Abstract
Objective:
The purpose of this study was to define the association between pretreatment health-related quality of life (HRQL) and surgical complications for patients with colorectal cancer.
Summary Background Data:
For patients with colorectal cancer, surgical complications arise from an interaction between underlying medical comorbidity, colorectal cancer severity, and quality and type of treatment provided. Measurement of HRQL provides a summarization of well-being in the context of medical comorbidity and colorectal cancer severity. The summarization of these factors may be useful in prospective risk assessment of patients about to undergo surgery for colorectal cancer.
Methods:
A single-institution, prospective, cohort study of patients with colorectal adenocarcinoma was performed from August 1, 1999, to March 31, 2002. Before treatment, all participants completed Medical Outcomes Survey SF-36 (SF-36); after the first year of the study, patients also completed the colorectal cancer module of the Functional Assessment of Cancer Therapy survey (FACT-C). Information was collected on demographics, treatment, tumor variables, and complications.
Results:
Ninety-seven patients have undergone open resection of their colorectal cancer. All patients completed SF-36; 65 completed FACT-C. Thirty patients (31%) experienced complications, including 4 (4%) deaths. Age, race, albumin level, American Society of Anesthesia class, specialty surgical training, tumor location, and stage were not associated with complications in univariate analysis. Patients experiencing surgical complications had significantly lower HRQL scores on SF-36 Social Functioning, General Health Perception, and Mental Health Index scales as well as the Mental Health Component summary score. FACT-C Social/Family, Emotional, Functional Well-Being scores, and the Colorectal Cancer Concerns score were also significantly lower for patients sustaining complications. When these HRQL scales were examined in a multivariate model including albumin level, tumor location, and ASA class, SF-36 Social Functioning (Odds Ratio [OR] = 0.98; 95% Confidence Interval [CI] = 0.97–0.99) and FACT-C Colorectal Cancer Concerns (OR = 0.89; 95% CI = 0.79–0.99) scales retained a significant association with complications.
Conclusions:
Pretreatment HRQL scores as measured by several scales of SF-36 and FACT-C were significantly associated with complications. Future studies should concentrate on defining the predictive role of HRQL in determining surgical outcome for patients with colorectal cancer.
A prospective cohort study was performed to identify an association between surgical complications and pretreatment health-related quality of life for patients with colorectal cancer. Surgical complications were independently associated with pretreatment Medical Outcomes Survey Short Form 36 Social Functioning score and Functional Assessment of Cancer Therapy for Colorectal cancer patients Colorectal Concerns score. In both cases, patients with lower scores at diagnosis had a significantly greater chance of experiencing a surgical complication.
Surgery is the primary form of therapy for patients with colon and rectal cancers, yet our understanding of the factors that help predict surgical complications is incomplete. Complications are likely the result of multiple patient-, tumor-, and treatment-related variables. A number of studies have attempted to define these variables. Studies have variously suggested advanced age, rural residence, African-American race, low serum albumin, high American Society of Anesthesia (ASA) classification, tumors located in the rectum, advanced disease stage, emergency surgery, and low surgical and hospital volume may be associated with poor outcomes.1–12 However, many of these variables capture only a single aspect of risk and have shown only a weak association with outcome. Prediction of surgical complications for patients with colorectal cancer is therefore difficult at present.
Health-related quality of life (HRQL) attempts to measure the influence of a patient’s health on his/her well-being. HRQL is traditionally thought of as an outcome. Well-being is, however, defined within the context of several domains, including physical, social, and psychologic functioning.13 As such, these measures may provide a summary of the impact of a patient’s past and present disease status on current well-being. This summary may prove useful in prediction of complications and risk adjustment. The purpose of this study was to test the hypothesis that patients with surgical complications would have significantly lower HRQL scores at the time of diagnosis than patients with uncomplicated postoperative courses.
METHODS
Over the period from August 1, 1999, to March 31, 2002, patients with newly diagnosed, biopsy-proven colorectal carcinoma were enrolled in an IRB-approved, single-institution, prospective cohort study. Before surgical or medical treatment of their colorectal cancers, patients were asked to complete self-administered HRQL questionnaires. All patients completed the Medical Outcomes Study Short Form-36 (SF-36), which investigates generalized HRQL. After the first year of this study, a disease-specific survey was added to this assessment: the Functional Assessment of Cancer Therapy for patients with Colorectal cancer (FACT-C). Both surveys have undergone extensive testing for reliability, validity, and sensitivity to change, and are in widespread use.14,15
The SF-36 is a validated health survey consisting of 36 questions that measure 8 health concepts: physical functioning, role limitations due to physical problems, bodily pain, general health, vitality, social functioning, role limitations secondary to emotional problems, and mental health. Additionally, 2 summary scores are available: a standardized physical component and a standardized mental component. Each summary score is derived from 4 scale scores; the Physical Component score is derived from physical functioning, role limitations due to physical problems, bodily pain, and general health. The Mental Component score is derived from the remaining 4 scales: vitality, social functioning, role limitations due to emotional problems, and mental health. For each participant, a single number derived from his/her responses summarizes each health concept. The scores are calibrated so that a higher score indicates an improved level of function. For example, a high score in the bodily pain category indicates a low level of bodily pain, while a high score in social functioning indicates a high level of social functioning.
The FACT-C is a disease-specific tool that provides more focused information about the impact of colorectal cancer on the patient’s HRQL. The survey consists of 34 questions organized into individual scales: Physical well-being, Social/Family well-being, Emotional well-being, and Functional well-being. These scales are applicable to the experience of all patients with cancer. A fifth scale, Colorectal Cancer Concerns, deals with issues directly related to colorectal cancer and includes questions pertaining to abdominal pain, bowel movements and control, weight, appetite, and body image. Similarly to SF-36, the individual scales are scored according to a standardized algorithm and adjusted such that a higher value is associated with an improved HRQL. Individual scale score may also be summated into a series of overall scores: the FACT-G Total score is equal to the summation of the 4 well-being scores; the FACT-C Total score is equal to the summation of all 5 individual scale scores. Missing scores for individual questions for both surveys were imputed on the basis of the existing responses using defined algorithms.
Demographic information including age, race, and urban versus rural residence was also collected. Disease and comorbid factors including serum albumin level, ASA class, pretreatment carcinoembryonic antigen level (CEA), location of tumor (colon versus rectum), and American Joint Committee on Cancer stage were recorded. In addition, the level of training of the surgeon was noted. Medical comorbidities were recorded according to standardized definitions.
Surgical therapy for patients with colon cancer was performed according to established guidelines.16 For patients with rectal cancer, a combination of clinical examination, endorectal ultrasound, and radiologic imaging was used to determine the appropriateness of preoperative chemotherapy and radiation. Patients with locally advanced tumors (> uT2) were considered for neoadjuvant therapy.
A complication was broadly defined as any event that required treatment measures not routinely employed in the postoperative care of patients having undergone surgery for colorectal cancer. Major complications were defined as any event that resulted in prolonged ICU stay (>48 hours) or return to the ICU or that required invasive intervention to correct. All readmissions to the hospital within 30 days of surgery were considered major complications. Postoperative death included death of a patient who remained hospitalized after colorectal cancer surgery or death occurring within 30 days regardless of the patient’s location.
Univariate analysis of complication rates was performed using the Mann-Whitney U test or χ2 test. Significant factors in univariate analysis were included in stepwise logistic regression models designed to identify variables that were significantly associated with surgical complications. To identify possible confounding, factors previously identified as significantly associated with postoperative complications including ASA class, serum albumin levels, and colon versus rectal location of tumor, were also considered in these models. All statistical analyses were performed using SPSS 10.0.1 (Chicago, IL).
RESULTS
A total of 112 patients were enrolled; 106 patients (95%) underwent surgical therapy. Of the 6 patients who were enrolled and did not undergo surgery, there were 4 who were deemed medically unfit for surgery and 2 who refused the surgical therapy offered. Of the 106 patients surgically treated, 5 have undergone diverting colostomy only, and 4 patients with distal rectal tumors were treated by transanal excision. Thus, there were 97 patients that underwent open surgical resections of their primary tumors. These patients form the basis for this analysis.
Demographic, Tumor, and Treatment Variables
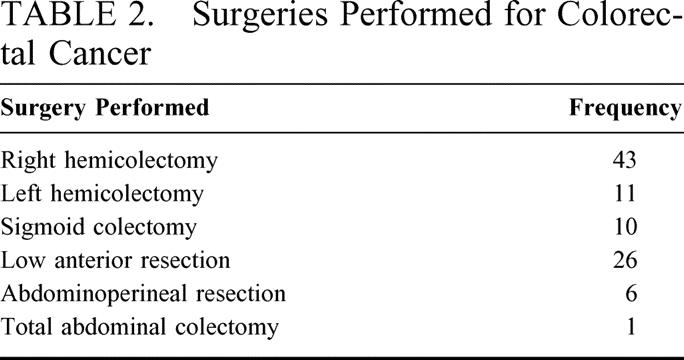
Complete demographic, tumor, and treatment information is available for the entire cohort. There were 3 females and 94 males. This distribution is reflective of the gender bias inherent in the Veteran population treated at our institution. The median age of the cohort was 66 (range, 51–85) years. Most patients were Caucasian and resided in urban settings. Medical comorbidity was common in this cohort of patients: over 25% of these patients had Diabetes Mellitus and/or coronary artery disease documented by cardiac catheterization or prior myocardial infarction documented by electrocardiogram. This high rate of comorbidity is reflected in the ASA classifications of these patients; over 60% were rated as either class III or class IV anesthetic risks. Median value of serum albumin was 3.9 (range, 2.4–4.8) g/dl. Median CEA value was 3.8 (range, 0.2–7076) ng/ml. The majority of patients had either AJCC stage I or II disease. Two patients with rectal cancer had complete pathologic responses to neoadjuvant therapy (2 of 13; 15%). Demographic, tumor, and treatment variables are summarized in Table 1; Table 2 summarizes the surgeries performed.
TABLE 1. Patient, Tumor, and Treatment-Related Factors
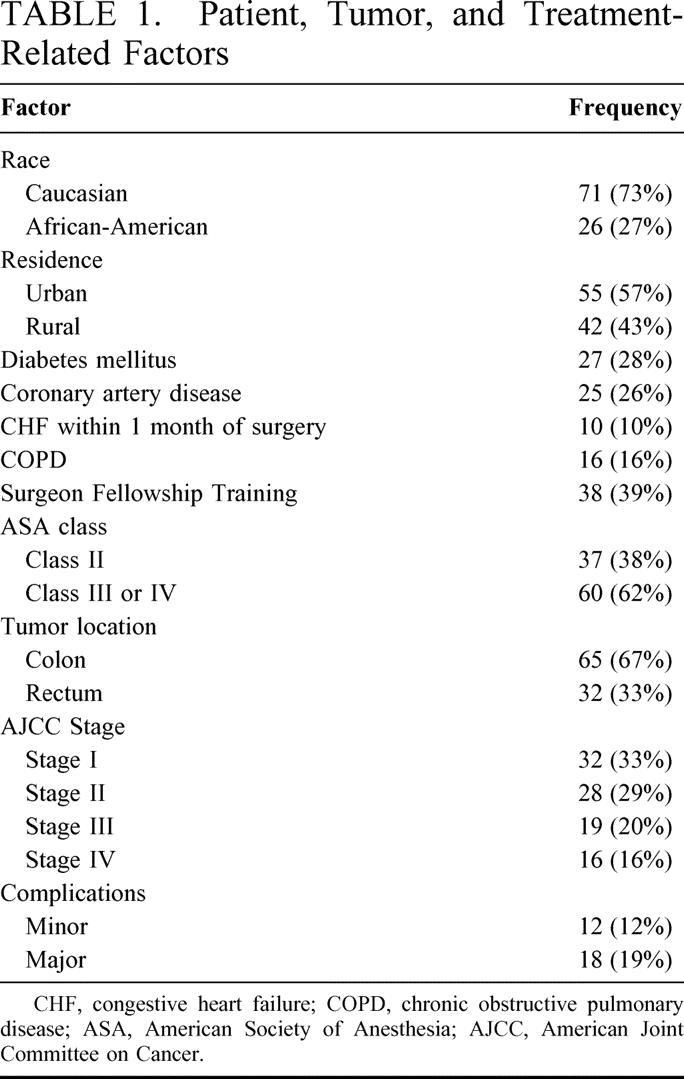
TABLE 2. Surgeries Performed for Colorectal Cancer
SF-36 and FACT-C Scores
Of the 97 patients included in the analysis who were asked to complete SF-36, all 36 questions were completed in 91 cases (94%). For the 65 patients who completed FACT-C, responses to all 34 questions were recorded in 62 cases (95%).
Complications
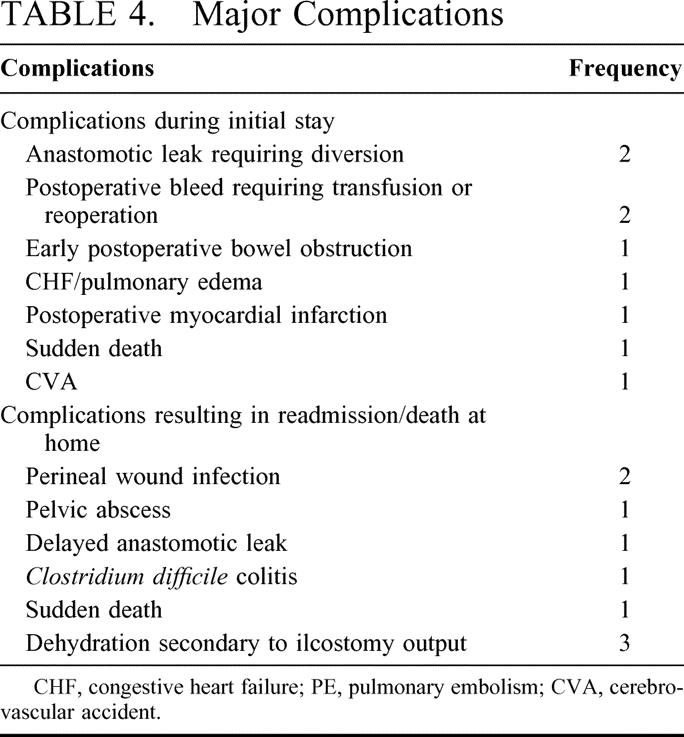
There were a total of 30 (31%) complications including 12 minor and 18 major complications. The majority of the minor complications were infectious in nature. The most common complication overall was superficial wound infection. The majority of major complications were delayed in presentation; major complications resulted in the readmission of 8 patients. Three of these patients were readmitted with dehydration secondary to excessive ileostomy output after creation of this stoma to protect a very low anastomosis. There were 4 deaths (4%) in this series: 2 deaths occurred without antecedent events, 1 patient each died secondary to cerebrovascular accident and multisystem organ failure after anastomotic leak. Major and minor complications are tabulated in Tables 3 and 4.
TABLE 3. Minor Complications
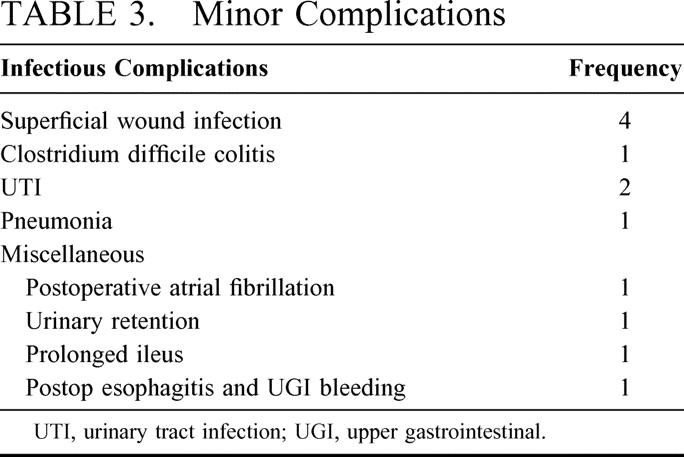
TABLE 4. Major Complications
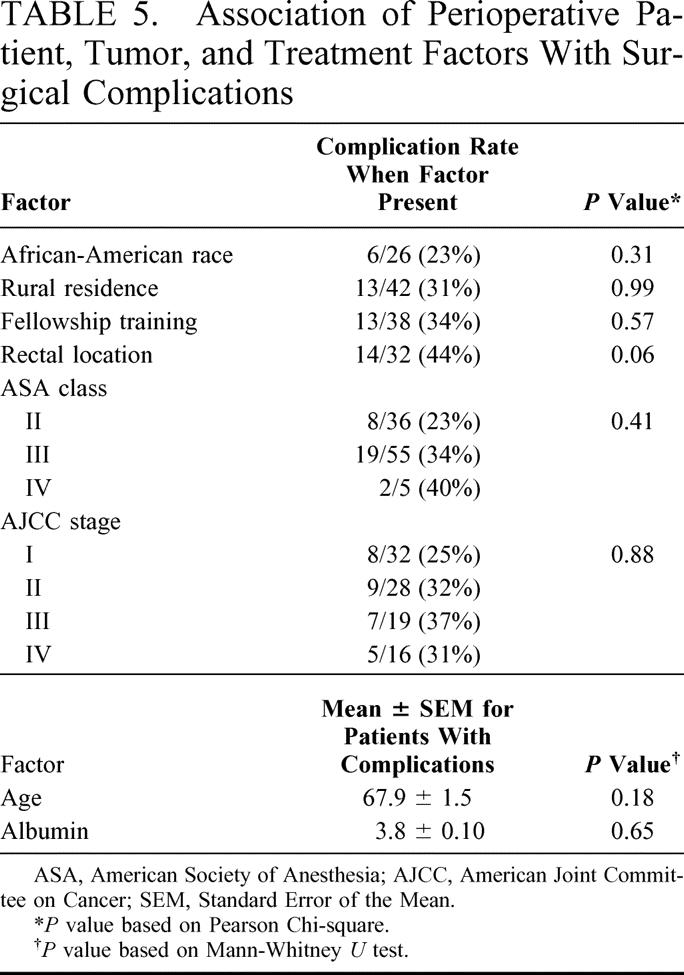
The Association of Perioperative Variables With Surgical Complications
Univariate analysis of perioperative patient-, tumor-, and treatment-related factors did not identify any significant associations between these variables and surgical complications. Table 5 summarizes the comparison between perioperative variables and surgical complications.
TABLE 5. Association of Perioperative Patient, Tumor, and Treatment Factors With Surgical Complications
The Association of Pretreatment HRQL Scores With Surgical Complications
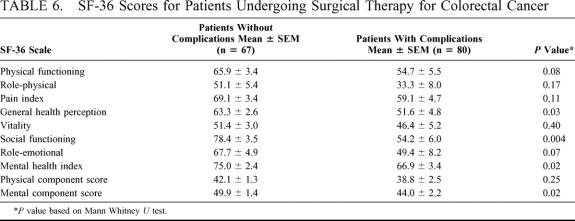
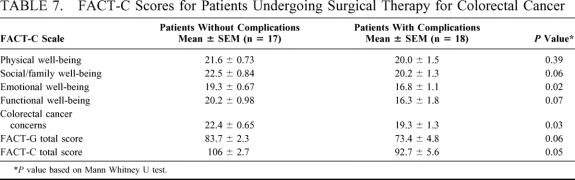
Comparison of both SF-36 and FACT-C scores between patients with surgical complications and those patients with uncomplicated postoperative courses was performed. There were 30 complications in the 97 patients completing SF-36 and 18 complications among the 65 patients completing FACT-C. For each individual scale of SF-36 and FACT-C, patients with complications had lower pretreatment scores than patients without complications. This difference achieved statistical significance for the Social Functioning, General Health Perception, and Mental Health Index scale scores of SF-36, and for the Social/Family, Emotional, and Functional well-being scales, as well as the Colorectal Cancer Concerns scales of FACT-C. Statistically significantly different scores were also noted for the SF-36 Mental Component Score as well as the summary scores of FACT-C (FACT-G Total and FACT-C Total scores). Tables 6 and 7 summarize SF-36 and FACT-C scores for patients undergoing surgical therapy for colorectal cancer.
TABLE 6. SF-36 Scores for Patients Undergoing Surgical Therapy for Colorectal Cancer
TABLE 7. FACT-C Scores for Patients Undergoing Surgical Therapy for Colorectal Cancer
Multivariate Analysis
A stepwise logistic regression analysis was performed using surgical morbidity as the dependent variable. This analysis was designed to test for possible confounding of the relationship identified in univariate analysis between HRQL and surgical morbidity/mortality. In each model, factors that were suggested in previous studies to be significantly associated with surgical complications were considered, along with the pretreatment HRQL scales that were significantly associated with surgical morbidity and mortality in univariate analysis. These factors included serum albumin, tumor location, and ASA class. The analysis first considered SF-36 Social Functioning, General Health Perception, and Mental Health Index scores. These scores were modeled as continuous variables. The SF-36 Social Functioning score was the only factor considered that was independently associated with complications (Odds Ratio [OR] = 0.98, P = 0.02; 95% Confidence Interval [CI] = 0.97–0.99). An improved Social Functioning score was associated with a decreased likelihood of surgical complications. When the analysis was repeated considering the FACT-C scales that were significant in univariate analysis, only the scale dealing with Colorectal Cancer Concerns was independently associated with surgical complications (OR= 0.89, P = 0.03; 95% CI = 0.79–0.99).
DISCUSSION
Surgery is the primary form of therapy for most patients with colorectal cancer. Despite the frequency with which surgery is employed to treat colorectal cancer, little is known concerning the factors that determine the likelihood of surgical complications. Surgical morbidity and mortality for colorectal cancer patients is likely dependent on multiple factors, including colorectal cancer severity, medical comorbidity, and the quality of treatment a patient receives. Prior studies have tended to focus on the quality of therapy as the main determinant of outcome.6–10,17 The role of disease severity and medical comorbidity has received less attention. Furthermore, physicians tend to concentrate on the physicallyobservable factors that determine complications and have discounted the psychosocial aspects that may also contribute to this outcome.18
Measurement of HRQL attempts to quantify the influence of a patient’s health on overall well-being. Multiple domains are considered, including, physical, social, and emotional well-being. Since HRQL comprehensively measures the influence of patient overall health status on well-being, it may also provide a summary measure of current and past disease severity. This summary measure may in turn be useful in the prediction of colorectal cancer surgical morbidity and mortality. To our knowledge, no study to date has tested this hypothesis. A first step in doing so is to identify potential differences in HRQL scores for those patients who sustained complications, compared with those patients who recovered uneventfully. Therefore, the purpose of this study was to identify the potential association between HRQL at the time of diagnosis with surgical outcome.
Increased understanding of the factors that contribute to surgical complications in patients with colorectal cancer may be beneficial on multiple fronts. Complications of surgery for colorectal cancer have obvious negative consequences for the patient, but they also result in considerable institutional costs. For example, surgical complications have a direct effect on length of stay and hospital resource consumption.19–21 Furthermore, public enthusiasm is growing for comparisons of outcomes, including surgical complications, between physicians and institutions. A clear understanding concerning the factors that govern surgical complications is required to properly risk-adjust populations being compared. Proper risk adjustment will allow accurate comparisons concerning differences in therapy rather than differences inherent in the patients.
Knowledge of how individual components of HRQL relate to perioperative complications may also be important with respect to suggesting strategies that could diminish these negative outcomes. For example, in patients with poor preoperative social functioning, early intervention by Social Services may help to decrease morbidity or mortality related to therapy. Similarly, in patients with low scores on the FACT-C Colorectal Cancer Concerns scale (ie, those with weight loss, cramps, loss of bowel control, diarrhea, poor digestion, decreased appetite, or diminished body image) and rectal cancer, initial chemoradiation therapy may be the more appropriate initial therapeutic option than surgery.
The complication rate of 31% in this study is higher than reported in most previous studies, especially given the exclusion of emergency surgical procedures from this cohort. There are several potential explanations for this. First, this study was performed prospectively; complications were recorded as they happened, making loss of this information less likely. Indeed, colorectal cancer surgical complication rates for retrospective studies are generally less that half of those reported for prospective series. The complication rate reported in this series is only marginally higher than the rate reported in other prospective series.8,9,19–21 Second, strict definitions of what constituted surgical morbidity and mortality were used. The inclusiveness of these definitions contributed to the number of complications identified. For example by inclusion of readmissions within 30 days as a major complication, the major complication rate more than doubled. Finally, the reported complication rate represents an unadjusted figure. Complication rates can vary considerably on the basis of the population being considered. The population in this cohort had substantial medical debility; this is reflected in ASA class scores. Over 60% of the cohort was either ASA class III or IV.
We chose to use both SF-36 and FACT-C to broadly survey our cohort. SF-36 offers the advantage of widespread use and familiarity. Since SF-36 is not specific for a particular disease process, it could also allow similar comparisons across other disease processes. The FACT-C survey was added after it had completed testing for reliability and validity.14 We theorized that the FACT-C survey would compliment SF-36, because it would provide more in-depth characterization of the impact of colorectal cancer disease severity on outcome. This appears to be borne out in our analysis, since individual scales of both SF-36 and FACT-C were significantly lower in patients with surgical complications.
While univariate analysis suggested that none of the standard perioperative variables were significantly associated with surgical complications, patients sustaining surgical complications had lower pretreatment scores on each scale of SF-36 and FACT-C. In the cases of SF-36 Social Functioning, General Health Perception, and Mental Health scales, these differences reached statistical significance. Likewise, patients incurring surgical complications had significantly lower scores on FACT-C Social /Family, Emotional, Functional, and Colorectal Cancer Concerns scales. Additionally, the pretreatment SF-36 Mental Component Score and FACT-G and FACT-C Total scores were also significantly lower in those patients with complications after surgery. Multivariate analysis suggested that surgical complications were associated significantly and independently with low scores on SF-36 Social Functioning or FACT-C Colorectal Cancer Concerns. Many of these scales of SF-36 and FACT-C capture information not commonly elicited in routine histories for patients with colorectal cancer. SF-36 Social Functioning scale measures the extent and time that current health is influencing the patient’s normal social interactions. We speculate that normal social functioning is one of the most “elective” aspects of normal well-being and therefore among the first to be altered by a negative change in health. This perhaps explains the finding that among all 8 individual scales of SF-36, only Social Functioning was independently associated with complications. Similarly, patients sustaining surgical complications also had a reduced score on the FACT-C Colorectal Cancer Concerns scale. This scale deals with many of the aspects of normal functioning that can be affected by colorectal cancer. Although many of these questions are part of a routine history for patients with colorectal cancer, they are usually not factored into an assessment of surgical risk. It is likely that taken together, these questions offer an overview of colorectal cancer severity. This information in turn helps predict surgical complications.
This study requires cautious interpretation. The relatively small sample size perhaps accounts for the lack of statistical associations between perioperative variables and complications that had been noted by previous studies. This, however, makes the results of this analysis even more striking; with a small number of patients, there were statistical separations in HRQL scores between those with and without complications. Furthermore, the uniformity of the findings across all scales suggests that our hypothesis is valid and these instruments may add considerably to our ability to understand and eventually to predict surgical complications.
Although this study suggests that patients with complications have lower initial HRQL than patients without complications, many questions remain. First, the small population size did not allow for an assessment of the correlation between pretreatment scores and major complications. Foreknowledge of those patients who would sustain major and potentially life-threatening complications may result in alteration of treatment. For instance, in the case of a patient with metastatic disease, this information may lead to avoidance of surgery altogether. Second, the instruments that were used in this study to measure HRQL were developed primarily to measure changes in HRQL over time, and not to measure risk of surgical complications. It is likely that more precise instruments for this purpose can be developed using subsets of questions from both surveys. Such refinement of instrumentation will lead to a more precise assessment of the relationship between HRQL and surgical complications. Finally, the small size of this cohort also does not allow for an assessment of the possible predicted value of pretreatment HRQL. It is possible that the information obtained from these measures of HRQL may replace or offer adjunctive information to current risk assessment strategies.
In summary, this study has defined the existence of an association between pretreatment HRQL scores and surgical outcome for patients with colorectal cancer. The exact role that this information will play in the prediction of surgical complications remains to be defined by future studies.
Footnotes
Reprints: Thomas Anthony, MD, FACS, Associate Professor of Surgery, University of Texas, Southwestern Medical Center, Chief of Surgical Service, VA North Texas Health Care System, 4500 S Lancaster Rd, Dallas, TX 75216. E-mail: Thomas.Anthony@UTSouthwestern.edu.
REFERENCES
- 1.Colorectal Cancer Collaborative Group. Surgery for colorectal cancer in elderly patients: a systematic review. Lancet. 2000;356:968–974. [PubMed] [Google Scholar]
- 2.Boring CC, Squires TS, Health CW. Cancer statistics for African Americans. CA Cancer J Clin. 1992;42:7–17. [DOI] [PubMed] [Google Scholar]
- 3.Campbell NC, Elliott AM, Sharp L, et al. Rural and urban differences in stage at diagnosis of colorectal and lung cancers. Br J Cancer. 2001;84:910–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dignam JJ, Colangelo L, Tian W, et al. Outcomes among African-Americans and Caucasians in colon cancer adjuvant therapy trials: findings from the National Surgical Adjuvant Breast and Bowel Project. J Natl Cancer Inst. 1999;91:1933–1940. [DOI] [PubMed] [Google Scholar]
- 5.Gervaz P, Bouzourene H, Cerottini JP, et al. Dukes B colorectal cancer: distinct genetic categories and clinical outcome based on proximal or distal tumor location. Dis Colon Rectum. 2001;44:364–372. [DOI] [PubMed] [Google Scholar]
- 6.Harmon JW, Tang DG, Gordon TA, et al. Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Ann Surg. 1999;230:404–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hodgson DC, Fuchs CS, Ayanian JZ. Impact of patient and provider characteristics on the treatment and outcomes of colorectal cancer. J Natl Cancer Inst. 2001;93:501–515. [DOI] [PubMed] [Google Scholar]
- 8.Longo WE, Virgo KS, Johnson FE, et al. Outcome after proctectomy for rectal cancer in Department of Veterans Affairs Hospitals: a report from the National Surgical Quality Improvement Program. Ann Surg. 1998;228:64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Longo WE, Virgo KS, Johnson FE, et al. Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum. 2000;43:83–91. [DOI] [PubMed] [Google Scholar]
- 10.Porter GA, Soskolne CL, Yakimets WW, et al. Surgeon-related factors and outcome in rectal cancer. Ann Surg. 1998;227:157–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Retchin SM, Penberthy L, Desch C, et al. Perioperative management of colon cancer under Medicare risk programs. Arch Intern Med. 1997;157:1878–1884. [PubMed] [Google Scholar]
- 12.Risser DR. Cancer incidence and mortality in urban versus rural areas of Texas, 1980 through 1985. Tex Med. 1996;92:58–61. [PubMed] [Google Scholar]
- 13.Sprangers MA. Quality-of-life assessment in colorectal cancer patients: evaluation of cancer therapies. Semin Oncol. 1999;26:691–696. [PubMed] [Google Scholar]
- 14.Ward WL, Hahn EA, Mo F, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Colorectal (FACT-C) quality of life instrument. Qual Life Res. 1999;8:181–195. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 16.Nelson H, Petrelli N, Carlin A, et al. National Cancer Institute EP. Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst. 2001;93:583–596. [DOI] [PubMed] [Google Scholar]
- 17.Payne JE, Meyer HJ. Independently predictive prognostic variables after resection for colorectal carcinoma. Aust N Z J Surg. 1997;67:849–853. [DOI] [PubMed] [Google Scholar]
- 18.Frost MH, Bonomi AE, Ferrans CE, et al. The Clinical Significance Consensus Meeting group. Patient, clinician, and population perspectives on determining the clinical significance of quality-of-life scores. Mayo Clinic Proceedings. 2002;77:488–494. [PubMed] [Google Scholar]
- 19.O’Brien BD, Brown MG, Kephart G. Estimation of hospital costs for colorectal cancer care in Nova Scotia. Can J Gastroenterol. 2001;15:43–47. [DOI] [PubMed] [Google Scholar]
- 20.Schoetz DJ Jr, Bockler M, Rosenblatt MS, et al. “Ideal” length of stay after colectomy: whose ideal? Dis Colon Rectum. 1997;40:806–810. [DOI] [PubMed] [Google Scholar]
- 21.Tartter PI. Postoperative stay associated with prognosis of patients with colorectal cancer. Ann Surg. 1996;223:351–356. [DOI] [PMC free article] [PubMed] [Google Scholar]