Abstract
Objective:
To evaluate anatomic variations of the biliary tree as applied to living donor liver transplantation.
Summary Background Data:
Anatomic variability is the rule rather than the exception in liver surgery. However, few studies have focused on the anatomic variations of the biliary tree in living donor liver transplantation in relation to biliary reconstruction.
Methods:
From November 1992 to June 2002, 165 patients underwent major hepatectomy with extrahepatic bile duct resection; right-sided hepatectomy in 110 patients and left-sided hepatectomy in 55. Confluence patterns of the intrahepatic bile ducts at the hepatic hilum in the surgical specimens were studied.
Results:
Confluence patterns of the right intrahepatic bile ducts were classified into 7 types. The right hepatic duct was absent in 4 of the 7 types and in 29 (26%) of the 110 livers. Confluence patterns of the left intrahepatic bile ducts were classified into 4 types. The left hepatic duct was absent in 1 of the 4 types and in 1 (2%) of the 55 livers.
Conclusions:
In harvesting the right liver from a donor without a right hepatic duct, 2 or more bile duct stumps will be present in the plane of transection in the graft in 3 patterns based on their relation to the portal vein. Accurate knowledge of the variations in the hepatic confluence is essential for successful living donor liver transplantation.
Living donor liver transplantation (LDLT) is an accepted alternative for patients waiting for cadaveric liver transplantation, especially in countries where the availability of brain-dead donors is severely restricted. The evolution of this procedure has expanded its applicability to the right liver lobe donations.1,2 A precise understanding of general anatomic principles and common variations is the key to safe LDLT. Despite extensive work on the anatomic and technical aspects of LDLT,3 few studies have focused on the anatomic variations of the biliary tree in relation to the safety of bile duct division and reconstruction.4 Misunderstanding of the biliary anatomy can lead to severe postoperative complications.5 Therefore, we studied the anatomic variations of the biliary tree based on our clinical experience with biliary malignancies to enhance the safety of LDLT.
PATIENTS AND METHODS
Between November 1992 and June 2002, 165 patients underwent major hepatectomy with extrahepatic bile duct resection: right-sided hepatectomy (right hepatectomy and right trisectionectomy) in 110 patients and left-sided hepatectomy (left hepatectomy and left trisectionectomy) in 55. Surgical specimens were used for this study.
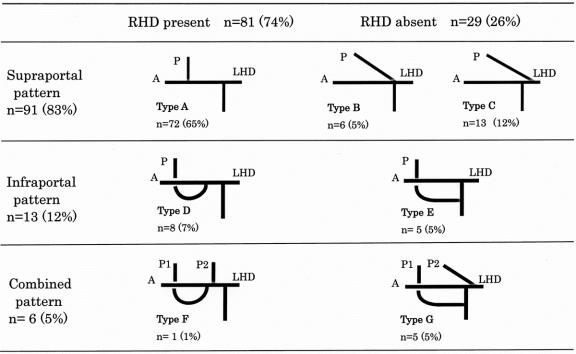
After performing cholangiography on the specimen, the extrahepatic bile duct was opened longitudinally from the distal margin of resection to the proximal margin. The specimen was fixed in 10% formalin for several days and serially sectioned at 5-mm intervals. Intrahepatic segmental and subsegmental ducts and extrahepatic bile ducts were identified on the serial sections according to our classification system, which is similar to Couinaud’s classification.6–8Subsegmental areas of the liver were identified initially, followed by identification of biliary ducts from the subsegmental ducts to the segmental and sectional ducts. The bile ducts in each section was reconstructed three-dimensionally and drawn on a paper two-dimensionally. We refer to this technique as the “pressed flower method.” Histologic extension of cancer along the bile ducts was mapped in each scheme (Fig. 1). Confluence patterns of the bile ducts at the hepatic hilum were determined using these two-dimensional records. Surgical specimens of right-sided hepatectomies (n = 110) were used to study the confluence patterns of the right intrahepatic and extrahepatic bile ducts (the right anterior and posterior sectional bile ducts, and the right and common hepatic ducts). Surgical specimens of left-sided hepatectomies (n = 55) were used to study confluence patterns of left intrahepatic and extrahepatic bile ducts (the left lateral anterior and posterior segmental ducts, the left medial segmental bile duct, and the left and common hepatic ducts).9
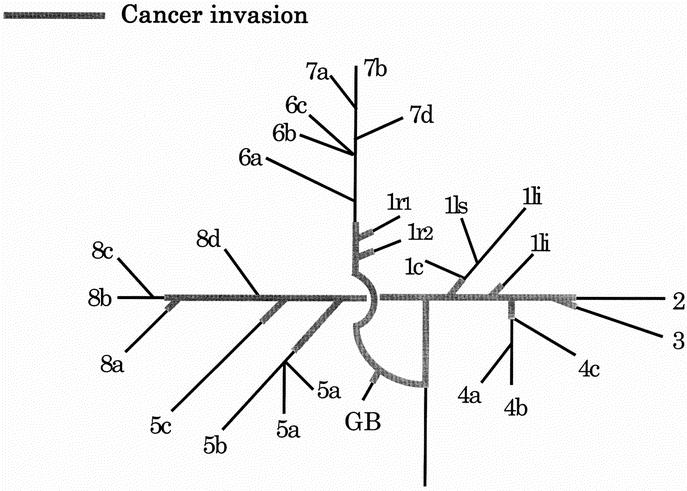
FIGURE 1. Two-dimensional map of the confluence patterns of intrahepatic and extrahepatic bile ducts and cancer extension along the bile ducts (the “pressed flower method”). Numbers refer to the Couinaud’s segment. 1li, left inferior branch; 1ls, left superior branch; 1c, caudate process branch; 1r, right branch; 4a, inferior branch; 4b, superior branch; 4c, dorsal branch; 5a, ventral branch; 5b, dorsal branch; 5c, lateral branch; 6a, ventral branch; 6b, dorsal branch; 6c, lateral branch; 7a, ventral branch; 7b, dorsal branch; 7d, medial branch; 8a, ventral branch; 8b, lateral branch; 8c, dorsal branch; 8d, medial branch; and GB, gallbladder.
RESULTS
Confluence Patterns of the Right Intrahepatic Bile Ducts
Confluence patterns of the right intrahepatic bile ducts were classified into three patterns according to the anatomic relation between the right posterior sectional bile duct and the portal vein (Fig. 2): supraportal pattern (n = 91) in which the right posterior sectional bile duct ran dorsally and cranially to the right or the right anterior portal vein and joined with the distal bile duct at its cranial side; infraportal pattern (n = 13) in which the right posterior sectional bile duct ran ventrally and caudally to the right or the right anterior portal vein and drained into the distal bile duct at its caudal side; and combined pattern (n = 6) in which some parts of the right posterior sectional bile duct entered the distal bile duct supraportally and the remaining parts of the right posterior sectional bile duct joined with the distal bile duct infraportally. The 91 cases of the supraportal pattern were classified into three subtypes (Fig. 3): the right posterior sectional bile duct joined with the right anterior sectional bile duct, forming the right hepatic duct (type A, n = 72); the right posterior sectional bile duct entered the confluence of the right anterior sectional bile duct and the left hepatic duct (type B, n = 6); the right posterior sectional bile duct drained into the left hepatic duct (type C, n = 13). In 1 of the 72 type A cases, a dorsal subsegmental branch of the right anterior inferior bile duct joined with the cystic duct. The 13 cases with the infraportal pattern were classified into two subtypes: the right posterior sectional bile duct joined with the right anterior sectional bile duct, forming the right hepatic duct (type D, n = 8); and the right posterior sectional bile duct entered the common hepatic duct (type E, n = 5). Six cases of a combined pattern also were classified into two subtypes: a portion of the right posterior sectional bile duct joined with the right anterior sectional bile duct infraportally, becoming the right hepatic duct, and the remaining parts of the right posterior sectional bile duct entered the right hepatic duct supraportally (type F, n = 1); and a portion of the right posterior sectional bile duct joined with the common hepatic duct infraportally and the remaining parts entered the left hepatic duct supraportally (type G, n = 5). The right hepatic duct was absent in types B, C, E, and G.
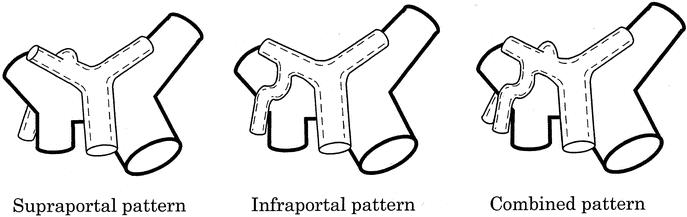
FIGURE 2. The three confluence patterns of the right posterior sectional bile ducts according to their anatomic relationship to the right portal vein.
FIGURE 3. Confluence patterns of the right intrahepatic bile ducts in 110 cases. Supraportal pattern: Type A, the right posterior sectional bile duct (P) joins the right anterior sectional bile duct (A); Type B, P drains into the confluence of A and left hepatic duct (LHD); and Type C, P enters LHD. Infraportal pattern: Type D, P joins A; Type E, P enters the common hepatic duct. Combined pattern: Type F, some elements of the right posterior sectional bile duct (P1) enter A infraportally and the remaining portion (P2) joins A supraportally; and Type G, P joins the common hepatic duct infraportally and P2 joins LHD supraportally. RHD, right hepatic duct.
Confluence Patterns of the Left Intrahepatic Bile Ducts
Confluence patterns of the left intrahepatic bile ducts were classified into four types according to confluence patterns of the left medial sectional bile duct (Fig. 4). The left medial sectional bile duct drained into the left lateral sectional bile duct in type H (n = 43); the left medial sectional bile duct entered the confluence of the left lateral anterior and posterior segmental bile ducts in type I (n = 2); the left medial sectional bile duct joined with the left lateral anterior segmental bile duct in type J (n = 9); the left medial sectional bile duct entered the hepatic confluence in type K (n = 1); and the left hepatic duct was absent in type K. In one case of type J, the left lateral anterior segmental bile duct ran caudally to the umbilical portion of the left portal vein: (type J’).
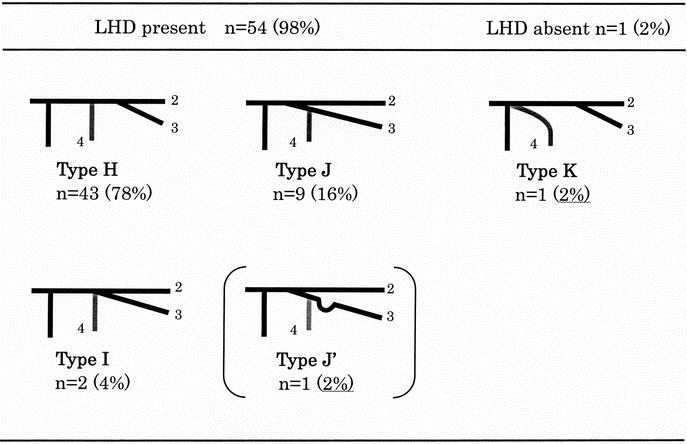
FIGURE 4. Confluence patterns of the left intrahepatic bile ducts in 55 cases. Type H, the left medial sectional bile duct4 enters the left lateral sectional bile duct. Type I, 4 enters the confluence of the left lateral anterior3 and posterior2 segmental bile ducts; Type J, 4 enters 3; Type J’, 3 runs caudally to the umbilical portion of the left portal vein; and Type K, 4 enters the hepatic confluence. LHD, left hepatic duct.
DISCUSSION
Compared with cadaveric liver transplantation, LDLT offers several advantages: a large number of organs available for children; elective basis for transplantation, resulting in lower morbidity, mortality, and overall cost; the absence of primary nonfunction resulting from minimal cold ischemia time and the use of healthy donor; and theoretical immunologic advantages, as suggested by a lower incidence of steroid-resistant rejection.10 Despite these technical and immunologic advantages, biliary complications remain one of the most common problems in LDLT and occur in approximately 30% of the cases.10,11 Careful attention to the bile duct must be paid not only in recipients but also in the donor organ. As anatomic variations of the biliary tree are very common, incomplete appreciation of the segmental biliary anatomy can lead to complications. Although Huang et al12 studied the confluence patterns of the biliary tree using endoscopic retrograde cholangiography, this is the first study to report anatomic variations of the hepatic confluence in relationship to the portal vein using surgical specimens.
As right liver harvesting has become increasingly common,13,14 knowledge of the anatomic variations of the right intrahepatic bile ducts is very important. In the current study, the right hepatic duct was absent in 29 (26%) of the 110 cases. When harvesting a donor without a right hepatic duct, two or more orifices of the bile ducts will be present in plane of transection of the graft. Biliary reconstruction of these variants is complicated and technically difficult. When the supraportal pattern is present (types B, C), the stump of the right posterior sectional bile duct is present cranial to the right anterior portal vein (Fig. 5A). In cases of the infraportal pattern (type E), the orifice opens caudally to the right anterior portal vein (Fig. 5B). In cases of the combined pattern (type G), s tumps are present both cranially and caudally (Fig. 5C). It is essential that both stumps must be reconstructed when they are present. Furthermore, particular care must be taken in harvesting the left liver from a donor with a type C or G variant. As the right posterior sectional bile duct will be divided from the left hepatic duct in these cases, oversight or ligation of the stump of the right posterior sectional bile duct will lead to biliary leakage or obstruction in the donor.
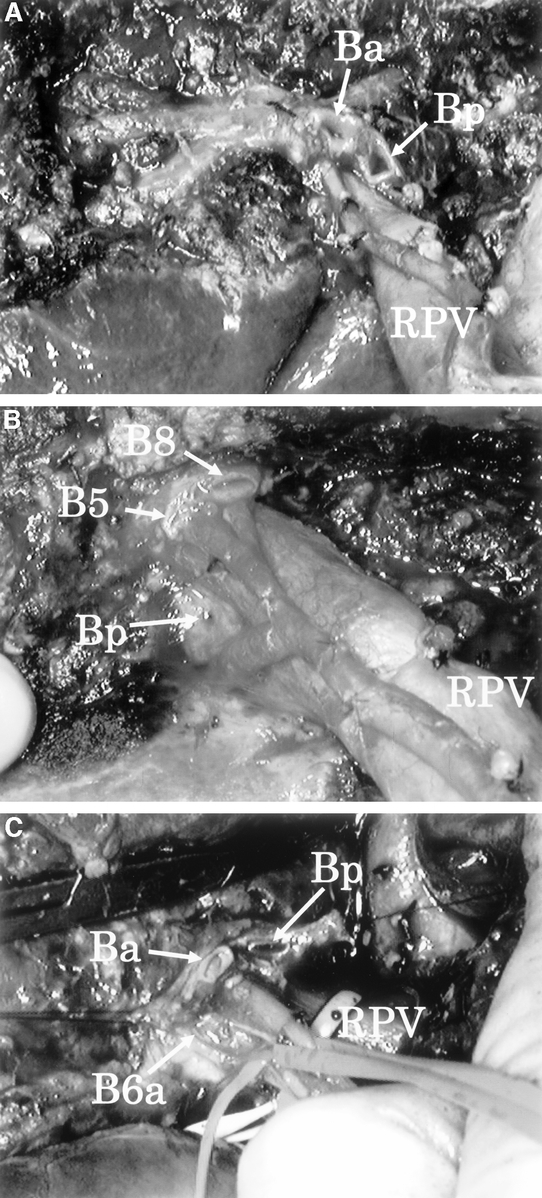
FIGURE 5. Intraoperative photographs of the plane of transection of the liver after left hepatectomy with caudate lobectomy, which is similar to the transection plane of the right liver graft. A: Supraportal pattern. The orifice of the right posterior sectional bile duct (Bp) is opened cranial to the right anterior portal vein. B: Infraportal pattern. Bp is opened caudal to the right anterior portal vein. C: Combined pattern. Stumps are present cranially and caudally to the right anterior portal vein. RPV, right portal vein; Ba, right anterior sectional bile duct; B5, right anterior inferior segmental bile duct; B8, right anterior superior segmental bile duct; and B6a, ventral subsegmental branch of the right posterior inferior segmental bile duct.
Although the confluence pattern of the left intrahepatic bile ducts has been reviewed by Reichert et al,15 they did not encounter the type K variant. When harvesting the left liver from a donor with this rare variant, overlooking the stump of the left medial sectional bile duct will lead to biliary complications. Type J’ also is a rare, but critical, variant. In harvesting the left lateral section from a donor with this variant, stumps of the left lateral posterior and anterior segmental bile ducts are open cranial and caudal to the umbilical portion of the left portal vein, respectively (Fig. 6). The stump of the left lateral anterior segmental bile duct can easily escape the notice.
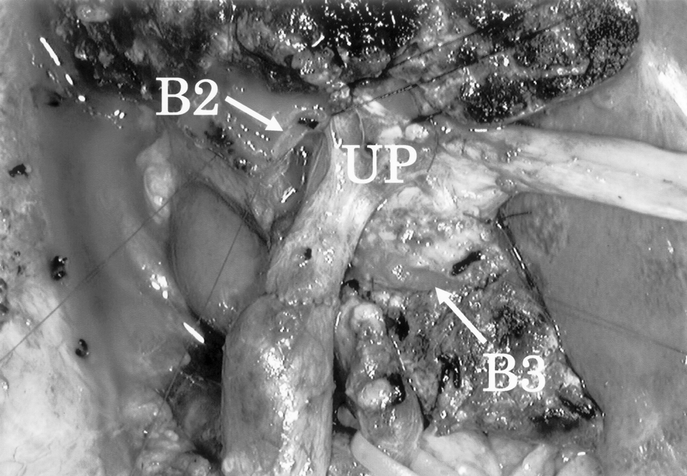
FIGURE 6. Intraoperative photograph of the plane of transection of the liver after right trisectionectomy and caudate lobectomy combined with portal vein resection and reconstruction in a patient with type J’ anatomy. The bile duct stumps can be seen on both sides of the umbilical portion of the left portal vein (UP). B2, left lateral posterior segmental bile duct; and B3, left lateral anterior segmental bile duct.
In LDLT, the biliary anatomy of the donor usually is evaluated using intraoperative cholangiography.1,16 The surgeon must make a snap decision as to the biliary anatomy and its relationship to the line of transection. When the right posterior sectional bile duct drains into the left hepatic duct, it runs supraportally; and when the right posterior sectional bile duct enters the common hepatic duct, it runs infraportally. Familiarity with the variations of the hepatic confluence, especially types B, C, E, G, J’, and K, will decrease the likelihood of surgical misadventure.
Footnotes
Reprints: Yuji Nimura, MD, Division of Surgical Oncology, Department of Surgery, Nagoya University Graduate School of Medicine, 65 Tsurumaicho, Showaku, Nagoya 466–8550, Japan. E-mail: ynimura@med.nagoya-u.ac.jp.
REFERENCES
- 1.Lo CM, Fan ST, Liu CL, et al. Adult-to-adult living liver transplantation using extended right lobe grafts. Ann Surg. 1997;226:261–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kawasaki S, Makuuchi M, Matsunami H, et al. Living related liver transplantation in adults. Ann Surg. 1998;227:269–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Imamura H, Makuuchi M, Sakamoto Y, et al. Anatomical keys and pitfalls in living liver transplantation. J Hepatobiliary Pancreat Surg. 2000;7:380–394. [DOI] [PubMed] [Google Scholar]
- 4.Renz JF, Reichert PR, Emond JC. Biliary anatomy as applied to pediatric living donor and split-liver transplantation. Liver Transpl. 2000;6:801–804. [DOI] [PubMed] [Google Scholar]
- 5.Nagasue N, Kohno H, Matsuo S, et al. Segmental (partial) liver transplantation from a living donor. Transplant Proc. 1992;24:1958. [PubMed] [Google Scholar]
- 6.Nimura Y, Hayakawa N, Kamiya J, et al. Hilar cholangiocarcinoma: surgical anatomy and curative resection. J Hepatobiliary Pancreat Surg. 1995;2:239–248. [Google Scholar]
- 7.Couinaud C. Surgical Anatomy of the Liver Revisited. Paris: Couinaud, 1989. [Google Scholar]
- 8.Nimura Y. Surgical anatomy of the biliary ducts. In: Rossi P, Bezzi M, eds. Biliary Tract Radiology. Berlin: Springer; 1997:21–30. [Google Scholar]
- 9.Strasberg SM, Belghiti J, Clavien P-A, et al. The Brisbane 2000 terminology of liver anatomy and resections. HPB. 2000;2:333–339. [Google Scholar]
- 10.Alonso EM, Piper JB, Echols G, et al. Allograft rejection in pediatric recipients of living related liver transplant. Hepatology. 1996;23:40–43. [DOI] [PubMed] [Google Scholar]
- 11.Heffton TG, Emond JC, Whitington PF, et al. Biliary complications in pediatric liver transplantation. Transplantation. 1992;53:391–395. [DOI] [PubMed] [Google Scholar]
- 12.Huang TL, Cheng YF, Chen CL, et al. Variants of the bile ducts: clinical application in the potential donor of living-related hepatic transplantation. Transplant Proc. 1996;28:1669–1670. [PubMed] [Google Scholar]
- 13.Shiffman ML, Brown RS, Olthoff KM, et al. Living liver transplantation: summary of a conference at the National Institutes of Health. Liver Transpl. 2002;8:174–188. [DOI] [PubMed] [Google Scholar]
- 14.Fan ST, Lo CM, Liu CL. Technical refinement in adult-to-adult living donor liver transplantation using right lobe graft. Ann Surg. 2000;231:126–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reichert PR, Renz JF, D’Albuquerque LC, et al. Surgical anatomy of the left lateral segment as applied to living-donor and split-liver transplantation. Ann Surg. 2000;232:658–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marcos A, Ham J, Fisher R, et al. Surgical management of anatomical variations of the right lobe in living donor liver transplantation. Ann Surg. 2000;231:824–831. [DOI] [PMC free article] [PubMed] [Google Scholar]