Abstract
Objective:
To compare length of hospital stay, in-hospital complications, in-hospital mortality, and rate of routine discharge between laparoscopic and open appendectomy based on a representative, nationwide database.
Summary Background Data:
Numerous single-institutional randomized clinical trials have assessed the efficacy of laparoscopic and open appendectomy. The results, however, are conflicting, and a consensus concerning the relative advantages of each procedure has not yet been reached.
Methods:
Patients with primary ICD-9 procedure codes for laparoscopic and open appendectomy were selected from the 1997 Nationwide Inpatient Sample, a database that approximates 20% of all US community hospital discharges. Multiple linear and logistic regression analyses were used to assess the risk-adjusted endpoints.
Results:
Discharge abstracts of 43,757 patients were used for our analyses. 7618 patients (17.4%) underwent laparoscopic and 36,139 patients (82.6%) open appendectomy. Patients had an average age of 30.7 years and were predominantly white (58.1%) and male (58.6%). After adjusting for other covariates, laparoscopic appendectomy was associated with shorter median hospital stay (laparoscopic appendectomy: 2.06 days, open appendectomy: 2.88 days, P < 0.0001), lower rate of infections (odds ratio [OR] = 0.5 [0.38, 0.66], P < 0.0001), decreased gastrointestinal complications (OR = 0.8 [0.68, 0.96], P = 0.02), lower overall complications (OR = 0.84 [0.75, 0.94], P = 0.002), and higher rate of routine discharge (OR = 3.22 [2.47, 4.46], P < 0.0001).
Conclusions:
Laparoscopic appendectomy has significant advantages over open appendectomy with respect to length of hospital stay, rate of routine discharge, and postoperative in-hospital morbidity.
The objective of our investigation was to compare outcomes between laparoscopic and open appendectomy based on a large administrative database. Discharge abstracts of over 43,000 patients were used for this analysis. Laparoscopic appendectomy was found to have significant advantages over open appendectomy with respect to length of hospital stay, rate of routine discharge, and postoperative in-hospital morbidity.
The objective of this retrospective study was to compare length of hospital stay, in-hospital complications, in-hospital mortality, and rate of routine discharge between laparoscopic (LA) and open appendectomy (OA) based on a large administrative database. Furthermore, we assessed these endpoints stratified for patients with and without appendiceal abscess or perforation.
Since its introduction by McBurney in 1894, appendectomy has been the treatment of choice for acute appendicitis.1 Appendicitis is the most common intraabdominal condition requiring emergency surgery, with a lifetime risk of 6%.2,3 For more than a century, OA remained the gold standard for the treatment of acute appendicitis. The advent of endoscopic surgery led to the idea of performing LA. In 1981 Semm, a German gynecologist, performed the first LA.4 More than 2 decades later, the benefits of LA are still controversial. Despite numerous case series and small, single-institutional randomized clinical trials comparing LA versus OA, a consensus concerning the relative advantages of each procedure has not yet been reached.5–8 The goal of the present investigation was to compare the effectiveness of LA and OA based on a large administrative database.
MATERIALS AND METHODS
Study Population
Patients with procedure codes for LA or OA were selected from the Nationwide Inpatient Sample (NIS) Release 6, 1997.9 Patients with diagnoses other than appendicitis were excluded from our analysis (Appendix A). The NIS is part of the Healthcare Cost and Utilization Project (HCUP) and contains about 7.1 million discharges (over 8 million procedures) from a sample from over 1000 hospitals in 22 US States. The American Hospital Association definition of “community hospital” (“nonfederal short-term general and other specialty hospitals, excluding hospital units of institutions”) was used to select hospitals for the HCUP database. The NIS was developed by the Agency for Healthcare Research and Quality as a partnership between industry, federal, and state level agencies to analyze trends in health care utilization, cost, quality, and outcomes. The 1997 NIS database provides demographic data, admission and discharge dates, discharge status, preoperative risk factors, postoperative complications, and vital status of patients discharged from US community hospitals during 1997. The procedure and diagnostic codes are classified according to the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9, CM).
The 1997 NIS approximates a 20% stratified sample representative of community hospitals in the United States. Sampling strata were used to create the NIS based on 5 hospital characteristics to ensure maximal representativeness of the US population (geographic region, ownership, location, teaching status, number of beds). Thus, the results of the present analysis can be extrapolated to the entire US patient population undergoing LA and OA in the US during 1997.
Endpoints
Length of Hospital Stay
The length of hospital stay (measured in days) is defined as the difference between date of admission and date of discharge of the patient. Length of stay was coded as 0 for patients discharged during the day of admission.
In-Hospital Complications
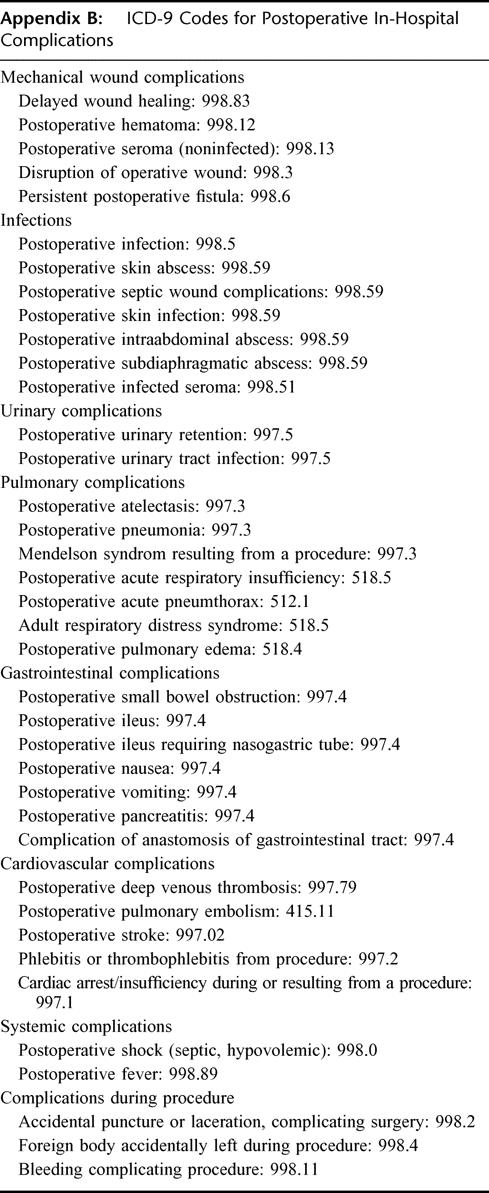
We examined all-cause, nonfatal in-hospital morbidity based on ICD-9 codes. Because the NIS contains inpatient data only, complications occurring after hospital discharge were not included in our analysis. Complications were grouped into 8 categories (mechanical wound complications, infections, urinary complications, pulmonary complications, gastrointestinal complications, cardiovascular complications, systemic complications, complications during procedure; Appendix B).
In-Hospital Mortality
Vital status is a parameter of the NIS database. Because the NIS database contains inpatient data only, deaths occurring after hospital discharge were not included in our analysis.
Rate of Routine Discharge
The NIS provides information about the patient’s discharge status (1, routine discharge; 2, short-term hospital stay; 3, skilled nursing facility; 4, intermediate care; 5, another type of facility; 6, home health care; 7, against medical advice; 8, death). Patients who left the hospital against medical advice (N = 71) and patients who died during hospitalization (N = 107) were excluded when analyzing this specific end point. The remaining patients were grouped into routine discharge (1) versus nonroutine discharge (2–6).
Evaluation of Endpoints Stratified by Presence of Abscess or Perforation
We assessed the endpoints in stratified analyses for patients with (ICD-9 540.0 and 540.1) and without presence of appendiceal perforation or abscess (ICD-9 540.9, 541, and 542). Stratified analyses were performed as the presence of appendiceal perforation or abscess is an important clinical feature and might substantially impact the endpoints.
Covariates
The primary predictor variable in the present investigation was type of procedure (LA vs. OA). Other covariates obtained from the NIS included age, gender, race (white, others), household income (median household income of patient’s ZIP code, 8 categories: 1 = $0-$15,000, 2 = $15,001–20,000, 3 = $20,001–25,000, 4 = $25,001–30,000, 5 = $30,001–35,000, 6 = $35,001–40,000, 7 = $40,001–45,000, 8 = $45,001+), comorbidity (Charlson scale modified by Deyo10,11), hospital volume (total number of discharges per year), location of the hospital (Northeast, Midwest, West, South), teaching status of hospital (rural nonteaching, urban nonteaching, urban teaching hospital), and degree of appendicitis (nonperforated appendicitis without abscess, perforated appendicitis without abscess, appendicitis with abscess).
Statistics
All statistical analyses were performed using Stata version 7.0 (Stata Corporation, College Station, TX) and GNU-R.12 Because the NIS is a stratified probability sample of US community hospitals, calculations were adjusted for survey sampling characteristics (probability weights, cluster sampling, and stratification). We used weights for a 20% sample of the total survey population, stratified for hospital region, ownership, teaching status, and number of beds, and having the hospital as the cluster unit. Differences between laparoscopic and open procedures with respect to baseline sociodemographic, comorbidity, and other predictor variables were tested using t-tests, χ2 tests, and analysis of variance.
Multiple linear regression models were used to examine the risk-adjusted association between the type of appendectomy and length of stay. Length of stay presented as a right-skewed distribution and was thus modeled using both raw length of stay and log-transformed length of stay. Similar results were found and, thus, only the findings using log-transformed length of stay are presented. Risk-adjusted median length of stay were predicted by exponentiating estimated log-transformed length of stay.13 To assess the risk-adjusted impact of the type of procedure (LA vs. OA) on rate of routine discharge, and the occurrence of complications (overall complication rate and specific subsets of complications), we used multiple logistic regression analyses. With the exception of death and cardiovascular complications, all models were adjusted for patient’s comorbidity, age, sex, race, income, appendicitis severity, teaching status and location of the hospital, and hospital volume. The total numbers of deaths and cardiovascular complications (death: N = 107, cardiovascular complications: N = 34) were too small to support multivariate analyses.14
RESULTS
Our database contained information about 46,101 patients who underwent LA or OA. After excluding patients with diagnosis of appendicolithiasis and appendicopathia oxyurica (N = 858) and patients who underwent incidental appendectomies (N = 1486), 43,757 patients remained in our analyses. 7618 patients (17.4%) underwent LA and 36,139 patients (82.6%) underwent OA.
Baseline Characteristics
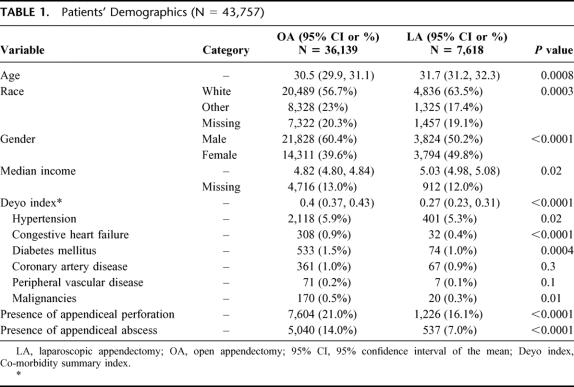
Patients were on average 30.7 years old, predominantly white (58.1%), and male (58.6%). Perforated appendices and appendiceal abscesses were present in 20.2% and 12.7%, respectively. Patients who underwent LA were significantly older (LA: 31.7 years, OA: 30.5 years), more likely white (LA: 63.5% white, OA: 56.7% white), more likely female (LA: 49.8% female, OA: 39.6% female), with higher income (average income class: LA: 5.03, OA: 4.82), and less comorbid (average Deyo index: LA: 0.27, OA: 0.4). Compared with the OA subset, patients undergoing LA had less hypertension, congestive heart failure, diabetes mellitus, malignancies, appendiceal perforation, and appendiceal abscess (Table 1).
TABLE 1. Patients’ Demographics (N = 43,757)
Length of Hospital Stay
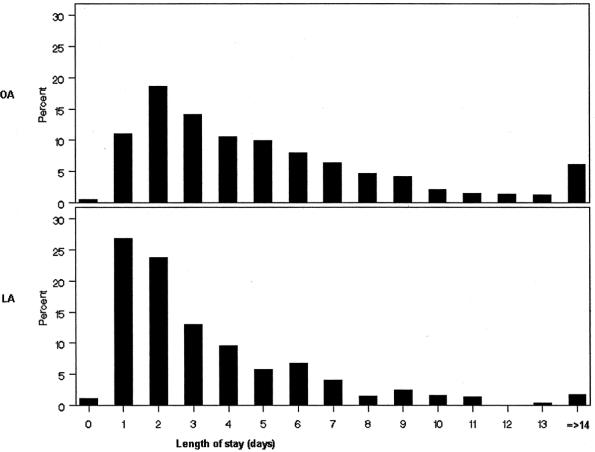
Length of hospital stay ranged from 0 days (N = 482; 131 [1.7%] after LA, 351 [1%] after OA, P < 0.0001) to 345 days (one patient after OA). Seven hundred and eighty-nine patients had a hospital stay equal to or greater than 14 days (46 [0.6%] after LA, 743 [2.1%] after OA, P < 0.0001). The distribution of length of stay for LA and OA is displayed in Figure 1. Sixty-seven percent (72/107) of patients who died had a hospital stay shorter than 14 days, whereas 33% (35/107) had a hospital stay equal to or longer than 14 days. The average length of hospital stay varied significantly between the regions (West: 3.2 days, Midwest: 3.6 days, South: 3.7 days, Northeast: 3.8 days, P < 0.0001). The unadjusted length of stay was significantly shorter after LA (2.6 days after LA, 3.8 days after OA, P < 0.0001).
FIGURE 1. Frequency distribution of length of hospital stay for patients after open (OA) and laparoscopic (LA) appendectomy.
Unadjusted Endpoints
In univariate analyses, LA was associated with lower rate of in-hospital death (0.05% after LA, 0.3% after OA, P = 0.002) and a higher rate of routine discharge of patients (98.4% routine discharge after LA, 95.1% routine discharge after OA, P < 0.0001). The rate of infections (LA: 0.8%, OA: 1.9%, P < 0.0001), gastrointestinal complications (LA: 3.6%, OA: 4.5%, P = 0.002), cardiovascular complications (LA: 0.01%, OA: 0.1%, P = 0.04), and overall complications (LA: 8.7%, OA: 11.1%, P < 0.0001) were significantly lower in patients undergoing LA (Table 2).
TABLE 2. In-Hospital Complications, In-Hospital Death, and Rate of Routine Discharge in Univariate Analyses
Risk-Adjusted Endpoints
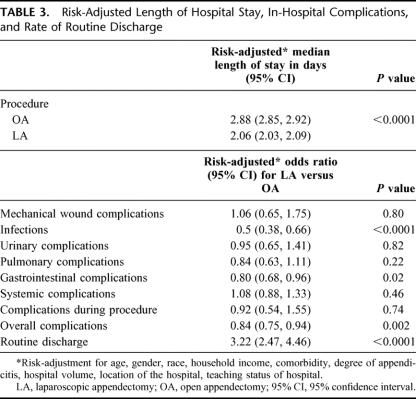
After adjusting for other covariates (Table 3), LA remained associated with shorter median hospital stay (LA: 2.06 days, OA: 2.88 days, P < 0.0001), lower rate of infections (odds ratio [OR] = 0.5 [0.38, 0.66], P < 0.0001), decreased gastrointestinal complications (OR = 0.8 [0.68, 0.96], P = 0.02), lower overall complications (OR = 0.84 [0.75, 0.94], P = 0.002), and higher rate of routine discharge (OR = 3.22 [2.47, 4.46], P < 0.0001).
TABLE 3. Risk-Adjusted Length of Hospital Stay, In-Hospital Complications, and Rate of Routine Discharge
Endpoints Stratified by the Presence of Appendiceal Abscess or Perforation
In stratified analyses (Table 4), length of stay remained significantly shorter (P < 0.0001) and the rate of routine discharge significantly higher (P < 0.0001) for patients undergoing LA, regardless of whether abscess or perforation were present. In-hospital infections were significantly lower in the subset of LA patients without abscess or perforation (0.53 [0.39, 0.73], P < 0.0001), whereas no significant difference between LA and OA was found for patients with abscess or perforation (P = 0.8). No difference was found for the patient subsets with and without perforation or abscess for mechanical wound complications, complications occurring during the surgical procedure, urinary, pulmonary, systemic, and overall complications.
TABLE 4. Risk-Adjusted Endpoints Stratified by the Presence of Appendiceal Abscess and/or Perforation

DISCUSSION
This is the first analysis comparing length of hospital stay, postoperative in-hospital morbidity and mortality, and rate of routine discharge in patients undergoing LA and OA based on data from a large administrative database. In our investigation patients undergoing LA had a significantly shorter median length of hospital stay (LA: 2.06 days, OA: 2.88 days, P < 0.0001) and higher rate of routine discharge (OR = 3.22 [2.47, 4.46], P < 0.0001) compared with OA patients. Patients after LA had significantly less postoperative infections (OR = 0.5 [0.38, 0.66], P < 0.0001), gastrointestinal complications (OR = 0.8 [0.68, 0.96], P = 0.02), and overall complications (OR = 0.84 [0.75, 0.94], P = 0.002).
The question of whether LA decreases the length of hospitalization has been a matter of great debate over the past decade.7,8,15–17 The literature provides contradictory results. Although some recent retrospective cohort studies or chart reviews found LA associated with significantly shorter hospital stay,18–24 other retrospective investigations reported nonsignificant differences.7,25–27 Similarly, some randomized controlled trials associated LA with decreased hospital stay;5,15,28–32 however, others report no significant difference between LA and OA.33–40 Even meta-analyses report controversial findings. Sauerland and associates summarized the results of 28 randomized controlled trials and almost 3000 patients and reported a significant decrease in length of hospital stay in patients undergoing LA.41 Similar results were found by Golub and colleagues,42 whereas another meta-analysis failed to show a statistically significant difference in length of hospital stay between LA and OA.43 The heterogeneity of published results regarding length of hospital stay may be caused by a variety of factors: The current literature describes that the difference may be affected by hospital factors44,45 or social habits,46 rather than reflecting differences resulting from the operative technique itself. Moreover, further discrepancies may arise from diverse health care policies in different countries. For instance, although Hebebrand et al from Germany reported a length of hospital stay of 5.3 days for LA and 7.6 days for OA,28 Mutter and colleagues (UK/France) found 5.3 versus 4.9 days,35 and Minne et al (USA) 1.1 (LA) and 1.2 days (OA).36 The average length of hospital stay in the Minne investigation is considerably shorter than in our analysis. This phenomenon could partially be explained by the fact that the Minne investigation was performed in the western part of the United States where average length of hospital stay is known to be shorter compared with the northeastern, midwestern, or southern regions.9 This was observed as well in our investigation, with significantly shorter hospital stay in the Western United States compared with other regions.
Most retrospective chart reviews, randomized controlled trials, and meta-analyses report similar occurrence in overall postoperative morbidity for LA and OA,15,18–20,25,27,31,32,37,41,47 whereas only a few investigations found statistically significant differences.24,29,30 Some investigations found significantly higher postoperative wound infections after OA,33,34,38,48,49 whereas others reported similar rates.15,28,30,31,35,50 In a recent meta-analysis, Golub and colleagues found a wound infection rate for LA that was less than half the rate in patients undergoing OA.42 Conversely, the authors reported an increase in the rate of intraabdominal abscesses after LA, which failed, however, to reach statistical significance. Other meta-analyses confirm these findings.41,43 Although it can be assumed that the definition of intraabdominal abscess is uniform among different studies, wound infection can be defined with great variability ranging from slight erythema to purulent secretion. This variability strongly influences the rate of reported postoperative wound infections. In the present investigation a lower rate of postoperative infections between the LA and OA group was found (OR = 0.5 [0.38, 0.66], P < 0.0001). It is impossible, however, to disentangle wound infections from intraabdominal abscesses as the ICD-9 codes are identical for both complications (998.59). This is a drawback of our investigation for which we could not adjust. Besides overall complication rate and postoperative infections, the occurrence of gastrointestinal complications was significantly rarer in LA patients (OR = 0.8 [0.68, 0.96], P = 0.02), whereas no difference could be found for pulmonary, urinary, systemic, mechanical wound, and intraoperative complications. Only few studies report pulmonary, gastrointestinal, and urinary complications.16,19,30,32,34,38–40 None of these studies found, however, a significant difference between LA and OA.
In most of randomized clinical trials and chart reviews comparing LA versus OA, no mortality was reported in either group.24,26,30,32,37 This is to be expected because appendicitis is a disease that disproportionally strikes young, healthy people, and appendectomy is a low-risk surgical procedure. In the present investigation the overall mortality rate was 0.24%. This mortality rate is similar to large studies from Sweden (0.24%)51 and Scotland (0.16%).52 In univariate analysis we found a significantly lower percentage of death in patients undergoing LA as compared with OA patients. Adjusting for other covariates was, however, not possible because the number of events in the subset of LA was too low to support multivariable analyses.14
In the present investigation routine discharge was significantly higher in patients undergoing LA versus OA (OR = 3.22 [2.47, 4.46]). Patients after LA were 3 times more likely to be discharged routinely compared with OA patients. To our knowledge, no other study has compared the rate of routine discharge between LA and OA. Some investigations have, however, assessed the impact of the surgical procedure on return to normal activities. Several studies found LA to be associated with significantly earlier return to normal activities compared with OA.15,30,37,48
It has been previously reported that the presence of appendiceal perforation or abscess is associated with poorer outcome.24,31 Most studies, however, did not stratify the findings by the presence of perforation or abscess as their patient numbers were too small for subset analyses. In a large retrospective study, stratified analyses were performed for patients with and without perforation.24 The average length of hospital stay was significantly shorter for LA patients with and without perforated appendicitis. Similar results regarding length of hospital stay were reported by Martin and associates.31 No differences, however, were found in either group for return to normal activity. In our study, median length of stay was shorter (P < 0.0001) and the rate of routine discharge higher (P < 0.0001) for patients undergoing LA, regardless of whether abscess or perforation was present. In-hospital infections were significantly lower in the subset of LA patients without abscess or perforation (0.53 [0.39, 0.73], P < 0.0001). The advantage of LA was, however, lost in patients with abscess and/or perforation (P = 0.8).
Study Limitations and Strengths
We would like to acknowledge the limitations of our study: First, because our investigation is based on a large administrative database, it is possible that some procedures and diagnoses are miscoded. Moreover, as pointed out above, complications, for example, wound infections, can be defined differently and therefore might have been coded and reported differently. It can be assumed, however, that length of hospital stay, discharge status, and vital status were adequately reported as these endpoints are not subject to subjective evaluation. Secondly, the NIS does not allow identifying patients who were converted from LA to OA. In adherence to the intention-to-treat principle, patients who underwent a conversion should be analyzed in the pool of laparoscopic procedures, since the laparoscopic approach was initially chosen. In the present investigation, we were unable to use the intention-to-treat principle, as conversions from LA to OA were coded as OAs. This may have biased our results towards performance of LA. It can be assumed, however, that the percentage of conversions is considerably lower in patients without appendiceal abscess or perforation and that this bias towards LA is less important in this subset of patients. In the present investigation, LA had advantages regarding length of hospital stay and routine discharge regardless of whether or not perforation or abscess were present. Lastly, the NIS allows the assessment of in-hospital morbidity and mortality only. Complications and death that occurred after discharge were not captured in the NIS database. As patients post-LA left the hospital significantly earlier than patients undergoing OA, it could be hypothesized that the rate of complications and death after LA captured in the NIS was falsely low when comparing to OA. It could be argued that the average one day earlier discharge of patients after LA did not considerably influence the rate of postoperative complications and death. Nonetheless, we were unable to adjust for the possible distortion of the findings in complication and mortality rate introduced due to the difference in length of hospital stay between LA and OA patients.
Despite the above-mentioned drawbacks inherent to secondary data analyses, the present investigation has also numerous strengths: The sample size is larger than in any previous publications, enabling us to reach conclusions with great confidence. Equally important, the findings of our analyses are based on “real-world” data because the NIS database is representative of the entire US population and show the effectiveness of LA and OA. This is opposed to the findings of randomized clinical trials for which selection bias potentially threatens external validity, and, at best, represent the therapies efficacy.
CONCLUSIONS
In summary, we have shown that LA has significant advantages over OA with respect to length of hospital stay, rate of routine discharge, and postoperative in-hospital morbidity. This is the first investigation comparing endpoints after LA and OA based on a representative US nationwide database. Our findings may have important health care implications, not only resulting in clinical patient benefit, but also lowering hospital costs. Exponentially increasing health costs have stimulated a massive health care reform effort, seeking cost containment. It is imperative that health-care professionals make fiscally prudent decisions, as the present environment necessitates a critical appraisal of apparently equi-efficacious therapeutic modalities. However, all aspects of LA and OA must be compared, including postoperative pain, patient’s quality of life, days away from work, procedural costs, total costs, and long-term complications. The present investigation is only a first step towards an assessment of all these aspects based on representative US-nationwide patient samples. Further analyses to evaluate the above-mentioned endpoints are required to define whether LA should be considered the treatment of choice for appendicitis.
ACKNOWLEDGMENTS
The authors thank the Swiss National Foundation, Bern/Switzerland, Krebsliga beider Basel, Basel, Switzerland; Freiwillige Akademische Gesellschaft, Basel, Switzerland; and Fondazione Gustav and Ruth Jacob, Aranno, Switzerland, for their financial support of Dr. Guller’s research fellowship.
Appendix A: Inclusion and Exclusion Criteria

Appendix B: ICD-9 Codes for Postoperative In-Hospital Complications
Footnotes
Reprints: Ricardo Pietrobon, MD, Duke University Medical Center, Box 3094 Durham, NC 27710. E-mail: rpietro@duke.edu.
REFERENCES
- 1.McBurney C. The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg. 1894;20:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Samelson SL, Reyes HM. Management of perforated appendicitis in children–revisited. Arch Surg. 1987;122:691–696. [DOI] [PubMed] [Google Scholar]
- 3.Editorial. A sound approach to the diagnosis of acute appendicitis. Lancet. 1987;i:198–200. [PubMed]
- 4.Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59–64. [DOI] [PubMed] [Google Scholar]
- 5.Long KH, Bannon MP, Zietlow SP, et al. A prospective randomized comparison of laparoscopic appendectomy with open appendectomy: clinical and economic analyses. Surgery. 2001;129:390–400. [DOI] [PubMed] [Google Scholar]
- 6.Maxwell JG, Robinson CL, Maxwell TG, et al. Deriving the indications for laparoscopic appendectomy from a comparison of the outcomes of laparoscopic and open appendectomy. Am J Surg. 2001;182:687–692. [DOI] [PubMed] [Google Scholar]
- 7.Peiser JG, Greenberg D. Laparoscopic versus open appendectomy: results of a retrospective comparison in an Israeli hospital. Isr Med Assoc J. 2002;4:91–94. [PubMed] [Google Scholar]
- 8.Fingerhut A, Millat B, Borrie F. Laparoscopic versus open appendectomy: time to decide. World J Surg. 1999;23:835–845. [DOI] [PubMed] [Google Scholar]
- 9.Agency for Healthcare Research and Quality. The Healthcare Cost and Utilization Project Nationwide Inpatient Sample. Release 6, 1997.
- 10.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 11.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 12.Ross I, Gentleman R. A language for data analysis and graphics. J Comp Graph Stat. 5:299–314.
- 13.Rutten-van Molken MP, van Doorslaer EK, van Vliet RC. Statistical analysis of cost outcomes in a randomized controlled clinical trial. Health Econ. 1994;3:333–345. [DOI] [PubMed] [Google Scholar]
- 14.Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–1379. [DOI] [PubMed] [Google Scholar]
- 15.Cox MR, McCall JL, Toouli J, et al. Prospective randomized comparison of open versus laparoscopic appendectomy in men. World J Surg. 1996;20:263–266. [DOI] [PubMed] [Google Scholar]
- 16.Klingler A, Henle KP, Beller S, et al. Laparoscopic appendectomy does not change the incidence of postoperative infectious complications. Am J Surg. 1998;175:232–235. [DOI] [PubMed] [Google Scholar]
- 17.Temple LK, Litwin DE, McLeod RS. A meta-analysis of laparoscopic versus open appendectomy in patients suspected of having acute appendicitis. Can J Surg. 1999;42:377–383. [PMC free article] [PubMed] [Google Scholar]
- 18.Vallina VL, Velasco JM, McCulloch CS. Laparoscopic versus conventional appendectomy. Ann Surg. 1993;218:685–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nazzal M, Ali MA, Turfah F, et al. Laparoscopic appendectomy: a viable alternative approach. J Laparoendosc Adv Surg Tech A. 1997;7:1–6. [DOI] [PubMed] [Google Scholar]
- 20.Heinzelmann M, Simmen HP, Cummins AS, et al. Is laparoscopic appendectomy the new ’gold standard’? Arch Surg. 1995;130:782–785. [DOI] [PubMed] [Google Scholar]
- 21.Johnson AB, Peetz ME. Laparoscopic appendectomy is an acceptable alternative for the treatment of perforated appendicitis. Surg Endosc. 1998;12:940–943. [DOI] [PubMed] [Google Scholar]
- 22.Kurtz RJ, Heimann TM. Comparison of open and laparoscopic treatment of acute appendicitis. Am J Surg. 2001;182:211–214. [DOI] [PubMed] [Google Scholar]
- 23.Agresta F, De Simone P, Michelet I, et al. [The rationale of laparoscopic treatment in acute appendiceal disease]. Chir Ital. 2000;52:171–178. [PubMed] [Google Scholar]
- 24.Richards KF, Fisher KS, Flores JH, et al. Laparoscopic appendectomy: comparison with open appendectomy in 720 patients. Surg Laparosc Endosc. 1996;6:205–209. [PubMed] [Google Scholar]
- 25.Moberg AC, Montgomery A. Appendicitis: laparoscopic versus conventional operation: a study and review of the literature. Surg Laparosc Endosc. 1997;7:459–463. [PubMed] [Google Scholar]
- 26.Apelgren KN, Molnar RG, Kisala JM. Laparoscopic is not better than open appendectomy. Am Surg. 1995;61:240–243. [PubMed] [Google Scholar]
- 27.Fallahzadeh H. Should a laparoscopic appendectomy be done? Am Surg. 1998;64:231–233. [PubMed] [Google Scholar]
- 28.Hebebrand D, Troidl H, Spangenberger W, et al. [Laparoscopic or classical appendectomy? A prospective randomized study]. Chirurg. 1994;65:112–120. [PubMed] [Google Scholar]
- 29.Ozmen MM, Zulfikaroglu B, Tanik A, et al. Laparoscopic versus open appendectomy: prospective randomized trial. Surg Laparosc Endosc Percutan Tech. 1999;9:187–189. [PubMed] [Google Scholar]
- 30.Attwood SE, Hill AD, Murphy PG, et al. A prospective randomized trial of laparoscopic versus open appendectomy. Surgery. 1992;112:497–501. [PubMed] [Google Scholar]
- 31.Martin LC, Puente I, Sosa JL, et al. Open versus laparoscopic appendectomy. A prospective randomized comparison. Ann Surg. 1995;222:256–261; discussion 261—262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Macarulla E, Vallet J, Abad JM, et al. Laparoscopic versus open appendectomy: a prospective randomized trial. Surg Laparosc Endosc. 1997;7:335–339. [PubMed] [Google Scholar]
- 33.Kum CK, Ngoi SS, Goh PM, et al. Randomized controlled trial comparing laparoscopic and open appendicectomy. Br J Surg. 1993;80:1599–1600. [DOI] [PubMed] [Google Scholar]
- 34.Kazemier G, de Zeeuw GR, Lange JF, et al. Laparoscopic vs open appendectomy. A randomized clinical trial. Surg Endosc. 1997;11:336–340. [DOI] [PubMed] [Google Scholar]
- 35.Mutter D, Vix M, Bui A, et al. Laparoscopy not recommended for routine appendectomy in men: results of a prospective randomized study. Surgery. 1996;120:71–74. [DOI] [PubMed] [Google Scholar]
- 36.Minne L, Varner D, Burnell A, et al. Laparoscopic vs open appendectomy. Prospective randomized study of outcomes. Arch Surg. 1997;132:708–711; discussion 712. [DOI] [PubMed] [Google Scholar]
- 37.Frazee RC, Roberts JW, Symmonds RE, et al. A prospective randomized trial comparing open versus laparoscopic appendectomy. Ann Surg. 1994;219:725–728; discussion 728—731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hansen JB, Smithers BM, Schache D, et al. Laparoscopic versus open appendectomy: prospective randomized trial. World J Surg. 1996;20:17–20; discussion 21. [DOI] [PubMed] [Google Scholar]
- 39.Laine S, Rantala A, Gullichsen R, et al. Laparoscopic appendectomy-is it worthwhile? A prospective, randomized study in young women. Surg Endosc. 1997;11:95–97. [DOI] [PubMed] [Google Scholar]
- 40.Tate JJ, Dawson JW, Chung SC, et al. Laparoscopic versus open appendicectomy: prospective randomised trial. Lancet. 1993;342:633–637. [DOI] [PubMed] [Google Scholar]
- 41.Sauerland S, Lefering R, Holthausen U, et al. Laparoscopic vs conventional appendectomy–a meta-analysis of randomised controlled trials. Langenbecks Arch Surg. 1998;383:289–295. [DOI] [PubMed] [Google Scholar]
- 42.Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg. 1998;186:545–553. [DOI] [PubMed] [Google Scholar]
- 43.Garbutt JM, Soper NJ, Shannon WD, et al. Meta-analysis of randomized controlled trials comparing laparoscopic and open appendectomy. Surg Laparosc Endosc. 1999;9:17–26. [PubMed] [Google Scholar]
- 44.Ramesh S, Galland RB. Early discharge from hospital after open appendicectomy. Br J Surg. 1993;80:1192–1193. [DOI] [PubMed] [Google Scholar]
- 45.Lord RV, Sloane DR. Early discharge after open appendicectomy. Aust N Z J Surg. 1996;66:361–365. [DOI] [PubMed] [Google Scholar]
- 46.Millat B, Fingerhut A, Gignoux M, et al. Factors associated with early discharge after inguinal hernia repair in 500 consecutive unselected patients. French Associations for Surgical Research. Br J Surg. 1993;80:1158–1160. [DOI] [PubMed] [Google Scholar]
- 47.Lejus C, Delile L, Plattner V, et al. Randomized, single-blinded trial of laparoscopic versus open appendectomy in children: effects on postoperative analgesia. Anesthesiology. 1996;84:801–806. [DOI] [PubMed] [Google Scholar]
- 48.Ortega AE, Hunter JG, Peters JH, et al. A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy. Laparoscopic Appendectomy Study Group. Am J Surg. 1995;169:208–212; discussion 212—213. [DOI] [PubMed] [Google Scholar]
- 49.Merhoff AM, Merhoff GC, Franklin ME. Laparoscopic versus open appendectomy. Am J Surg. 2000;179:375–378. [DOI] [PubMed] [Google Scholar]
- 50.Henle KP, Beller S, Rechner J, et al. [Laparoscopic versus conventional appendectomy: a prospective randomized study]. Chirurg. 1996;67:526–530; discussion 522. [PubMed] [Google Scholar]
- 51.Blomqvist PG, Andersson RE, Granath F, et al. Mortality after appendectomy in Sweden, 1987–1996. Ann Surg. 2001;233:455–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bisset AF. Appendicectomy in Scotland: a 20-year epidemiological comparison. J Public Health Med. 1997;19:213–218. [DOI] [PubMed] [Google Scholar]