Abstract
Objective/Background:
This report describes the first round of results for Phase II of the Alabama CABG Project, a regional quality improvement initiative.
Methods:
Charts submitted by all hospitals in Alabama performing CABG (ICD-9 codes 36.10–36.20) were reviewed by a Clinical Data Abstraction Center (CDAC) (preintervention 1999–2000; postintervention 2000–2001). Variables that described quality in Phase I were abstracted for Phase II and data describing the new variables of β-blocker use and lipid management were collected. Data samples collected onsite by participating hospitals were used for rapid cycle improvement in Phase II.
Results:
CDAC data (n = 1927 cases in 1999; n = 2001 cases in 2000) showed that improvements from Phase I in aspirin prescription, internal mammary artery use, and duration of intubation persisted in Phase II. During Phase II, use of β-blockers before, during, or after CABG increased from 65% to 76% of patients (P < 0.05). Appropriate lipid management, an aggregate variable, occurred in 91% of patients before and 91% after the educational intervention. However, there were improvements in 3 of 5 subcategories for lipid management (documenting a lipid disorder [52%–57%], initiating drug therapy [45%–53%], and dietary counseling [74%–91%]; P < 0.05).
Conclusions:
In Phase II, this statewide process-oriented quality improvement program added two new measures of quality. Achievements of quality improvement from Phase I persisted in Phase II, and improvements were seen in the new variables of lipid management and perioperative use of β-blockers.
During Phase II of the Alabama Coronary Artery Bypass Grafting Project, the performance of two new variables improved (appropriate lipid management and perioperative use of beta-blocking drugs). Moreover, the achievements from Phase I persisted in Phase II, indicating that the effects of this project were durable for 2 years. Partnership between a regional Quality Improvement Organization and surgeons is a model for quality improvement that may be useful for other surgical specialties.
The Alabama Coronary Artery Bypass Grafting (CABG) Project is a statewide voluntary process-oriented quality improvement initiative. Alabama’s Quality Improvement Organization (QIO) (Alabama Quality Assurance Foundation [AQAF]) has collaborated with physicians on this project since its inception in August 1995. Funding for the project was provided by a contract with the Centers for Medicare and Medicaid Services (CMS), formerly known as the Health Care Financing Administration.
Preliminary work on this project included defining process and outcome variables, and establishing criteria for chart abstraction by a Clinical Data Abstraction Center (CDAC). In Phase I, arrangements were made for the collection of data from another state that does not provide performance feedback to practitioners (comparison state) and a national sample of CABG patients supplied by the CMS. Phase I began with the collection and analysis of baseline data that described individual hospital and aggregate statewide performance for the process and outcome variables that were chosen by the study committee,1 followed by an intervention aimed at decreasing the duration of post-CABG mechanical ventilation. Duration of ventilation was the process variable chosen to be the basis of an educational initiative for three reasons. The regional performance lagged behind the comparison state, the duration of ventilation seemed amenable to improvement by a regional educational initiative, and shortening the duration of ventilation was likely to improve patient outcomes and lower the cost of the CABG operation.
Phase I was completed after the postintervention data were collected and analyzed. The results were presented to participants at a meeting in September 1999 and were later published.2 The educational intervention was temporally associated with a profile of favorable changes in the duration of mechanical ventilation (the target variable), prevalence of internal mammary artery use, and prevalence of aspirin prescription at discharge that was not matched by secular trends measured in a comparison state or a national sample. Moreover, these improvements were achieved without an increase in adverse events (eg, reintubation, bleeding complications, readmission to intensive care unit, use of intra-aortic balloon pump). Risk-adjusted mortality was significantly lower in Alabama after the intervention than before; however, this improvement was not significantly better than improvements in risk-adjusted mortality that were found in the national and comparison state samples.2
The present report describes the first round of results for Phase II of the Alabama CABG Project. In Phase II, the list of quality indicators from Phase I was increased to include variables describing perioperative use of β-blockers and appropriate lipid management during the admission for CABG surgery. The purpose of the present analysis is twofold: 1) to define the durability of the improvements that were achieved in Phase I, and 2) to determine if the program of measurement/education/remeasurement that was used in Phase I of this study can be successfully expanded to two more processes of care in CABG surgery.
METHODS
Overview
The Alabama CABG Project and its Phase I findings are described in detail elsewhere.1,2 Briefly, a project study group consisting of cardiothoracic surgeons, cardiologists, and AQAF staff identified indicators that measure the quality of care delivered to CABG patients. In Phase I, baseline performance on these quality indicators was measured for each hospital in Alabama where CABG surgery is performed, followed by an intervention that provided feedback on performance and suggested means for improvement. Performance was again measured after this intervention. Changes in performance across Alabama were compared with changes in a comparison state where no educational intervention had been performed, and to changes observed in a national sample. The same cycle of baseline data collection, educational intervention, and follow-up data collection was used in Phase II of the study where the variables of β-blocker utilization and lipid management became the focus of the statewide quality improvement effort. Comparison state and national sample data were not available for the present analysis of Phase II.
Quality Indicators
The quality indicators for Phase I were as follows: aspirin therapy at discharge, use of the internal mammary artery for myocardial revascularization, duration of intubation after CABG, intraoperative use of an intra-aortic balloon pump, reoperation for excessive bleeding, readmission rate to the intensive care unit (ICU) after ICU discharge, hospital readmission rate within 30 days of discharge, and risk-adjusted in-hospital mortality. The processes in the analysis were considered as indicated in all CABG patients unless a specific contraindication was documented in the chart. A list of the contraindications for these quality indicators was previously published.1
In Phase II, the variables of perioperative β-blocker use and appropriate lipid management were added. As in Phase I, the processes in the analysis were considered as indicated in all CABG patients unless a specific contraindication was documented in the chart. The aggregate variable perioperative β-blocker use included any one of the following: use of β-blocking drugs prior to surgery, during the operation, or following CABG surgery. The aggregate variable appropriate lipid management included three subvariables: measurement of lipids during admission or planned following discharge, documenting the presence or absence of a lipid disorder in the patient chart, and initiating drug or dietary therapy for lipid management during the hospitalization or planning for such therapy after discharge.
Physicians chose the quality indicators to represent optimal practices for CABG surgery. In most instances (eg, IMA use, β-blocker use, and lipid management), the information regarding the benefits of the indicator to patient survival is compelling.3–9 Other variables (eg, median post-CABG intubation time) are less well established but have sufficient evidence of providing benefit that they were accepted as quality indicators by consensus of the physician panel.10–12
Achievable Benchmarks of Care13,14 were defined in both phases of the Alabama CABG Study. The mean performance for all hospitals in the state was another benchmark. In Phase I of this project, performance in a comparison state and in a national sample of CABG patients was used to distinguish the effect of the educational intervention from contemporary secular trends in cardiac surgery. Secular trends were not measured in this portion of Phase II, although data from a comparison state are currently being collected for the final Phase II analysis.
The Achievable Benchmark of Care for a specific quality or quality control indicator is unique because it represents the average for the top 10% of performers among Alabama hospitals for the variable with adjustments for patient volume13 (also see http://www.main.uab.edu/show.asp?durki=11311). The Achievable Benchmark of Care sets higher standards than the average performance, yet the standards are realistic goals for centers striving for excellence.
Project Samples and Data Collection
Data for this analysis included Medicare patients, who had isolated CABG procedures (ICD-9 codes 36.10–36.20, excluding diagnostic-related group [DRG] 104, 105, and 468). Phase II baseline (January 1, 1999 to June 30, 1999; n = 1927 patients) and postintervention samples (January 1, 2000 to June 30, 2000; n = 2001 patients) were collected by a CDAC of the CMS. In addition to the CDAC samples for Phase II, 2-week samples of data were collected at participating hospitals using software supplied to the individual hospital quality improvement teams by the AQAF and the CMS (MedQuest; Fu Associates; Arlington, VA). These samples were taken in November 2000 (n = 161 patients from all 21 hospitals), February 2001 (n = 120 patients from 20 of 21 hospitals), May 2001 (n = 352 patients from 17 of 21 hospitals), and August 2001 (n = 74 patients from 19 of 21 hospitals). The variables examined included β-blocker use and lipid management.
Project Intervention
Each of the Alabama hospitals providing CABG agreed to participate in this project and identified a CABG quality improvement team for the hospital. AQAF staff organized meetings of all the teams. These meetings each lasted 1 day and took place in a central location (Birmingham).
The first meeting for Phase I was held in January 1997, with the purpose of describing the CABG project’s objectives and methods to the participants. Results from the initial round of data analysis, ie, baseline data covering CABG operations performed between July 1, 1995 and June 30, 1996, were presented at a second meeting in January 1998. At the third meeting in July 1998, the goal of decreasing the duration of post-CABG mechanical ventilation was presented. Suggestions were given on how this goal could be achieved.
The Phase II study variables and the MedQuest data acquisition software were introduced at a meeting in September 1999. The first Phase II follow-up meeting took place 1 year later. As with the other meetings, every hospital’s quality improvement team was given its own facility’s performance compared with statewide mean performance, as well as the other facilities’ anonymous performances. Graphs depicting statewide performance for all the CDAC and MedQuest data samples were also presented in Phase II. Attendance at the meeting ranged from 120 to 175 people and included anesthesiologists, surgeons, nurses, physician assistants, perfusionists, and respiratory therapists who were members of local quality improvement teams.
In Phases I and II, suggestions were made for implementing quality improvement programs at local hospitals. Teleconferences, which included presentation of MedQuest data in Phase II, were held to discuss the progress of teams at each hospital. Project updates and educational materials were periodically mailed to local quality improvement teams. Hospital quality improvement teams were given software for onsite data collection (MedQuest) and instructions for rapid cycle improvement initiatives.
Educational materials include newsletters, books, videotapes, and posters that explain quality improvement in general terms, explain the rationale for the interventions of the CABG Project (early extubation, β-blocker use, and lipid management), and give suggestions on implementation. Keynote speakers were chosen for the regional meetings to describe the background of the educational initiative or quality improvement in general.
Three “train the trainer” sessions were held in Phase II of the CABG Project in an effort to boost performance for early post-CABG extubation at individual hospitals. These sessions were sponsored by the AQAF and held at different locations (one each in northern, central, and southern Alabama). Nurses and respiratory therapists were asked to attend. Continuing educational units were offered to those completing the session. Information describing the CABG Project is available to members of local quality improvement teams and the public on the AQAF website (http://www.aqaf.com/).
A member of the AQAF staff made on-site visits at participating hospitals to consult on local improvement efforts and monitor interim progress. Hospitals were encouraged, but not required, to participate in comparative process analysis visits, which were modeled after the round-robin site visits previously used by the Northern New England Cardiovascular Disease Study Group.15 Typically, the visiting surgeons would watch cardiac operations during the morning, while other team members observed and spoke with their counterpart at the host hospital. At the end of the visit, the host and visiting teams met to answer any questions that had arisen regarding the procedures and processes of care used by the host hospital. Within 1 month of the visit, the visiting team completed a written summary that described similarities and differences in the hospitals’ approaches to CABG surgery. Thirteen different Alabama hospitals participated in at least one comparative process analysis visit.
Data Analysis
The change from baseline to year 2000 CDAC samples for process and outcome variables was compared by χ2 tests for discrete variables and by nonparametric analysis of variance (Kruskal-Wallis) for continuous variables (SAS Institute, Inc; Cary, NC). Baseline for the variables describing lipid management, β-blocker use, length of stay, same-day surgery, and mortality was the 1999 CDAC data (ie, baseline data for Phase II). The rest of the quality and quality control indicators were compared with the 1995 CDAC data (ie, baseline data for Phase I).
RESULTS
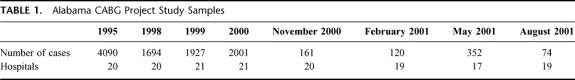
Table 1 displays the number of cases contained in each data sample. Data samples abstracted by the CDAC had more than 1000 CABG patients, while the data that were gathered by individual hospitals using the MedQuest software included fewer cases.
TABLE 1. Alabama CABG Project Study Samples
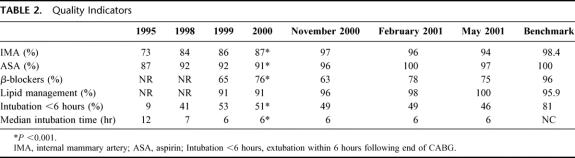
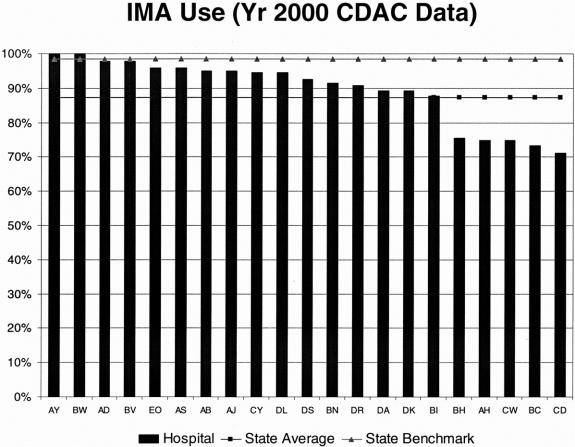
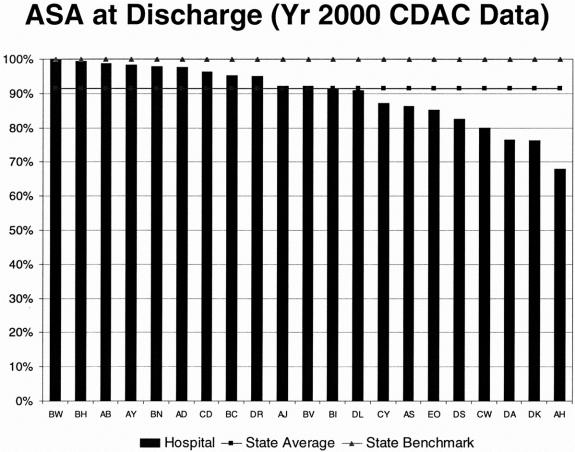
The quality indicators are shown in Table 2. The prevalence of IMA use and prescription of ASA at discharge increased from the baseline measurement in 1995 and remained improved in the most recent CDAC and MedQuest data samples. The variability in IMA use and prescription of ASA at discharge among individual hospitals in Alabama decreased during Phase I of the study;2 however, a degree of variability between individual hospital rates for these variables persisted in the most recent CDAC sample (Figs. 1 and 2). In all reports of the CDAC data, individual hospital performance was displayed relative to the statewide average as well as the Achievable Benchmark of Care. By definition, roughly 90% of hospitals fell below the Achievable Benchmark of Care. The aim of this benchmark is to show what can be achieved by the best hospitals in the region rather than to show the mean performance for the variable.
TABLE 2. Quality Indicators
FIGURE 1. Prevalence of internal mammary artery utilization in the year 2000 CDAC sample is shown. Letters on the x-axis are anonymous indicators for individual Alabama hospitals.
FIGURE 2. Prevalence of aspirin prescription at hospital discharge in the year 2000 CDAC sample is shown. Letters on the x-axis are anonymous indicators for individual Alabama hosptials.
β-blocker use and lipid management as shown in Table 2 are aggregate variables describing the perioperative application of β-blockers or appropriate lipid management according to at least one of the categories listed in Tables 3 and 4. The aggregate variables and specific subvariables convey different information. For instance, appropriate use of β-blockers during the CABG admission improved from 65% to 76% of patients undergoing CABG (P < 0.001; 1999 vs. 2000 CDAC samples) with similar results in two of the three MedQuest samples. However, Table 4 indicates that the prevalence of β-blocker use during hospitalization did not change significantly from 1999 to 2000 for two of the three β-blocker variables. The difference between aggregate and specific variables for β-blocker use was due to more patients receiving β-blockers at some time during their CABG admission in the year 2000 CDAC sample.
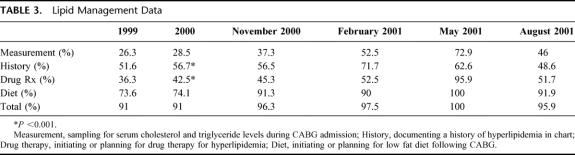
TABLE 3. Lipid Management Data
TABLE 4. β-Blocker Use

Lipid management was appropriate according to aggregate the lipid management variable in 91% of cases for the year 1999 and 91% of the year 2000 CDAC abstractions, and there were higher rates in the MedQuest data samples. It is noteworthy that the lipid management variables in Table 3 reveal substantial improvements from 1999 to 2000 in obtaining a history of hyperlipidemia and initiating therapy for hyperlipidemia.
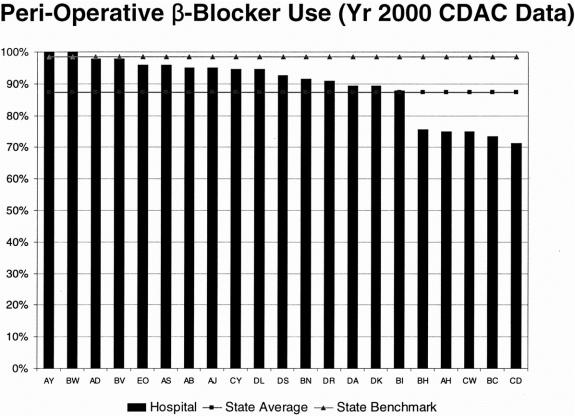
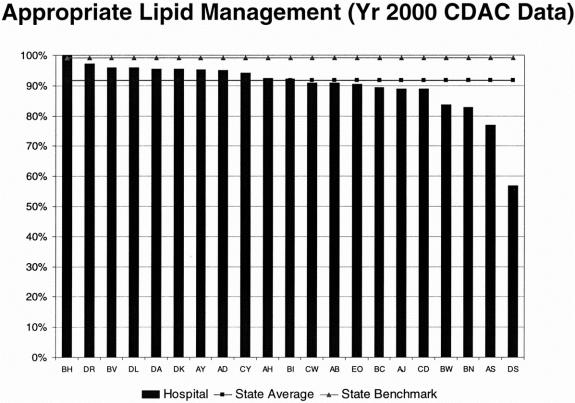
As with the other quality improvement variables, there is still room for improvement in β-blocker use and lipid management at the individual hospital level. The variability for these quality indicators across the participating Alabama hospitals is shown with the mean hospital performance and Achievable Benchmark of Care in Figures 3 and 4.
FIGURE 3. Prevalence of β-blocker use in the peri-operative interval for the year 2000 CDAC sample is shown. Letters on the x-axis are anonymous indicators for individual Alabama hospitals.
FIGURE 4. Prevalence of appropriate lipid management in the year 2000 CDAC sample is shown. Letters on the x-axis are anonymous indicators for individual Alabama hospitals.
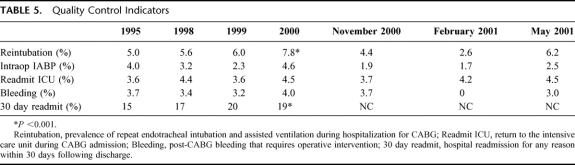
The quality control indicators in Table 5 were chosen to measure complications related to CABG and monitor for potential adverse effects due to the project interventions (eg, the measurement of reintubation rate is a control for overly aggressive extubation following CABG). In Table 5, a 2.8% increase in the prevalence of reintubation was noted (P < 0.001; 1995 vs. 2000 CDAC data). It is possible that this statistically significant, but clinically modest, increase is related to the shorter intubation times that were measured in the 1998, 1999, and 2000 CDAC samples.
TABLE 5. Quality Control Indicators
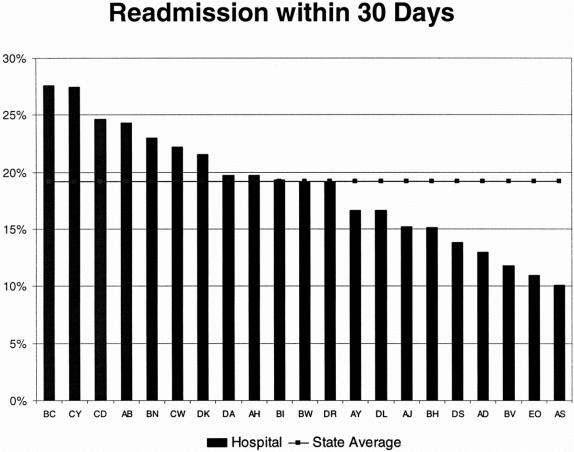
The prevalence of intraoperative intra-aortic balloon pump use and ICU readmission were similar across time. The prevalence of 30-day readmission was as much as 5% higher in the CDAC samples following the baseline recording in 1995 (P > 0.001; 1995 vs. 2000 CDAC samples). This trend was concerning in view of the decreasing length of hospitalization as noted in Table 6, and an analysis of readmission was undertaken for the 2000 CDAC sample. The prevalence of 30-day readmission varied across individual Alabama hospitals, with 7 hospitals having a 30-day readmission rate <20% in the CDAC sample for 2000 (Fig. 5). The DRG codes for all readmissions were gathered. The most common readmission diagnosis was heart failure and shock (DRG 127 in 21% of readmissions), followed by other circulatory system disorders (DRG 144 in 11% of readmissions) and arrhythmias (DRGs 138 and 139 in 10% of readmissions). Postoperative infection (DRG 418) accounted for 6% of readmissions, and respiratory illness (pneumonia DRG 089 and other respiratory system diagnoses DRG 101) occurred in 7% of readmissions. The major disease categories (MDCs) were similarly weighted to cardiopulmonary disease. Circulatory system (MDC 05) accounted for 42% of readmissions, and respiratory system (MDC 04) accounted for 21% of readmissions. Infectious disease (MDC 18) accounted for 11% of readmissions.
TABLE 6. Outcome Data
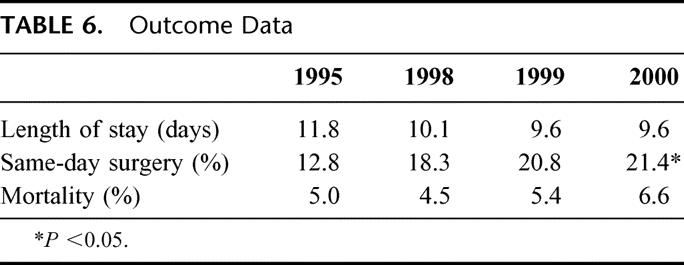
FIGURE 5. The rate of readmission to any hospital within Alabama within 30 days following discharge post-CABG surgery is illustrated for the individual hospitals participating in the study.
Table 6 includes outcome data. The duration of hospitalization for CABG decreased by 2.2 days over Phases I and II of the study. The prevalence of same-day surgery increased by 8.6%. In Phase I of the study (1995–1998), there was a decrease in the risk-adjusted mortality for CABG surgery in Alabama. However, the risk-adjusted mortality as well as the decrease in adjusted mortality between the two data samples in Alabama was not significantly different from secular trends that were measured in the national sample or comparison state.2 The 6.6% mortality in the 2000 CDAC sample is not adjusted for risk and is higher than it was previously.
DISCUSSION
The Alabama CABG Project is a collaborative effort between the physicians in Alabama and the state QIO. The AQAF is physician directed and has expertise in organizing regional quality assessment and improvement projects. The funding for this project was obtained through a contract between the HCFA and the AQAF. Statistical expertise for analyzing results in Phase I of the study was drawn from in-house staff at the AQAF and from collaboration with participating investigators at UAB and Duke University. We think that such a collaborative effort between physicians, a QIO with experience in the field of quality assessment/improvement, and experts in clinical research can be successfully implemented in other regions and for other surgical disciplines. Collaboration between a specialty group like cardiothoracic surgeons and a physician-led regional QIO is ideally suited to provide useful information at a reasonable cost. Nevertheless, it is not clear at present where funding will come from for similar regional quality improvement projects in cardiac surgery. This remains one of the challenges for regions embarking on quality improvement initiatives.
In the present study, the improvements in quality indicators that were achieved in Phase I of the project were maintained during Phase II. This suggests that it may be possible to drop or rotate variables examined by a quality improvement project as the project moves forward without sacrificing gains that were previously made. A strategy of changing or rotating quality indicators in and out of the study is one method to contain the cost of data abstraction and analysis, and generally make the process of quality improvement more efficient.
In Phase II of the Alabama CABG Project, variables describing β-blocker use and lipid management were added. The choice of these variables was based on literature indicating that their uniform application to patients undergoing CABG would provide short- and/or long-term benefits. Randomized control trials that quantify the effect of an intervention are the gold standard for defining regional improvement initiatives, but we recognized that the number of randomized control trials in cardiac surgery is small. Thus, recommendations for the practice guidelines in the present study were based primarily on evidence from retrospective analyses or nonrandomized trials, together with consensus among practicing physicians regarding the intervention’s potential for improving patient outcome. The scarcity of secure information for designing study interventions in cardiac surgery makes the collection of other variables that monitor for possible adverse consequences of the intervention imperative.
The new indicators of lipid management and β-blocker use are more difficult to characterize as discrete variables than the quality indicators previously included in the project (eg, prescription of ASA at discharge and IMA use). The committee decided to use aggregate variables (Table 2) composed of discrete subvariables (Tables 3 and 4) to describe these processes of care. The data indicate that there were improvements in β-blocker use and lipid management during the period of this study. However, there is clearly room for further improvement, for instance, by achieving uniform application of each specific subvariable to every patient (Tables 3 and 4). When hospital performance for the aggregate variables is examined (Figs. 3 and 4), further opportunities for improvement are apparent at the individual hospital level. For instance, lipid management was appropriate in at least one subcategory for 91% of Alabama patients in the 1999 and 2000 CDAC samples. However, there were 7 hospitals in Alabama where >10% of patients had no lipid testing, counseling, or treatment during their admission for CABG surgery (year 2000 data).
Other interesting findings in Phase II came from analysis of the quality control indicators. There has been a slow but steady increase in the prevalence of reintubation since emphasis was placed on early (<6 hours) extubation after CABG surgery. The increase in reintubation was not associated with a consistent increase in the duration of hospitalization or ICU readmission rate; however, this trend bears continued observation during the remainder of Phase II.
The 30-day hospital readmission rate has risen by 4% to 5% since the inception of the project. This was associated with a decrease in the duration of hospitalization following CABG surgery in Alabama and warrants further scrutiny, especially in view of the most common reasons for hospital readmission (cardiopulmonary diseases including heart failure and arrhythmias).
Others16–18 have addressed the tradeoff between earlier discharge from an acute care hospital and subsequent events such as death or hospital readmission. It has also been noted that a shorter duration of stay in an acute care hospital may be associated with an increased utilization of skilled nursing facilities and rehabilitation centers,16 although this is not always the case.17 In a previous study by Cowper et al of patients who had CABG in 1992,18 it was shown that the early discharge of elderly patients was not associated with an increase in the 60-day hospital readmission rate. Indeed, among all patients who were discharged within 5 days post-CABG, the risk-adjusted rates of death and readmission for cardiovascular disease were less than in patients with a longer hospital admission. A complete consideration of this issue is beyond the scope of the present paper and is an important topic. The answer will require risk adjustment for the length of stay variable,19,20 together with more complete information describing the reasons for rehospitalization.
The Alabama CABG Project provides information describing individual hospital performance to practitioners (surgeons, nurses, and other members of the local quality improvement and CABG provider teams) in a confidential manner under protection as peer review material. We believe that confidentiality is important to gain the confidence and support of providers because it shows by actions that the project is aimed primarily at improvements in care rather than punishing outliers. The question of how to reconcile the public right to review data describing quality improvement, and the benefits of protecting the confidentiality of peer review information has yet to be resolved.21 However, the present study shows that maintaining the confidentiality of this peer-review information did not render the project ineffective in improving the quality of care for CABG patients. It is interesting that the public release of surgeon-specific mortality data in New York State did not influence the referral patterns of cardiologists or the pattern of hospital utilization by patients,22,23 although it was associated with a decrease in risk-adjusted mortality for CABG surgery in New York.24 Furthermore, the finding that risk-adjusted CABG mortality data have less to do with the choice of CABG providers by third party payers than what the providers are willing to pay argues against the need for these data to guide the purchasing of healthcare services.25
Data collected on-site at participating hospitals using the MedQuest software were included for the first time in Phase II of the Alabama CABG Project. Professional off-site data abstraction in Phases I and II were provided by a CMS-approved CDAC on a fee-for-service basis. There are advantages and disadvantages to each approach. For example, the accuracy of abstraction was checked in the CDAC data by reabstraction of data samples, while there was no mandatory quality control program for locally acquired MedQuest data. However, the process of chart copying followed by abstraction and reporting from the CDAC required several months for completion and is expensive as compared with the smaller locally acquired data samples.
The primary purpose of gathering MedQuest data was to provide local quality improvement teams with timely information for rapid cycle improvement. In the present study, the MedQuest data mirrored the CDAC data, suggesting that voluntary data collection is adequate for rapidly determining the effect of quality improvement initiatives at the local level. The large samples abstracted by a CDAC are subjected to stringent quality control, which makes them more suitable for comparisons with other regional or national data samples.
The Alabama CABG Project continues to use the Achievable Benchmark of Care concept to stimulate improvements in clinical care. In a randomized controlled trial separate from the Alabama CABG Project, the inclusion of Achievable Benchmarks of Care in physician feedback led to 33% to 57% higher odds of patients receiving appropriate care as compared with patients whose physicians did not have this information.14 The desire to perform at the level of the best centers is expected to accelerate regional process improvement in the Alabama CABG Project, although this was not tested in the present study.
During the remainder of Phase II of the Alabama CABG Project, further analysis of post-CABG hospital readmissions is planned, as is continued surveillance of readmission within 30 days of CABG. Data are now being collected by a comparison state that does not provide formal feedback to practitioners, thus providing a control for secular trends in cardiac surgery. Individual hospitals in Alabama will continue to use MedQuest data for ongoing rapid cycle improvement efforts in Phase II. Confidential process-oriented reports for individual surgeons will be added to the hospital-level reports. Charts describing surgeon performance according to quartiles or quintiles will be included in this report. In addition, tracking variables that describe blood product utilization (erythrocyte and nonerythrocyte) and postoperative physician follow-up within 2 weeks after discharge from CABG will be collected and reported to participants.
REFERENCES
- 1.Holman WL, Peterson ED, Athanasuleas CL, et al. Alabama coronary artery bypass grafting cooperative project: baseline data. Ann Thorac Surg. 1999;68:1592–1598. [DOI] [PubMed] [Google Scholar]
- 2.Holman WL, Allman RM, Sansom M, et al. Alabama coronary artery bypass grafting project: results of a statewide quality improvement initiative. JAMA. 2001;285:3003–3010. [DOI] [PubMed] [Google Scholar]
- 3.Boylan MJ, Lytle BW, Loop FD, et al. Surgical treatment of isolated left anterior descending coronary stenosis: comparison of left internal mammary artery and venous autograft at 18 to 20 years of follow-up. J Thorac Cardiovasc Surg. 1994;107:657–662. [PubMed] [Google Scholar]
- 4.Cohn LH. Use of the internal mammary artery graft and in-hospital mortality and other adverse outcomes associated with coronary artery bypass surgery. Circulation. 2001;103:483–484. [DOI] [PubMed] [Google Scholar]
- 5.Mangano DT, Layug EL, Wallace A, et al. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. N Engl 9J Med. 1996;335:1713–1720. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson TB Jr, Coombs LP, Peterson ED. Preoperative beta-blocker use and mortality and morbidity following CABG surgery in North America. JAMA. 2002;287:2221–2227. [DOI] [PubMed] [Google Scholar]
- 7.Post Coronary Artery Bypass Graft Trial Investigators. The effect of aggressive lowering of low-density lipoprotein cholesterol levels and low-dose anticoagulation on obstructive changes in saphenous vein coronary artery bypass grafts. N Engl J Med. 1997;336:153–162. [DOI] [PubMed] [Google Scholar]
- 8.White CW, Gobel FL, Campeau L, et al. Effect of an aggressive lipid lowering strategy on progression of atherosclerosis in the left main coronary artery from patients in the post coronary artery bypass graft trial. Circulation. 2001;104:2660–2665. [DOI] [PubMed] [Google Scholar]
- 9.Hunninghake DB. Is aggressive cholesterol control justified? Review of the post-coronary artery bypass graft trial. Am J Cardiol. 1998;82:45T–48T. [DOI] [PubMed] [Google Scholar]
- 10.Lee JH, Graber R, Popple CG, et al. Safety and efficacy of early extubation of elderly coronary artery bypass surgery patients. J Cardiothorac Vasc Anesth. 1998;12:381–384. [DOI] [PubMed] [Google Scholar]
- 11.Lee JH, Kim KH, vanHeeckeren DW, et al. Cost analysis of early extubation after coronary bypass surgery. Surgery. 1996;120:611–617. [DOI] [PubMed] [Google Scholar]
- 12.Cheng DC, Karski J, Peniston C, et al. Morbidity outcome in early versus conventional tracheal extubation after coronary artery bypass grafting: a prospective randomized controlled trial. J Thorac Cardiovasc Surg. 1996;112:755–764. [DOI] [PubMed] [Google Scholar]
- 13.Kiefe CI, Weissman NW, Allison JJ, et al. Identifying achievable benchmarks of care: concepts and methodology. Int J Qual Health Care. 1998;10:443–447. [DOI] [PubMed] [Google Scholar]
- 14.Kiefe CI, Allison JJ, Williams OD, et al. Improving quality improvement using achievable benchmarks for physician feedback: a randomized controlled trial. JAMA. 2001;285:2871–2879. [DOI] [PubMed] [Google Scholar]
- 15.O’Connor GT, Plume SK, Olmstead EM, et al. A regional intervention to improve the hospital mortality associated with coronary artery bypass graft surgery: the Northern New England Cardiovascular Disease Study Group [see comments]. JAMA. 1996;275:841–846. [PubMed] [Google Scholar]
- 16.Lazar HL, Fitzgerald CA, Ahmad T, et al. Early discharge after coronary artery bypass graft surgery: are patients really going home earlier? J Thorac Cardiovasc Surg. 2001;121:943–950. [DOI] [PubMed] [Google Scholar]
- 17.Engelman RM, Rousou JA, Flack JE III, et al. Fast-track recovery of the coronary bypass patient. Ann Thorac Surg. 1994;58:1742–1746. [DOI] [PubMed] [Google Scholar]
- 18.Cowper PA, Peterson ED, DeLong ER, et al. Impact of early discharge after coronary artery bypass graft surgery on rates of hospital readmission and death: the Ischemic Heart Disease (IHD) Patient Outcomes Research Team (PORT) Investigators. J Am Coll Cardiol. 1997;30:908–913. [DOI] [PubMed] [Google Scholar]
- 19.Rosen AB, Humphries JO, Muhlbaier LH, et al. Effect of clinical factors on length of stay after coronary artery bypass surgery: results of the cooperative cardiovascular project. Am Heart J. 1999;138:69–77. [DOI] [PubMed] [Google Scholar]
- 20.Weintraub WS, Jones EL, Craver JM, et al. Determinants of prolonged length of hospital stay after coronary bypass surgery. Circulation. 1989;80:276–284. [DOI] [PubMed] [Google Scholar]
- 21.Committee on Regional Health Data Networks. Public Disclosure of Data on Health Care Providers and Practitioners. In: Donaldson MS, Lohr KN, eds. Health Data in the Information Age: Use, Disclosure, and Privacy. Washington, DC: National Academy Press, 1994:91–135. [PubMed] [Google Scholar]
- 22.Hannan EL, Stone CC, Biddle TL, et al. Public release of cardiac surgery outcomes data in New York: what do New York state cardiologists think of it? [corrected and republished article originally printed in Am Heart J. 1997;134:55–61]. Am Heart J. 1997;134:1120–1128. [DOI] [PubMed] [Google Scholar]
- 23.Chassin MR, Hannan EL, DeBuono BA. Benefits and hazards of reporting medical outcomes publicly. N Engl J Med. 1996;334:394–398. [DOI] [PubMed] [Google Scholar]
- 24.Hannan EL, Kilburn HJ, Racz M, et al. Improving the outcomes of coronary artery bypass surgery in New York State. JAMA. 1994;271:761–766. [PubMed] [Google Scholar]
- 25.Erickson LC, Torchiana DF, Schneider EC, et al. The relationship between managed care insurance and use of lower-mortality hospitals for CABG surgery. JAMA. 2000;283:1976–1982. [DOI] [PubMed] [Google Scholar]