardiac sympathetic nerves. Furthermore, it is likely that postoperative thoracic epidural analgesia for 48–72 hours is required to assure the maximum cardiac benefits. A randomized study conducted by Baron et al did not demonstrate a decrease in cardiac morbidity in patients undergoing aortic reconstructions treated with intraoperative thoracic epidural anesthesia and light general anesthesia, compared with those treated with general anesthesia only.14 However, this study did not control for postoperative analgesia. In fact, 63% of epidural anesthesia patients did not receive postoperative epidural analgesia, and 59% of general anesthesia patients received postoperative epidural analgesia. This study suggests that the beneficial effects of TEA on cardiac morbidity in high risk (eg, aortic reconstructions) may require several days of postoperative epidural analgesia, a finding not unexpected because cardiac morbidity frequently occurs on the third or fourth day after surgery.
TABLE 1. Statistically Significant and Potential/Probable Benefits of Epidural Anesthesia/Analgesia Compared With General Anesthesia and Systemic Analgesia
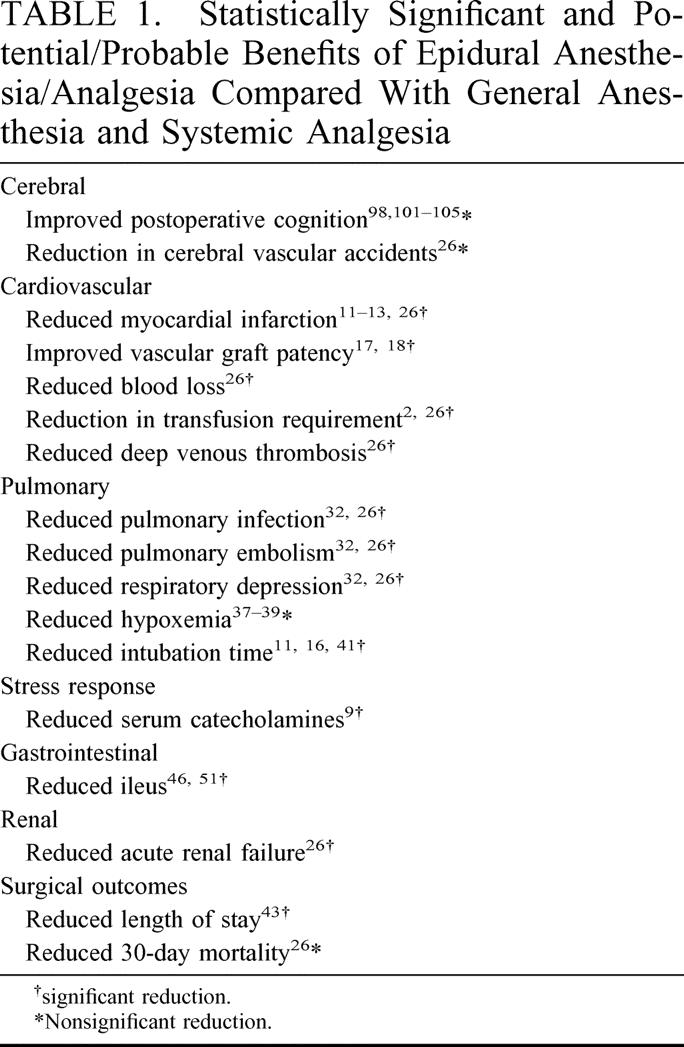
The beneficial effects of epidural anesthesia/analgesia in patients undergoing vascular surgery are well documented (Table 1).15–18 In 1993, Tuman et al17 reported a randomized study comparing outcomes in patients undergoing major vascular operations. Eighty patients were randomized to epidural bupivacaine/fentanyl anesthesia/analgesia or general anesthesia plus IV-PCA analgesia groups. Similar to the studies mentioned above, there were fewer episodes of congestive heart failure and myocardial infarction in the epidural patients (10 versus 5% and 8 versus 0%, respectively, P < 0.05). These authors also reported a dramatic reduction in vascular graft occlusion (1 versus 9, P < 0.007), as well as a significant difference in thromboelastographs between groups, a finding suggesting that general anesthesia patients were hypercoagulable, whereas the epidural group maintained normal coagulation.
Another prospective randomized study comparing 100 patients undergoing infra-inguinal revascularizations reported significant differences in vascular graft occlusions in the epidural versus the general anesthesia groups (4 of 49 [8%] versus 22 of 51 [43%], P < 0.01).18 In a companion study, these investigators also assessed the status of the fibrinolytic system in their patients.19 Levels of plasminogen activator inhibitor-1 (PAI-1), which blocks plasmin-mediated fibrinolysis, were significantly elevated in the general anesthesia group, whereas levels were maintained at preoperative levels in the epidural group, presumably contributing to the differences in graft occlusion rates. Of interest, the epidural anesthesia patients did not receive postoperative epidural analgesia, suggesting that the effects on coagulation are produced by intraoperative epidural anesthesia. Finally, a recently reported randomized, controlled VA Cooperative Study16 concluded that epidural anesthesia and analgesia improved the overall outcomes and shortened intubation times and ICU stays in patients undergoing abdominal aortic operations.
In summary, 4 large studies involving high-risk (eg, aortic reconstruction) surgery patients have reported significant reductions in cardiac morbidity associated with use of intraoperative and postoperative epidural anesthesia/analgesia using local anesthetics plus opioids. In addition, intraoperative epidural administration of local anesthetics blunts the physiologic hypercoagulable surgical stress response and modifies the perioperative hypercoagulable state. This occurs via several mechanisms, such as blockade of sympathetic efferent signals, enhanced fibrinolytic activity, and systemic absorption of local anesthetics. The clinical relevance of these phenomena are confirmed by convincing data that intraoperative epidural anesthesia improves graft patency in lower extremity vascular reconstruction patients.
COAGULATION
Thromboembolic events in the postoperative period have been linked to the hypercoagulable environment initiated during surgery. The primary contributors to this pro-thrombotic state are a reduction in venous blood flow secondary to positive pressure ventilation, neuromuscular blockade, and activation of the sympathetic system. Sympathetic stimulation produces marked increases in factor VIII- and factor VIII–related antigen (von Willibrand factor), inhibits fibrinolysis through PAI-1, decreases antithrombin III (a powerful natural anticoagulant), and initiates platelet aggregation.20–22 Epidural analgesia and anesthesia (EAA) attenuates the hypercoagulable perioperative state and decreases thromboembolic complications associated with surgery by blunting the sympathetic response and improving lower extremity blood flow. In addition, the systemic absorption of local anesthetics, improved pain control, and earlier mobility likely decrease the incidence of clot formation. Blunting the sympathetic response to surgery with EAA is associated with demonstrable effects on the coagulation cascade, with normalization of both factor VIII- and factor VIII–related protein, decreases in PAI-1, and an increased antithrombin III.19,21 Several studies have demonstrated that systemic absorption of local anesthetic act as an anticoagulant by blocking thromboxane A2 (TX) signaling23 and reduce blood viscosity by minimizing protein, erythrocyte, and platelet aggregation.24,25
The clinical merits of epidural analgesia’s effects on coagulation have been addressed in 2 recent meta-analyses of randomized clinical studies. Rodgers et al26 analyzed 141 randomized clinical trials comparing EAA to general anesthesia and calculated 44% reduction in deep venous thrombosis and a subsequent 55% reduction in pulmonary emboli (Table 1). Another analysis of 22 randomized studies in patients undergoing lower abdominal and lower extremity orthopedic surgery found a significant reduction in thromboembolic complications when general-epidural anesthesia/analgesia was compared with general anesthesia-systemic analgesia (28% to 62%, respectively).27 Interestingly, in a subgroup comparison of 5 randomized trials in abdominal surgery patients, these investigators found a less impressive reduction of thromboembolic complications of 22.4% to 15.7%. They propose 2 explanations for the discrepancy. First, thoracic epidurals have a less significant effect on lower extremity and deep pelvis blood flow. Second, only 1 of the 5 studies emphasized aggressive postoperative mobility in both groups to exploit all the benefits of epidural analgesia’s effects.
Epidural anesthesia significantly minimizes blood loss during lower abdominal/pelvis and hip surgery. The proposed mechanisms are by lowering the mean arterial blood pressure (MAP) through sympatholysis and redirecting blood flow away from the operative site (Table 1).2
In summary, patients undergoing major operations under EAA benefit from improved venous blood flow, attenuation of the sympathetic response to surgery, the anticoagulant properties of local anesthetics, early mobility, and lowering of MAP.
PULMONARY
Pulmonary morbidity in the postoperative period has been attributed to the type of anesthetic agent and physiologic perturbations of the pulmonary system. Thoracic epidural analgesia/anesthesia (TEAA) can reduce the incidence of postoperative atelectasis, pneumonia, and hypoxemia by directly influencing these variables.28–32
Perhaps the most profound effect of major abdominal and thoracic surgery on pulmonary function is a reduction in the functional residual capacity (FRC) due to diaphragmatic dysfunction, decreased chest wall compliance, and pain-limited inspiration. As a result, FRC decreases by at least 20% after abdominal surgery, reaching its lowest point at 24–48 hours and not returning to normal until 1 week.30,31 On the other hand, TEAA with a local anesthetic and general anesthesia when compared with IV-PCA and general anesthesia resulted in a 27% increase in the FRC and an overall improvement in pulmonary outcome.33 Reflex inhibition of the phrenic nerve after major surgery also causes measurable impairment of diaphragm contractility that continues 5–7 days postoperatively.28 The reflex inhibition is not affected by the use of systemic or epidural opioids. However, TEAA with a local anesthetic disrupts the reflex arc and permits normal diaphragm function.28–31,34 In addition, an increase in chest wall muscle tone and decreased chest wall compliance secondary to both the spinal reflex arc and pain are blunted with TEAA. Thus, TEAA improves measurable pulmonary function by blunting spinal reflex arcs, controlling pain, and increasing chest wall compliance. It should be noted, however, that while there is demonstrated improvement in pulmonary function tests after major abdominal or thoracic surgery under TEAA, well-conducted studies have found no significant correlation between postoperative pulmonary function tests and the incidence of pulmonary complications.32 Therefore, pulmonary morbidity must be evaluated not only by surrogate markers, but rather by the incidence of pneumonia, respiratory failure, atelectasis, and hypoxemia.
Postoperative hypoxemia contributes to both pulmonary dysfunction and myocardial ischemia.35–37 Specifically, Catley et al38 found significantly fewer hypoxemic events in elderly patients undergoing lower extremity orthopedic procedures when they received epidural anesthesia with local anesthetic (Table 1).38 The use of systemic and epidural opioids is associated with a higher incidence of hypoxemic events compared with epidural analgesia with a local anesthetic alone.11,37–39 A recent meta-analysis of randomized controlled clinical trials assessed improvements in pulmonary outcomes comparing systemic opioids, epidural opioid, and epidural local anesthetic. They found that the use of epidural opioids, compared with systemic opioids, was associated with significantly less atelectasis and a reduced incidence of pulmonary complications.32 However, epidural local anesthetics significantly reduced the incidence of pulmonary complications, atelectasis, and pneumonia and raised the postoperative partial pressure of oxygen even higher.32 Subsequently, a meta-analyses of 141 randomized trials found a 39% reduction in pneumonia and a 59% reduction in respiratory depression (both P < 0.001) in patients treated with TEAA using local anesthetic, compared with patients treated with general anesthesia and PCA (Table 1).25 A review of 462 surgical cancer patients managed with either epidural analgesia or systemic opioids found a distinct advantage with TEAA. Patients receiving epidural analgesia were extubated sooner (0.5 days versus 1.2 days, P < 0.05), spent less time in the intensive care unit (ICU) (1.3 days versus 2.8 days, P < 0.05), and spent less time in the hospital (11 days versus 17 days, P < 0.05). The authors calculated a cost savings of $4675 for each patient managed with epidural analgesia.40 As mentioned above, a recently published prospective multicenter study also reported decreased intubation times and ICU stays in epidural patients after abdominal aortic operations.16
On the other hand, several randomized studies have not demonstrated any improvement in pulmonary outcome with the use of TEAA. These studies, however, consisted mostly of healthy low-risk patients, did not control for postoperative analgesia, and/or lacked sufficient statistical power40–42
In summary, we believe the data support the conclusion that epidural analgesia with local anesthetic can improve pulmonary outcomes by attenuating the physiologic response to surgery, controlling postoperative pain, permitting earlier extubation, and reducing length of stay.
GASTROINTESTINAL FUNCTION
Gastrointestinal ileus dramatically effects morbidity and length of hospital stay after major surgery.44 The pathophysiology of postoperative ileus is clearly related to abdominal pain and surgical stress-activated reflex arcs of sympathetic activity. Afferent pain fibers and sympathetic efferent fibers contribute to ileus.1 Blockage of afferent pain signals and efferent sympathetic reflex arcs by intraoperative epidural anesthetic and postoperative epidural analgesic techniques should abolish the stress response and minimize the effect of surgery on bowel function.1,45 In addition, the anatomy of the autonomic nervous system permits the use of epidural anesthesia and analgesia to block the inhibitory sympathetic efferents to the gut while preserving the stimulatory parasympathetic efferents.1,45 Parasympathetic innervation via both the vagus nerve and sacral nerve roots can be spared, while sympathetic innervations to the gut (T5-L2) can be selectively blocked when local anesthetics are delivered through a midthoracic epidural catheter. Thus, in theory and in practice, TEA can enhance bowel motility not only by producing pain relief and lessening the systemic stress response, but also by creating a sympathectomy, resulting in unopposed parasympathetic innervations to the gut. Sympathetic stimulation, pain, opioids, nitrous oxide, inhalation anesthetics, and increased endogenous catecholamines all contribute to postoperative ileus, and all are blunted or blocked in patients treated with perioperative TEA.1,2,45 Steinbrook46 has proposed 6 mechanisms whereby TEA may promote gastrointestinal motility: (1) blockage of nociceptive afferent nerves; (2) blockade of thoracolumbar sympathetic efferent nerves; (3) unopposed parasympathetic efferent nerves; (4) reduced need for postoperative opioids; (5) increased gastrointestinal blood flow; and (6) systemic absorption of local anesthetic. Illustrating the effect of epidural local anesthetics on intestinal motility is a report of thoracic epidural bupivacaine administration resulting in resolution of acute colonic pseudo-obstruction or Ogilvie syndrome, a condition generally considered to reflect an imbalance of sympathetic and parasympathetic colonic innervation, usually aggravated by systemic narcotic effects.47
Many studies comparing TEA versus balanced general anesthesia and systemic opioid analgesia have reported more rapid recovery of bowel function in TEA patients.1,2,45,48–51 Gastrointestinal function typically returns 2–3 days earlier in patients randomized to TEA and postoperative epidural analgesia. Objective endpoints such as transit of radiopaque markers and GI myoelectric actively, as well as the more subjective endpoints such as flatus or bowel movements, are consistently improved.52 Eight prospective randomized studies have concluded that patients treated with TEA and epidural analgesia demonstrate faster recovery of gastrointestinal function than those treated with balanced anesthesia and systemic opioid analgesia.1 Studies not demonstrating beneficial effects of epidural catheters with respect to duration of ileus either administered systemic opioids postoperatively, prior to the return of bowel function, or used lumbar epidural catheters.4 Randomized studies have also shown that gastrointestinal motility resumed more quickly with the use of epidural local anesthetics compared with epidural narcotics (Table 1).1,51,53 Epidural opioids alone likely have minimal advantage over systemic opioids with respect to duration of intestinal ileus. In summary, the data demonstrated that intraoperative TEA and postoperative thoracic epidural analgesia with regimens containing local anesthetics results in more rapid recovery of bowel function. It is emphasized that there are several prerequisites for achieving this result. First, the epidural must be placed and activated prior to the surgical stress and nociceptive afferent stimulation. Second, the epidural catheter should include the T5-L2 dermatomes, and the solution administered into the catheter should include local anesthetics to affect a sympathetic blockade of the gut. Third, the epidural local anesthetics need to be administered postoperatively until bowel function returns (usually 2–3 days) to achieve the full benefits of the technique.
Are there potential risks of epidural anesthesia in patients undergoing gastrointestinal surgery? Some authors have questioned whether epidural analgesia might be detrimental to healing of gastrointestinal anastomoses because of the increased bowel motility. There is substantial experimental and clinical evidence, however, that epidural anesthesia/analgesia is safe for patients undergoing bowel resections with anastomoses. In addition, studies in animals and humans have demonstrated that TEA with local anesthetics during surgical stimulation maintains intestinal mucosal blood flow and gastric mucosal pH at physiologic levels compared with controls treated with general anesthetics.54–56 It has been hypothesized that the increased mucosal flow would promote anastomotic healing.57 In fact, retrospective cohort controlled studies suggest that regional anesthetic techniques were associated with a beneficial effect on anastomotic healing rates.58,59
STRESS
The stress response to surgery initiates a predictable cascade of physiologic and metabolic events through direct activation of the sympathetic and somatic nervous system. The response begins with the initiation of general anesthesia and lasts 3 to 4 days postoperatively.18 The resultant release of neuroendocrine mediators and cytokines (IL-1, IL-6, TNF-α) produces the clinical sequelae of tachycardia, hypertension, fever, immunosuppression, and protein catabolism, which peaks postoperatively and is temporally related to postoperative morbidity.60–65 The magnitude of the stress response, as reflected by serum and urinary markers, likely correlates with postoperative cardiac, vascular, and infectious morbidity; attenuation should decrease these morbidities.66 Epidural anesthesia has the potential to block completely the sympathetic response to surgery below the umbilicus and to blunt significantly the response to surgery above the umbilicus.67,68 This is shown by a prospective randomized study of patients undergoing an elective abdominal aortic aneurysm (AAA) repair who had a marked reduction in serum cortisol levels (P < 0.01) and urinary catecholamines (P < 0.01) with epidural anesthesia (Table 1).9 However, providing adequate postoperative analgesia does not necessarily equate with blocking the sympathetic response. Epidural local anesthetics block the sympathetic response, whereas epidural opioids incompletely block the signal.67,68 This is consistent with the fact that opioids only block the nociceptive pathways of sympathetic activation while local anesthetics inhibit both nociceptive and non-nociceptive routes.
Two studies have demonstrated superiority of EAA over other analgesics in blunting the stress response. Kehlet and Holte27 evaluated the effect of analgesia, including IV-PCA, nonsteroidal antiinflammatory drugs (NSAIDs), and epidural anesthesia, on attenuating this response in an effort to reduce morbidity. Only epidural analgesia significantly reduced the magnitude of the stress response.69,27 As further support, a study by Moller70 found that IV-PCA provided effective postoperative analgesia without altering the magnitude of the stress response after surgery.
Does a reduction in the stress response result in a reduction in postoperative morbidity? Reductions in postoperative cardiac, pulmonary, coagulation, and infectious morbidity have been demonstrated in patients treated with epidural techniques, likely related to blunting of the stress response. For example, Yeager et al11 demonstrated a significant reduction in cardiac morbidity in EAA patients that correlated with concurrent, significantly lower urinary cortisol excretion compared with levels measured during general anesthesia. A decline in serum catecholamines and their subsequent effects of tachycardia, hypertension, and increased myocardial oxygen consumption were proposed as the probable mechanism.11 A similar study18 has demonstrated a reduction in graft occlusions and lower plasma catecholamine levels in a series of patients with epidurals undergoing lower extremity vascular surgery. Additionally, sympathetic activation increases metabolism resulting in hyperglycemia and protein catabolism, both of which have been implicated in infectious complications and impaired wound healing.71 Thus, the predictable cascade of events unleashed during the stress response can be blunted with EAA and may minimize common postoperative complications.
IMMUNE RESPONSE
Impairment of the immune system after surgery is a well-recognized phenomenon that has been linked to both an increase in postoperative infections and the progression of cancer.72–80 Although the exact etiology is unclear, activation of the surgical stress response, inhaled general anesthetics, and intravenous opioids are 3 suspected factors. The stress response causes suppression of T cell, B cell, monocyte, neutrophil, and cytotoxic natural killer (NK) cell activity, and inhaled general anesthetics and intravenous opioids directly decrease cytotoxic activity of NK cells and inhibit leukocyte function.72,74,76,78,81–96 As described previously, EAA may preserve postoperative immune function by attenuating the stress response, reducing the minimum alveolar concentration (MAC) of inhaled anesthetics and minimizing the use of parenteral opioids, thus helping to maintain a competent immune system.11,17,40,41,69
In several studies, significant reductions in the incidence of postoperative infections have been reported in patients treated with EAA containing local anesthetics when compared with the incidence in patients treated with parenteral analgesia.11,17 Although growth of primary tumors and metastasis has been associated with postoperative immunosuppression in several animal models,72–76,78 these effects have never been demonstrated in humans. In summary, blunting of perioperative immunosuppression by EAA is associated with reduced infectious complications and has theoretical benefits in surgical oncology outcomes.
COGNITIVE
Cognitive dysfunction occurs postoperatively in approximately 20% of patients, peaking on the second postoperative day and resolving 1 week after surgery.97 No clear etiology has been elucidated, but it has been correlated with episodes of hypoxemia, medications, preoperative depression, and general anesthesia.98–100 The elderly seem to suffer the highest incidence of confusion in the postoperative period (20–50%) as well as the subsequent sequelae of increased pneumonia, urinary complications, decubitus ulcers, and longer hospital stays.98,101 In addition, their mental status impairment may last up to 1 month.100 Whether EAA has an effect on cognitive dysfunction is controversial.97,98,102–106 A recent prospective randomized trial of 262 total knee replacements in patients with a mean age of 69 years found no significant difference in cognitive tests at 1 week and 6 months postoperatively between epidural and general anesthesia groups.104 Conversely, a prospective randomized trial by Hole et al99 found significant improvement in postoperative mental status and PaO2 values in elderly individuals undergoing total hip replacements with EAA (Table 1).
EAA can affect other important variables that may minimize postoperative cognitive dysfunction. A prospective, randomized, double-blinded, placebo-controlled trial found that epidural anesthesia significantly reduced the MAC of sevoflurane (>50%) needed by 44 patients undergoing elective surgery.105 However, many experts believe that postoperative cognitive dysfunction is related to the postoperative analgesic rather than the intraoperative anesthetic. This being the case, EAA has been shown to cause less sedation in the postoperative period when compared with IV-PCA.107,108 It is our bias that EAA minimizes the amount of general anesthetic, allows better pain control with less sedation, and increases postoperative PaO2, all of which may contribute to improved postoperative cognition.
COMPLICATIONS
Potential complications of EAA may decrease the acceptance and enthusiasm for these techniques. Neurovascular injury during catheter placement and local anesthetic/analgesic reactions are uncommon. However, local anesthetic neurotoxicity is a well-described phenomenon related to the type and concentration of anesthetic and systemic absorption. Specifically, intrathecal lidocaine at high doses has been associated with neurologic side effects not related to hemorrhage or infection.109,110 Systemic absorption of local anesthetics at high doses can produce seizures, loss of airway protective reflexes, respiratory depression, coma, cardiac arrhythmias, hemodynamic instability, and motor or autonomic blockade (urinary retention, weakness) in 0–45% of patients.111–113 These potential problems have been addressed by the use of thoracic versus lumbar epidurals, lower anesthetic concentrations, and avoidance of lidocaine.113
Hypotension and bradycardia are 2 important potential hemodynamic consequences of EAA induced sympatholysis. A recent prospective multicenter randomized trial found the incidence of hypotension after epidural-general anesthesia, defined as a >30% reduction from baseline blood pressure, to be 41% compared with 23% after general anesthesia alone (P = 0.049). There were no significant differences in heart rate or episodes of bradycardia.114 Strategies employed to balance these untoward effects include preinduction fluid administration, avoidance of lidocaine, and selected use of epidural fentanyl.115 Critics of EAA worry that sympatholysis will result in hypotension and excessive fluid administration. However, as discussed above, the incidence of complications associated with excess fluid administration, cardiac, pulmonary, and/or hemodilution are actually reduced with EAA (Table 1).
Another potential problem with postoperative analgesia is opioid-induced respiratory depression. Large surveys of patients receiving morphine through epidural catheters have found the incidence of respiratory depression less than 1%, comparable to parenteral and oral morphine.116 Additionally, the combination of epidural opioid and local anesthetic can reduce the amount of opioid needed.116,117
Catheter complications result from inadvertent penetration of the dural space, damage to neurovascular structures, or infection. Accidental dural puncture during needle insertion occurred 0.16–1.3% in a series of 51,000 epidural catheters, and subsequent postdural headaches developed in 16–86% of these patients.118–121 Although the exact etiology is unclear, transient neurologic symptoms (TNS), characterized by sharp radicular back pain or paresthesias, may be related to nerve root irritation by the catheter or intrathecal injection of local anesthetics.122 Risk factors for the development of TNS are lidocaine as the local anesthetic, lithotomy position, obesity, and outpatient status.123 Symptoms usually resolve after catheter removal. Meningitis and epidural abscess are rare. A review of 65,000 epidural cases identified only 3 cases of meningitis and no epidural abscess.124 Dural puncture, septicemia, prolonged indwelling catheter, and nonsterile technique may increase the risk of meningitis.125,126 However, a review of 75 ICU patients with epidural catheters, 9 of whom were bacteremic, found no catheter-related infections.127 Paraplegia, the most feared complication of epidural anesthesia, is usually the result of an epidural hematoma during catheter placement or removal.128 Rarely, a spinal abscess or anterior spinal artery syndrome will cause paraplegia. The incidence of epidural hematoma formation was estimated to be less than 1 in 150,000 in one study and found to be none in a second series of 100,000.129,130 Injury to the spinal vasculature during catheter placement occurs in approximately 3–12% of cases, yet this rarely results in symptomatic epidural hematomas.131,132 Symptomatic epidural hematomas are usually associated with anticoagulation, catheter placement/removal during anticoagulation, and/or trauma during catheter placement. Early recognition and emergent decompressive laminectomy within 8 hours of diagnosis have been shown to improve outcomes.133 A review of 61 cases of symptomatic epidural hematomas found that 41 (68%) patients had coagulation defects. This association has led to one of the most controversial issues surrounding EAA: the use of anticoagulation and risk of epidural hematoma formation.
Many critics of EAA have commented on the inability to provide appropriate deep venous thrombosis prophylaxis or anticoagulation in their patients. Reports in the late 1990s of epidural hematomas associated with low–molecular weight heparin (LMWH) prompted The American Society of Regional Anesthesia and Pain Medicine (ASRA) to address the use of anticoagulation and EAA.134 The ASRA reviewed several studies using therapeutic and/or subtherapeutic anticoagulation with EAA. Therapeutic anticoagulation and epidural anesthesia had been used in 1000 vascular surgery patients treated with either perioperative coumadin (INR >1.5) or with intravenous intraoperative heparin without the development of epidural hematomas. All of these patients had their epidural catheters safely removed > 48 hours.135 Two other large studies of more than 650 orthopedic patients with epidural catheters receiving low-dose coumadin postoperatively had no evidence of epidural hematomas.136,137 The safe use of unfractionated subcutaneous heparin for deep venous thrombosis (DVT) prophylaxis and epidural anesthesia was supported in a review of more than 5000 patients.132 Thus, the safety of both therapeutic anticoagulation and DVT prophylaxis has been affirmed in multiple studies and by the ASRA. In addition, the other noted benefits of improved lower extremity blood flow, anticoagulant properties of local anesthetic, and earlier mobility will likely augment the benefits of anticoagulation.
LMWH deserves particular attention because of the disparity in the literature regarding the risk of epidural hematoma. LMWH was first approved for use in Europe before its release in the United States in 1993. Review of the European experience with epidural anesthesia and LMWH in over 9000 patients reported no bleeding complications associated with LMWH and regional anesthesia.133,137 However, in the United States, there were several reports of hemorrhagic complications during LMWH use. Over a 5-year period between 1993 and 1998, 40 epidural hematomas were reported in association with LMWH, an incidence of approximately 1 in 10,000.139 The reason for the difference between the 2 continents was postulated to be the dosing (higher doses in the USA), timing differences, and the more frequent use of spinals in Europe which carry a lower risk than epidurals. In any case, the higher bleeding complications associated with LMWH and the inability to reverse its effects warrants caution, and the risk of epidural hematoma should be compared with the potential benefits of epidural anesthesia on an individual basis. The ASRA maintains an excellent informative web site, http://www.asra.com/items_of_interest/consensus_statements/index.iphtml, which provides current recommendations regarding the application of regional anesthesia during various forms of anticoagulation.134
OVERALL MORTALITY/COST AND LENGTH OF STAY
As reviewed above, epidural anesthesia and analgesia positively affect several important outcome measures (eg, vascular graft patency, DVT, intestinal ileus). There are few good data, however, to suggest that epidural anesthesia/analgesia result in improved postoperative mortality, cost of care, or hospital length of stay in surgical patients.50,140–143 Retrospective studies have concluded that effective epidural analgesia does affect length of stay. For example, a large retrospective study of 462 consecutive cancer patients undergoing surgery reported that both ICU days (1.3 days versus 2.8 days, P < 0.05) and hospital length of stay (11 days versus 17 days, P < 0.05) were decreased in patients treated with perioperative epidural anesthesia/analgesia compared with those treated with general anesthesia/IV-PCA (Table 1).43 A recent randomized study in patients undergoing colonic surgery reported not only a positive impact on bowel function and intake of food, but also long-lasting effects on exercise capacity and health-related quality of life.16
“Preemptive analgesia” describes the concept of decreasing pain perception and overall analgesic needs after surgery by use of a drug regimen capable of inhibiting CNS sensitization before the application of painful stimuli.144 The hypothesis of preemptive analgesia, therefore, is that blockade of painful stimuli (ie, nociception) by techniques such as regional anesthesia before the surgical stimulus will affect the perception of subsequent painful stimuli.141,145 A recent study reported that preemptive epidural analgesia in patients undergoing radical prostatectomy was associated with significantly decreased postoperative pain not only during hospitalization, but even weeks after discharge.146 Another study has suggested that phantom limb pain might be reduced in patients treated with perioperative epidural anesthesia/analgesia. However, the validity and clinical relevance of preemptive analgesia has been questioned.144,145,147,148 Our review of the literature suggests it is unlikely that any effects of preemptive analgesia translate into clinically relevant long-term improvements in patient satisfaction or outcome.
SUMMARY
This review indicates that the use of intraoperative epidural anesthesia combined with postoperative epidural analgesia is associated with reduction in the incidence and severity of perioperative physiologic perturbations and postoperative morbidity (Table 1). In most cases, thoracic epidural anesthesia/analgesia with local anesthetics administered throughout the perioperative period, beginning before surgical stimulation and continuing for 24–72 hours postoperatively, is essential to maximize these surgical outcome benefits. However, it is emphasized that the combination of epidural opioids and local anesthetics provides synergistic analgesia, provides superior analgesia with activity, and can be accomplished with less toxicity than either class of drugs alone. Reductions in morbidity due to thrombotic complications in complex vascular operations make epidural anesthesia and analgesia the standard of care in these settings. Shortened duration of postoperative ileus after abdominal operations using these techniques undoubtedly will translate into decreased length of stay and patient satisfaction. Can the effects of epidural analgesia on the surgical stress response, thromboembolic complications, immune function, respiratory function, and the cardiovascular system result in objective improvements in outcomes in surgical patients? We believe the answer is “Yes.” Surgeons should become familiar with and embrace this technology, and they should actively participate in the design and conduct of studies that will answer the question posed above.
Footnotes
Reprints: Richard C. Thirlby, MD, Virginia Mason Medical Center, 1100 Ninth Avenue, C6-SUR, P.O. Box 900, Seattle, Washington 98101-0900. E-mail: richard.thirlby@vmmc.org.
REFERENCES
- 1.Liu S, Carpenter RL, Neal JM. Epidural anesthesia and analgesia. Anesthesiology. 1995;82:1474-1506. [DOI] [PubMed] [Google Scholar]
- 2.Grass JA. The role of epidural anesthesia and analgesia in postoperative outcome. Anesthesiol Clin North America. 2000;18:407-428. [DOI] [PubMed] [Google Scholar]
- 3.Park WY, Thompson JS, Lee KK. Effect of epidural anesthesia and analgesia on peri-operative outcome. Ann Surg. 2001;234:560-571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Groban L, Zvara DA, Deal DD, et al. Thoracic epidural anesthesia reduces infarct size in canine model of myocardial ischemia and reperfusion injury. J Cardiothorac Vasc Anesth. 1999;13:579-585. [DOI] [PubMed] [Google Scholar]
- 5.Collins GJ, Barber JA, Zajtchuk R. The effects of operative stress on the coagulation profile. Am J Surg. 1977;133:612-616. [DOI] [PubMed] [Google Scholar]
- 6.Blomberg S, Emanuelsson H, Kvist H, et al. Effects of thoracic epidural anesthesia on coronary arteries and arterioles in patients with coronary artery disease. Anesthesiology. 1990;73:840-847. [DOI] [PubMed] [Google Scholar]
- 7.Davis R, DeBoer LWV, Maroko PR. Thoracic epidural analgesia reduces myocardial infarct size after coronary artery occlusion in dogs. Anesth Analg. 1986;65:711-717. [PubMed] [Google Scholar]
- 8.Blomberg S, Curelaru I, Emanuelsson H, et al. Thoracic epidural anaesthesia in patients with unstable angina pectoris. Eur Heart J. 1989;10:437-444. [DOI] [PubMed] [Google Scholar]
- 9.Smeets HJ, Kievit J, Dulfer FT, et al. Endocrine-metabolic response to abdominal aortic surgery: a randomized trial of general anesthesia versus general plus epidural anesthesia. World J Surg. 1993;17:601-607. [DOI] [PubMed] [Google Scholar]
- 10.Gold MS, DeCrosta D, Rizzuto C, et al. The effect of lumbar epidural and general anesthesia on plasma catecholamines and hemodynamics during abdominal aortic aneurysm repair. Anesth Analg. 1994;78:225-230. [DOI] [PubMed] [Google Scholar]
- 11.Yeager MP, Glass DD, Neff RK, et al. Epidural anesthesia and analgesia in high risk surgical patients. Anesthesiology. 1987;66:729-736. [DOI] [PubMed] [Google Scholar]
- 12.Beattie WS, Buckley DN, Forrest JB. Epidural morphine reduces the risk or postoperative myocardial ischemia in patients with cardiac risk factors. Can J Anaesth. 1993;40:532-541. [DOI] [PubMed] [Google Scholar]
- 13.de Leon-Casasola OA, Lema MJ, Karabella D, et al. Postoperative myocardial ischemia: a pilot project. Reg Anesth. 1995;20:105-112. [PubMed] [Google Scholar]
- 14.Baron JF, Bertrand M, Barre E, et al. Combined epidural and general anesthesia versus general anesthesia for abdominal aortic surgery. Anesthesiology. 1991;75:611-618. [DOI] [PubMed] [Google Scholar]
- 15.Her C, Kizelshteyn G, Walker V. Combined epidural and general anesthesia for abdominal aortic surgery. J Cardiothorac Anesth. 1990;4:552-557. [DOI] [PubMed] [Google Scholar]
- 16.Park WY, Thompson JS, Lee KK. Dept of Veterans Affairs Cooperative Study #345 Study Group. Effect on epidural anesthesia and analgesia on peri-operative outcome. A randomized, controlled Veterans Affairs Cooperative Study. Ann Surg. 2001;234:560-571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tuman KJ, McCarthy RJ, March RJ, et al. Effects of epidural anesthesia and analgesia on coagulation and outcome after major vascular surgery. Anesth Analg. 1991;73:696-704. [DOI] [PubMed] [Google Scholar]
- 18.Christopherson R, Beattie C, Frank SM, et al. The peri-operative ischemia randomized anesthesia trial study group: peri-operative morbidity in patients randomized to epidural or general anesthesia for lower extremity vascular surgery. Anesthesiology. 1993;79:422-434. [DOI] [PubMed] [Google Scholar]
- 19.Rosenfeld BA, Beattie C, Christopherson R, et al. The peri-operative ischemia randomized anesthesia trial study group: the effects of different anesthetic regimens on fibrinolysis and the development of postoperative arterial thrombosis. Anesthesiology. 1993;79:435-443. [DOI] [PubMed] [Google Scholar]
- 20.Bredbacka S, Blomback M, Hagnevik K, et al. Pre- and postoperative changes in coagulation and fibrinolytic variables during abdominal hysterectomy under epidural or general anesthesia. Acta Anaesthesiol Scand. 1986;30:204-210. [DOI] [PubMed] [Google Scholar]
- 21.Modig J, Borg T, Bagge L, et al. Role of extradural and of general anesthesia on fibrinolysis and coagulation after total hip replacement. Br J Anaesth. 1983;55:625-629. [DOI] [PubMed] [Google Scholar]
- 22.Rem J, Feddersen C, Brandt MR, et al. Postoperative changes in coagulation and fibrinolysis independent of neurogenic stimuli and adrenal hormones. Br J Surg. 1981;68:229-233. [DOI] [PubMed] [Google Scholar]
- 23.Kohrs R, Hoenemann CW, Feirer N, et al. Bupivacaine inhibits whole blood coagulation in vitro. Reg Anesth Pain Med. 1999;24:326-330. [DOI] [PubMed] [Google Scholar]
- 24.Borg T, Modig J. Potential antithrombotic effects of local anaesthetics by there inhibition of platelet aggregation. Acta Anaesthesiol Scand. 1985;29:739-742. [DOI] [PubMed] [Google Scholar]
- 25.Orr JE, Lowe GD, Nimmo WS, et al. A haemorheological study of lignocaine. Br J Anaesth. 1986;58:306-309. [DOI] [PubMed] [Google Scholar]
- 26.Rodgers A, Walker N, Schug S, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomized trials. Br Med J. 2000;321:1493-1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001;87:62-72. [DOI] [PubMed] [Google Scholar]
- 28.Fratacc MD. Diaphragmatic shortening after thoracic surgery in humans. Effects of mechanical ventilation and thoracic epidural analgesia. Anesthesiology. 1993;79:654-665. [DOI] [PubMed] [Google Scholar]
- 29.Ford G, Whitelaw W, Rosenal T, et al. Diaphragm function after upper abdominal surgery in humans. Am Rev Respir Dis. 1987;127:431-436. [DOI] [PubMed] [Google Scholar]
- 30.Meyers J, Lembeck L, O’Kane H, et al. Changes in functional residual capacity of the lung after operation. Arch Surg. 1975;110:576-583. [DOI] [PubMed] [Google Scholar]
- 31.Kansard J-L, Mankikian B, Bertrand M, et al. Effects of thoracic epidural blockade on diaphragmatic electrical activity and contractility after upper abdominal surgery. Anesthesiology. 1993;78:63-71. [DOI] [PubMed] [Google Scholar]
- 32.Ballantyne JC, Carr DB, deFerranti S, et al. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized, controlled trials. Anesth Analg. 1998;86:598-612. [DOI] [PubMed] [Google Scholar]
- 33.Wahaba WM, Don HF, Craig DB. Post operative epidural analgesia: effects on lung volume. Can Anaesth Soc J. 1975;22:519-527. [DOI] [PubMed] [Google Scholar]
- 34.Mankikian B, Cantineau JP, Bertrand M, et al. Improvement in diaphragmatic function by a thoracic epidural block after upper abdominal surgery. Anesthesiology. 1988;68:379-386. [DOI] [PubMed] [Google Scholar]
- 35.Reeder MK, Muir AD, Foex P, et al. Postoperative myocardial ischemia: temporal association with nocturnal hypoxaemia. Br J Anaesth. 1991;67:626-631. [DOI] [PubMed] [Google Scholar]
- 36.Rosenberg J, Rasmussen V, von Jessen F, et al. Late postoperative episodic and constant hypoxaemia and associated ECG abnormalities. Br J Anaesth. 1990;65:684-691. [DOI] [PubMed] [Google Scholar]
- 37.Hollenberg M, Mangano D, Browner W, et al. Predictors of postoperative myocardial ischemia in patients undergoing non-cardiac surgery. JAMA. 1992;268:205-209. [PubMed] [Google Scholar]
- 38.Catley D, Thornton C, Jordan C, et al. Pronounced, episodic oxygen desaturation in the postoperative period: it’s association with ventilatory pattern and analgesic regimen. Anesthesiology. 1985;63:20-28. [DOI] [PubMed] [Google Scholar]
- 39.Wheatley R, Somerville I, Sapsford D. Postoperative hypoxaemia: comparison of extradural, I. M. and patient-controlled analgesia. Br J Anaesth. 1990;64:267-275. [DOI] [PubMed] [Google Scholar]
- 40.de Leon-Casasola OA, Parker BM, Lema MJ, et al. Epidural analgesia versus intravenous patient-controlled analgesia: differences in the postoperative course of cancer patients. Reg Anesth. 1994;19:307-315. [PubMed] [Google Scholar]
- 41.Jayr C, Thomas H, Rey A, et al. Postoperative pulmonary complications: epidural analgesia and opioids vs. parenteral opioids. Anesthesiology. 1993;78:666-676. [DOI] [PubMed] [Google Scholar]
- 42.Hjortso NC, Neumann P, Frosig F, et al. A controlled study on the effect of epidural analgesia with local anesthetics and morphine on morbidity after abdominal surgery. Acta Anaesthesiol Scand. 1985;29:705-719. [DOI] [PubMed] [Google Scholar]
- 43.Jayr C, Mollie A, Bourgain JL, et al. Postoperative pulmonary complications: general anesthesia with postoperative parenteral morphine compared with epidural analgesia. Surgery. 1987;104:57-63. [PubMed] [Google Scholar]
- 44.Livingston EH, Passaro EP Jr. Postoperative ileus. Dig Dis Sci. 1990;35:121-132. [DOI] [PubMed] [Google Scholar]
- 45.Carpenter RL. Gastrointestinal benefits of regional anesthesia/analgesia. Reg Anesth. 1996;21:13-17. [PubMed] [Google Scholar]
- 46.Steinbrook RA. Epidural anesthesia and gastrointestinal motility. Anesth Analg. 1998;86:837-44. [DOI] [PubMed] [Google Scholar]
- 47.Lee JT, Taylor BM, Singleton BC. Epidural anesthesia for acute pseudo-obstruction of the colon (Ogilvie’s Syndrome). Dis Colon Rectum. 1988;31:686-691. [DOI] [PubMed] [Google Scholar]
- 48.Ryan P, Schweitzer SA, Woods RJ. Effect of epidural and general anaesthesia compared with general anaesthesia alone in large bowel anastomoses. A prospective study. Eur J Surg. 1992;158:45-49. [PubMed] [Google Scholar]
- 49.Stevens RA, Mikat-Stevens M, Flanigan R, et al. Does the choice of anesthetic technique affect the recovery of bowel function after radical prostatectomy? Urology. 1998;52:213-218. [DOI] [PubMed] [Google Scholar]
- 50.Carli F, Phil M, Mayo N, et al. Epidural analgesia enhances functional exercise capacity and health-related quality of life after colonic surgery. Anesthesiology. 2002;97:540-549. [DOI] [PubMed] [Google Scholar]
- 51.Lui SS, Carpenter RL, Mackey DC, et al. Effects of peri-operative analgesic technique on rate of recovery after colon surgery. Anesthesiology. 1995;83:757-765. [DOI] [PubMed] [Google Scholar]
- 52.Ahn H, Bronge A, Johansson K, et al. Effect of continuous postoperative epidural analgesia on intestinal motility. Br J Surg. 1988;75:1176-1178. [DOI] [PubMed] [Google Scholar]
- 53.Lehman JF, Wiseman JS. The effect of epidural analgesia on the return of peristalsis and the length of stay after elective colonic surgery. Am Surg. 1995;61:1009-1012. [PubMed] [Google Scholar]
- 54.Kapral S, Gollmann G, Bachmann D, et al. The effects of thoracic epidural anesthesia on intra-operative visceral perfusion and metabolism. Anesth Analg. 1999;88:402-406. [DOI] [PubMed] [Google Scholar]
- 55.Sutcliffe NP, Mostafa SM, Gannon J, et al. The effect of epidural blockade on gastric intramucosal pH in the peri-operative period. Anaesthesia. 1996;51:37-40. [DOI] [PubMed] [Google Scholar]
- 56.Johansson K, Ahn H, Lindhagen J, et al. Effect of epidural anaesthesia on intestinal blood flow. Br J Surg. 1988;75:73-76. [DOI] [PubMed] [Google Scholar]
- 57.Sala C, Garcia-Garcia-Granero E, Molina MJ, et al. Effect of epidural anesthesia on colorectal anastomosis. A tonometric assessment. Dis Colon Rectum. 1997;40:958-961. [DOI] [PubMed] [Google Scholar]
- 58.Aitkinhead A, Wishart H, Peebles-Brown D. High spinal nerve block for large bowel anastomosis: a retrospective study. Br J Anaesth. 1978;50:177-183. [DOI] [PubMed] [Google Scholar]
- 59.Schnitzler M, Kilbride MJ, Senagore M. Effect of epidural analgesia on colorectal anastomotic healing and colonic motility. Reg Anesth. 1992;17:143-147. [PubMed] [Google Scholar]
- 60.Kehlet H. General vs. regional anesthesia, In: Rogers MC, Tinker JH, Covino BG, et al, eds. Principles and practice of anesthesiology. St. Louis: Mosby-Year Book, 1993:1218-1234. [Google Scholar]
- 61.Carli F, Webster J, Pearson M, et al. Protein metabolism after abdominal surgery: effects of 24-h extradural block with local anesthetic. Br J Anaesth. 1991;67:729-734. [DOI] [PubMed] [Google Scholar]
- 62.Vedrinne C, Vedrinne JM, Guiraud M, et al. Nitrogen sparing effect of epidural administration of local anesthetics in colon surgery. Anesth Analg. 1989;69:354-359. [PubMed] [Google Scholar]
- 63.Udelsman R. Endocrine and molecular responses to surgical stress. Curr Probl Surg. 1994;8:663-720. [PubMed] [Google Scholar]
- 64.Naito Y, Tamai S, Shingu K, et al. Responses of plasma adrenocorticotropic hormone, cortisol, and cytokines during and after upper abdominal surgery. Anesthesiology. 1992;77:426-431. [DOI] [PubMed] [Google Scholar]
- 65.Udelsman R, Norton FA, Jelenich SE, et al. Responses of the hypothalamic–pituitary-adrenal and renin-angiotensin and the sympathetic system during controlled surgical and anesthetic stress. J Clin Endocrinol Metab. 1987;64:986-994. [DOI] [PubMed] [Google Scholar]
- 66.Hosoda R, Hattori M, Shimada Y. Favorable effects of epidural analgesia on hemodynamics, oxygenation, and metabolic variables in the immediate post anesthetic period. Acta Anesthesiol Scand. 1993;37:469-474. [DOI] [PubMed] [Google Scholar]
- 67.Kehlet H. The stress response to surgery: release mechanisms and modifying effect of pain relief. Acta Chir Scand. 1988;550(suppl):22-28. [PubMed] [Google Scholar]
- 68.Magnusdottir H, Kimo K, Ricksten SE, et al. High thoracic epidural anesthesia does not inhibit sympathetic nerve activity in the lower extremities. Anesthesiology. 1999;91:1299-1304. [DOI] [PubMed] [Google Scholar]
- 69.Cuschieri RJ, Morran CG, Howie JC, et al. Postoperative pain and pulmonary complications: comparison of three analgesic regimes. Br J Surg. 1985;72:495-498. [DOI] [PubMed] [Google Scholar]
- 70.Moller IW, Dinesen K, Sondergard S, et al. Effect of patient-controlled analgesia on plasma catecholamine, cortisol and glucose concentrations after cholecystectomy. Br J Anaesth. 1988;61:160-164. [DOI] [PubMed] [Google Scholar]
- 71.Kehlet H. The surgical stress response: should it be prevented? Can J Surg. 1991;34:565-567. [PubMed] [Google Scholar]
- 72.Tanemura H, Sakata K, Kunieda T, et al. Influences of operative stress on cell-mediated immunity and on tumor metastasis and their prevention by non-specific immunotherapy: experimental studies in rats. J Surg Oncol. 1982;21:189-195. [DOI] [PubMed] [Google Scholar]
- 73.Lundy J, Lovett EJI, Conran P. Halothane, surgery, immunosupression and artificial pulmonary metastases. Cancer. 1978;41:827-830. [DOI] [PubMed] [Google Scholar]
- 74.Pollock RE, Lotzova E, Stanford SD. Mechanism of surgical stress impairment of human peri-operative natural killer cell cytotoxicity. Arch Surg. 1991;126:338-342. [DOI] [PubMed] [Google Scholar]
- 75.Eggermont AMM, Steller EP, Sugarbaker PH. Laparotomy enhances intraperitoneal tumor growth and abrogates the anti-tumor effects of interleukin-2 and lymphocyte activated killer cells. Surgery. 1987;102:71-78. [PubMed] [Google Scholar]
- 76.Yeager MP. Effect of morphine on growth of metastatic colon cancer in vivo. Arch Surg. 1991;126:454-456. [DOI] [PubMed] [Google Scholar]
- 77.Moss NM, Gough DB, Jordan AL. Temporal correlation of impaired immune response after thermal injury with susceptibility of infection in a murine model. Surgery. 1988;104:882-887. [PubMed] [Google Scholar]
- 78.Radosevic-Stasic B, Udovic-Sirola M, Stonjanov L, et al. Growth of allogenic sarcoma in mice subjected to halothane anesthesia and/or surgical stress. Anesth Analg. 1989;69:570-574. [PubMed] [Google Scholar]
- 79.de Leon-Casasola OA. Immunomodulation and epidural anesthesia and analgesia. Reg Anesth. 1996;21(6S):24-25. [PubMed] [Google Scholar]
- 80.Meakins JL. Surgeons, surgery and immunomodulation. Arch Surg. 1991;126:494-498. [DOI] [PubMed] [Google Scholar]
- 81.Davis JM, Albert JD, Tracy KJ, et al. Increased neutrophil mobilization and decreased chemotaxis during cortisol and epinephrine infusions. J Trauma. 1991;31:725-732. [PubMed] [Google Scholar]
- 82.Kehlet H, Thompsen M, Kjaer M, et al. Postoperative depression of lymphocyte transformation response to microbial antigens. Br J Surg. 1977;64:890-893. [DOI] [PubMed] [Google Scholar]
- 83.Redmond HP. Inhibition of neutrophil apoptosis after elective surgery. Surgery. 1999;126:527-534. [PubMed] [Google Scholar]
- 84.Yokoyama M, Itano Y, Mizobuchi S, et al. The effects of epidural block on the distribution of lymphocyte subsets and natural-killer cell activity in patients with and without pain. Anesth Analg. 2001;92:463-469. [DOI] [PubMed] [Google Scholar]
- 85.Hole A, Unsgaard G, Breivik H. Monocyte functions are depressed during and after surgery under general anaesthesia but not under epidural anaesthesia. Acta Anaesthesiol Scand. 1982;26:301-307. [DOI] [PubMed] [Google Scholar]
- 86.Tonnesen E, Wahlgreen C. Influence of extradural and general anaesthesia on natural killer cell activity and lymphocyte subpopulations in patients undergoing hysterectomy. Br J Anaesth. 1988;60:500-507. [DOI] [PubMed] [Google Scholar]
- 87.Stevenson GW, Hall SC, Rudnick S, et al. The effect of anesthetic agents on the human immune response. Anesthesiology. 1990;72:542-552. [DOI] [PubMed] [Google Scholar]
- 88.Moore TC, Spruck CH, Leduc LE. Depression of lymphocyte traffic in sheep by anaesthesia and associated changes in efferent lymph PGE2 and antibody level. Immunology. 1998;63:139-143. [PMC free article] [PubMed] [Google Scholar]
- 89.Salo M. Effect of anaesthesia and surgery on the number of mitogen-induced transformation of T and B lymphocytes. Ann Clin Res. 1978;10:1-13. [PubMed] [Google Scholar]
- 90.Kutza J, Gratz I, Afshar M, et al. The effects of general anesthesia and surgery on basal and interferon stimulated natural-killer cell activity of humans. Anesth Analg. 1997;85:918-923. [DOI] [PubMed] [Google Scholar]
- 91.Markovic SN, Knight PR, Murasko DM. Inhibition of interferon stimulation of natural killer cell activity in mice anaesthesized with halothane or isoflurane. Anesthesiology. 1993;78:700-706. [DOI] [PubMed] [Google Scholar]
- 92.Procopio MA, Rassias AJ, DeLeo JA, et al. The in vivo effects of general and epidural anesthesia on human immune function. Anesth Analg. 2001;93:460-465. [DOI] [PubMed] [Google Scholar]
- 93.Fanning NF, Porter J, Shorten GD, et al. Epidural anesthesia is associated with improved natural killer cell cytotoxicity and a reduced stress response. Am J Surg. 1996;171:68-73. [DOI] [PubMed] [Google Scholar]
- 94.Rem J, Brandt MR, Kehlet H. Prevention of postoperative lymphopenia and granulocytosis by epidural analgesia. Lancet. 1980;1:283-284. [DOI] [PubMed] [Google Scholar]
- 95.Hole A. Pre and postoperative monocyte and lymphocyte functions: effects of sera from patients operated under general or epidural anaesthesia. Acta Anaesthesiol Scand. 1984;28:287-291. [DOI] [PubMed] [Google Scholar]
- 96.Hole A, Unsagaard G. The effect of epidural and general anesthesia on lymphocyte function during and after major orthopaedic surgery. Acta Anaesthesiol Scand. 1983;27:135-141. [DOI] [PubMed] [Google Scholar]
- 97.Riis J, Lomholt B, Haxholdt O, et al. Immediate and long term mental recovery from general versus epidural anesthesia in elderly patients. Acta Anaesthesiol Scand. 1983;27:44-49. [DOI] [PubMed] [Google Scholar]
- 98.Berggren D, Gustafason Y, Eriksson B, et al. Postoperative confusion after anesthesia in elderly patients with femoral neck fractures. Anesth Analg. 1987;66:497-504. [PubMed] [Google Scholar]
- 99.Hole A, Terjesen T, Breivik H. Epidural versus general anesthesia for total hip arthroplasty in elderly patients. Acta Anesthesiol Scanda. 1980;24:279-287. [DOI] [PubMed] [Google Scholar]
- 100.Marcantonio ER, Juarez G, Goldman L, et al. The relationship of postoperative delirium with psychoactive medications. JAMA. 1994;272:1518-1522. [PubMed] [Google Scholar]
- 101.Muravchick S. Anesthesia for the elderly. In: Miller R, ed. Anesthesia, 3rd edn. New York: Churchill Livingstone; 1990:1969-1985. [Google Scholar]
- 102.Ghoneim MM, Hinrichs JV, O’Hara MW, et al. Comparison of psychologic and cognitive functions after general or regional anesthesia. Anesthesiology. 1988;69:507-515. [DOI] [PubMed] [Google Scholar]
- 103.Asbjorn J, Jakobesen BW, Pilegaard HK, et al. Mental function in elderly men after surgery during epidural analgesia. Acta Anesthesiol Scand. 1989;33:369-373. [DOI] [PubMed] [Google Scholar]
- 104.Williams-Russo P, Sharrock NE, Mattis S, et al. Cognitive effects after epidural vs. general anesthesia in older adults. JAMA. 1995;274:44-50. [PubMed] [Google Scholar]
- 105.Hodgson PS, Liu SS, Gras TW. Does epidural anesthesia have general anesthetic effects? Anesthesiology. 1999;91:1687-1692. [DOI] [PubMed] [Google Scholar]
- 106.Handley GH, Silbert BS, Mooney PH, et al. Combined general and epidural anesthesia versus general anesthesia for major abdominal surgery: postanesthesia recovery characteristics. Reg Anesth. 1997;22:435-441. [DOI] [PubMed] [Google Scholar]
- 107.Salomaki TE, Leppaluoto J, Laitinen JO, et al. Epidural vs. intravenous fentanyl for reducing hormonal, metabolic and physiologic responses after thoracotomy. Anesthesiology. 1993;79:672-679. [DOI] [PubMed] [Google Scholar]
- 108.Sydow FW. The influence of anesthesia and postoperative analgesic management on lung function. Acta Chir Scand. 550(suppl):159-168, 1989. [PubMed] [Google Scholar]
- 109.Ready LB, Plumer MH, Haschke RH, et al. Neurotoxicity of intrathecal local anesthetics in rabbits. Anesthesiology. 1985;63:364-370. [PubMed] [Google Scholar]
- 110.Rigler ML, Drasner K, Krejcie TC, et al. Cauda equine syndrome after continuous spinal anesthesia. Anesth Analg. 1991;72:275-281. [DOI] [PubMed] [Google Scholar]
- 111.Albright GA. Cardiac arrest following regional anesthesia with etidocaine and bupivicaine. Anesthesiology. 1979;51:285-287. [DOI] [PubMed] [Google Scholar]
- 112.Auroy Y, Narchi P, Messiah A, et al. Serious complications related to regional anesthesia. Anesthesiology. 1997;87:479-486. [DOI] [PubMed] [Google Scholar]
- 113.Horlocker TT. Regional anesthesia: complications of spinal and epidural anesthesia. Anesthesiol Clin North America. 2000;18:461-485. [DOI] [PubMed] [Google Scholar]
- 114.Borghi B, Casati A, Iuorio S, et al. Frequency of hypotension and bradycardia during general anesthesia, epidural anesthesia, or integrated epidural-general anesthesia for total hip replacement. J Clin Anesth. 2002;14:102-106. [DOI] [PubMed] [Google Scholar]
- 115.Emmett RS, Cyna AM, Andrew M, et al. Techniques for preventing hypotension during spinal anesthesia for caesarean section. Cochrane Database Syst Rev. 2002:CD002251. [DOI] [PubMed]
- 116.Ready LB, Loper KA, Nessly M, et al. Postoperative epidural morphine is safe on surgical wards. Anesthesiology. 1991;75:452-456. [DOI] [PubMed] [Google Scholar]
- 117.Kaneko M, Saito Y, Kirihara Y, et al. Synergistic antinocioceptive interaction after epidural co-administration of morphine and lidocaine in rats. Anesthesiology. 1994;80:137-150. [DOI] [PubMed] [Google Scholar]
- 118.Kehlet H, Dahl JB. The value of multi-modal or balanced analgesia in postoperative pain relief. Anesth Analg. 1993;77:1048-1056. [DOI] [PubMed] [Google Scholar]
- 119.Tanaka K, Watanabe R, Harada T, et al. Extensive applications of epidural anesthesia and analgesia in a university hospital: incidence of complications related to technique. Reg Anesth. 1993;18:34-38. [PubMed] [Google Scholar]
- 120.Stride PC, Cooper GM. Dural taps revisited: A 20 year survey from Birmingham Maternity Hospital. Anaesthesia. 1993;48:247-255. [DOI] [PubMed] [Google Scholar]
- 121.Neal JM. Management of postdural puncture headache, epidural and spinal analgesia and anesthesia: contemporary issues. In: Benumof JL, Bantra MS, eds. Anesthesiology clinics of North America. Philadelphia: WB Saunders; 1993:163-178. [Google Scholar]
- 122.Schneider M, Ettlin T, Kaufmann M, et al. Transient neurologic toxicity after hyperbaric subarachnoid anesthesia with 5% lidocaine. Anesth Analg. 1993;76:1154-1157. [DOI] [PubMed] [Google Scholar]
- 123.Freedman JM, Li D, Drasner K, et al. Transient neurologic symptoms after spinal anesthesia: an epidemiologic study of 1863 patients. Anesthesiology. 1998;89:633-641. [DOI] [PubMed] [Google Scholar]
- 124.Kane RE. Neurologic deficits following epidural or spinal anesthesia. Anesth Analg. 1981;60:150-161. [PubMed] [Google Scholar]
- 125.Weed LH, Wegeforth P, Ayer JB, et al. The production of meningitis by release of cerebral spinal fluid during experimental septicemia. JAMA. 1991;72:190-193. [Google Scholar]
- 126.Bader AM, Gilbertson L, Kirz L, et al. Regional anesthesia in woman with chorioamnionitis. Reg Anesth. 1992;17:84-86. [PubMed] [Google Scholar]
- 127.Darchy B, Forceville X, Bavoux E, et al. Clinical and bacteriologic survey of epidural analgesia in patients in the intensive care unit. Anesthesiology. 1996;85:988-989. [DOI] [PubMed] [Google Scholar]
- 128.Schmidt A, Nolte H. Subdural and epidural hematoma following epidural anesthesia: a literature review. Anaesthesist. 1992;41:276-284. [PubMed] [Google Scholar]
- 129.Tyrba M. Epidural regional anesthesia and low molecular heparin: Pro (German). Anasth Intensivmed Notfallmed Schmerzther. 1993;28:179-181. [DOI] [PubMed] [Google Scholar]
- 130.Sage DJ. Epidurals, spinals and bleeding disorders in pregnancy: a review. Anaesth Intensive Care. 1990;18:319-326. [DOI] [PubMed] [Google Scholar]
- 131.Dahlgren N, Tornebrandt K. Neurologic complications after anesthesia: a follow-up of 18, 000 spinal and epidural anaesthetics preformed over three years. Acta Anaesthesiol Scand. 1995;39:872-880. [DOI] [PubMed] [Google Scholar]
- 132.Schwander D, Bachmann F. Heparin and spinal or epidural anesthesia: decision analysis. Ann Fr Anesth Reanim. 1991;10:284-296. [DOI] [PubMed] [Google Scholar]
- 133.Vandermeulen EP, Van Aken H, Vermylen J. Anticoagulants and spinal-epidural anesthesia. Anesth Analg. 1994;79:1165-1177. [DOI] [PubMed] [Google Scholar]
- 134.Horlocker TT, Benzon HT, Brown DL, et al. Regional anesthesia in the anticoagulated patient - defining the risks [American Society of Regional Anesthesia and Pain Medicine web site]. April 28, 2002. Available at: http://www.asra.com/items_of_interest/consensus_statements/index.iphtml. Accessed February 26, 2003. [DOI] [PubMed]
- 135.Rao TLK, El-Etr AA. Anticoagulation following placement of epidural and subarachnoid catheters: an evaluation of neurologic sequelae. Anesthesiology. 1981;55:618-620. [DOI] [PubMed] [Google Scholar]
- 136.Horlocker TT, Wedel DJ, Schlicting JL. Postoperative epidural analgesia and oral anticoagulant therapy. Anesth Analg. 1994;79:89-93. [DOI] [PubMed] [Google Scholar]
- 137.Wu CL, Perkins FM. Oral anticoagulant prophylaxis and epidural catheter removal. Reg Anesth. 1996;21:517-524. [PubMed] [Google Scholar]
- 138.Bergqvist D, Linblad B, Matzsch T. Low molecular weight heparin for thromboprophylaxis and epidural/spinal anaesthesia: is there a risk? Acta Anaesthesiol Scand. 1992;36:605-609. [DOI] [PubMed] [Google Scholar]
- 139.Horlocker TT, Wedel DJ. Neuroaxial block and low molecular weight heparin: balancing peri-operative analgesia and thromboprophylaxis. Reg Anesth Pain Medicine. 1998;23(suppl 2):164-177. [DOI] [PubMed] [Google Scholar]
- 140.Bradshaw BGG, Lui SS, Thirlby RC. Standardized peri-operative care protocols and reduced length of stay after colon surgery. J Am Coll Surg. 1998;186:501-506. [DOI] [PubMed] [Google Scholar]
- 141.Buggy DL, Smith G. Editorial. Epidural anaesthesia and analgesia: better outcome after major surgery? Growing evidence suggest so. BMJ. 1999;319:530-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Johnstone RE, Martinec CL. Costs of anesthesia. Anesth Analg. 1993;76:840-848. [DOI] [PubMed] [Google Scholar]
- 143.Rigg JR, Jamrozik K, Myles PS, et al. Epidural anesthesia and analgesia and outcome of major surgery: a randomized trial. Lancet. 2002;359:1276-1282. [DOI] [PubMed] [Google Scholar]
- 144.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630-641. [DOI] [PubMed] [Google Scholar]
- 145.McQuay HJ. Editorial. Preemptive analgesia. Br J Anaesth. 1992;69:1-3. [DOI] [PubMed] [Google Scholar]
- 146.Gottschalk A, Smith DS, Jobes DR, et al. Preemptive epidural analgesia and recovery from radical prostatectomy: a randomized controlled trial. JAMA. 1998;279:1076-1081. [DOI] [PubMed] [Google Scholar]
- 147.Bridenbaugh PO. Editorial. Preemptive analgesia - is it clinically relevant? Anesth Analg. 1994;78:203-4. [DOI] [PubMed] [Google Scholar]
- 148.Ko CY, Thompson JE, Alcantara A, et al. Preemptive analgesia in patients undergoing appendectomy. Arch Surg. 1997;132:874-878. [DOI] [PubMed] [Google Scholar]


